Learn about brain health and nootropics to boost brain function
Scientists uncover brain mechanisms for social memory recall in mice
The human brain has the extraordinary ability to rapidly discern a stranger from someone familiar, even as it can simultaneously remember details about someone across decades of encounters. Now, in mouse studies, scientists at Columbia’s Zuckerman Institute have revealed how the brain elegantly performs both tasks.
“These findings are the first evidence that a single population of neurons can use different codes to represent novel and familiar individuals,” said co-corresponding author Stefano Fusi, PhD, professor of neuroscience at Columbia’s Vagelos College of Physicians and Surgeons, a principal investigator at Columbia’s Zuckerman Institute and a member of Columbia’s Center for Theoretical Neuroscience.
In a paper published today in Neuron , Columbia scientists explored social memory, the ability to remember encounters with others. This form of memory consists of two distinct mental processes-;distinguishing novel and familiar individuals, and recalling details about those who are recognized. We can readily determine whether someone is familiar but may have difficulty in recollecting the details of where and how we know that individual, especially when encountered out of context.” Steven A. Siegelbaum, PhD, co-corresponding author, Chair of the Department of Neuroscience at Columbia’s Vagelos College of Physicians and Surgeons Prior work found it difficult to pinpoint how the brain performs both tasks, given their conflicting demands. The ability to detect whether somebody is familiar or not has to apply across many different locations and events, while recollection involves remembering many specific experiences regarding a given individual.
In the new study, the scientists investigated a brain area called CA2, part of the hippocampus, a pair of seahorse-shaped brain structures essential for memory. Dr. Siegelbaum previously made the groundbreaking discovery that CA2 neurons are specifically important for social memory.
The researchers analyzed the brains of mice using calcium imaging, a technique that relies on genetically altered cells-;in this case, in CA2-;that rapidly change color when active. Calcium imaging enabled Lara Boyle, a former MD-PhD student in the Siegelbaum lab and co-first author of the study, to precisely know which neurons they were examining.
“This helped clear up uncertainty from previous research when it came to distinguishing the mouse brain’s responses to novel and familiar individuals,” said Dr. Siegelbaum, the Gerald D. Fischbach, MD, Professor of Neuroscience and of Pharmacology, and a principal investigator at the Zuckerman Institute.
The scientists first recorded how the rodents’ CA2 cells reacted when they were exposed either to a pair of strangers or a pair of familiar littermates. They next used computational methods, led by Dr. Fusi’s team, to analyze the pattern of activity in roughly 400 to 600 neurons in CA2.
The scientists found the same population of neurons encoded memories of both familiar and unfamiliar individuals. Unexpectedly, the neurons used different patterns of activity depending on a mouse’s level of familiarity with another rodent.
When mice were exposed to other mice that were unknown to them, the resulting activity in CA2 was relatively simple or, in the scientists’ parlance, “low-dimensional.” It’s as if several members of an orchestra played the exact same notes, explained Dr. Fusi. In contrast, exposure to familiar littermates led to more complex, high-dimensional CA2 activity, as if the musicians all played different melodies.
The calculations and the simulations of the researchers suggest that the more complex, or higher-dimensional, neural activity can help the brain encode the detailed memories of past encounters with familiar individuals. In contrast, the simpler, or lower-dimensional activity can help the brain reliably identify novel individuals across different contexts.
“When you encounter someone new, you may use abstract categories to describe them in your head-;for instance, that’s a child, with brown hair, red backpack,” said postdoctoral research associate Lorenzo Posani, PhD, a co-first author on the study who led the computational analysis. “Then, as you get to know them, they become a specific person and personality.”
This fundamental discovery regarding the way in which details about others are encoded may shed light on disorders affecting memory.
“When we look at different mouse models of human diseases like schizophrenia or Alzheimer’s that are known to affect memory, we now can ask more precisely how the neural activity supporting familiarity detection and recollection might be altered,” Dr. Siegelbaum said. “Our hope is that what we have learned may lead to a better understanding of the types of interventions that can rescue memory deficits in those disorders.”
The paper, “Tuned geometries of hippocampal representations meet the computational demands of social memory,” was published online in Neuron on TK, 2024.
The full list of authors includes Lara M. Boyle, Lorenzo Posani, Sarah Irfan, Steven A. Siegelbaum and Stefano Fusi.
Source:
Columbia University
Journal reference:
Boyle, L. M., et al. (2024) Tuned geometries of hippocampal representations meet the computational demands of social memory. Neuron. doi.org/10.1016/j.neuron.2024.01.021 .
Be the first to rate this article
Posted in: Medical Science News | Medical Research News
Bio-inspired neuroprosthetics: Sending signals the brain can understand
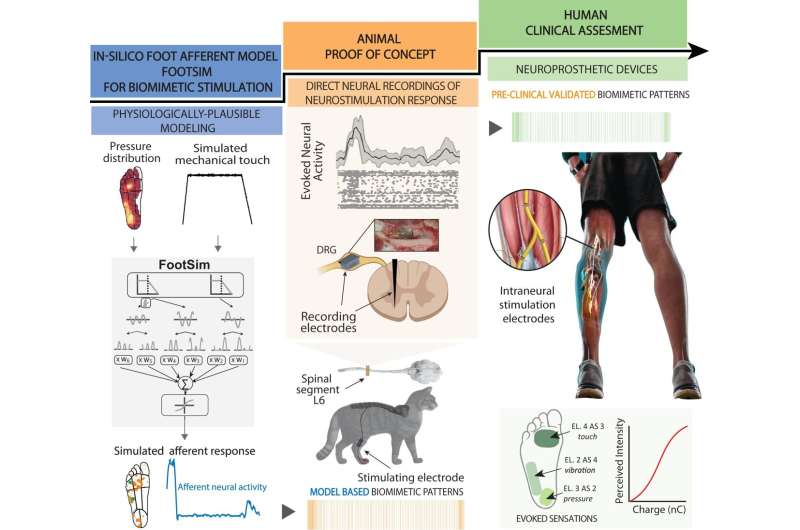
Neuroscience-driven development of a biomimetic neuroprosthetic device. The successful development of a somatosensory neuroprosthesis is based on three main pillars: (1) In-silico models of the biological sensory processing have to be exploited for emulating the natural neural activation of the nervous system to external tactile stimuli (blue segment); (2) animal proof of concept allows for experimental validation of the mechanisms behind the use of specific neurostimulation strategies defined with the use of modeling (orange segment); (3) A rigorous clinical validation of the biomimetic technology with implanted humans has to be performed in order to assess the functional outcomes in real-life scenarios (green segment). Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-45190-6 A few years ago, a team of researchers working under Professor Stanisa Raspopovic at the ETH Zurich Neuroengineering Lab gained worldwide attention when they announced that their prosthetic legs had enabled amputees to feel sensations from this artificial body part for the first time.
Unlike commercial leg prostheses, which simply provide amputees with stability and support, the ETH researchers’ prosthetic device was connected to the sciatic nerve in the test subjects’ thigh via implanted electrodes.
This electrical connection enabled the neuroprosthesis to communicate with the patient’s brain, for example relaying information on the constant changes in pressure detected on the sole of the prosthetic foot when walking. This gave the test subjects greater confidence in their prosthesis—and it enabled them to walk considerably faster on challenging terrains.
“Our experimental leg prosthesis succeeded in evoking natural sensations. That’s something current neuroprostheses are mainly unable to do; instead, they mostly evoke artificial, unpleasant sensations,” Raspopovic says.
This is probably because today’s neuroprosthetics are using time-constant electrical pulses to stimulate the nervous system. “That’s not only unnatural, but also inefficient,” Raspopovic says.
In a recently published paper in Nature Communications , he and his team used the example of their leg prostheses to highlight the benefits of using naturally inspired, biomimetic stimulation to develop the next generation of neuroprosthetics. Model simulates activation of nerves in the sole
To generate these biomimetic signals, Natalija Katic—a doctoral student in Raspopovic’s research group—developed a computer model called FootSim. It is based on data collected by collaborators in Canada, who recorded the activity of natural receptors, named mechanoreceptors, in the sole of the foot while touching different points on the feet of volunteers with a vibrating rod.
The model simulates the dynamic behavior of large numbers of mechanoreceptors in the sole of the foot and generates the neural signals that shoot up the nerves in the leg towards the brain—from the moment the heel strikes the ground and the weight of the body starts to shift forward to the outside of the foot until the toes push off the ground ready for the next step.
“Thanks to this model, we can see how sensory receptors from the sole, and the connected nerves, behave during walking or running, which is experimentally impossible to measure,” Katic says. Information overload in the spinal cord
To assess how closely the biomimetic signals calculated by the model correspond to the signals emitted by real neurons, Giacomo Valle—a postdoc in Raspopovic’s research group—worked with colleagues in Germany, Serbia and Russia on experiments with cats, whose nervous system processes movement in a similar way to that of humans. The experiments took place in 2019 at the Pavlov Institute of Physiology in St. Petersburg and were carried out in accordance with the relevant European Union guidelines.
The researchers implanted electrodes, connecting some to the nerve in the leg and some to the spinal cord to discover how the signals are transmitted through the nervous system. When the researchers applied pressure to the bottom of the cat’s paw, thereby evoking the natural neural response that occurs when a cat takes a step, the peculiar pattern of activity recorded in the spinal cord did indeed resemble the patterns that were elicited in the spinal cord when the researchers stimulated the leg nerve with biomimetic signals.
By contrast, the conventional approach of time-constant stimulation of the sciatic nerve in the cat’s thigh elicited a markedly different pattern of activation in the spinal cord. “This clearly shows that the commonly used stimulation methods cause the neural networks in the spine to be flooded with information,” Valle says. “This information overload could be the reason for the unpleasant sensations or paraesthesia reported by some users of neuroprosthetics,” Raspopovic adds. Learning the language of the nervous system
In their clinical trial with leg amputees, the researchers were able to show that biomimetic stimulation is superior to time-constant stimulation. Their work clearly demonstrated how the signals that mimicked nature produced better results: not only were the test subjects able to climb steps faster, they also made fewer mistakes in a task that required them to climb the same steps while spelling words backwards.
“Biomimetic neurostimulation allows subjects to concentrate on other things while walking,” Raspopovic says, “so we concluded that this type of stimulation is more naturally processed and less taxing on the brain.”
Raspopovic, whose lab forms part of the ETH Institute of Robotics and Intelligent Systems, believes that these new findings are not only relevant to the limb prostheses he and his team have been working on for over half a decade. He argues that the need to move away from unnatural, time-constant stimulation towards biomimetic signals also applies to a whole series of other aids and devices, including spinal implants and electrodes for brain stimulation.
“We need to learn the language of the nervous system,” Raspopovic says. “Then we’ll be able to communicate with the brain in ways it really understands.”
