Nature Knows and Psionic Success
God provides
Study finds daily fiber supplement improves older adults’ brain function in just 12 weeks

Credit: Pixabay/CC0 Public Domain A daily fiber supplement improved brain function in people over 60 in just 12 weeks. The study, published recently in Nature Communications by researchers from the School of Life Course & Population Sciences showed that this simple and cheap addition to diet can improve performance in memory tests associated with early signs of Alzheimer’s disease.
However, the prebiotic supplements inulin and FOS were found to have no effect on muscle strength over this period.
“We are excited to see these changes in just 12 weeks. This holds huge promise for enhancing brain health and memory in our aging population. Unlocking the secrets of the gut-brain axis could offer new approaches for living more healthily for longer,” says first author Dr. Mary Ni Lochlainn from the Department of Twin Research.
As populations age globally, the prevalence of age-related conditions such as cognitive decline and muscle loss is on the rise. Researchers at TwinsUK, the U.K.’s largest adult twin registry based at King’s College London, sought to understand how targeting the microbiota, the diverse community of microorganisms residing in our intestines, using two cheap, commercially available plant fiber supplements inulin and FOS, could impact both muscle health and brain function .
Researchers assigned 36 twin pairs—72 individuals—over 60 years old to receive either a placebo or the supplement every day for 12 weeks. Neither the analysis team, nor the participants knew which they received until the analysis was complete (double-blind). Alongside this, all study participants did resistance exercises and ate a protein supplement which was aimed at improving muscle function.
Researchers monitored participants remotely via video, online questionnaires and cognitive tests. They found the fiber supplement led to significant changes in the participants’ gut microbiome composition, particularly an increase in the numbers of beneficial bacteria such as Bifidobacterium.
While there was no significant difference in muscle strength between the groups, the group receiving the fiber supplement performed better in tests assessing brain function, including the Paired Associates Learning test which is an early marker for Alzheimer’s disease, together with tests of reaction time and processing speed. These measures are important for daily living—for example reacting to traffic or stopping a simple trip-up turning into a fall.
“These plant fibers, which are cheap and available over the counter, could benefit a wide group of people in these cash-strapped times. They are safe and acceptable too. Our next task is to see whether these effects are sustained over longer periods and in larger groups of people,” says senior author Professor Claire Steves, professor of aging and health.
Another novel aspect of the study was its remote design which demonstrated the feasibility of conducting trials in older adults without the need for extensive travel or hospital visits, which could be delivered in many settings globally. Challenges such as digital literacy and access to the necessary technology were acknowledged and will be addressed in future larger scale projects with the aim to enhance the quality of life for aging populations worldwide.
More information: Mary Ni Lochlainn et al, Effect of gut microbiome modulation on muscle function and cognition: the PROMOTe randomised controlled trial, Nature Communications (2024). DOI: 10.1038/s41467-024-46116-y
Provided by King’s College London
A noninvasive treatment for ‘chemo brain’
Patients undergoing chemotherapy often experience cognitive effects such as memory impairment and difficulty concentrating — a condition commonly known as “chemo brain.”
MIT researchers have now shown that a noninvasive treatment that stimulates gamma frequency brain waves may hold promise for treating chemo brain. In a study of mice, they found that daily exposure to light and sound with a frequency of 40 hertz protected brain cells from chemotherapy-induced damage. The treatment also helped to prevent memory loss and impairment of other cognitive functions.
This treatment, which was originally developed as a way to treat Alzheimer’s disease, appears to have widespread effects that could help with a variety of neurological disorders, the researchers say.
“The treatment can reduce DNA damage, reduce inflammation, and increase the number of oligodendrocytes, which are the cells that produce myelin surrounding the axons,” says Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory and the Picower Professor in the MIT Department of Brain and Cognitive Sciences. “We also found that this treatment improved learning and memory, and enhanced executive function in the animals.”
Tsai is the senior author of the new study, which appears today in Science Translational Medicine . The paper’s lead author is TaeHyun Kim, an MIT postdoc.
Protective brain waves
Several years ago, Tsai and her colleagues began exploring the use of light flickering at 40 hertz (cycles per second) as a way to improve the cognitive symptoms of Alzheimer’s disease. Previous work had suggested that Alzheimer’s patients have impaired gamma oscillations — brain waves that range from 25 to 80 hertz (cycles per second) and are believed to contribute to brain functions such as attention, perception, and memory.
Tsai’s studies in mice have found that exposure to light flickering at 40 hertz or sounds with a pitch of 40 hertz can stimulate gamma waves in the brain, which has many protective effects, including preventing the formation of amyloid beta plaques. Using light and sound together provides even more significant protection. The treatment also appears promising in humans: Phase 1 clinical trials in people with early-stage Alzheimer’s disease have found the treatment is safe and does offer some neurological and behavioral benefits.
In the new study, the researchers set out to see whether this treatment could also counteract the cognitive effects of chemotherapy treatment. Research has shown that these drugs can induce inflammation in the brain, as well as other detrimental effects such as loss of white matter — the networks of nerve fibers that help different parts of the brain communicate with each other. Chemotherapy drugs also promote loss of myelin, the protective fatty coating that allows neurons to propagate electrical signals. Many of these effects are also seen in the brains of people with Alzheimer’s.
“Chemo brain caught our attention because it is extremely common, and there is quite a lot of research on what the brain is like following chemotherapy treatment,” Tsai says. “From our previous work, we know that this gamma sensory stimulation has anti-inflammatory effects, so we decided to use the chemo brain model to test whether sensory gamma stimulation can be beneficial.”
As an experimental model, the researchers used mice that were given cisplatin, a chemotherapy drug often used to treat testicular, ovarian, and other cancers. The mice were given cisplatin for five days, then taken off of it for five days, then on again for five days. One group received chemotherapy only, while another group was also given 40-hertz light and sound therapy every day.
After three weeks, mice that received cisplatin but not gamma therapy showed many of the expected effects of chemotherapy: brain volume shrinkage, DNA damage, demyelination, and inflammation. These mice also had reduced populations of oligodendrocytes, the brain cells responsible for producing myelin.
However, mice that received gamma therapy along with cisplatin treatment showed significant reductions in all of those symptoms. The gamma therapy also had beneficial effects on behavior: Mice that received the therapy performed much better on tests designed to measure memory and executive function.
“A fundamental mechanism”
Using single-cell RNA sequencing, the researchers analyzed the gene expression changes that occurred in mice that received the gamma treatment. They found that in those mice, inflammation-linked genes and genes that trigger cell death were suppressed, especially in oligodendrocytes, the cells responsible for producing myelin.
In mice that received gamma treatment along with cisplatin, some of the beneficial effects could still be seen up to four months later. However, the gamma treatment was much less effective if it was started three months after the chemotherapy ended.
The researchers also showed that the gamma treatment improved the signs of chemo brain in mice that received a different chemotherapy drug, methotrexate, which is used to treat breast, lung, and other types of cancer.
“I think this is a very fundamental mechanism to improve myelination and to promote the integrity of oligodendrocytes. It seems that it’s not specific to the agent that induces demyelination, be it chemotherapy or another source of demyelination,” Tsai says.
Because of its widespread effects, Tsai’s lab is also testing gamma treatment in mouse models of other neurological diseases, including Parkinson’s disease and multiple sclerosis. Cognito Therapeutics, a company founded by Tsai and MIT Professor Edward Boyden, has finished a phase 2 trial of gamma therapy in Alzheimer’s patients, and plans to begin a phase 3 trial this year.
“My lab’s major focus now, in terms of clinical application, is Alzheimer’s; but hopefully we can test this approach for a few other indications, too,” Tsai says.
The research was funded by the JPB Foundation, the Ko Hahn Seed Fund, and the National Institutes of Health.
Does intermittent fasting have benefits for our brain?

Intermittent fasting has become a popular dietary approach to help people lose or manage their weight . It has also been promoted as a way to reset metabolism, control chronic disease, slow ageing and improve overall health .
Meanwhile, some research suggests intermittent fasting may offer a different way for the brain to access energy and provide protection against neurodegenerative diseases like Alzheimer’s disease .
This is not a new idea – the ancient Greeks believed fasting enhanced thinking . But what does the modern-day evidence say?
Read more: I want to eat healthily. So why do I crave sugar, salt and carbs? First, what is intermittent fasting?
Our diets – including calories consumed, macronutrient composition (the ratios of fats, protein and carbohydrates we eat) and when meals are consumed – are factors in our lifestyle we can change. People do this for cultural reasons, desired weight loss or potential health gains.
Intermittent fasting consists of short periods of calorie (energy) restriction where food intake is limited for 12 to 48 hours (usually 12 to 16 hours per day), followed by periods of normal food intake. The intermittent component means a re-occurrence of the pattern rather than a “one off” fast.
Food deprivation beyond 24 hours typically constitutes starvation. This is distinct from fasting due to its specific and potentially harmful biochemical alterations and nutrient deficiencies if continued for long periods. 4 ways fasting works and how it might affect the brain
The brain accounts for about 20% of the body’s energy consumption .
Here are four ways intermittent fasting can act on the body which could help explain its potential effects on the brain.
1. Ketosis
The goal of many intermittent fasting routines is to flip a “ metabolic switch ” to go from burning predominately carbohydrates to burning fat. This is called ketosis and typically occurs after 12–16 hours of fasting, when liver and glycogen stores are depleted. Ketones – chemicals produced by this metabolic process – become the preferred energy source for the brain.
Due to this being a slower metabolic process to produce energy and potential for lowering blood sugar levels, ketosis can cause symptoms of hunger, fatigue, nausea, low mood , irritability, constipation, headaches, and brain “fog”.
At the same time, as glucose metabolism in the brain declines with ageing, studies have shown ketones could provide an alternative energy source to preserve brain function and prevent age-related neurodegeneration disorders and cognitive decline .
Consistent with this, increasing ketones through supplementation or diet has been shown to improve cognition in adults with mild cognitive decline and those at risk of Alzheimer’s disease respectively.
