Nature Knows and Psionic Success
God provides
The nice spice: Try allspice, a natural source of beneficial plant compounds

Killing Gaza | Full Documentary | HS Documentary Advertisement
It may sound like allspice is a premade blend of spices, but it’s actually a single spice.
Allspice has a unique flavor profile that is often described as a blend of up to four different spices, hence the name. The spice is also used in folk medicine due to its potential health benefits.
Allspice , also called Jamaican pepper, newspice or pimienta, is the dried, unripe berries of Pimenta dioica , a plant that belongs to the Myrtaceae family. It’s native to Jamaica, the tropical forests of South and Central America, and Southern Mexico, but it’s also commercially grown in Cuba, Honduras and Trinidad.
Allspice is made by picking the berries from the plant’s small flowers and drying them in the sun until they’re browned. Allspice is available ground or whole. It is often used as a seasoning for meats, desserts and liqueurs. (Related: Tips to help bring out the flavor of your homemade spice blends .)
When used as a spice in small amounts, allspice is considered safe to use.
However, older research suggests that people with hand dermatitis may develop allergic reactions when cooking with it.
Drug interactions are not well documented. Anecdotal evidence, however, suggests a potentially negative effect when large amounts of allspice are consumed while taking blood clotting medication.
Because of the lack of human studies on allspice’s health benefits, an appropriate dosage has yet to be determined. Beneficial compounds in allspice
Due to its many uses in folk medicine, the compounds in allspice have been studied widely.
Those behind allspice’s benefits include:
Ericifolin
Ericifolin is a phenolic compound that may have antibacterial and cancer-fighting properties.
Eugenol
Eugenol is derived from phenylpropene. It has potential antibacterial, antifungal, anti-inflammatory, and cancer-fighting properties.
Gallic acid
Gallic acid is yet another powerful antioxidant and it may have cancer-fighting and antiviral effects.
Gallic acid has also been studied for potential protective effects on brain health, especially the prevention of Alzheimer’s disease and Parkinson’s.
Quercetin
Quercetin is a type of flavonoid, a powerful antioxidant that may help protect against harmful molecules called free radicals.
Its antioxidant capacity may have cancer-fighting properties, and it’s also known for its potential antiviral and anti-inflammatory effects. Health benefits of allspice
Allspice provides many health benefits. Here are some of them, all backed by science:
Antimicrobial and antifungal effects
The eugenol and ericifolin in allspice may provide antimicrobial and antifungal effects.
Studies on essential oils extracted from allspice berries suggest that it has antifungal properties against Candida albicans , a yeast that is resistant to certain antifungal drugs.
Additionally, the essential oil shows antibacterial properties against E. coli , Listeria monocytogenes , salmonella and S. aureus . Its effects are mainly attributed to its eugenol content, which may damage bacterial membranes. Menopause treatment Menopause is the termination of the menstrual cycle in women aged 45 to 52. The condition causes hormonal changes, particularly a decline in estrogen and progesterone levels.This may cause the following symptoms: Hot flashes Mood disorders Night sweats Sleep disturbances Unintentional weight gain While hormone therapy has traditionally been the primary treatment for menopause symptoms, complementary therapies are becoming more popular, such as herbal remedies.Research suggests that allspice extract binds to estrogen receptors. This means it may trick your body into believing that its estrogen levels are up, thus helping manage symptoms. Can protect against cancer Many of allspice’s beneficial plant compounds have potential cancer-fighting properties.According to test-tube and animal studies, ericifolin, eugenol, gallic acid and quercetin may decrease tumor growth, prevent the spread of tumors and promote apoptosis or the programmed death of cancerous cells.Allspice’s anticancer effects have been studied on breast, colon, duodenal, gastric and prostate cancers. Its effect varies depending on the type of cancer.Research conducted on breast cancer cell lines suggests that allspice extract leads to autophagy , or the body’s way of clearing unnecessary or damaged cells, such as cancerous cells, by degrading them.Prostate cancer cells can also be eliminated through apoptosis, while gastric cancer cell lines were affected by allspice extracts’ ability to inhibit the growth of Helicobacter pylori , a bacterium that’s considered carcinogenic. Cooking with allspice You may buy allspice berries, whole or ground, in the supermarket’s spice aisle. Allspice essential oil can also be bought at stores and online.Store allspice in a cool, dry place, like your kitchen pantry.Allspice’s unique flavor profile makes it a versatile ingredient that can be used to give a warm, peppery flavor to different dishes. Use allspice to season seafood or fish or a dessert like allspice crumb muffins.Use whole berries the same way you would use whole cloves. Ground allspice is mostly used in baking or as a seasoning for meats, poultry, stews and vegetables.Here are some sweet and savory dishes that you can make using allspice: Autumn spice cake with cream cheese frosting Bourbon molasses cookies Chai-spiced banana bread Cincinnati chili Homemade allspice dram Pumpkin pie Slow cooker chicken with Moroccan spices Since allspice can be used in almost any dish , make sure you have it in your pantry as you prepare for the holidays.Watch the video below to learn how to make keto apple cider donuts with allspice . KETO Apple Cider Donuts Recipe JUST 2 NET CARBSThis is a modal window.No compatible source was found for this media.This video is from the Keto Recipes channel on Brighteon.com . More related stories: The sweet spice: Health benefits of nutmeg and tips for proper storage. 12 Medicinal herbs and spices that can boost the immune system. Easy kitchen hacks: How to boost the anti-inflammatory benefits of vegetables. Sources include: Healthline.com InsanelyGoodRecipes.com Brighteon.com
Researchers Identify Brain Center Responsible for Responses to Rapid Temperature Change

Research Similar to the tale of the boiling frog, flies more likely to react to rapid heating
We’ve all heard it: Put a frog in boiling water, and it will jump out. But put the same frog in lukewarm water and heat it gradually, and you’ll cook the frog. Often used as a metaphor for the unhurried and stubborn response many have to a slowly rising threat, the mechanisms underlying the urban myth have become a subject of scientific fascination.