More information: Giacomo Valle et al, Biomimetic computer-to-brain communication enhancing naturalistic touch sensations via peripheral nerve stimulation, Nature Communications (2024). DOI: 10.1038/s41467-024-45190-6
Provided by ETH Zurich
Study suggests how brain waves are part of memory

Representative image. Image Credit: ANI Spatial navigation and memory are essential components of our daily lives. Without these talents, we would struggle to navigate our surroundings and remember previous experiences. However, the neural foundation of spatial memory remains poorly known. A study group directed by Prof. Lukas Kunz, who just joined the University Hospital Bonn (UKB), has discovered fresh information on this knowledge gap. He discovered, along with scientists from New York and Freiburg, that different types of nerve cells become active simultaneously during spatial memory and are coordinated by brain waves (“ripples”). The findings have now been published in the journal Nature Neuroscience.
Associative memory allows different pieces of information are linked together. “In the context of spatial memory, associative memory enables us to remember the locations of certain objects in the spatial environment,” explains Prof. Kunz, research group leader for Cognitive and Translational Neuroscience at the Department of Epileptology at the UKB. He is also a member of the Transdisciplinary Research Area (TRA) “Life & Health” at the University of Bonn. “For example, we can remember where in the house we put our keys”. At older age or in certain diseases such as Alzheimer’s, however, this ability is limited. “It is therefore important to investigate the neuronal basis of different forms of human memory,” said Prof. Kunz. In the long term, this could help develop new therapies for memory impairments.
Nerve cells are active while information is retrieved from memory. To further investigate this phenomenon, the researchers recorded the activity of individual nerve cells in epilepsy patients performing a memory task. “In a virtual world, the participants were asked to remember the locations of different objects,” explains Prof. Kunz. The recordings showed that different types of nerve cells became active during this memory task. Some nerve cells responded to certain objects, while other nerve cells activated in response to certain locations. The scientists observed that interactions between the different types of nerve cells became stronger over time when participants remembered the right object in the right place.
In addition to place and object neurons, the researchers observed hippocampal brain waves (“ripples”) that also occurred during the memory task, presumably playing a crucial role in the formation and retrieval of associative memories. “Ripples could be important for the connection of different types of nerve cells and the formation of complex memories. It will be exciting to further investigate this idea in future studies,” explains Prof. Kunz. It will also be interesting to study how memory performance is modulated when ripples are suppressed or triggered, providing insights into the causal relevance of ripples. Prof. Kunz intends to continue the findings that he gained with his colleagues at Columbia University’s School of Engineering and Applied Science in New York and the University of Freiburg at the University Hospital Bonn.
“The department of epileptology at the UKB is well-known for its excellent brain research. The department has the unique opportunity to record the activity of individual nerve cells in the human brain in the video EEG monitoring unit, which is the heart of every epilepsy center. This provides exciting insights into the functioning of the human brain, which is only possible at a few research centers worldwide,” describes Prof. Kunz. In his interdisciplinary research, he builds on the close exchange with other researchers and medical doctors, which is essential for the development of new research ideas. (ANI)
(This story has not been edited by Devdiscourse staff and is auto-generated from a syndicated feed.)
Neuroscientist Shares Five Supplements To Improve Memory And Reduce Risk Of Alzheimer’s

In the quest for cognitive well-being, understanding the supplements that can genuinely make a difference is paramount. Neuroscientist Robert W.B. Love took to Instagram to shed light on five supplements that hold the potential to enhance memory and reduce the risk of Alzheimer’s. Let’s delve into the nuanced details of these scientifically-backed options, providing a robust foundation for fortifying brain health. Supplements To Improve Memory And Reduce Risk Of Alzheimer’s
View this post on Instagram A post shared by Robert W.B. Love (@robertwblove) Magnesium Threonate: A Potential Cognitive Booster
Magnesium L-threonate emerges as a promising cognitive booster, supported by studies demonstrating its ability to shield against brain cell death. Preliminary research conducted on zebrafish and mouse models underscores its efficacy in preserving cognitive function. Magnesium threonate not only shows promise in memory improvement but also in addressing nerve pain. This supplement offers a sneak peek into the evolving landscape of brain health supplements, hinting at potential breakthroughs in cognitive enhancement.
Also Read: 7 Alzheimer’s Disease Facts To Be Aware Of On World Alzheimer’s Day 2023 Ceylon Cinnamon: Cognitive Function and Alzheimer’s Risk Reduction
Beyond its culinary allure, Ceylon Cinnamon, also known as True Cinnamon, unfolds as a multifaceted ally in cognitive well-being. Recent research illuminates its impact on cognitive function, unveiling neuroprotective qualities. The spice’s properties extend to combating inflammation, fortifying the immune response, and reducing cancer risk through its antioxidant prowess. From disrupting oxidative stress to inhibiting tau protein accumulation, Ceylon Cinnamon emerges as a natural asset in the endeavour to reduce Alzheimer’s risk and preserve memory. Fish Oil: Omega-3 Fatty Acids for Brain Health
Derived from fatty fish, fish oil takes centre stage with its rich content of omega-3 fatty acids, specifically EPA and DHA, renowned for cardiovascular benefits. Expanding beyond its recognized role in heart health, fish oil showcases profound impacts on brain function, particularly in addressing mild memory loss and depression. Exploring its potential to enhance brain function in conditions like mild cognitive impairment opens a promising avenue for advancing cognitive well-being. In the realm of brain health supplements, fish oil emerges as a beacon of hope, offering potential life-changing discoveries for those grappling with cognitive challenges. Zinc: A Crucial Trace Element for Memory Formation
Zinc, a trace element, assumes a pivotal role in the creation of new neurons in the brain’s hippocampus, a cornerstone for memory formation. Adequate zinc levels play a protective role, supporting the synthesis of memories, emotions, and sensations. Disruptions in this intricate process can be mitigated with sufficient zinc levels, offering a safeguard against memory-related challenges and cognitive impairment. Beyond memory formation, zinc contributes to effective communication among brain cells, acting as a defender against the nebulous realm of cognitive challenges.
Also Read: Alzheimer’s Disease: Here’s How You Can Embrace Lifestyle Changes For Optimal Brain Health Lion’s Mane: A Nootropic for Cognitive Health
Lion’s Mane, categorized as a nootropic, unveils a trove of compounds that contribute to improved brain health and function. Notably, its impact on nerve growth factor levels positions it as a potential shield against disorders like Alzheimer’s. Scientific trials indicate its effectiveness in alleviating symptoms of mild cognitive impairment, presenting Lion’s Mane as a natural remedy for cognitive enhancement. As the understanding of cognitive health evolves, Lion’s Mane stands out as a fascinating avenue for those seeking a natural and research-backed approach to fortify cognitive resilience. Bottomline
In the ever-evolving landscape of neuroscience, these supplements offer a spartan yet compelling approach to memory improvement and Alzheimer’s risk reduction. Exploring these supplements, firmly grounded in scientific research, becomes a journey toward fortifying cognitive resilience and embracing a future where cognitive well-being takes centre stage.
Neuroscientist Shares Five Supplements To Improve Memory And Reduce Risk Of Alzheimer’s

In the quest for cognitive well-being, understanding the supplements that can genuinely make a difference is paramount. Neuroscientist Robert W.B. Love took to Instagram to shed light on five supplements that hold the potential to enhance memory and reduce the risk of Alzheimer’s. Let’s delve into the nuanced details of these scientifically-backed options, providing a robust foundation for fortifying brain health. Supplements To Improve Memory And Reduce Risk Of Alzheimer’s
View this post on Instagram A post shared by Robert W.B. Love (@robertwblove) Magnesium Threonate: A Potential Cognitive Booster
Magnesium L-threonate emerges as a promising cognitive booster, supported by studies demonstrating its ability to shield against brain cell death. Preliminary research conducted on zebrafish and mouse models underscores its efficacy in preserving cognitive function. Magnesium threonate not only shows promise in memory improvement but also in addressing nerve pain. This supplement offers a sneak peek into the evolving landscape of brain health supplements, hinting at potential breakthroughs in cognitive enhancement.
Also Read: 7 Alzheimer’s Disease Facts To Be Aware Of On World Alzheimer’s Day 2023 Ceylon Cinnamon: Cognitive Function and Alzheimer’s Risk Reduction
Beyond its culinary allure, Ceylon Cinnamon, also known as True Cinnamon, unfolds as a multifaceted ally in cognitive well-being. Recent research illuminates its impact on cognitive function, unveiling neuroprotective qualities. The spice’s properties extend to combating inflammation, fortifying the immune response, and reducing cancer risk through its antioxidant prowess. From disrupting oxidative stress to inhibiting tau protein accumulation, Ceylon Cinnamon emerges as a natural asset in the endeavour to reduce Alzheimer’s risk and preserve memory. Fish Oil: Omega-3 Fatty Acids for Brain Health
Derived from fatty fish, fish oil takes centre stage with its rich content of omega-3 fatty acids, specifically EPA and DHA, renowned for cardiovascular benefits. Expanding beyond its recognized role in heart health, fish oil showcases profound impacts on brain function, particularly in addressing mild memory loss and depression. Exploring its potential to enhance brain function in conditions like mild cognitive impairment opens a promising avenue for advancing cognitive well-being. In the realm of brain health supplements, fish oil emerges as a beacon of hope, offering potential life-changing discoveries for those grappling with cognitive challenges. Zinc: A Crucial Trace Element for Memory Formation
Zinc, a trace element, assumes a pivotal role in the creation of new neurons in the brain’s hippocampus, a cornerstone for memory formation. Adequate zinc levels play a protective role, supporting the synthesis of memories, emotions, and sensations. Disruptions in this intricate process can be mitigated with sufficient zinc levels, offering a safeguard against memory-related challenges and cognitive impairment. Beyond memory formation, zinc contributes to effective communication among brain cells, acting as a defender against the nebulous realm of cognitive challenges.
Also Read: Alzheimer’s Disease: Here’s How You Can Embrace Lifestyle Changes For Optimal Brain Health Lion’s Mane: A Nootropic for Cognitive Health
Lion’s Mane, categorized as a nootropic, unveils a trove of compounds that contribute to improved brain health and function. Notably, its impact on nerve growth factor levels positions it as a potential shield against disorders like Alzheimer’s. Scientific trials indicate its effectiveness in alleviating symptoms of mild cognitive impairment, presenting Lion’s Mane as a natural remedy for cognitive enhancement. As the understanding of cognitive health evolves, Lion’s Mane stands out as a fascinating avenue for those seeking a natural and research-backed approach to fortify cognitive resilience. Bottomline
In the ever-evolving landscape of neuroscience, these supplements offer a spartan yet compelling approach to memory improvement and Alzheimer’s risk reduction. Exploring these supplements, firmly grounded in scientific research, becomes a journey toward fortifying cognitive resilience and embracing a future where cognitive well-being takes centre stage.