Read more: Does it matter what time of day I eat? And can intermittent fasting improve my health? Here’s what the science says
2. Circadian syncing
Eating at times that don’t match our body’s natural daily rhythms can disrupt how our organs work. Studies in shift workers have suggested this might also make us more prone to chronic disease .
Time-restricted eating is when you eat your meals within a six to ten-hour window during the day when you’re most active. Time-restricted eating causes changes in expression of genes in tissue and helps the body during rest and activity.
A 2021 study of 883 adults in Italy indicated those who restricted their food intake to ten hours a day were less likely to have cognitive impairment compared to those eating without time restrictions. Matching your eating to the active parts of your day may have brain benefits. 3. Mitochondria
Intermittent fasting may provide brain protection through improving mitochondrial function, metabolism and reducing oxidants.
Mitochondria’s main role is to produce energy and they are crucial to brain health. Many age-related diseases are closely related to an energy supply and demand imbalance, likely attributed to mitochondrial dysfunction during ageing .
Rodent studies suggest alternate day fasting or reducing calories by up to 40% might protect or improve brain mitochondrial function . But not all studies support this theory.
4. The gut-brain axis
The gut and the brain communicate with each other via the body’s nervous systems. The brain can influence how the gut feels (think about how you get “butterflies” in your tummy when nervous) and the gut can affect mood, cognition and mental health.
In mice, intermittent fasting has shown promise for improving brain health by increasing survival and formation of neurons (nerve cells) in the hippocampus brain region, which is involved in memory, learning and emotion. What we eat can affect our brain, and vice versa. There’s no clear evidence on the effects of intermittent fasting on cognition in healthy adults. However one 2022 study interviewed 411 older adults and found lower meal frequency (less than three meals a day) was associated with reduced evidence of Alzheimer’s disease on brain imaging.
Some research has suggested calorie restriction may have a protective effect against Alzheimer’s disease by reducing oxidative stress and inflammation and promoting vascular health.When we look at the effects of overall energy restriction (rather than intermittent fasting specifically) the evidence is mixed. Among people with mild cognitive impairment, one study showed cognitive improvement when participants followed a calorie restricted diet for 12 months.Another study found a 25% calorie restriction was associated with slightly improved working memory in healthy adults. But a recent study , which looked at the impact of calorie restriction on spatial working memory, found no significant effect. Read more: Yes, intermittent fasting can boost your health, but how and when to restrict food consumption is crucial Bottom line Studies in mice support a role for intermittent fasting in improving brain health and ageing, but few studies in humans exist, and the evidence we have is mixed.Rapid weight loss associated with calorie restriction and intermittent fasting can lead to nutrient deficiencies, muscle loss, and decreased immune function, particularly in older adults whose nutritional needs may be higher.Further, prolonged fasting or severe calorie restriction may pose risks such as fatigue, dizziness, and electrolyte imbalances, which could exacerbate existing health conditions.If you’re considering intermittent fasting , it’s best to seek advice from a health […]
Lithium: The little-known element that can protect people from brainwashing by global elites, says researcher, author and medical doctor

For experts such as Dr. Michael Nehls, a world-renowned author, medical doctor and post-doctoral molecular geneticist, the globalist anti-human agenda is being rolled out via a warfare inside human brains – hijacking cognitively to influence and disrupt both the mental and physical immune systems.
But there is an essential trace element that could inhibit any disruption to the optimal functioning of the human brain, such as brain fog, Wuhan coronavirus (COVID-19) post-vaccination syndrome, chronic fatigue syndrome, depression, Alzheimer’s disease and even “globalists’ indoctrination” agenda: lithium.
“The natural inhibitor is lithium, which is the only substance at low molecular levels. One milligram per day is sufficient to actually stop the Alzheimer’s progression and other disruptions to brain functions,” Nehls told “Health Ranger Report” host Mike Adams during a sit-down interview at the Brighteon studio. He added that the element can also be taken as a supplement .
“Lithium was shown to activate the process of autophagy and microautophagy,” he stated. Autophagy is the body’s process of reusing old and damaged cell parts while microautophagy serves diverse biological functions, including protein quality control. “It was actually proposed in a paper… that it can even get rid of the microbe of the spike protein in the brain.”
In his Substack newsletter, Nehls further explained that microdosing lithium can reduce the risk of entering a life-threatening cycle. Said cycle is the long-term dysfunction of the hippocampus, a complex brain structure embedded deep into the temporal lobe that plays a major role in learning and memory, leads to reduced psychological resilience, which triggers an excessive and chronic stress response, which in turn over activates the brain’s immune system and leads to an increased and particularly persistent release of pro-inflammatory messengers.
“A slightly higher dosage even offers the legitimate hope of breaking an existing cycle. But although there is ample scientific evidence that lithium, in addition to its well-known therapeutic benefits, is also an essential trace element, it is not yet recognized as such and, for example, cannot be marketed as a dietary supplement in most European Union member states,” Nehls pointed out in the article. (Related: Study: Supplementing with vitamin D helps prevent cancer, especially if it’s taken more frequently .)
Although microdosed lithium is available in the United States as an over-the-counter supplement, Nehls pointed out that its perceived non-essential status “and the misperceived risk of side effects” inhibits its growth in popularity as a natural preventative measure against chronic inflammation.
The geneticist also mentioned that 7Up, an American brand of lemon-lime-flavored carbonated drink, got its name from lithium because it “used to contain” the element. The number seven is the molecular mass of lithium and they used the word “up” because it claims to pick up the mood of the person drinking the soda. However, the manufacturers would not admit this as they were no longer allowed to use the element. They claim that “lithium is not good for technocratic narrative.”
“Does this also explain why lithium is sometimes prescribed to people for depression or mental health?” Adams further asked. “It is almost without side effects for the cause. The side effects only come if you go into much higher doses like with bipolar disorders. It can shut down mood alterations by giving high doses,” the doctor explained. Global elites control governments around the world
Elsewhere in the show, Adams brought up the new law implemented in France, wherein any person who dares to openly criticize mRNA vaccines will be liable to fines and imprisonment. Critics call it the “Pfizer law.” It calls for fines of up to 45,000 euros and possibly three years in prison for debunking an approved medical treatment, the Epoch Times reported.
If it can happen in France, it can happen throughout Europe, then the Commonwealth, and then the United States, Brownstone Institute founder Jeffrey Tucker warned in the said article. “It is global. The elites that have seized control of our governments coordinate across borders. That’s why it is hugely important to pay attention to what’s going on across the pond.”
“It’s fortunate when I’m flying home, we are not landing in France and we are directly jumping over it,” said Nehls, who hails from France’s neighboring country Germany.
We are building the infrastructure of human freedom and empowering people to be informed, healthy and aware. Support us at HealthRangerStore.com and read about our “human freedom infrastructure” mission at this article link .
Watch the full episode of the ” Health Ranger Report ” with Mike Adams featuring Michael Nehls below.
This video is from the Health Ranger Report channel on Brighteon.com . More related stories:
Scientific literature shows chlorophyll-rich chlorella to be among the most effective nutritional supplements for dioxin DETOX .
Study: Vitamin D supplementation found to reduce the risk of heart attack .
Study: Multivitamin supplements can help improve memory . Sources include:
Brighteon.com
MichaelNehls.Substack.com
TheEpochTimes.com Take Action:
Support Natural News by linking to this article from your website.
Permalink to this article:
Copy
Embed article link:
CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
Study finds direct correlation between increased screen time for toddlers and delays in language development

A recent study conducted by the Telethon Kids Institute in Australia has found a direct correlation between increased screen time for toddlers and delays in their language development .
The study, which spanned two-and-a-half years and involved monitoring 220 Australian families, uncovered alarming insights into the potential impact of technology on the crucial early years of a child’s linguistic growth.
The families, who had toddlers aged 18 to 36, had their kids wear a device capturing 16 hours of audio daily in their homes, leading to over 7,000 hours worth of recordings. Families involved in the study were unaware that screen time would be measured during recording to ensure a more realistic view of young children’s screen exposure. (Related: Screen time linked to developmental delays in young children .)
According to the results, published in JAMA Pediatrics , toddlers who are 18 to 36 months of age spend approximately three hours a day on screens, which, in turn, results in a significant decline in their language skills.
The study found that at 36 months, there is a concerning decrease of 6.6 adult words for each additional minute of screen time. This cumulative effect amounted to a loss of 1,139 adult words, 843 vocalizations and 194 conversations per day.
Mary Brushe, senior researcher for the study, explained the importance of early interaction for language development. She claimed that screen time disrupts the necessary amount of talking and interaction children require.
“Our findings support the notion of ‘technoference’ as a real issue for Australian families , whereby young children’s exposure to screen time is interfering with opportunities to talk and interact in their home environment,” said Brushe. “Because we haven’t been able to capture parents’ silent screen-related activities, such as reading emails, texting, or quietly scrolling through websites or social media. The devices only picked up noise associated with screen time – for example, TV shows, videos or games. This meant we ended up with a more realistic view of young children’s screen exposure because parents were not subconsciously altering their normal habits.”
Furthermore, psychology lecturer Rachael Sharman at the University of the Sunshine Coast in Queensland reveals a link between increased screen time and social skill problems at younger ages. She explained that brain imaging studies suggested that increased screen time is associated with reduced white matter tracts in the brain, which is crucial for the development of language and cognitive abilities.
“Spending a great deal of time in the outdoors is associated with higher grey matter in regions associated with working memory and attention,” she said. Parents know the adverse effects of screen time, but some have no choice but to allow it
According to the Australian Institute of Family Studies , parents consider excessive screen time and its adverse effects to be the foremost health concern for their children.
For instance, one parent, deeply concerned about the potential harm, shared on the social platform Reddit that their three-year-old daughter is strictly prohibited from using any tablet or phone under any circumstances. The parent, working in product design, discussed their awareness of the problems these apps cause for adults, let alone children.
“I wouldn’t judge those that allow their kids to; I know how tough it is to find a break, but I’ve been strict for a reason. I work in product design and know a lot of the problems these apps cause adults, never mind children. We are learning more and more about the damage caused, and it genuinely frightens me,” the parent wrote.