The One Psychological Brain Tool That Can Create A More Positive Mindset, According To A Psychologist

The One Psychological Brain Trick That Can Create A More Positive Mindset, According To A Psychologist Our thoughts, beliefs, and attitudes shape our perception of the world and influence our experiences. While this may cause some to have an inherently negative perception of life, there’s an effective psychological brain tool that can help you perceive the world through a more positive lens. A brain training specialist took to TikTok to share one psychological brain trick that transformed her life.
Emilie Leyes , a hypnosis practitioner and podcast host of “How To Like Your Life,” posted a video on TikTok to share the one brain tool she incorporated into her life that helped her “stop [her] brain from thinking so negatively all the time” and adopt a more positive mindset.
Leyes explained how the human brain struggles with negativity bias , meaning we tend to focus more heavily on the impact of negative experiences rather than positive ones.
RELATED: 3 Neurological Tricks To Get The Exact Life You Want
“That used to support us back in early human evolution, but it just doesn’t anymore. It keeps us from enjoying the good things that do actually happen to us,” Leyes said.
Developed by Rick Hanson, Ph.D ., a neuropsychologist and best-selling author, we can rewire our minds to perceive the world with more optimism using a tool called installation, a mindfulness practice that encourages awareness and gratitude for all the positive things in our lives.
“It’s all about noticing the positive experiences that we actually have in our lives that normally pass us by because of this negativity bias, but then deliberately keeping your attention on it, and growing and amplifying the emotional experiences that you’re having within that good thing so that it can actually change your brain and have an impact on you,” Leyes expressed. Leyes explained there are three steps to learning how to appreciate the good in your life:
1. Notice the positive experiences throughout your day
Pay attention to the little joys that surround you in your day. Not every day will be a great one, but there is always something to be grateful for. These positive experiences could be noticing a dog riding in a car with his head out the window, hearing a funny story from a co-worker, discovering a new song that you love, or simply going for a walk outside.
RELATED: 10 Tiny Habits That Will Make You More Positive Than 98% Of People 2. Stay with the experience
Similarly to how we tend to let negative experiences affect our days, absorb the positive experiences instead! Allow yourself to sit with this positive encounter to intensify its impact.
“Turn up the volume on the good feelings that you’re experiencing,” Leyes suggested.
According to a webinar session with Dr. Hanson and Ruth Buczynski, Ph.D., “It takes around 30 seconds for an experience to really register in the brain, body, and mind, enough to have a lasting impact.” 3. Set an intention to allow this experience to make your day
After practicing the mindfulness of the first two steps, let yourself feel grateful for the positive experiences that left a mark on you. Let these experiences change you and lift your spirits.
Remember the smile you made seeing the joy of a furry friend having the time of his life on a car ride, hold on to the laughter you exchanged with your colleague, and let the powerful notes and lyrics of that great new song replay in your mind.
Life is hard enough on us— we don’t need to add to our stress by ignoring the daily positive experiences of our lives because the negative ones seem to hold more weight.
RELATED: How To Trick Your Brain Into Releasing Chemicals That Make You Happy There are other ways to reverse negativity bias and live a life rich in gratitude.
Katerina Barrata , a licensed associate counselor, shared some good news on TikTok about the reality of negativity bias . In her video, Barrata explained how research developed by Laura Carstensen , a professor of psychology at Stanford University, shows that negativity bias actually “declines, and even reverses, in old age.”
Additionally, you can train your mind to convert your inherently negative perspective to a positive one by simply “[contemplating] your own mortality.”
This method, also known as maranasati meditation in Buddhism , essentially conveys the impermanence of our lives and enforces the virtue of being present.
Related Stories From YourTango:
The Life-Changing Reason To Choose Your Words Carefully
5 Loving Ways To Save Your Relationship From Toxic Negativity
5 Psychological Self-Love Techniques That Can Improve Your Life
Buddhists have practiced this meditation technique for thousands of years to “deepen their appreciation and gratitude for their precious human life.”
By recognizing the transience of our lives, we can learn to cultivate gratitude for every day we’re alive and get to experience the little joys and pleasures that are indubitably not so little. You decide how much power your daily experiences hold over you. The truth is, the obstacles and challenges that frequently cross our paths are inevitable, but we get to choose how these experiences affect us . Life is too short to spend worrying about all the problems we face throughout our lives.It’s important to understand this perspective doesn’t suggest avoiding or ignoring our problems, rather it offers useful tools to help us rise above our challenges and focus our attention on what truly matters — love, gratitude, and hope. RELATED: 7 Psychological Tricks To Help You Get Stuff Done — Even On Days You Don’t Feel Like It Francesca Duarte is a writer on YourTango’s news and entertainment team based in Orlando, FL. She covers lifestyle, human-interest, and spirituality topics.
Are stressed-out brain cells the root cause of neurodegenerative disease?
Many neurodegenerative diseases, such as Alzheimer’s and Parkinson’s diseases, are characterized by the accumulation of protein clumps, or aggregates, in the brain, which has led scientists to assume that the protein tangles kill brain cells. The search for treatments that break up and remove these tangled proteins has had little success, however.
But a new discovery by University of California, Berkeley, researchers suggests that the accumulation of aggregated proteins isn’t what kills brain cells. Rather, it’s the body’s failure to turn off these cells’ stress response.
In a study published online Jan. 31 in the journal Nature , the researchers reported that delivering a drug that forces the stress response to shut down saves cells that mimic a type of neurodegenerative disease known as early-onset dementia.
According to lead researcher Michael Rapé, the finding could offer clinicians another option for treatment for some neurodegenerative diseases, at least for those caused by mutations in the protein that switches off the cellular stress response. These include inherited diseases that lead to ataxia, or loss of muscle control, and early-onset dementia.
In addition, Rapé noted that other neurodegenerative diseases, including Mohr-Tranebjærg syndrome, childhood ataxia and Leigh syndrome, are also characterized by stress responses in overdrive and have symptoms similar to those of the early onset dementia mimicked in the new study.
“We always thought that protein clumps directly kill neurons, for example by puncturing membrane structures within these cells. Yet, we now found that aggregates prevent silencing of a stress response that cells originally mount to cope with bad proteins. The stress response is always on, and that’s what kills the cells,” said Rapé, head of the new division of molecular therapeutics in UC Berkeley’s Department of Molecular and Cell Biology and a Howard Hughes Medical Institute investigator. “We think that the same mechanisms may underlie more common pathologies that also show widespread aggregation, such as Alzheimer’s disease or frontotemporal dementia, but more work is needed to investigate the role of stress signaling in these diseases.”
Key to the discoveries by Rapé’s lab was the researchers’ finding that stress responses need to be turned off once a brain cell has successfully addressed a difficult situation. Rapé explained this finding to his son in simple terms: You not only need to clean up your room, but also turn out the light before going to bed. If you don’t turn off the light, you can’t fall asleep, but if you turn it off before you cleaned up your room, you would stumble if you had to get up in the dark.
Similarly, a cell has to clean up protein aggregates before turning off the stress response. If it doesn’t turn off the stress response, the cell will ultimately die.
“Aggregates don’t kill cells directly. They kill cells because they keep the light on,” he said. “But that means that you can treat these diseases, or at least the dozen or so neurodegenerative diseases that we found have kept their stress responses on. You treat them with an inhibitor that turns off the light. You don’t have to worry about completely getting rid of large aggregates, which changes how we think about treating neurodegenerative diseases. And most importantly, it makes this really doable.”
In their paper, Rapé and his colleagues describe a very large protein complex they discovered and called SIFI (SIlencing Factor of the Integrated stress response). This machine serves two purposes: It cleans up aggregates and, afterward, turns off the stress response triggered by the aggregated proteins. The stress response controlled by SIFI is switched on to deal with specific intracellular problems — the abnormal accumulation of proteins that end up at the wrong location in the cell. If components of SIFI are mutated, the cell will accumulate protein clumps and experience an active stress response. But it is the stress response signaling that kills the cells.
“The SIFI complex would normally clear out the aggregating proteins. When there are aggregates around, SIFI is diverted from the stress response, and the signaling continues. When aggregates have been cleared — the room has been cleaned up before bedtime — then the SIFI is not diverted away anymore, and it can turn off the stress response,” he said. “Aggregates kind of hijack that natural stress response-silencing mechanism, interfere with it, stall it. And so that’s why silencing never happens when you have aggregates, and that’s why cells die.”
A future treatment, Rapé said, would likely involve administration of a drug to turn off the stress response and a drug to keep SIFI turned on to clean up the aggregate mess.
Ubiquitin
Rapé, who is also the Dr. K. Peter Hirth Chair of Cancer Biology, studies the role of ubiquitin — a ubiquitous protein in the body that targets proteins for degradation — in regulating normal and disease processes in humans. In 2017, he discovered that a protein called UBR4 assembles a specific ubiquitin signal that was required for the elimination of proteins that tend to aggregate inside cells.
Only later did other researchers find that mutations in UBR4 are found in some inherited types of neurodegeneration. This discovery led Rapé to team up with colleagues at Stanford University to find out how UBR4 causes these diseases.
“This was a unique opportunity: We had an enzyme that makes an anti-aggregation signal, and when it’s mutated, it causes aggregation disease,” he said. “You put these two things together and you can say, ‘If you figure out how this UBR4 allows sustained cell survival, that probably tells you how aggregates kill cells.'”
They found that UBR4 is actually part of a much larger protein complex, which Rapé dubbed SIFI, and they found that this SIFI machinery was needed when a cell couldn’t sort proteins into its mitochondria. Such proteins that end up at the wrong location in cells tend to clump and, in turn, cause neurodegeneration.
“Surprisingly, though, we found that the core substrates of the SIFI complex were two proteins, one of which senses when proteins don’t make it into mitochondria. That protein detects that something is wrong, and it then activates […]
LOCKDOWNS KILL: Study reveals social isolation can increase inflammation in the body

According to a study, spending too much time on your own can increase inflammation in the body . Details of the study were published in the journal Brain, Behavior, and Immunity.
The research team warned that being excessively solitary may impact both your mental health and your physical health. This highlights the often-forgotten importance of balancing your digital connections and the need for genuine human interaction.
The researchers conducting the study focused on “the impact of social isolation during early adulthood and midlife .” The results showed that there was a strong correlation between loneliness and inflammation markers.
The research team also said it was worth noting how childhood isolation was closely linked to higher soluble urokinase plasminogen activator receptor (suPAR) levels, a marker of chronic inflammation.
They added that this association persisted into adulthood, highlighting the long-lasting effect of early-life social experiences on inflammatory responses.
The research used diverse data sources to support their findings, such as data from the TRIAGE Danish study, a longitudinal study conducted in New Zealand and a comprehensive British twin analysis. The combined findings consistently stressed the crucial role of social isolation in influencing inflammation levels, as specifically evidenced by suPAR.
Overall, the study shows the negative consequences of social isolation , especially when living alone, because it contributes to elevated suPAR levels, signaling chronic inflammation.
This link also proved robust across various demographic groups, suggesting that social experiences may have a lasting influence on the body’s inflammatory responses over time. (Related: Thai black ginger found to delay arthritis progression and suppress inflammation .) Avoid social isolation by fostering healthy relationships and caring for your overall well-being
You may find yourself spending a lot of time on your devices and social media in today’s modern world.
If you are worried about your physical and mental health, follow these tips to improve your social connections and create a sense of community.
They can also help prevent social isolation linked to inflammation:
Join group activities
If you have different hobbies but no one to share them with, look for group activities or classes in your neighborhood.
Joining these groups will help you share your love for your interests, like a book club or gym class.
Volunteer in your community
Volunteering doesn’t just help you feel like part of your community, it also gives you a chance to contribute to a greater cause as you connect with others who share your passion for making a positive impact.
Volunteering at the local animal shelter or soup kitchen is a fulfilling way to build a sense of community.
Attend local events
Instead of mindlessly scrolling social media while you’re in bed, go outside and explore different events in your local community.
In your free time, attend gatherings, workshops, or cultural events to meet new people and expand your social circle.
Stay connected with loved ones
Don’t spend all day at work or binge-watching TV.
Regularly reach out to your family and friends. If they’re too far away to visit, call them on the phone, video chat, or send a handwritten letter to help maintain strong connections.
Use digital platforms mindfully
Leverage social media to stay connected with friends and family.
Just make sure you’re always mindful of screen time. It’s also better to prioritize in-person or meaningful virtual interactions to strengthen your relationships. Practice active listening Talking to family and friends won’t do you any good if you have poor active listening skills.When engaging in conversations, practice active listening. You can do this by showing genuine interest in a friend’s stories and experiences. Adopt a pet Pets can help improve your physical and mental health, especially since they provide companionship and love.If you are physically able to care for a pet, adopt a dog . They’re great companions because many dog breeds are active and require regular physical activity, which is also good for you if you’re feeling low.You can also meet new people by walking your dog to the nearest park.Keep in mind that fighting social isolation is an ongoing process that requires your continued efforts to nurture connections and create a supportive social environment. Maintain healthy habits and care for both your physical and mental health to prevent inflammation linked to many health issues.Visit Mental.news for more stories about how loneliness and social isolation can affect your mental health and overall well-beingWatch the video below to learn how turmeric can help with inflammation .This video is from the All About Herbs channel on Brighteon.com . More related stories: Chinese medicinal herb astragalus found to reduce inflammation and improve immunity in heart attack patients. Loneliness increases risk of PREMATURE DEATH by nearly 30%, declared an EPIDEMIC by surgeon general. Study shows EXTRA VIRGIN COCONUT OIL can promote weight loss, reduce body fat and improve liver health. Anti-inflammatory superfoods: Fight inflammation with this creamy broccoli soup recipe. Sources include: NaturalHealth365.com ScienceDirect.com HealthDirect.gov.au Brighteon.com
Breakthrough AI Uses Brain Scans to Predict Antidepressant Effectiveness in Just One Week

Researchers from Amsterdam UMC and Radboudumc have developed an AI algorithm capable of predicting the effectiveness of antidepressants within just a week of treatment initiation. This promising technique employs brain scans coupled with clinical information to rapidly determine whether sertraline—one of the most commonly prescribed antidepressants—will alleviate symptoms of major depressive disorder (MDD), a condition that affects approximately 280 million people globally.
Traditionally, the efficacy of an antidepressant can take anywhere from six to eight weeks to assess, a lengthy period fraught with patient anxiety and the potential exacerbation of symptoms. The current methodology not only delays relief for those suffering but also bears significant economic and social costs due to reduced patient productivity and increased healthcare expenses.
The study, published in the American Journal of Psychiatry, involved analyzing MRI brain scans and clinical data from 229 patients who participated in a prior study conducted by the University of Texas Southwestern Medical Center and affiliated institutions. The Amsterdam team’s AI algorithm was then applied to this dataset to predict individual responses to sertraline treatment after just one week.
“The algorithm suggested that those who had a lot of blood flow in the anterior cingulate cortex, the area of brain involved in emotion regulation, would be helped by the drug. And at the second measurement, a week after the start, this turned out to be the severity of their symptoms,” articulated Eric Ruhé, psychiatrist at Radboudumc, elucidating the biological markers the AI used to predict treatment success.
This could revolutionize the approach to prescribing antidepressants. Notably, the algorithm correctly identified one-third of patients as likely responders to the drug, potentially avoiding two-thirds of ineffective sertraline prescriptions. By doing so, it mitigates the patient’s burden of unnecessary side effects and reduces the societal costs linked with prolonged depressive episodes.
“For patients, it means better quality of care,” emphasized Professor Liesbeth Reneman from Amsterdam UMC. By enabling earlier intervention with the correct medication, this AI-driven method holds the potential to drastically improve the quality of life for individuals with MDD by promptly restoring well-being and reducing the risk of comorbidities associated with prolonged depression.
The researchers are committed to further refining the algorithm by adding more data, which could enhance its predictive accuracy and clinical applicability. This commitment signals a shift towards more personalized and precise mental health treatment—ushering in an era where AI augments clinical decisions to deliver faster, more effective care to those battling depression.
Relevant articles:
– Artificial intelligence helps predict whether antidepressants will work in patients. By inputting a brain scan and an individual’s clinical information into an AI algorithm, researchers from Amsterdam UMC and Radboudumc could see up to 8 weeks faster whether or not the medication would work
– AI in Precision Medicine: Predicting Antidepressant Outcomes , Psychology Today, Fri, 09 Feb 2024 02:13:53 GMT
– AI Predicts Antidepressant Success in a Week , Neuroscience News, Wed, 07 Feb 2024 14:39:11 GMT
– Breakthrough in depression treatment: AI predicts antidepressant response within a week , Open Access Government, Wed, 07 Feb 2024 13:08:01 GMT
As Biden’s memory issues draw attention, neurologists weigh in

Win McNamee Since a report released on Thursday by special counsel Robert Hur described President Joe Biden as an “elderly man with a poor memory,” there have been significant misperceptions about the cognitive changes associated with aging, neurologists say.
The report on Biden’s handling of classified documents noted that the president hadn’t remembered the exact time frame that he served as vice president and was struggling to recall the period when his late son, Beau Biden, had passed away. Biden defiantly rejected the changes in a press conference late Thursday , saying “my memory’s fine.”
There’s also been scrutiny of other recent events when the 81-year-old president mixed up names of foreign leaders .
However, neurologists say blanking on the names of acquaintances or having difficulty remembering dates from the past, especially when under stress, can simply be part of normal aging.
“If you asked me when my mother passed away, I couldn’t necessarily tell you the exact year because it was many years ago,” Dr. Paul Newhouse, clinical core leader for the Vanderbilt Alzheimer’s Disease Research Center, said.
Almost every older patient has trouble remembering people’s names, Newhouse said.
“I think it’s by far the most universal complaint of every person as they age,” Newhouse said.
In Newhouse’s experience, this type of forgetfulness doesn’t actually predict who ends up having memory disorders. Only a person’s doctor or neurologist can make that diagnosis, not outside observers, brain experts say.
Dr. Dennis Selkoe, co-director of the Ann Romney Center for Neurologic Diseases at Brigham and Women’s Hospital in Boston, agreed that forgetting names doesn’t actually provide much insight into potential memory problems. In fact, stress and a lack of sleep, can interfere with memory, no matter how old someone is.
“Naming proper nouns is not an adequate basis to make a conclusion about whether an individual has a more consistent and more concerning substantive progressive memory disorder,” Selkoe said. What are normal memory changes?
It’s normal for older brains to have more difficulty retaining new information and then retrieving the information, but mental processes like decision-making and judgment can actually improve with age, said Dr. Thomas Wisniewski, director of NYU Langone Health’s Alzheimer’s Disease Research Center and its Center for Cognitive Neurology.
“Although the raw power of memory has some degree of decline, perhaps wisdom can increase because the individual has a greater backlog of experiences and different situations as to what is the best thing to do,” Wisniewski said.
The problem isn’t having trouble remembering names or calling someone by the wrong name, but when someone’s memory is fuzzy about recent or past experiences, said Newhouse. Issues with episodic memory — memory for events in time or if a person doesn’t remember going shopping, for example — can be a sign of a progressive disorder, but not always.
Wisniewski said he becomes concerned when people don’t even recognize that they are forgetting things.
“They forgot that they went shopping and they’re unaware that they’ve forgotten,” he said.
Overall, neurologists tend to worry less about a patient’s ability to remember remote memories from many years ago and more troubled by an inability to recall more recent events. That’s because dementia first affects the part of the brain that’s responsible for short-term memories, as opposed to long-term memories, said Newhouse.
“What I’m more concerned about is, can you remember what happened yesterday? Or an hour ago?” Newhouse said.
While the conversation surrounding aging is often framed around a person’s diminishing memory or executive functioning, there are cognitive benefits that come with growing older, Selkoe said.
“There is a type of emotional intelligence and ability to handle many different kinds of experiences in life that come with greater longevity,” he said. “People can make decisions more carefully and more rationally.”
As Biden’s memory issues draw attention, neurologists weigh in

Since a report released on Thursday by special counsel Robert Hur described President Joe Biden as an “elderly man with a poor memory,” there have been significant misperceptions about the cognitive changes associated with aging, neurologists say.
The report on Biden’s handling of classified documents noted that the president hadn’t remembered the exact time frame that he served as vice president and was struggling to recall the period when his late son, Beau Biden, had passed away. Biden defiantly rejected the changes in a press conference late Thursday , saying “my memory’s fine.”
There’s also been scrutiny of other recent events when the 81-year-old president mixed up names of foreign leaders .
However, neurologists say blanking on the names of acquaintances or having difficulty remembering dates from the past, especially when under stress, can simply be part of normal aging.
“If you asked me when my mother passed away, I couldn’t necessarily tell you the exact year because it was many years ago,” Dr. Paul Newhouse, clinical core leader for the Vanderbilt Alzheimer’s Disease Research Center, said.
Almost every older patient has trouble remembering people’s names, Newhouse said.
“I think it’s by far the most universal complaint of every person as they age,” Newhouse said.
In Newhouse’s experience, this type of forgetfulness doesn’t actually predict who ends up having memory disorders. Only a person’s doctor or neurologist can make that diagnosis, not outside observers, brain experts say.
Dr. Dennis Selkoe, co-director of the Ann Romney Center for Neurologic Diseases at Brigham and Women’s Hospital in Boston, agreed that forgetting names doesn’t actually provide much insight into potential memory problems. In fact, stress and a lack of sleep, can interfere with memory, no matter how old someone is.