However, some parents, despite reservations, still find themselves resorting to using screens as a temporary solution to juggle daily responsibilities.
“We have a 14-month-old and only use the TV when we really need a break. We have no family nor friends nearby, so sometimes, for example, if one of us is showering and the other one has to make dinner, we use the TV. It’s easy to say ‘Let the toddler play with you in the kitchen meanwhile then’ or whatever, but sorry, our son is super demanding and wants to be held A LOT. So no, sometimes we need to use the TV to be able to function,” the parent explained.
Visit BrainDamaged.news for more stories about the harmful effects of screen time.
Watch this video to learn how excessive screen time and the pandemic affect children’s eyesight .
This video is from the High Hopes channel on Brighteon.com . More related stories:
Study: Childhood inactivity and screen time linked to heart damage in young adults .
Are screens as bad for toddlers as they say? Study says yes .
Study: Excessive screen time during COVID-19 lockdowns impaired children’s sense of balance .
Excessive use of video games, social media and the internet linked to poor academic performance .
Screen time found to have direct impact on speech delays in babies, reveals new research .
Sources include:
TheEpochTimes.com
TelethonKids.org.au
Brighteon.com Take Action:Support Natural News by linking to this article from your website.Permalink to this article:CopyEmbed article link:CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
6 Best Natural Adderall Alternatives for Adults in 2024
In recent years, there has been a growing interest in natural alternatives to prescription medications like Adderall. This shift comes from a desire to avoid side effects associated with pharmaceuticals and to embrace a more holistic approach to health. As we step into 2024, several natural supplements have emerged as potential substitutes for those seeking to manage ADHD symptoms or enhance cognitive performance without the use of traditional stimulant medications. Below we explore six top natural Adderall alternatives that adults might consider.
1.Ginkgo Biloba
Ginkgo Biloba is an ancient plant extract known for its cognitive-enhancing properties. Studies suggest that it can improve focus, memory, and executive functions, which makes it a popular alternative for adults looking for a natural cognitive boost.
2.L-Theanine with Caffeine
Found naturally in green tea, L-Theanine has calming properties that can moderate the jitters often associated with caffeine intake. When combined, L-Theanine and caffeine can provide smooth energy and concentration improvements, mimicking some of the beneficial effects of Adderall.
3.Rhodiola Rosea
Rhodiola Rosea is an adaptogen herb acclaimed for its stress-reducing and brain-boosting benefits. It supports the body’s stress response system and can enhance mental stamina, providing an alternative way to improve focus and productivity.
4.Bacopa Monnieri
An herb commonly used in Ayurvedic medicine, Bacopa Monnieri may support cognitive processes such as learning rate, memory formation, and verbal recall. It’s considered one of the most effective natural nootropics available.
5.Omega-3 Fatty Acids
Omega-3 fatty acids are essential nutrients that play a significant role in brain health and function. High concentrations are found in fish oil supplements, which can support brain cell structure and neurotransmitter function, translating into improved focus and cognition.
6.Ashwagandha
Ashwagandha is another adaptogen that has been shown to help reduce anxiety and stress while improving concentration and energy levels. Its potential positive impact on brain health and cortisol levels makes it a sought-after natural stimulant-free alternative to pharmaceutical options like Adderall.
While these natural supplements show promise as potential alternatives to Adderall for cognitive enhancement or ADHD symptom management in adults, it’s important to consult with a healthcare provider before making any changes to your medication regimen. Natural doesn’t always mean risk-free, so professional guidance is crucial when considering these options.
AI Reveals Brain Oscillations for Memory and Disease

Summary: A recent study showcases a significant leap in the study of brain oscillations, particularly ripples, which are crucial for memory organization and are affected in disorders like epilepsy and Alzheimer’s. Researchers have developed a toolbox of AI models trained on rodent EEG data to automate and enhance the detection of these oscillations, proving their efficacy on data from non-human primates.
This breakthrough, stemming from a collaborative hackathon, offers over a hundred optimized machine learning models, including support vector machines and convolutional neural networks, freely available to the scientific community. This development opens new avenues in neurotechnology applications, especially in diagnosing and understanding neurological disorders.
Key Facts:
> AI-Driven Innovation: The study introduces a toolbox of AI models capable of detecting brain ripples, key in memory organization and neurological diseases.
Cross-Species Application: Initially trained on rodent data, these models have been successfully tested on non-human primate EEG data, indicating potential for human application.
Open-Source Contribution: Over a hundred machine learning models from the project are now openly available for research use and further development, demonstrating the collaborative spirit of the scientific community.
Source: CSIC
The study of brain oscillations has advanced our understanding of brain function. Ripples are a type of fast oscillations underlying the organization of memories. They are affected in neurological disorders such as epilepsy and Alzheimer’s.
For this reason, they are considered an electroencephalographic (EEG) biomarker. However, ripples exhibit various waveforms and properties that can be missed by standard spectral methods. The model toolbox emerged as a result of a hackathon, which resulted in a short list for the best detection models. Credit: Neuroscience News Recently, the neuroscience community called for the need to better automate, harmonize, and improve the detection of ripples across a range of tasks and species. In the study, the authors used recordings obtained in laboratory mice to train a toolbox of machine learning models.
“We have tested the ability of these models using data from non-human primates that were collected at Vanderbilt University (Nashville, USA) by Saman Abbaspoor and lab leader Kari Hoffman as part of the Brain Initiative.
“We found that it is possible to use rodent EEG data to train AI algorithms that can be applied to data from primates and possibly human, provided the same type of recording techniques are used.”, De la Prida explains.
The model toolbox emerged as a result of a hackathon, which resulted in a short list for the best detection models. These architectures were then harmonized and optimized by the authors who now provide all codes and data openly to the research community.
Models include some of the best-known supervised learning architectures, such as support vector machines, decision trees, and convolutional neural networks.
“We have identified more than one hundred possible models from the different architectures that are now available for application or retraining by other researchers.”, commented Andrea Navas Olivé and Adrián Rubio, who are first authors of the work.
“This bank of AI models will provide new applications in the field of neurotechnologies and can be useful for detection and analysis of high-frequency oscillations in pathologies such as epilepsy, where they are considered clinical markers” concludes De la Prida, who is part of the CSIC’s AI-HUB connection aimed at advancing the use of AI and its applications. About this AI and neuroscience research news
Author: Maria Gonzalez
Source: CSIC
Contact: Maria Gonzalez – CSIC
Image: The image is credited to Neuroscience News
Original Research: Open access.
“ A machine learning toolbox for the analysis of sharp-wave ripples reveals common waveform features across species ” by Kari Hoffman et al. Communications Biology
Abstract
A machine learning toolbox for the analysis of sharp-wave ripples reveals common waveform features across species
The study of sharp-wave ripples has advanced our understanding of memory function, and their alteration in neurological conditions such as epilepsy is considered a biomarker of dysfunction.
Sharp-wave ripples exhibit diverse waveforms and properties that cannot be fully characterized by spectral methods alone.
Here, we describe a toolbox of machine-learning models for automatic detection and analysis of these events.
The machine-learning architectures, which resulted from a crowdsourced hackathon, are able to capture a wealth of ripple features recorded in the dorsal hippocampus of mice across awake and sleep conditions. When applied to data from the macaque hippocampus, these models are able to generalize detection and reveal shared properties across species.
We hereby provide a user-friendly open-source toolbox for model use and extension, which can help to accelerate and standardize analysis of sharp-wave ripples, lowering the threshold for its adoption in biomedical applications.Join our Newsletter I agree to have my personal information transferred to AWeber for Neuroscience Newsletter ( more information )Sign up to receive our recent neuroscience headlines and summaries sent to your email once a day, totally free.
Brain Waves at Night: The Key to Preventing Alzheimer’s and Parkinson’s?

Scientists have discovered that the brain’s activity during sleep, particularly the generation of rhythmic brain waves, is crucial for flushing out waste. This process could offer new strategies for preventing neurodegenerative diseases and improving sleep efficiency, potentially reducing the necessity for long sleep durations. Findings could pave the way for innovative strategies to tackle Alzheimer’s and various other neurological disorders.
There lies a paradox in sleep. Its apparent tranquility juxtaposes with the brain’s bustling activity. The night is still, but the brain is far from dormant. During sleep, brain cells produce bursts of electrical pulses that cumulate into rhythmic waves – a sign of heightened brain cell function.
But why is the brain active when we are resting?
Slow brain waves are associated with restful, refreshing sleep. And now, scientists at Washington University School of Medicine in St. Louis have found that brain waves help flush waste out of the brain during sleep. Individual nerve cells coordinate to produce rhythmic waves that propel fluid through dense brain tissue, washing the tissue in the process.
“These neurons are miniature pumps. Synchronized neural activity powers fluid flow and removal of debris from the brain,” explained first author Li-Feng Jiang-Xie, PhD, a postdoctoral research associate in the Department of Pathology & Immunology. “If we can build on this process, there is the possibility of delaying or even preventing neurological diseases, including Alzheimer’s and Parkinson’s disease, in which excess waste – such as metabolic waste and junk proteins – accumulate in the brain and lead to neurodegeneration.”
The findings were recently published in the journal Nature . Brain Cells and Waste Removal
Brain cells orchestrate thoughts, feelings, and body movements, and form dynamic networks essential for memory formation and problem-solving. But to perform such energy-demanding tasks, brain cells require fuel. Their consumption of nutrients from the diet creates metabolic waste in the process.
“It is critical that the brain disposes of metabolic waste that can build up and contribute to neurodegenerative diseases,” said Jonathan Kipnis, PhD, the Alan A. and Edith L. Wolff Distinguished Professor of Pathology & Immunology and a BJC Investigator. Kipnis is the senior author on the paper. “We knew that sleep is a time when the brain initiates a cleaning process to flush out waste and toxins it accumulates during wakefulness. But we didn’t know how that happens. These findings might be able to point us toward strategies and potential therapies to speed up the removal of damaging waste and to remove it before it can lead to dire consequences.” The Mechanism of Brain Cleaning
But cleaning the dense brain is no simple task. Cerebrospinal fluid surrounding the brain enters and weaves through intricate cellular webs, collecting toxic waste as it travels. Upon exiting the brain, contaminated fluid must pass through a barrier before spilling into the lymphatic vessels in the dura mater – the outer tissue layer enveloping the brain underneath the skull. But what powers the movement of fluid into, through, and out of the brain?