“Naming proper nouns is not an adequate basis to make a conclusion about whether an individual has a more consistent and more concerning substantive progressive memory disorder,” Selkoe said. What are normal memory changes?
It’s normal for older brains to have more difficulty retaining new information and then retrieving the information, but mental processes like decision-making and judgment can actually improve with age, said Dr. Thomas Wisniewski, director of NYU Langone Health’s Alzheimer’s Disease Research Center and its Center for Cognitive Neurology.
“Although the raw power of memory has some degree of decline, perhaps wisdom can increase because the individual has a greater backlog of experiences and different situations as to what is the best thing to do,” Wisniewski said.
The problem isn’t having trouble remembering names or calling someone by the wrong name, but when someone’s memory is fuzzy about recent or past experiences, said Newhouse. Issues with episodic memory — memory for events in time or if a person doesn’t remember going shopping, for example — can be a sign of a progressive disorder, but not always.
Wisniewski said he becomes concerned when people don’t even recognize that they are forgetting things.
“They forgot that they went shopping and they’re unaware that they’ve forgotten,” he said.
Overall, neurologists tend to worry less about a patient’s ability to remember remote memories from many years ago and more troubled by an inability to recall more recent events. That’s because dementia first affects the part of the brain that’s responsible for short-term memories, as opposed to long-term memories, said Newhouse.
“What I’m more concerned about is, can you remember what happened yesterday? Or an hour ago?” Newhouse said.
While the conversation surrounding aging is often framed around a person’s diminishing memory or executive functioning, there are cognitive benefits that come with growing older, Selkoe said.
“There is a type of emotional intelligence and ability to handle many different kinds of experiences in life that come with greater longevity,” he said. “People can make decisions more carefully and more rationally.”
Akshay Syal, M.D.
Akshay Syal, M.D., is a medical fellow with the NBC News Health and Medical Unit.
Ghael Fobes
Ghael Fobes is an Associate White House Producer with the NBC News White House Unit in Washington, D.C.
5 Ways Mindfulness Rewires Your Brain and Improves Your Life

David Gyung/Shutterstock Life is busy. Parenting , work, hobbies, friends, problems, and pressure fill each day with more items on our to-do list than we can accomplish. Who has time for mindfulness meditation ? But as these pressures erode sleep, increase anxiety , turn into depression , and lead to inflammation, we might want to reconsider the benefits of a simple mindfulness practice. Why We Get Stuck
Being on autopilot and letting the default mode network of our brain dominate our thinking are two fundamental challenges that interfere with how we handle the pressures of life.
When we are on autopilot, we don’t pay attention to what we are thinking and how our thinking connects to our emotions and behavior. Instead, we react to life events and go from calm to irritated or anxious in just moments. When we are away from the pressures of our lives, the brain’s default mode network triggers rumination and constructs unhelpful thoughts about the past and the future.
Mindfulness helps us increase our awareness of our thoughts, feelings, physical sensations, and behaviors, but it also helps us have more control over how we respond to life pressures. Mindfulness changes the resting state of the brain to be less judgmental, fearful, and anxious, reducing the impact of the default mode network and creating a sense of well-being.
Here are five ways mindfulness helps rewire the brain, giving us better control over how we respond to stress, handle difficult emotions, manage pain, and adapt to change. 1. Mindfulness improves our brain chemistry.
Research suggests that regular mindfulness practices help the brain increase levels of GABA, which helps us stay calm; dopamine , the pleasure and reward neurotransmitter; and serotonin, which helps us experience positive emotions. 2. Mindfulness changes our fear and stress response.
When we take in sensory information about a possible threat, the amygdala is the first brain structure to process that information. The amygdala evaluates images and sounds; if it detects a threat, it passes on the information to the hippocampus, which activates the body to prepare for a threat. With regular mindfulness practice, the size of the amygdala shrinks . A smaller amygdala is correlated with a reduced fear response, increased calmness, better management of anxiety, and a feeling of well-being. 3. Mindfulness helps us stay connected to the present moment.
Falling and staying asleep is often a challenge when we experience stressful periods of life. Our mind races back and forth between our regrets about the past and worries about the future, keeping us awake. During the day, our busy minds distract us from being present with the people we love and the work we need to accomplish. Because of changes in the insula and cingulate cortex , mindfulness practices help harness our ability to shift and focus our attention on our bodily sensations and regulate the emotional responses associated with those physical sensations. 4. Mindfulness facilitates learning and memory.
The gray matter of the memory areas of the brain generally decreases with age, impacting memory processes, emotional regulation , and perspective-taking . As a result, our memory suffers as we get older, we become less flexible with change, and we find it difficult to appreciate the perspective of others. Mindfulness has been demonstrated to increase the size of the hippocampus , which leads to improved learning, memory, and stress management. 5. Mindfulness helps with brain healing and pain management.
Mindfulness practices greatly enhance neuroplasticity . Recovery from brain injury requires healing damaged areas of the brain and using other areas to recover lost functioning. Mindfulness can improve emotional regulation and mental fatigue and help regulate pain . ( Click here to learn more about how mindfulness helps pain management.) How To Get Started
If you are ready to try mindfulness, there are many learning options. Some will find it easier to follow along listening to instructions that guide your attention. If that is you, consider following a short, guided meditation using the body scan exercise .
For those who want to sit quietly and learn to increase their awareness through focused concentration , follow these steps with the “clouds in the sky” exercise: Sit comfortably, close your eyes, and direct your attention to your breath.
Notice the gentle movement of your stomach as you breathe.
As you breathe quietly, thoughts, emotions, and physical sensations will come and go like clouds passing in an open blue sky.
Be open and curious about what comes and goes from your awareness.
Try to suspend judgment and evaluation of what you experience.
Accept what you experience without wishing things to be different or trying to make them different.
Hold your thoughts, emotions, and physical sensations with compassion and kindness.
You will notice that even with much effort, your mind will still be busy. Have compassion for yourself as you notice where your mind wanders. Gently bring it back and focus your attention once again. In no time, you will soon see that your thoughts and emotions will come and go, just like the breaths you take from moment to moment. Start practicing five minutes twice a day and increase the length of your practice sessions week by week—it won’t be long before you look forward to each practice and notice the changes in how you handle the pressures of life.
Study links micro- and nanoplastics to Parkinson’s and dementia
Advertisement
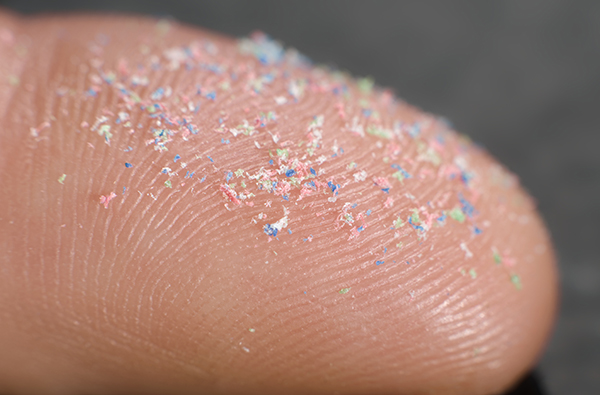
A study has found that microplastics and nanoplastics affect a specific protein found in the brain, causing changes associated with Parkinson’s disease and some types of dementia. Microplastics and nanoplastics
Microplastics and nanoplastics are two types of plastic waste that have become a major concern for environmental and human health.
Produced from the degradation of larger plastic items (such as bags, bottles, covers, car tires, fishing nets, packaging material and others), microplastic particles are larger than one micrometer but smaller than five millimeters in size. On the other hand, nanoplastics are very tiny particles that range from one to 100 nanometers in size.
Bits of microplastic and nanoplastics accumulate in organisms and contaminate soil and water – causing harm to ecosystems, humans and wildlife. These plastic wastes also act as carriers of chemical pollutants that pose health risks to both animals and humans when ingested or inhaled.
Primary microplastics are intentionally manufactured to be as small as possible (e.g., microbeads in cosmetics and personal care products), or as microfibers in textiles (e.g., polyamide, polyester and polypropylene).
Because of their extremely small size, nanoparticles eventually end up inside the body, penetrating cells and tissues and causing more harm to humans and animals compared to bigger-sized microplastics. (Related: MICROPLASTIC INVASION: Researchers find microplastics in human heart tissue .) Nanoplastics linked to Parkinson’s and some types of dementia
According to the Parkinson’s Foundation, nearly a million people in the U.S. are living with Parkinson’s disease, one of the most devastating neurological disorders characterized by the death of a specialist population of nerve cells that control movement.
“Parkinson’s disease has been called the fastest-growing neurological disorder in the world. Numerous studies suggested that environmental factors play a prominent role in increasing the risk of developing the disease but such factors have, for the most part, not been specifically identified,” said Dr. Andrew West, who directs the Duke Center for Neurodegeneration and Neurotherapeutic Research.
As per the Parkinson’s Foundation, almost one million Americans are afflicted with the disease and around 90,000 new cases are being diagnosed each year. Globally, more than 10 million people are suffering from it.
Researchers from the Duke University School of Medicine initially used different types of nanoplastic particles to facilitate biomarker assays for the diagnosis of Parkinson’s disease and dementia. (Related: Study: Microplastics accumulate in the brain and cause behavioral changes associated with dementia .)
Using three models – cultured neurons, a mouse model (genetically engineered to be predisposed to a condition similar to Parkinson’s) and test tube solutions – West and his team found that polystyrene nanoplastics interact with alpha-synuclein , a brain protein that plays an important role in nerve cell communication. Normally, alpha-synuclein is recycled within the nerve cells.
The study, published in the journal Science Advances , reported that the presence of polystyrene nanoplastics attracted unusually large clumps of alpha-synuclein. Of particular interest to the scientists were the tight chemical bonds formed between them.
The researchers also discovered that when the proteins clumped together and formed alpha-synuclein fibrils (aberrant forms of alpha-synuclein), the machinery in the nerve cells that handles waste disposal could not keep up with the waste. This finding suggests that nanoplastics affect the levels of alpha-synuclein in the brain by interfering with the natural cleaning process of neurons.
West and his team emphasized that these were early findings and no tests had been done in humans yet.
“While microplastic and nanoplastic contaminants are being closely evaluated for their potential impact in cancer and autoimmune diseases, the striking nature of the interactions we could observe in our models suggest a need for evaluating [the impact of] increasing nanoplastic contaminants on Parkinson’s disease and dementia risk and progression,” said West. Plastic pollution a new risk factor for dementia
The authors suggested that increasing micro- and nanoplastic pollution could represent a new risk factor for developing Parkinson’s and dementia. However, more research is needed to better understand how these plastics interact with the human brain and whether different types of plastics have different effects.
The authors also highlighted the importance of monitoring contamination levels with nanoplastics and limiting human exposure.