Studying the brains of sleeping mice, the researchers found that neurons drive cleaning efforts by firing electrical signals in a coordinated fashion to generate rhythmic waves in the brain, Jiang-Xie explained. They determined that such waves propel the fluid movement.
The research team silenced specific brain regions so that neurons in those regions didn’t create rhythmic waves. Without these waves, fresh cerebrospinal fluid could not flow through the silenced brain regions and trapped waste couldn’t leave the brain tissue. Enhancing the Brain’s Cleaning Process
“One of the reasons that we sleep is to cleanse the brain,” Kipnis said. “And if we can enhance this cleansing process, perhaps it’s possible to sleep less and remain healthy. Not everyone has the benefit of eight hours of sleep each night, and loss of sleep has an impact on health. Other studies have shown that mice that are genetically wired to sleep less have healthy brains. Could it be because they clean waste from their brains more efficiently? Could we help people living with insomnia by enhancing their brain’s cleaning abilities so they can get by on less sleep?”
Brain wave patterns change throughout sleep cycles. Of note, taller brain waves with larger amplitude move fluid with more force. The researchers are now interested in understanding why neurons fire waves with varying rhythmicity during sleep and which regions of the brain are most vulnerable to waste accumulation.
“We think the brain-cleaning process is similar to washing dishes,” neurobiologist Jiang-Xie explained. “You start, for example, with a large, slow, rhythmic wiping motion to clean soluble wastes splattered across the plate. Then you decrease the range of the motion and increase the speed of these movements to remove particularly sticky food waste on the plate. Despite the varying amplitude and rhythm of your hand movements, the overarching objective remains consistent: to remove different types of waste from dishes. Maybe the brain adjusts its cleaning method depending on the type and amount of waste.”
Reference: “Neuronal dynamics direct cerebrospinal fluid perfusion and brain clearance” by Li-Feng Jiang-Xie, Antoine Drieu, Kesshni Bhasiin, Daniel Quintero, Igor Smirnov and Jonathan Kipnis, 28 February 2024, Nature .
DOI: 10.1038/s41586-024-07108-6
The study was funded by the National Institutes of Health.
Debunking the 10% Brain Myth
Many people believe that we only use 10% of our brains, but this idea isn’t supported by science. This article will explore where this myth came from, why it’s so appealing, and what the truth really is about our brain’s capabilities. Despite being disproven by modern neuroscience, the myth continues to capture our imagination, suggesting we have vast unused potential. Let’s uncover the facts and understand how our brains truly function. Origins of the 10% Brain Usage Myth
The myth that humans only use 10% of their brains is a widely accepted notion, yet thoroughly unfounded in scientific fact. Its origins are murky but can be traced back to the early 20th century, when it was mistakenly propagated by misinterpretations of neurological research. Over time, this myth has been perpetuated by popular culture, self-help industries, and even some educators, without any empirical evidence to support it. Fact Check
Claim: Humans only use 10% of their brains
Description: A widely circulated belief suggests that humans only utilize 10% of their brain’s capacity, implying that there is a vast amount of untapped potential. This belief, often propagated by popular culture and self-help industries, has been thoroughly debunked by modern neuroscience, which demonstrates active use and function across nearly all parts of the brain.
Rating: False
Rating Explanation: The claim that humans only use 10% of their brains is not supported by scientific evidence. Research, especially neuroimaging studies, show that much more of the brain is active even during simple tasks.
One probable source for this myth is the work of psychologist William James, who in the 1900s, suggested that individuals are not making full use of their mental capacities. However, James never specified any percentage, which indicates the 10% figure could have been an arbitrary embellishment that was added as the statement was passed along. Additionally, the advent of neuroimaging has debunked this myth by showing that, even during simple tasks, much more than 10% of the brain is active.
Another contributing factor to the persistence of this myth is its appeal to the imagination and its implication that achieving untapped potential is merely a matter of tapping into the dormant 90% of our brainpower. This notion is inherently appealing, suggesting a vast reservoir of untapped intellectual and cognitive abilities just waiting to be unlocked. However, neuroscience has repeatedly shown that nearly all parts of the brain have a known function and are active at various times depending on the activity being performed.
The endurance of the 10% brain usage myth also reflects a misunderstanding of brain plasticity and the brain’s operational efficiency. Brain plasticity refers to the organ’s ability to adapt to new experiences, a process that engages various areas of the brain beyond any simplistic fractional capacity. Moreover, the human brain is an organ of remarkable efficiency; its structure and functionality have evolved to maximize its operational capabilities and metabolic energy consumption. Utilizing only a fraction of its capacity would contradict the principles of evolutionary biology that govern organ development.
In exploring the rationale behind the myth, it’s essential to consider the allure of the unknown that characterizes much of the human experience. Myths like these flourish in environments where curiosity meets a lack of understanding. They offer simplistic explanations for complex phenomena and provide a framework for interpreting the vast capabilities and mysteries of the human mind. Despite being debunked, the myth persists, a testament to the enduring appeal of human potential and the quest for self-improvement.
The perpetuation of the 10% myth serves as a reminder of the importance of critical thinking and the need for public education in scientific literacy. Debunking such myths is crucial in fostering a more scientifically informed public, capable of distinguishing fact from fiction in an age dominated by an overload of information. While the allure of unlocking ‘hidden’ potential is enticing, it is through the diligent application of scientifically sound principles and practices that true cognitive and intellectual growth occurs. Scientific Evidence Against the Myth
Modern neuroscience tells us that the human brain’s capacity is far more complex and capable than the outdated myth of using only 10% of our brain power. Instead of focusing on debunked myths, current research delves into the brain’s real capabilities, exploring how it processes information, adapts to new challenges, and enables human beings to learn and grow throughout their lives.
One of the brain’s remarkable qualities is its ability to reorganize itself by forming new neural connections. This process, known as neuroplasticity, occurs not just in childhood but throughout an individual’s lifetime. It allows the brain to compensate for injury, adjust to new experiences, and learn new information and skills. In essence, the brain’s adaptability is crucial for our ability to navigate the world, solve problems, and develop personal and collective knowledge.
Neuroscientists have also uncovered that each part of the brain holds specific functions, yet they work together in a sophisticated network. While certain areas might be responsible for language, others govern emotion or decision-making. This division of labor, known as functional specialization, demonstrates that far more than a mere 10% of the brain is constantly at work, even in simple daily tasks.
Another area of fascination in neuroscience is the exploration of the brain’s capacity for memory. The human brain can store a vast amount of information, from factual knowledge to personal memories, and even skills we don’t consciously think about, like riding a bicycle. This capacity for memory is not fixed but can expand and change with experience, a phenomenon linked closely to the brain’s plasticity.
Moreover, the speed at which the brain processes information is astounding. It interprets signals from our senses, allows us to react to the world around us, and fuels our thoughts and creativity. This rapid processing capability is essential for understanding complex environments and making quick decisions.
However, despite these incredible capabilities, the brain also has its limits. Factors such as stress, lack of sleep, and poor nutrition can negatively affect brain function, highlighting the importance of taking care of both our physical and mental health.
In conclusion, […]
Don’t Give Up on Your Memory No Matter Your Age

Key points
Memory loss seems like an inevitable feature of aging, especially with current news stories.
New research shows how these attitudes about aging can penetrate one’s confidence in one’s own memory.
Some effort plus self-confidence may be all a person needs to keep their memory in shape no matter their age.
Memory is in the news with the release of the Special Counsel Report claiming that President Joe Biden suffers from severe memory lapses. It goes without saying that these claims were made without the benefit of any psychological testing. However, this fact seems to escape public attention . Apart from any political damage this inflicts on Biden, there are statements in the report that would lead anyone, President or not, to worry about their memory as they age. One quote from the New York Times article particularly stands out as emerging from the report: “It would be difficult to convince a jury that ‘a former president well into his 80s’ was guilty of a felony that ‘requires a mental state of willfulness.'”
Such statements tap into the general belief age is associated with inevitable mental decline, a view that permeates many people’s everyday speech. Indeed, reading about the assessment of Biden’s memory could make anyone, whether 80-ish or not, wonder if there is no way to escape age’s toll on your memory.
Yet, how sure are researchers that memory actually does fall apart in a steady drip-drip of loss? Even one of the world’s greatest experts on cognitive aging, Baycrest Academy’s Fergus Craik (2023), suggests that there is a great deal of neuroplasticity in later life and that much of what goes wrong in memory isn’t due to faulty recall. Instead, faulty encoding of new information is the culprit, a process further hampered when people don’t put enough energy into trying to lock this new information in place. As such, the data fit the well-known adage about memory in general: “If you don’t encode, you can’t retrieve.” Put your effort into encoding, and you could avoid what seems like an inevitable mental decay. How Can Encoding Be Improved?
There may be neurophysiological changes in later life that hamper that all-important process of encoding, as Craik also points out, so not all of the poorer performance of older adults can be attributed to a lack of effort in the data entry stage of memory. However, given that your brain will do what your brain wants to do, how can you nudge it to become more efficient?
A new study by Hong Kong Technical Institute’s Michael Yeung (2024) provides some potential answers. Related to “effort” is the process known as “metamemory,” or your thoughts and beliefs about how to snap your mental powers into shape. Specifically, “the knowledge and monitoring of one’s own memory” includes control, in which you “deploy strategies to enhance subsequent learning and memory.” When you go through that all-important encoding process of new information, you can decide how hard it will be to recall it later, and when you then need to retrieve it, you can similarly try to predict whether the information will come back to you.