“If we knew the specific molecular nature of particularly bad nanoplastic actors, we could develop policies and technologies to make sure they don’t end up in our food and water,” said West.
“We also need to have a better idea of what lifetime exposures to different types of nanoplastics look like so that our models in the lab are more informative,” he added.
Watch the following video to learn about invisible plastic and Parkinson’s disease – the surprising link . This video is from the Daily Videos channel on Brighteon.com . More related stories:
Report reveals recycling plastic releases toxic “chemical cocktail into the environment .
Study: Plastic pollution in some lakes is WORSE than the most contaminated parts of the oceans .
Microplastics are everywhere, including New Zealand’s rainfall .
Sources include:
TheEpochTimes.com ThisVsThat.io Parkinson.org LetsTalkScience.ca Science.org MedicalNewsToday.com Brighteon.com
Steve Kirsch: CDC FORGOT to warn the public that COVID-19 vaccines cause DEMENTIA

Advertisement
Vaccine Safety Research Foundation founder Steve Kirsch recently found that the number of Wuhan coronavirus (COVID-19) vaccine recipients having dementia had increased 1,000 times. According to the World Health Organization (WHO), it is currently the seventh leading cause of death and one of the major causes of disability and dependency among older people globally.
The data is all out in the open but may have been covered up or agencies such as the Centers for Disease Control and Prevention (CDC) may have failed to inform the public. But Kirsch took the liberty to check and it took him just a few seconds to uncover the truth. From the graph on the National Vaccine Information Center website, he found 998 cases where the brain condition was symptomatic as against the types of vaccines from the Dec. 29, 2023 release of Vaccine Adverse Event Reporting System (VAERS) data. He further explained that the calculation is relative to the average vaccine and not against all vaccines in history combined. It would be important to note that many of these vaccines have far more doses than the coronavirus vaccine and if that is considered, the difference would be more extreme, Kirsch added.
“The results are self-explanatory: the COVID-19 vaccines cause dementia ,” Kirsch concluded in his Substack newsletter dated Jan. 30. “Anyone who tells you that ‘correlation isn’t causation’ should explain the actual cause of this if it wasn’t the COVID-19 vaccine.” He also said that no one would even want to go on a debate with him on this because nobody would want to talk about the truth. Worse, the mainstream media would not even cover and report this.
The independent investigator further reminded that people who want to get an immigration visa to the U.S. would be required to take the COVID-19 vaccine. “So you can get dementia too!” he added. And unlike other shots, no medical conditions would allow an individual to opt out of the SARS-CoV-2 vaccine. What is more stunning, he said, is that the said jabs are recommended especially to pregnant women. And this is despite nurse Michelle Gershman’s bombshell revelation that it can increase the rate of fetal demise by 50 times or more. Finally, he still recommended religious exemption to those who wished not to take the jabs. But almost no one gets approved as per observers.
Back in August last year, Kirsch also released a report that COVID-19 vaccines are linked to a 2,500 percent increased risk of early onset dementia . He spoke to a charge nurse at a rehabilitation and long-term elderly care facility who told him what she is now seeing in terms of the sheer number of new dementia cases cropping up all around her. Before the pandemic, the healthcare professional would rarely see anyone suddenly exhibit dementia-like behaviors including sudden onset hallucinations for no apparent reason. Just a year or two after the roll-out of vaccines, the nurse has seen early onset dementia symptoms appear nearly 50 times, which represents a 25-fold increase in the illness rate. (Related: COVID jabs linked to 2,500% increased risk of early onset dementia .) Drug manufacturers craft cures to injuries that their COVID-19 vaccines brought
At one point in the testimonials during the House Select Subcommittee on the Coronavirus Pandemic hearing earlier in January, Rep. Marjorie Taylor Greene (R-GA) raised a concern apart from the given and proven fact that the “shots” contained foreign spike proteins that harm the body systems and create blood clots. Controversial doctors Peter McCullough, Ryan Cole and Kirk Milhoan have cited several studies proving these are true but lamented how President Joe Biden’s government agencies ignored them. Another point is that the Big Pharma companies seem to have manufactured medications and vaccines that would “cure” the adverse reactions brought about by the COVID-19 shots.
Green even quoted Big Pharma: “‘Sell the disease and then sell the cure. And their friends in Congress, in turn, force Americans to pay for it. This is how Washington works in many cases.’ Is it fair to say then that these vaccine manufacturers created these vaccines with synthetic mRNA that has created heart disease, strokes, neurological problems and everything that you’ve talked about, do these same manufacturers sell the cures for the diseases that they’re creating?”
Cole, a board-certified anatomic and clinical pathologist, did not answer directly but said he finds it ironic that major drug manufacturer Pfizer just spent $40 billion on a cancer treatment company. According to reports, since the commencement of COVID-19 vaccines, there has been an unprecedented rise in the deaths of young people between 2021 and 2022 from rapidly metastasizing and terminal cancers , according to data from the U.K.’s Office for National Statistics. Also, Pfizer’s mRNA vaccine was found to be contaminated with cancer-causing DNA fragments.
Internist and cardiologist McCullough chimed in stating that following the roll-out of the mRNA vaccines, he has never prescribed so many blood thinners in his career. “This is extraordinary. All day long, I’m confronted with blood clots of different scenarios,” he said. The early treatment proponent for coronavirus also revealed how the prices are skyrocketing for medical procedures. Recently, he has been ordering more and more cardiac magnetic resonance images (MRIs) and electrocardiograms (ECG or EKG) and seeing recurrent visits to the emergency room, especially in those who are military servicemen.
Watch the full unedited coverage of the Congressional hearing on the injuries caused by COVID-19 vaccines below. VaccineInjuryNews.com has more stories on the adverse events of the coronavirus injections.
Sources for this article include:
WHO.int
KirschSubstack.com 1
KirschSubstack.com 2
Expose-News.com
How the “Little Brain” Fuels Motivation and Addiction

Key points
First-of-its-kind research shows how the cerebellum modulates dopamine release within the basal ganglia.
Motivation and addiction are both fueled by dopamine activation in the basal ganglia’s substantia nigra.
Too little dopamine causes Parkinson’s disease. Stimulating the cerebellum may be a new treatment option.
The cerebellum (“little brain”) is tucked underneath the basal ganglia; it sits in the back of the skull below the cerebrum. Source: CLIPAREA l Custom media/Shutterstock
Neuroscientists have unearthed a previously unknown dopamine -driven neural pathway between the cerebellum (Latin for “little brain”) and reward centers in the basal ganglia that appears to fuel both the vigor of motivation and the intensity of addiction . These findings ( Washburn et al., 2024 ) were published on January 25 in Nature Neuroscience . The Cerebellum and Basal Ganglia: Separate but Interconnected
We’ve known for decades that the cerebellum helps to control and coordinate voluntary movements. Fluidity and grace when playing sports or doing everyday things like driving a car rely on the cerebellum’s coordination capacities. Damage to the cerebellum can impair fluid movements and well-timed motor control, often resulting in noticeable discombobulation and jerkiness, as seen in people with cerebellar ataxia. The basal ganglia is a subcortical structure in the midbrain located above the cerebellum and below the cerebral cortex. Source: CLIPAREA l Custom media/Shutterstock
As a completely separate subcortical brain structure, the basal ganglia’s substantia nigra region has traditionally been viewed as the brain’s go-no-go reward center that’s turned “on” by dopamine and turned “off” by a lack thereof. When the substantia nigra is flooded with dopamine, it turbocharges reward-seeking behaviors that often drive addiction and cue-induced relapse . Notably, a lack of dopamine in the substantia nigra is a hallmark of Parkinson’s disease.
Until now, the cerebellum’s muscle-coordinating powers and the basal ganglia’s reward-seeking influence were viewed as separate entities that weren’t directly interconnected or intertwined.
The recent discovery of a direct dopaminergic pathway between these two subcortical brain structures is the first direct evidence that the cerebellum modulates dopamine levels in the basal ganglia, influencing reward processing, movement initiation, and motivational vigorousness. New Discovery: The Cerebellum Controls Dopamine Release
The latest (2024) research by Farzan Nadim and colleagues suggests, for the first time, that the cerebellum modulates the release of dopamine into the basal ganglia’s substantia nigra pars compacta (SNc), a reward processing center involved in habit formation , addiction, motivation, and neurodegenerative diseases that affect voluntary movement, such as Parkinson’s disease.
“We are exploring a direct communication between two major components of our brain’s movement system, which is absent from neuroscience textbooks. These systems are traditionally thought to function independently,” Nadim said in a news release . “This pathway is physiologically functional and potentially affects our behaviors every day.”
This study in mice used state-of-the-art optogenetic activation techniques to hack into monosynaptic bilateral projections from the cerebellum to the substantia nigra that the researchers identified as modulating the release of dopamine in ways that drive reward-seeking behaviors. Stimulating or Suppressing the Cerebellum Affects Motivation and Movement
When the scientists shut down this cerebellum>SNc pathway and blocked dopamine signaling from the cerebellum to the basal ganglia’s substantia nigra using optogenetics, motivation to perform voluntary movements necessary to obtain a reward evaporated.
Conversely, when this dopamine-producing pathway was stimulated, it increased the vigor of mice’s motivation to seek rewards. The cerebellum also seemed to attach a higher value to the reward in real-time, which led to mice intensely pursuing a potentially addictive substance and giving them the dopamine-fueled motivation to do so.
More research is needed. But someday, in humans, shutting down this cerebellum-rooted pathway with targeted medications might mitigate addiction. In terms of daily physical activity, finding drug-free, holistic ways to activate the cerebellum’s dopamine-producing pathway could increase people’s motivation to seek exercise, not avoid it.
Theoretically, stimulating the cerebellum with transcranial magnetic stimulation or other therapeutic techniques could jumpstart dopamine production in the substantia nigra in ways that might help people with Parkinson’s disease. Next Steps: Focus on Parkinson’s Disease Treatment Options
“This pathway seems very important to our vigor of movement and speed of cognitive processes,” Nadim says. “Parkinson’s patients not only suffer from suppression of movement but apathy in some cases. The cerebellum’s location at the back of the brain makes it a much easier target for novel therapeutic techniques.”
After establishing that the cerebellum can directly excite the substantia nigra’s dopamine neurons, the researchers’ next step is to explore how stimulating this pathway and jumpstarting dopamine activity in the basal ganglia might relieve Parkinson’s disease symptoms.
References
Samantha Washburn, Maritza Oñate, Junichi Yoshida, Jorge Vera, Ramakrishnan Bhuvanasundaram, Leila Khatami, Farzan Nadim & Kamran Khodakhah. “The Cerebellum Directly Modulates the Substantia Nigra Dopaminergic Activity.” Nature Neuroscience (First published: January 25, 2024) DOI: 10.1038/s41593-023-01560-9
Study finds brain mechanism that may explain how physical exercise improves mood
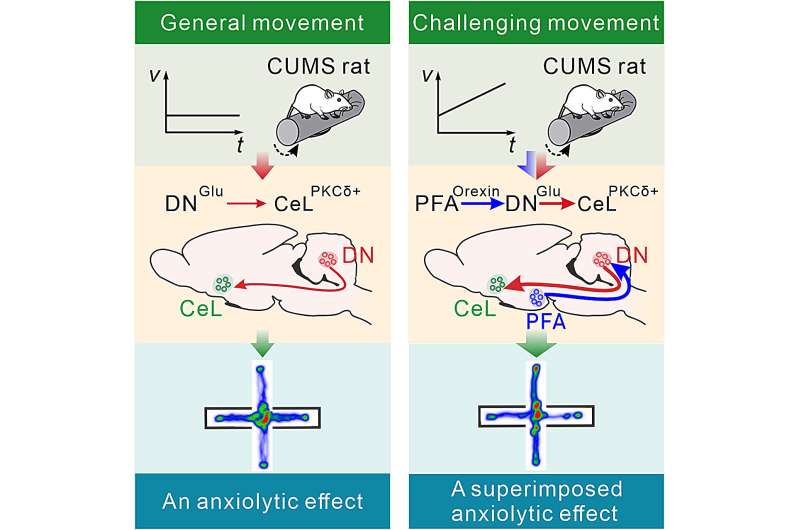
by Nanjing University School of Life Sciences Challenging movement can improve anxiety more effectively by recruiting the hypothalamic-cerebellar orexinergic circuit which more strongly activates the cerebello-amygdalar glutamatergic monosynaptic projections. Credit: Neuron (2024). DOI: 10.1016/j.neuron.2024.01.007 “Only exercise can remove all kinds of doubts,” Goethe said. Physical exercise is the lubricant between the body and the mind. Alleviation of anxiety by motor activity forms an integral part of our daily life; whether going for a walk to refresh our mind or running excessively in the park to recuperate from a stressful event, we are all well aware of the beneficial impact.
In fact, the plain view that exercise can prevent anxiety and depression has been supported by accumulating prospective cohort studies in recent years. Yet, apart from some general interactions between the periphery of our body and our central nervous system, it has remained unclear which mechanisms inside our brain underlie this process of motor-dependent anxiolysis.
In a recent study titled “A role for the cerebellum in motor-triggered alleviation of anxiety” published in the journal Neuron , Dr. Jing-Ning Zhu’s group from the School of Life Sciences at Nanjing University explores a hypothalamo-cerebello-amygdalar circuit that may mediate motor-dependent alleviation of anxiety. This three-neuron loop, in which the cerebellum takes center stage, bridges the motor system with the emotional system.
The cerebellum is the largest subcortical motor structure. The attention to the potential role of the cerebellum in higher functions, including emotion and cognition, next to that for sensorimotor coordination, has been increasing. It has been implicated in orchestrating and integrating somatic and non-somatic activities to generate an appropriate behavioral response to changes in external and internal environments.
However, little is known about whether there are direct neural connections between the cerebellum and the limbic system, which is responsible for emotional regulation. Notably, the study finds a trend of negative correlation between cerebello-amygdalar functional connectivity and the Hamilton Anxiety Rating Scale (HAMA) score in patients with bipolar disorder , suggesting an interaction between two brain regions that may be related to anxiety.
By employing the trans-monosynaptic retrograde rabies tracing and fluorescence micro-optical sectioning tomography (fMOST), the researchers map, for the first time, the long-range direct afferent projections from the cerebellar nuclear neurons to amygdala neurons at the mesoscopic scale in rodents, suggesting that the cerebello-amygdalar circuit appears well conserved among species.
Furthermore, using miniature fluorescence microscopy, they find amygdala neurons are activated while rats are running on a rotating rotarod, and among them, the majority also respond to optogenetic stimulation of the cerebellar nuclei, indicating that the cerebello-amygdalar projections carry exercise-dependent information.
Electrophysiological results show that the cerebello-amygdalar projections are monosynaptic glutamatergic and can not only excite but also evoke long-term potentiation in amygdala neurons, which may account for the persistent effect of exercise on mood. Opto-/chemo-genetic activation of cerebello-amygdalar projections significantly ameliorates anxiety, while chemogenetic suppression of the projections eliminates the anxiolytic effect of rotarod running.
So, what kind of motor paradigm can more effectively improve anxiety? Based on their previous findings that hypothalamic neuropeptide orexin not only helps to cope with motor challenges but also promotes stress resilience, the researchers find that challenging animals on an accelerated rather than a constant rotarod engages hypothalamic neurons that provide a superimposed anxiolytic effect via an orexinergic projection to the cerebellar nuclear neurons that activate the amygdala. Thus, the hypothalamo-cerebello-amygdalar loop may exert anxiolytic effects at two levels of intensity, operating like an engine with multiple transitions.
“The results advance our understanding of cerebellar nonmotor functions and the neural mechanisms underlying motor-emotional interaction and somatic-nonsomatic integration,” said Jing-Ning Zhu. “The findings may also shed light on developing more effective movement prescriptions for anxiety and mood disorders in general, such as high-intensity interval training (HIIT) or vigorous intermittent lifestyle physical activity (VILPA), and provide a novel strategy for both invasive and non-invasive forms of interventions targeting cerebellum to alleviate anxiety.”
Provided by Nanjing University School of Life Sciences
5 easy ways to start following the MIND diet for longevity and brain health

Health 5 easy ways to start following the MIND diet for longevity and brain health
Facebook Email Twitter LinkedIn Copy Link
Read in app The MIND diet focuses on eating patterns that protect your brain as you age, and you can get started with simple habits like adding more berries or greens to your meals. A simple, Mediterranean-style eating plan may be one of the best ways to protect your brain (and body) as you age , and experts say you can start with easy additions to your grocery list and meal routine.
The MIND diet — which stands for Mediterranean-DASH Intervention for Neurodegenerative Delay — incorporates elements of the notably healthy Mediterranean diet and heart-healthy DASH diet, along with foods linked to preventing cognitive decline as we age.
It’s been ranked one of the healthiest ways to eat , alongside the Mediterranean diet, and is a similarly non-restrictive, flexible eating plan. It was developed by a team of Harvard and Rush University researchers led by epidemiology professor Dr. Martha Clare Morris, who died in 2020.
Her daughter, Laura Morris, is a chef, personal trainer, who has carried on her work, co-authoring ” The Official MIND Diet .”
She told Business Insider that what separates it from other Mediterranean-style diets and similar health eating plans is that it offers more specific recommendations with 10 food groups to eat more of, which include leafy greens, other veggies, berries, olive oil, nuts and seeds, fish, chicken, whole grains, beans, and wine (in moderation).
The recommendations are based on research about which foods, nutrients, and eating patterns can help prevent health issues like dementia, and are good for overall longevity too, according to Morris.
The MIND diet focuses on helping you add more foods that benefit cognitive function, while gradually reducing foods linked to worse brain health, like red meat and sweets. What’s distinct is that you aren’t expected to cut out your favorite foods entirely, said Jennifer Ventrelle, a registered dietitian who co-authored the “The Official MIND Diet.”
“As a diet, people probably expect a strict set of rules but we’ve written it so the idea is to start as you are,” she told Business Insider.
Whether you’re new to healthy eating. or an established nutrition nerd, Ventrelle and Morris offer a week-to-week guide on how to follow the MIND diet without turning your life or kitchen upside down.
To get started, assess what you’re currently eating, add a few extra servings of specific foods each week, and build up gradually to avoid common beginner mistakes like doing too much too soon, or becoming restrictive with your eating. Start by tracking what you’re already eating
The first step of starting the MIND diet doesn’t even require a trip to the grocery. Before you jump in, Ventrelle and Morris recommend keeping a log of what you eat , so you can assess how your typical habits compare to the recommendations.
From there, you can start reducing a little at a time, such as cutting out a few servings per week of processed or fried food, and gradually adding more recommended foods.
“You don’t know what to change if you don’t know what the problem is,” Morris said. Add brain-healthy foods like berries and greens to what you’re already eating
One distinct feature of the MIND diet is that instead of banning foods or focusing on what you can’t eat, it emphasizes adding foods to improve your health (and even lose weight , if that’s a goal).
That means you can incorporate the MIND diet into your current habits by building on meals and snacks you typically enjoy, like adding a handful of berries to your morning yogurt or blending some greens into a shake .
“It’s not meant to say you can only eat the 10 foods on the list and stay away from the foods on the list to limit,” Ventrelle said. Focus on a few servings of healthy foods per week
While the MIND diet is relatively simple, trying to change everything at once can be overwhelming. Ventrelle said she still uses simple tools like the MIND diet tracker at home to help her improve over time. Begin with a small shift in a single category at a time, such as eating fewer servings of red meat or more helpings of berries. That way, you can build progress over time.
“Pick one or two things to change, and find very specific and measurable ways to change. Give yourself some grace,” Morris said. Don’t wait — right now is the best time to start the MIND diet
The MIND diet can be beneficial at just about any age, since brain changes can begin as early as your 30s, according to Morris. And while the diet can’t reverse Alzheimer’s disease, evidence suggests it may be protective in older adults, too.
“There is no right time. It’s never too early or too late,” she said. Don’t worry about being perfect
Before you panic about checking off every box on the MIND diet guide, know that it isn’t an all-or-nothing endeavor. Research suggests the benefits of the MIND diet can happen on a spectrum so making some small changes can protect your brain even if you don’t manage to get exactly the right servings of every food each week.
“You can absolutely still follow it if it’s not perfect. The idea is to improve where you are,” Morris said.
Sign up for notifications from Insider! Stay up to date with what you want to know.
Subscribe to push notifications
The Science of Sleep: Understanding What Happens When You Sleep

man in sleep study Sleep accounts for one-quarter to one-third of the human lifespan. But what exactly happens when you sleep? Before the 1950s, most people believed sleep was a passive activity during which the body and brain were dormant. “But it turns out that sleep is a period during which the brain is engaged in a number of activities necessary to life—which are closely linked to quality of life,” says Johns Hopkins sleep expert and neurologist Mark Wu, M.D., Ph.D. Researchers like Wu are spending many of their waking hours trying to learn more about these processes and how they affect mental and physical health. Here is a glimpse into the powerful (often surprising) findings of sleep researchers—and what they’re still trying to discover about the science of sleep. All Sleep Is Not the Same
Throughout your time asleep, your brain will cycle repeatedly through two different types of sleep: REM (rapid-eye movement) sleep and non-REM sleep.
The first part of the cycle is non-REM sleep , which is composed of four stages. The first stage comes between being awake and falling asleep. The second is light sleep, when heart rate and breathing regulate and body temperature drops. The third and fourth stages are deep sleep. Though REM sleep was previously believed to be the most important sleep phase for learning and memory, newer data suggests that non-REM sleep is more important for these tasks, as well as being the more restful and restorative phase of sleep.