You can relate to this process if you think about the increasingly common two-factor authentication that many apps and online sites use to validate your identity . You see the six-digit code pop up on your phone or in your email, and then it’s up to you to remember it long enough to key it in. When you see those numbers, do you panic and think there’s no way they’ll stick around long enough in your head to recall them, even for a few seconds? Or does this seem so easy that it doesn’t trouble you at all?
Prior research, Yeung maintains, hasn’t come to a clear set of conclusions about how effective monitoring is when it comes to real-life situations such as these, or at least as tested in the lab. Describing this effect as “elusive,” he suggests that part of the reason for the lack of clarity is that there’s more than simple memory involved in metamemory. This ability to think about your thinking comes from “ executive functioning ,” a feature associated with the quality of your brain’s ability to plan and organize. The goal of his study was to disentangle the two possibilities. Building Confidence to Build Metamemory
The Hong Kong researcher believed that not only would executive functioning and metamemory predict cognitive performance in his older participants but that feelings of confidence could become critical as well. He divided the standard paired-associate learning task (associating faces with pictures) into the phases of judgments of learning (JOL), or predicting the outcome of performance, from feeling of knowing (FOK), or thinking an item was familiar. Additionally, he added retrospective confidence judgments (RCFs) into the study’s model, to see how people could help or hinder their performance through this bit of mental cheerleading.
The 104 Chinese participants in the study ranged from 18 to 79 years old, stratified by age and sex into three groups. In the test phase of the learning task, participants answered questions about the recall-ability of each pair (JOL) as well as their belief that the face was one they had seen (FOK). Then they provided a simple confidence rating of whether they were correct or not on a 1-9 scale.
You could practice this task yourself the next time you have one of those authenticator screens pop up, and this will give you a sense of what participants were asked to do. The executive functioning task that the research team gave to participants also includes one you can try out yourself, namely, generating as many different animals as you can in one minute.
On average, older adults did remember fewer pairs, but they also had high confidence in both JOL and FOK. The predictive model the authors tested showed, more importantly, that higher confidence ratings, plus better executive functioning, were significant predictors of memory scores among the older adult participants. As the authors concluded: “Thus, the increased confidence […]
Natural ways to manage aches and pains

Here are some drug-free ways to manage aches and pains that have been recommended by naturopathic doctors.
For best results, speak with a naturopathic doctor who can help determine the root cause of your problem and prescribe a treatment that will work for you. Some of the natural treatments available include: Acupressure and therapeutic massage
Acupressure is a type of massage therapy – manual pressure is applied to specific pressure points on your body, similar to acupuncture – except that fingers are used instead of needles.
Deep tissue massage is known for its positive effects on back and neck pain, as well as sports injuries. Therapeutic massage may also relieve stress and help with health conditions, such as high blood pressure and fibromyalgia – a chronic (long-lasting) disorder that causes pain and tenderness throughout the body, as well as fatigue and trouble sleeping. Yoga
Yoga is a mind-body therapy that is often recommended to treat not only back pain but also the stress that accompanies it. Various yoga poses improve muscle flexibility, increase the body’s release of endorphins that block the nerve cells that receive pain signals (essentially turning off your pain), promote relaxation and improve your confidence and sense of self-control. Music therapy
Music is commonly incorporated into various modes of exercise or regular physical activity by competitive athletes and recreational exercisers alike.
A study published in the British Journal of General Practic e is one of many studies that provide considerable evidence of music helping to decrease pain levels. Researchers explain that when you listen to music, your brain releases endorphins that block the nerve cells that receive pain signals , essentially turning off your pain.
In another study published in the Journal of Functional Morphology and Kinesiology , researchers found that listening to music while exercising often results in improved performance . Natural herbs and spices
Mother Nature has provided these natural pain management solutions – e.g., aloe vera, boswellia (Indian frankincense), chamomile, chili peppers, cinnamon, cloves, devil’s claw, echinacea, eucalyptus, garlic, ginger, ginkgo biloba, ginseng, lavender, maritime pine bark, peppermint, rosemary, turmeric and white willow bark – that are gentle to your body and just as effective at relieving pain as prescription medications. (Related: These 7 herbs can help you through life’s aches and pains .) Heat and cold therapy
Alternating heat and cold therapy helps reduce exercise-induced muscle pain or osteoarthritis effectively.
Cold therapy (ice packs are a great choice for the first 72 hours after an injury) helps reduce the temperature of the skin and muscles and decreases blood flow and metabolic processes, which, in turn, reduces inflammation or swelling that causes the pain.
Heat therapy, on the other hand, does the opposite, thus soothing stiff joints and relaxing the muscles.
Note that neither option should be used for more than 10-15 minutes at a time , according to the U.S. Pain Foundation. Seek a professional
Consulting with a licensed natural health practitioner to find the right treatment for your health issues is always the best choice. To find a licensed naturopath near you, visit the American Association of Naturopathic Physicians’ (AANP) website .
AlternativeMedicine.news has more stories about natural remedies for various ailments.
Watch the following video to learn about a natural pain-killing plant that you can find in most backyards in every U.S. state . This video is from the Saranra channel on Brighteon.com . More related stories:
Not just a cute plant, the bunny ears cactus relieves pain naturally.
Tamarind more effective than standard analgesics, study shows.
The cabbage tree relieves pain and inflammation without any of the side effects caused by conventional drugs.
Sources include:
VerywellHealth.com
MedicalNewsToday.com
NIAMS.NIH.gov
Healthline.com
NCBI.NLM.NIH.gov 1
NCBI.NLM.NIH.gov 2 USPainFoundation.org Naturopathic.org Brighteon.com
Bioactive compounds in GINKGO BILOBA found to improve cognitive recovery after stroke

A preliminary study revealed that ischemic stroke survivors had faster and better recovery of cognitive function after receiving injections of ginkgo diterpene lactone meglumine (GDLM) – a combination of the biologically active components of the “living fossil,” ginkgo biloba.
One of the three main strokes, ischemic stroke occurs when a blood clot (called a thrombus) blocks or clogs an artery leading to the brain.
GDLM is made of extracts from ginkgo biloba, an herb used in Traditional Chinese Medicine (TCM) and considered the oldest living tree species in the world. GDLM is composed of ginkgolides A, B and K and has been widely used in the treatment of ischemic stroke in China. (Related: Ginkgo biloba shows potential value in the treatment of over 100 diseases .) How the study was done
In early 2023, researchers tested the effects of GDLM on more than 3,000 survivors of mild to moderate stroke at 100 centers in China and analyzed their cognitive recovery. Most of the patients’ cognitive status was reported as “moderately impaired” using the Montreal Cognitive Assessment Scale (MoCA), with an average score of 17 out of 30.
About half of the stroke survivors were randomly selected to receive daily intravenous injections of 25 milligrams (mg) of GDLM for 14 days, while the other half received daily intravenous placebo injections.
Capital Medical University Clinical Epidemiology Assistant Professor Dr. Anxin Wang at the Beijing Tiantan Hospital said: “If our positive results are confirmed in other trials, GDLM injections may someday be used to improve cognitive function for patients after ischemic stroke.” What the researchers found
Compared to initial cognitive screening assessment scores, the researchers reported that: By day 14, stroke survivors who received the GDLM injections had improved cognitive scores at an average of 3.93 points – 3.62 points higher than those who received placebo injections.
By day 90, those who received the GDLM injections had even more improved cognitive scores at an average of 5.51 points – 5.04 points higher than those who received the placebo treatment.
Wang said: “The proportion of patients who reached a clinically significant level of improvement was 20 percent higher in the GDLM group – indicating that GDLM injections may improve cognitive function in patients with acute ischemic stroke. Since the follow-up time in this study was only 90 days, the longer-term effect of GDLM injections requires longer-term research.”
Wang further noted that GDLM shows a neuroprotective effect through multiple mechanisms, such as expanding brain blood vessels, improving the tolerance of brain cells to hypoxia (inadequate oxygen) and increasing cerebral blood flow. Other studies have also found that GDLM can promote the release of chemicals that help prevent neurodegenerative diseases like Alzheimer’s and Parkinson’s disease.
Published in JAMA Network Open , the study shows that ginkgo biloba’s active compounds exert a variety of neuroprotective and reparative effects that can help maintain the blood-brain barrier; reduce brain edema; improve energy metabolism; protect against oxidation, inflammation and apoptosis; and promote angiogenesis, or the formation of new blood vessels that normally supports wound healing and supplies oxygen-rich blood to organs and tissues.
The results of this randomized clinical trial were presented at the American Stroke Association’s International Stroke Conference 2024, which was held in Phoenix on Feb. 7-9.
Visit Herbs.news for more on the health benefits of Ginkgo biloba.
Learn about ” Ginkgo biloba’s brain benefits ” by watching the video below.
This video is from the Holistic Herbalist channel on Brighteon.com . More related stories:
Ginkgo biloba promotes better blood flow and a healthy brain.
Ginkgo biloba found to have neuroprotective effects against retinal degeneration.
Ginkgo biloba, resveratrol and cacao beans scientifically proven to combat cognitive decline.
Sources include:
Newsroom.Heart.org
Stroke.org.UK
ScienceDirect.com
Nature.com
JAMANetwork.com
Brighteon.com Take Action:
Support Natural News by linking to this article from your website.Permalink to this article:CopyEmbed article link:CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
Revolutionary brain stimulation technique shows promise for treating brain disorders
The human brain’s adaptability to internal and external changes, known as neural plasticity, forms the foundation for understanding cognitive functions like memory and learning, as well as various neurological disorders. New research conducted by a team led by Dr. PARK Joo Min of the Center for Cognition and Sociality within the Institute for Basic Science (IBS) unveils a novel technique that could transform the treatment landscape for brain disorders. The team developed a non-invasive brain stimulation method called Patterned Low-Intensity Low-Frequency Ultrasound (LILFUS), which holds tremendous potential for inducing long-lasting changes in brain function.