As you cycle into REM sleep , the eyes move rapidly behind closed lids, and brain waves are similar to those during wakefulness. Breath rate increases and the body becomes temporarily paralyzed as we dream.
The cycle then repeats itself, but with each cycle you spend less time in the deeper stages three and four of sleep and more time in REM sleep. On a typical night, you’ll cycle through four or five times. An image of a fruit fly’s brain, with the sleep-controlling neurons highlighted in green. Your Body’s Built-In Sleep Controls
According to Wu, there are two main processes that regulate sleep: circadian rhythms and sleep drive .
Circadian rhythms are controlled by a biological clock located in the brain. One key function of this clock is responding to light cues, ramping up production of the hormone melatonin at night, then switching it off when it senses light. People with total blindness often have trouble sleeping because they are unable to detect and respond to these light cues.
Sleep drive also plays a key role: Your body craves sleep, much like it hungers for food. Throughout the day, your desire for sleep builds, and when it reaches a certain point, you need to sleep. A major difference between sleep and hunger: Your body can’t force you to eat when you’re hungry, but when you’re tired, it can put you to sleep, even if you’re in a meeting or behind the wheel of a car. When you’re exhausted, your body is even able to engage in microsleep episodes of one or two seconds while your eyes are open. Napping for more than 30 minutes later in the day can throw off your night’s sleep by decreasing your body’s sleep drive. Why You Need Sleep
If you have ever felt foggy after a poor night’s sleep, it won’t surprise you that sleep significantly impacts brain function. First, a healthy amount of sleep is vital for “brain plasticity,” or the brain’s ability to adapt to input. If we sleep too little, we become unable to process what we’ve learned during the day and we have more trouble remembering it in the future. Researchers also believe that sleep may promote the removal of waste products from brain cells—something that seems to occur less efficiently when the brain is awake.
Sleep is vital to the rest of the body too. When people don’t get enough sleep, their health risks rise. Symptoms of depression, seizures, high blood pressure and migraines worsen. Immunity is compromised, increasing the likelihood of illness and infection. Sleep also plays a role in metabolism: Even one night of missed sleep can create a prediabetic state in an otherwise healthy person. “There are many important connections between health and sleep,” says Wu.
New Tech Could Record Deep-Brain Activity From Surface
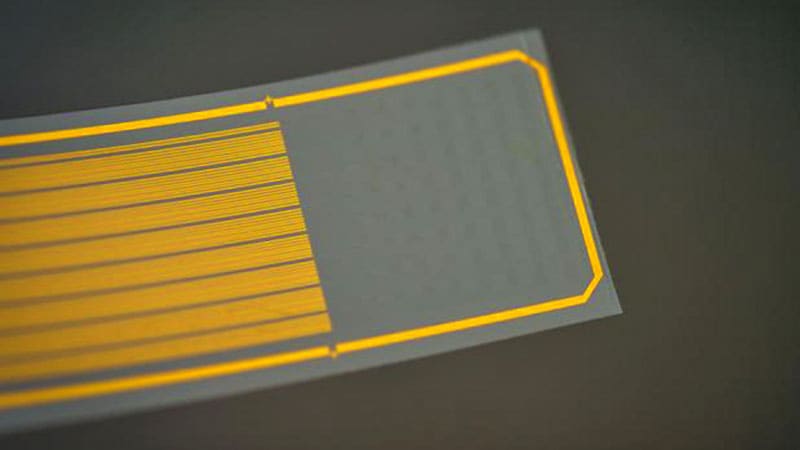
0
Modern technology for recording deep-brain activity involves sharp metal electrodes that penetrate the tissue, causing damage that can compromise the signal and limiting how often they can be used.
A rapidly growing area in materials science and engineering is to fix the problem by designing electrodes that are softer, smaller, and flexible — safer for use inside the delicate tissues of the brain. Just last week, researchers from the University of California, San Diego, reported the development of a thin, flexible electrode that can be inserted deep within the brain and communicate with sensors on the surface.
But what if you could record detailed deep-brain activity without piercing the brain?
A team of researchers (as it happens, also from UC San Diego) have developed a thin, flexible implant that “resides on the brain’s surface” and “can infer neural activity from deeper layers,” said Duygu Kuzum, PhD , a professor of electrical and computer engineering, who led the research.
By combining electrical and optical imaging methods, and artificial intelligence, the researchers used the device — a polymer strip packed with graphene electrodes — to predict deep calcium activity from surface signals, according to a proof-of-concept study published this month in Nature Nanotechnology .
“Almost everything we know about how neurons behave in living brains comes from data collected with either electrophysiology or two-photon imaging,” said neuroscientist Joshua H. Siegle, PhD , of the Allen Institute for Neural Dynamics in Seattle , who not involved in the study. ” Until now, these two methods have rarely been used simultaneously.”
The technology, which has been tested in mice, could help advance our knowledge of how the brain works and may lead to new minimally invasive treatments for neurologic disorders. Multimodal Neurotech: The Power of 2-in-1
Electrical and optical methods for recording brain activity have been crucial in advancing neurophysiologic science, but each technique has its limits. Electrical recordings provide high “temporal resolution”; they reveal when activation is happening, but not really where. Optical imaging, on the other hand, offers high “spatial resolution,” showing which area of the brain is lighting up, but its measurements may not correspond with the activity’s timing.
Research over the past decade has explored how to combine and harness the strengths of both methods. One potential solution is to use electrodes made of transparent materials such as graphene, allowing a clear field of view for a microscope during imaging. Recently, University of Pennsylvania scientists used graphene electrodes to illuminate the neural dynamics of seizures .
But there are challenges. If graphene electrodes are very small — in this case, 20 µm in diameter — they become more resistant to the flow of electricity. Kuzum and colleagues addressed this by adding tiny platinum particles to improve electrical conductivity. Long graphene wires connect electrodes to the circuit board, but defects in graphene can interrupt the signal, so they made each wire with two layers; any defects in one wire could be hidden by the other.
By combining the two methods (microelectrode arrays and two-photon imaging), the researchers could see both when brain activity was happening and where, including in deeper layers. They discovered a correlation between electrical responses on the surface and cellular calcium activity deeper down. The team used these data to create a neural network (a type of artificial intelligence that learns to recognize patterns) that predicts deep calcium activity from surface-level readings.
The tech could help scientists study brain activity “in a way not possible with current single-function tools,” said Luyao Lu, PhD , professor of biomedical engineering at George Washington University in Washington, DC, who was not involved in the study. It could shed light on interactions between vascular and electrical activity, or explain how place cells (neurons in the hippocampus) are so efficient at creating spatial memory.
It could also pave the way for minimally invasive neural prosthetics or targeted treatments for neurologic disorders, the researchers say. Implanting the device would be a “straightforward process” similar to placing electrocorticography grids in patients with epilepsy , said Kuzum.
But first, the team plans to do more studies in animal models before testing the tech in clinical settings, Kuzum added.
You must remember this: VT discovery may lead to keeping good memories, removing bad ones
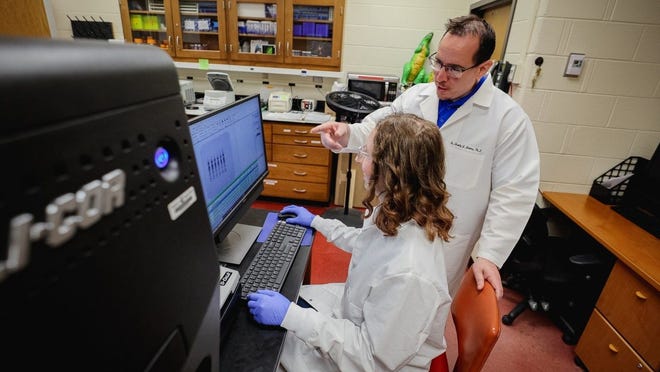
A protein in the brain may pave the way for targeted therapeutic interventions to enhance memory or alleviate negative memories.
Virginia Tech researchers discovered a new function for a common protein in the brain — a development that sheds new light on the mysteries of the mind and holds promising implications for the treatment of memory loss and post-traumatic stress disorder, according to a press release.
The protein normally performs necessary housekeeping in the brain’s hippocampus by working as part of a larger protein complex called the proteasome to destroy other proteins.
But researchers in the College of Agriculture and Life Sciences’ School of Animal Sciences recently noticed this protein, called RPT6, behaving in a previously undetected way. Research scientist Kayla Farrell and Associate Professor Tim Jarome in the School of Animal Sciences are part of a Virginia Tech research team that discovered a new function for a common protein in the brain. “We found that RPT6 is capable of this completely different function where it can bind to DNA and increase the expression of other genes or proteins during memory formation,” said Tim Jarome, associate professor of neurobiology. “This indicates that RPT6 plays a unique dual role in memory formation, both inside and outside the proteasome complex.”
The discovery, published this month in the Journal of Neuroscience, opens up new avenues for exploration of how RPT6 functions in the brain and how it could be manipulated to improve memory and alleviate memory disorders such as Alzheimer’s disease and post-traumatic stress disorder (PTSD), the release said.
The project was led by research scientist Kayla Farrell, who received her Ph.D. from the School of Animal Sciences in December. Farrell previously headed a study identifying a protein that could lead to better therapeutic treatment for women with PTSD.
Gene expression is critical to memory formation. It helps to build the neural networks needed to form and strengthen memories. Researchers don’t yet understand why RPT6 has this dual function or how it is helping to control the cells that are recruited to form a memory.
“There has to be something else that’s working with it to regulate gene expression,” Jarome said. “We are trying to understand now how it’s doing that.”
Ultimately, the discovery will be helpful to the ongoing research in Jarome’s lab, which focuses on understanding and treating memory disorders such as Alzheimer’s, dementia and PTSD, the release said.
“This discovery is leading us somewhere new in unraveling the complexities of the brain and how we learn and store memories,” Jarome said. “We hope that this will help to inform new directions into understanding how gene expression is controlled during memory. In the long-term, this could lead to potential therapeutic targets for controlling and improving memory or treating maladaptive memories.” Key findings
Dual function of RPT6: RPT6, a protein found in every cell, was previously known for its role within the proteasome complex. The study reveals that during memory formation, RPT6 can also bind to DNA and regulate gene expression, presenting a unique dual functionality.
Implications for memory manipulation: Understanding the dual role of RPT6 provides insights into the complex processes of memory formation. This knowledge could pave the way for targeted therapeutic interventions to enhance memory or alleviate negative memories associated with conditions such as PTSD.
Significance for future research: The study marks a crucial step in unraveling the complexities of the brain and gene expression control during memory formation. Researchers anticipate that further investigation into RPT6’s mechanisms will inform new directions for understanding memory at the molecular level.