Traditionally, magnetic and electrical brain stimulation methods have been used to modulate brain function. However, these methods come with inherent limitations that restrict their spatial resolution and penetration depth, making it challenging to precisely stimulate specific brain regions with optimal efficacy. More invasive methods, such as those that require surgical procedures, exhibit superior control and therapeutic effects for specific deep brain stimulation, but they come with risks such as tissue damage, inflammation, and infection. These limitations have fueled the search for alternative approaches that can overcome these constraints and provide more efficient and precise modulation of brain function.
In the latest study unveiled by the IBS, researchers used ultrasound to enable precise stimulation of specific brain areas. Unlike electromagnetic waves, ultrasound has the advantage of being able to penetrate deep into the brain tissues. The researchers discovered that ultrasound stimulation can modulate neural plasticity — the brain’s ability to rewire itself — through the activation of key molecular pathways. Specifically, the study pinpointed the ultrasound’s effect on mechanosensitive calcium channels in astrocytes, which controls the cells’ ability to uptake calcium and release neurotransmitters.
LILFUS was designed based on specific ultrasound parameters that mimic the brainwave patterns of theta (5 Hz) and gamma (30 Hz) oscillations observed during learning and memory processes. The new tool allowed the researchers to either activate or deactivate specific brain regions at will — intermittent delivery of the ultrasound was found to induce long-term potentiation effects, while continuous patterns resulted in long-term depression effects.
One of the most promising aspects of this new technology is its ability to facilitate the acquisition of new motor skills. When the researchers delivered ultrasound stimulation to the cerebral motor cortex in mice, they observed significant improvements in motor skill learning and the ability to retrieve food. Interestingly, researchers were even able to change the forelimb preference of the mice. This suggests potential applications in rehabilitation therapies for stroke survivors and individuals with motor impairments.
The implications of this research extend far beyond motor function. It may be used to treat conditions such as depression, where altered brain excitability and plasticity are prominent features. With further exploration, LILFUS could be adapted for various brain stimulation protocols, offering hope for various conditions ranging from sensory impairments to cognitive disorders.
Dr. Park stated, “This study has not only developed a new and safe neural regulation technology with long-lasting effects but has also uncovered the molecular mechanism changes involved in brainwave-patterned ultrasound neural regulation.” He further conveyed, “We plan to continue follow-up studies to apply this technology for the treatment of brain disorders related to abnormal brain excitation and inhibition and for the enhancement of cognitive functions.”
Talking fast linked to better brain health in old age
Photo by Connor Olson from Unsplash TORONTO, Ontario — It turns out that talking slowly and clearly may not be so great after all. Researchers from the Baycrest Centre for Geriatric Care and the University of Toronto have found that talking speed can serve as an important indicator of brain health – even more so than having a difficulty finding certain words in old age.
Study authors add this is one of the first studies to assess both the differences in natural speech and brain health among a group of healthy adults.
“Our results indicate that changes in general talking speed may reflect changes in the brain,” says Dr. Jed Meltzer, Baycrest’s Canada Research Chair in Interventional Cognitive Neuroscience and the lead author on this study, in a media release . “This suggests that talking speed should be tested as part of standard cognitive assessments to help clinicians detect cognitive decline faster and help older adults support their brain health as they age.”
This project included 125 healthy volunteers (ages 18-90). Participants filled out three distinct assessments. The first test was a picture-naming game, in which they had to answer questions about pictures while ignoring distracting words heard through headphones. For instance, while looking at an image of a mop, participants might have to answer: “Does it end in ‘p’?” – all while simultaneously hearing the word “broom” as a distraction. This approach allowed researchers to test peoples’ capacity to recognize an image and recall the name.
Then, researchers recorded participants as they described two complex images. Each picture was on display for a total of 60 seconds. Next, language performances underwent an analysis using AI-based software, provided by Winterlight Labs. Study authors analyzed how fast each participant spoke and how much they paused.
Finally, the last test entailed participants completing standard tests aimed at assessing mental abilities known to decline with age and show a link to dementia risk. More specifically, executive function, which refers to the ability to manage conflicting information, stay focused, and avoid distractions . Researchers have found that talking speed can serve as an important indicator of brain health (credit: University of Texas at Austin) As researchers predicted, many cognitive skills showed a clear decline with age, such as word-finding speed. Surprisingly, however, while the ability to recognize a picture and recall its name both tended to deteriorate with age, this development did not show an association with a decline in other mental abilities. In other words, the amount and length of pauses participants needed to find the right words showed no link to brain health .
Instead, how fast participants could name pictures predicted how fast they spoke in general, and both of those factors showed a link to executive function . So, the results suggest it isn’t pausing to find words that shows the strongest link to brain health, but the speed of speech surrounding pauses.
Although plenty of older people understandably grow concerned about their need to pause to search for words, these findings suggest such issues are nothing more than a normal part of growing old. The slowing down of normal speech, though, independent of pausing, may be a much more important indicator of brain health changes.
Moving forward, researchers would like to conduct the same tests with a group of participants over several years in order to analyze if speed speech is truly predictive of brain health for individuals as they age. The results of such studies could serve as vital support for the development of tools for detecting cognitive decline as early as possible. This would help clinicians and doctors prescribe interventions to help older patients maintain or even improve their brain health and cognition.
The study is published in the journal Aging Neuropsychology and Cognition.
You might also be interested in:
Draft law in France proposes exorbitant fine, jail time for OPPONENTS of COVID-19 injections

A draft law in France has put forward an exorbitant fine of €45,000 ($48,627) and three years’ jail time for individuals who speak out against the dangerous Wuhan coronavirus (COVID-19) injection.
Professor Michel Chossudovsky, the founder and director of the Center for Research on Globalization (CRG), expounded on this draft law in a Feb. 18 piece. He mentioned that on Feb. 14, the French National Assembly adopted a controversial draft law to fight what it called “sectarian drift.”
The French Interministerial Mission of Vigilance and Combat against Sectarian Drifts (MIVILUDES) defined the concept as “a diversion of freedom of thought, opinion or religion that violates public order.” In other words, sectarian drift pertains to ideas, opinions or actions that go against the dictates of a totalitarian government.
According to Chossudovsky, Article Four of the draft law seeks to extend the concept of sectarian drift to health and medicine by creating a new crime of “provocation to abstention from medical care.” Under this edict, “provocation” on a sick person to “abandon or refrain from following medical treatment” if this abandonment is presented as beneficial when it could lead to dangerous consequences is now punishable under the French Criminal Code. It also acknowledged that this sectarian draft increased dramatically during the COVID-19 pandemic and “the use of social networks.”
The CRG founder added that Article Four “aims to fight against ‘charlatans’ and ‘gurus 2.0,'” who allegedly promote on the internet methods presented as “miracle solutions” to cure serious diseases such as cancers. Often without scientific training and in defiance of science, they can drift toward behaviors of sectarian influence, the French government claimed.
Chossudovsky pointed out that French citizens engaging in these “provocations” could face “three years of imprisonment and a fine of €45,000 ($48,627).” But looking at it closely, Article Four of the draft law codifies punishment for opposition to medical tyranny and the COVID-19 vaccine – even though the document does not mention it explicitly. (Related: Opposition to mRNA injections now considered a CRIME in France, violators face 45,000 euro fine and 3 years in prison for questioning “the science.” ) France’s draft law criminalizes health freedom
The CRG founder and director further explained that sectarian drift “points to non-conformity in response to an official government narrative.” He continued: “[While] the draft law does not explicitly refer to the COVID-19 vaccine … it constitutes an abominable threat [as] it criminalizes the protest movement against the COVID-19 vaccine.”
French lawyer David Guyon also pointed out the absurdity of the draft law. “In reality, it is clear that anyone who has criticized vaccination against COVID-19 could be considered of having committed and offense,” he said. “This is why it must be fought.”
According to Chossudovsky, the draft law is the brainchild of French President Emmanuel Macron. It will be presented to the French Senate by Interior Minister Gerard Darmanin in the name of former Prime Minister Elisabeth Borne.
“What this decision … implies is that the lie has become the truth. You can be arrested for informing friends and neighbors that the COVID-19 vaccine is a toxic substance,” he remarked. “What we are witnessing is the outright ‘criminalization of the state apparatus’ – whereby politicians, members of parliament [and] senior government officials are routinely bribed, co-opted or threatened to abide by a diabolical project, which is literally destroying people’s lives worldwide.”
“The French government, the National Assembly and the Senate must be challenged by a mass movement across France and the European Union,” Chossudovsky concluded, calling on the French upper legislature to “dismiss the National Assembly’s adoption of the draft law.”
Head over to MedicalTyranny.com for more stories about laws criminalizing opposition to the COVID-19 injection.
Watch this video that discusses France’s new draft law that criminalizes opposition to COVID-19 vaccines.
This video is from the chriswillard777 channel on Brighteon.com . More related stories:
Vaccine pioneer France is now skeptical of coronavirus vaccines.
Thousands take to the streets in protest of COVID-19 vaccine passports in France.
French health minister threatens to make coronavirus vaccinations compulsory for health workers.
OBEY OR ELSE: French government wants all adults aged 24-59 to be forcibly vaccinated for covid.
Vaccine passport now MANDATORY in France, following more than a year of corporate media propagandists claiming the idea was a “conspiracy theory.”
Sources include:
GlobalResearch.ca
Brighteon.com Take Action:
Support Natural News by linking to this article from your website.
Permalink to this article:
Copy
Embed article link:CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
How to boost neuron growth in the brain, aka neurogenesis
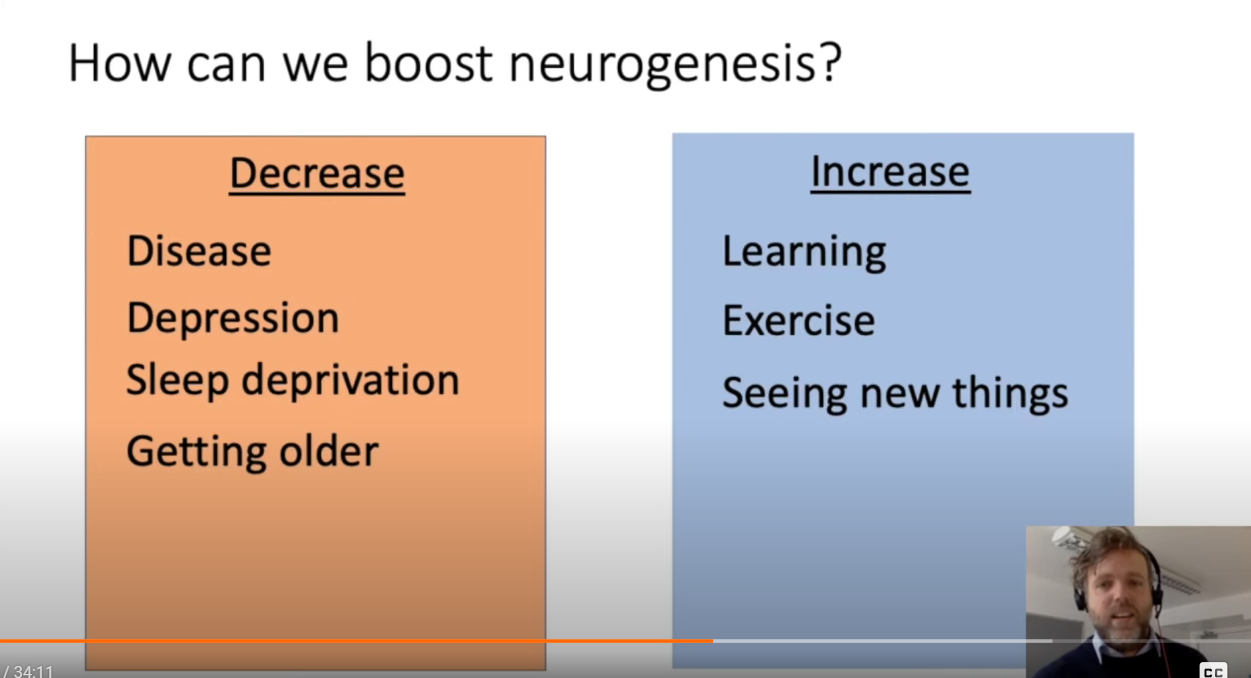
For a long time, neuroscientists believed that the neurons you are born with are the neurons you have for the rest of your life, and any neuron lost will not be replaced. Recent research has shown that specific brain regions contain neural stem cells that can generate new neurons. In this talk, Dr Daniel Berg of the University of Aberdeen will discuss what we know about these stem cells and what we can do to activate them to generate more neurons.
CDC’s expansion of vaccination schedule for Americans sparks controversy
The Centers for Disease Control and Prevention ‘s (CDC) decision to expand the vaccination schedule for Americans has sparked controversy.
According to a report by Natural Health 365 , “in recent years, the childhood injection schedule has expanded beyond addressing the diseases most commonly affecting children – such as measles, mumps and rubella.” True enough, the CDC has proposed further additions to the vaccination schedule. It released the updated schedule in September, which is months earlier than usual, to speed up insurance payments for the newly-recommended vaccines.
The updated schedule now includes several new diseases – monkeypox, respiratory syncytial virus (RSV), Wuhan coronavirus (COVID-19) hepatitis, human papillomavirus (HPV), flu and pneumococcal disease.
“The escalation in the number of shots administered at closely spaced intervals during childhood has raised significant concerns,” Natural Health 365 pointed out. “Some childhood advocacy groups are now questioning the CDC’s motives and the safety measures involved in recommending these alterations to the [vaccine] schedule.” (Related: RSV introduced into population by polio vaccines; now Pfizer’s RSV vaccines risk harming, killing people .)
Moreover, some critics have dubbed the escalating number of injections as “a risky medical experiment.” For example, children aged zero to 18 may now require up to 80 injections, representing a significant increase from the 1983 recommendation of just 11 shots.
They also argue that the CDC hasn’t subjected the entire childhood immunization schedule to thorough safety or efficacy testing. The public health agency is also in hot water for its prioritization of shots over broader public health concerns and its susceptibility to pharmaceutical influence. Several experts voice out opposition to CDC’s vaccine push
Several medical experts voiced out their opposition to the CDC’s expansion of the immunization schedule to include recent diseases.
“This amounts to nothing more than a very dangerous medical experiment foisted on America’s infants and children,” said Brian Hooker of Children’s Health Defense. He also noted that the CDC has never tested the efficacy or the safety of the entire childhood vaccination schedule.
“The CDC continues to function as a powerful promoter of vaccines, not as a protector of public health,” said integrative physician Dr. Mary Kelly Sutton. She added that there is little evidence of vaccines’ effectiveness and a lack of officially accepted research on their adverse effects.
“The CDC could give wise guidance on vaccines but has so far accepted ACIP [Advisory Committee on Immunization Practices] approvals without studies,” remarked Sutton, who who lost her license in three states for writing eight COVID-19 vaccine exemptions in California. “Universally, vaccines lack true placebo controls, and recently, lack human trials of any kind. The sad truth is pharma money rules the CDC, and the American people … are deceived and placed at risk.”
“It’s an outrage,” said pediatrician Dr. Michelle Perro. “It’s not necessary and they’re hurting our children.”
Head over to CDC.news to find more stories about the public health agency’s promotion of COVID-19 vaccines and other deadly injections.
Watch Dr. Janette Nesheiwat explain to Tucker Carlson why the COVID-19 vaccine shouldn’t be included in the CDC’s childhood immunization schedule .
This video is from the Chinese taking down EVIL CCP channel on Brighteon.com . More related stories:
VACCINES COST LIVES: Child mortality is HIGHER in developed nations that require more vaccines – new study.
Study: COVID-19 vaccines linked to increased risk of brain clots and stroke when combined with flu vaccines.
SMOKING GUN: CDC altered definition of “breakthrough” COVID infections following emails about “vaccine failure.”
CDC knowingly labeled accurate news stories about the dangers of COVID-19 vaccines “misinformation,” internal messages show.
SUPPRESSED: CDC scrapped draft alert warning of link between COVID-19 vaccines and myocarditis, deliberately keeping Americans in the dark about vaccine dangers.
Sources include:
NaturalHealth365.com
Brighteon.com Take Action:
Support Natural News by linking to this article from your website.
Permalink to this article:
Copy
Embed article link:CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
Scientists uncover brain mechanisms for social memory recall in mice
The human brain has the extraordinary ability to rapidly discern a stranger from someone familiar, even as it can simultaneously remember details about someone across decades of encounters. Now, in mouse studies, scientists at Columbia’s Zuckerman Institute have revealed how the brain elegantly performs both tasks.
“These findings are the first evidence that a single population of neurons can use different codes to represent novel and familiar individuals,” said co-corresponding author Stefano Fusi, PhD, professor of neuroscience at Columbia’s Vagelos College of Physicians and Surgeons, a principal investigator at Columbia’s Zuckerman Institute and a member of Columbia’s Center for Theoretical Neuroscience.
In a paper published today in Neuron , Columbia scientists explored social memory, the ability to remember encounters with others. This form of memory consists of two distinct mental processes-;distinguishing novel and familiar individuals, and recalling details about those who are recognized. We can readily determine whether someone is familiar but may have difficulty in recollecting the details of where and how we know that individual, especially when encountered out of context.” Steven A. Siegelbaum, PhD, co-corresponding author, Chair of the Department of Neuroscience at Columbia’s Vagelos College of Physicians and Surgeons Prior work found it difficult to pinpoint how the brain performs both tasks, given their conflicting demands. The ability to detect whether somebody is familiar or not has to apply across many different locations and events, while recollection involves remembering many specific experiences regarding a given individual.
In the new study, the scientists investigated a brain area called CA2, part of the hippocampus, a pair of seahorse-shaped brain structures essential for memory. Dr. Siegelbaum previously made the groundbreaking discovery that CA2 neurons are specifically important for social memory.
The researchers analyzed the brains of mice using calcium imaging, a technique that relies on genetically altered cells-;in this case, in CA2-;that rapidly change color when active. Calcium imaging enabled Lara Boyle, a former MD-PhD student in the Siegelbaum lab and co-first author of the study, to precisely know which neurons they were examining.
“This helped clear up uncertainty from previous research when it came to distinguishing the mouse brain’s responses to novel and familiar individuals,” said Dr. Siegelbaum, the Gerald D. Fischbach, MD, Professor of Neuroscience and of Pharmacology, and a principal investigator at the Zuckerman Institute.
The scientists first recorded how the rodents’ CA2 cells reacted when they were exposed either to a pair of strangers or a pair of familiar littermates. They next used computational methods, led by Dr. Fusi’s team, to analyze the pattern of activity in roughly 400 to 600 neurons in CA2.
The scientists found the same population of neurons encoded memories of both familiar and unfamiliar individuals. Unexpectedly, the neurons used different patterns of activity depending on a mouse’s level of familiarity with another rodent.
When mice were exposed to other mice that were unknown to them, the resulting activity in CA2 was relatively simple or, in the scientists’ parlance, “low-dimensional.” It’s as if several members of an orchestra played the exact same notes, explained Dr. Fusi. In contrast, exposure to familiar littermates led to more complex, high-dimensional CA2 activity, as if the musicians all played different melodies.
The calculations and the simulations of the researchers suggest that the more complex, or higher-dimensional, neural activity can help the brain encode the detailed memories of past encounters with familiar individuals. In contrast, the simpler, or lower-dimensional activity can help the brain reliably identify novel individuals across different contexts.
“When you encounter someone new, you may use abstract categories to describe them in your head-;for instance, that’s a child, with brown hair, red backpack,” said postdoctoral research associate Lorenzo Posani, PhD, a co-first author on the study who led the computational analysis. “Then, as you get to know them, they become a specific person and personality.”
This fundamental discovery regarding the way in which details about others are encoded may shed light on disorders affecting memory.
“When we look at different mouse models of human diseases like schizophrenia or Alzheimer’s that are known to affect memory, we now can ask more precisely how the neural activity supporting familiarity detection and recollection might be altered,” Dr. Siegelbaum said. “Our hope is that what we have learned may lead to a better understanding of the types of interventions that can rescue memory deficits in those disorders.”
The paper, “Tuned geometries of hippocampal representations meet the computational demands of social memory,” was published online in Neuron on TK, 2024.
The full list of authors includes Lara M. Boyle, Lorenzo Posani, Sarah Irfan, Steven A. Siegelbaum and Stefano Fusi.
Source:
Columbia University
Journal reference:
Boyle, L. M., et al. (2024) Tuned geometries of hippocampal representations meet the computational demands of social memory. Neuron. doi.org/10.1016/j.neuron.2024.01.021 .
Be the first to rate this article
Posted in: Medical Science News | Medical Research News
Bio-inspired neuroprosthetics: Sending signals the brain can understand
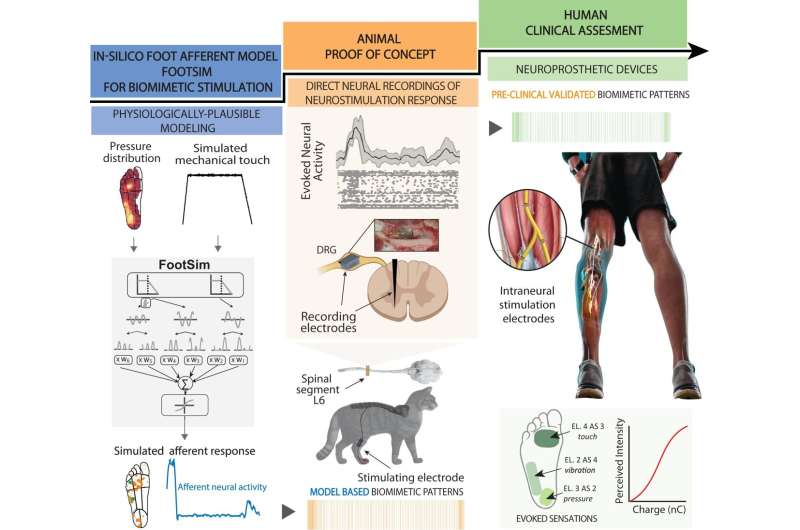
Neuroscience-driven development of a biomimetic neuroprosthetic device. The successful development of a somatosensory neuroprosthesis is based on three main pillars: (1) In-silico models of the biological sensory processing have to be exploited for emulating the natural neural activation of the nervous system to external tactile stimuli (blue segment); (2) animal proof of concept allows for experimental validation of the mechanisms behind the use of specific neurostimulation strategies defined with the use of modeling (orange segment); (3) A rigorous clinical validation of the biomimetic technology with implanted humans has to be performed in order to assess the functional outcomes in real-life scenarios (green segment). Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-45190-6 A few years ago, a team of researchers working under Professor Stanisa Raspopovic at the ETH Zurich Neuroengineering Lab gained worldwide attention when they announced that their prosthetic legs had enabled amputees to feel sensations from this artificial body part for the first time.
Unlike commercial leg prostheses, which simply provide amputees with stability and support, the ETH researchers’ prosthetic device was connected to the sciatic nerve in the test subjects’ thigh via implanted electrodes.
This electrical connection enabled the neuroprosthesis to communicate with the patient’s brain, for example relaying information on the constant changes in pressure detected on the sole of the prosthetic foot when walking. This gave the test subjects greater confidence in their prosthesis—and it enabled them to walk considerably faster on challenging terrains.
“Our experimental leg prosthesis succeeded in evoking natural sensations. That’s something current neuroprostheses are mainly unable to do; instead, they mostly evoke artificial, unpleasant sensations,” Raspopovic says.
This is probably because today’s neuroprosthetics are using time-constant electrical pulses to stimulate the nervous system. “That’s not only unnatural, but also inefficient,” Raspopovic says.
In a recently published paper in Nature Communications , he and his team used the example of their leg prostheses to highlight the benefits of using naturally inspired, biomimetic stimulation to develop the next generation of neuroprosthetics. Model simulates activation of nerves in the sole
To generate these biomimetic signals, Natalija Katic—a doctoral student in Raspopovic’s research group—developed a computer model called FootSim. It is based on data collected by collaborators in Canada, who recorded the activity of natural receptors, named mechanoreceptors, in the sole of the foot while touching different points on the feet of volunteers with a vibrating rod.
The model simulates the dynamic behavior of large numbers of mechanoreceptors in the sole of the foot and generates the neural signals that shoot up the nerves in the leg towards the brain—from the moment the heel strikes the ground and the weight of the body starts to shift forward to the outside of the foot until the toes push off the ground ready for the next step.
“Thanks to this model, we can see how sensory receptors from the sole, and the connected nerves, behave during walking or running, which is experimentally impossible to measure,” Katic says. Information overload in the spinal cord
To assess how closely the biomimetic signals calculated by the model correspond to the signals emitted by real neurons, Giacomo Valle—a postdoc in Raspopovic’s research group—worked with colleagues in Germany, Serbia and Russia on experiments with cats, whose nervous system processes movement in a similar way to that of humans. The experiments took place in 2019 at the Pavlov Institute of Physiology in St. Petersburg and were carried out in accordance with the relevant European Union guidelines.
The researchers implanted electrodes, connecting some to the nerve in the leg and some to the spinal cord to discover how the signals are transmitted through the nervous system. When the researchers applied pressure to the bottom of the cat’s paw, thereby evoking the natural neural response that occurs when a cat takes a step, the peculiar pattern of activity recorded in the spinal cord did indeed resemble the patterns that were elicited in the spinal cord when the researchers stimulated the leg nerve with biomimetic signals.
By contrast, the conventional approach of time-constant stimulation of the sciatic nerve in the cat’s thigh elicited a markedly different pattern of activation in the spinal cord. “This clearly shows that the commonly used stimulation methods cause the neural networks in the spine to be flooded with information,” Valle says. “This information overload could be the reason for the unpleasant sensations or paraesthesia reported by some users of neuroprosthetics,” Raspopovic adds. Learning the language of the nervous system
In their clinical trial with leg amputees, the researchers were able to show that biomimetic stimulation is superior to time-constant stimulation. Their work clearly demonstrated how the signals that mimicked nature produced better results: not only were the test subjects able to climb steps faster, they also made fewer mistakes in a task that required them to climb the same steps while spelling words backwards.
“Biomimetic neurostimulation allows subjects to concentrate on other things while walking,” Raspopovic says, “so we concluded that this type of stimulation is more naturally processed and less taxing on the brain.”
Raspopovic, whose lab forms part of the ETH Institute of Robotics and Intelligent Systems, believes that these new findings are not only relevant to the limb prostheses he and his team have been working on for over half a decade. He argues that the need to move away from unnatural, time-constant stimulation towards biomimetic signals also applies to a whole series of other aids and devices, including spinal implants and electrodes for brain stimulation.
“We need to learn the language of the nervous system,” Raspopovic says. “Then we’ll be able to communicate with the brain in ways it really understands.”
More information: Giacomo Valle et al, Biomimetic computer-to-brain communication enhancing naturalistic touch sensations via peripheral nerve stimulation, Nature Communications (2024). DOI: 10.1038/s41467-024-45190-6
Provided by ETH Zurich
Study suggests how brain waves are part of memory

Representative image. Image Credit: ANI Spatial navigation and memory are essential components of our daily lives. Without these talents, we would struggle to navigate our surroundings and remember previous experiences. However, the neural foundation of spatial memory remains poorly known. A study group directed by Prof. Lukas Kunz, who just joined the University Hospital Bonn (UKB), has discovered fresh information on this knowledge gap. He discovered, along with scientists from New York and Freiburg, that different types of nerve cells become active simultaneously during spatial memory and are coordinated by brain waves (“ripples”). The findings have now been published in the journal Nature Neuroscience.
Associative memory allows different pieces of information are linked together. “In the context of spatial memory, associative memory enables us to remember the locations of certain objects in the spatial environment,” explains Prof. Kunz, research group leader for Cognitive and Translational Neuroscience at the Department of Epileptology at the UKB. He is also a member of the Transdisciplinary Research Area (TRA) “Life & Health” at the University of Bonn. “For example, we can remember where in the house we put our keys”. At older age or in certain diseases such as Alzheimer’s, however, this ability is limited. “It is therefore important to investigate the neuronal basis of different forms of human memory,” said Prof. Kunz. In the long term, this could help develop new therapies for memory impairments.
Nerve cells are active while information is retrieved from memory. To further investigate this phenomenon, the researchers recorded the activity of individual nerve cells in epilepsy patients performing a memory task. “In a virtual world, the participants were asked to remember the locations of different objects,” explains Prof. Kunz. The recordings showed that different types of nerve cells became active during this memory task. Some nerve cells responded to certain objects, while other nerve cells activated in response to certain locations. The scientists observed that interactions between the different types of nerve cells became stronger over time when participants remembered the right object in the right place.
In addition to place and object neurons, the researchers observed hippocampal brain waves (“ripples”) that also occurred during the memory task, presumably playing a crucial role in the formation and retrieval of associative memories. “Ripples could be important for the connection of different types of nerve cells and the formation of complex memories. It will be exciting to further investigate this idea in future studies,” explains Prof. Kunz. It will also be interesting to study how memory performance is modulated when ripples are suppressed or triggered, providing insights into the causal relevance of ripples. Prof. Kunz intends to continue the findings that he gained with his colleagues at Columbia University’s School of Engineering and Applied Science in New York and the University of Freiburg at the University Hospital Bonn.
“The department of epileptology at the UKB is well-known for its excellent brain research. The department has the unique opportunity to record the activity of individual nerve cells in the human brain in the video EEG monitoring unit, which is the heart of every epilepsy center. This provides exciting insights into the functioning of the human brain, which is only possible at a few research centers worldwide,” describes Prof. Kunz. In his interdisciplinary research, he builds on the close exchange with other researchers and medical doctors, which is essential for the development of new research ideas. (ANI)
(This story has not been edited by Devdiscourse staff and is auto-generated from a syndicated feed.)