This parable seems to have inspired new Northwestern University research, which identified a brain pathway responsible for rapid-threat detection.
“Animals are more likely to react to rapid rather than slow environmental change,” said lead author Marco Gallio , associate professor of neurobiology in Northwestern’s Weinberg College of Arts and Sciences . “In the present study, we identify a brain circuit in fruit flies that selectively responds to rapid thermal change, priming behavior for escape.”
The findings were published last week in the journal Nature Communications .
Gallio generally uses fruit flies to understand sensory circuits and the ways they create perceptions of the physical world. Using the fly as a model, the lab studies basic decision-making principles in an animal that has a fraction of the number of neurons (100,000) than humans have (roughly 100 billion). As a well-studied model organism for biological research, flies also are useful subjects because of the pre-existing tools to study fly neurons and behavior.
“There are often two types of responses to external stimuli in the brain: Some neurons respond to a stimulus like light or temperature with very persistent activity,” Gallio said. “Other neurons fire just at the beginning, like when a light turns on, and then their activity is gone. We’ve always wondered what the significance of these short-lived responses is.”
In visual stimuli, brains are wired to notice a large contrast between light and dark. Gallio said that the response intuitively also makes sense for the sense of touch: You don’t think about pressure when your hand is resting on a surface. Run your hand over something new, however, and you will detect subtle changes in texture. Gallio’s team wanted to see if the same was true for the sense of temperature.
To explore how flies respond to rapid change, the team used a high-resolution camera to observe flies navigating different temperature environments. When flies encounter a rapid heat front, they always produce a U-turn away from it.
The lab found flies always responded in cases of rapid temperature change, but not for slow change.
The team also identified a circuit in the fly brain that responds only to rapid temperature change (more than 0.2 degrees Celsius per second). Much like light-ON cells of the visual system, these neurons fired at the beginning of rapid heating and then went quiet.
“Our hypothesis was that these heat-ON responses may indeed correlate with the rate of temperature change,” said Jenna Jouandet, the study’s first author and a PhD student in the Gallio Lab. “And therefore, may allow flies to anticipate dangerous thermal conditions and prepare to escape.”
Indeed, when the researchers experimentally inactivated those neurons, flies escaped less promptly. William Kath To better understand how the activity of these neurons may be important for the behavior of the fly, the researchers collaborated with William Kath , applied math professor at Northwestern and deputy director of the new National Institute for Theory and Mathematics in Biology . Applied math PhD student Richard Suhendra built a small computer model with two antennae and two wheels to demonstrate how adding a neuron that anticipates dangerous heat could improve the flexibility of the vehicle response.
<< Play with the model through a simple game on the Gallio Lab webpage .>>
“The neurons that we initially discovered take input from the thermosensory neurons on the antennae and carry information to the higher brain,” Gallio said. “Flies are a great model to map brain circuits in that we were able to reconstruct the full circuit from sensory neurons all the way down to the centers that produce movement.”
Gallio explained that rapid changes are nearly always dangerous for a small fly.
“If the temperature is changing by half a degree per second — which is not that much — within 30 or 40 seconds, that fly could be dead,” Gallio said. “This system is an alarm bell that rings to prime an animal’s behavior for escape. We see the fly escape.”
Gallio hypothesizes that the results are broadly generalizable, especially because he sees it play out in humans, whether someone is entering a room that’s a different temperature or getting into a hot shower. He said these neurons seem to be able to sense something others do not — they seem to be able to anticipate the future. Recent Articles
Inverted Perovskite Solar Cell Breaks 25 Percent Efficiency Record
Professor Ted Sargent improved cell efficiency using a combination of molecules to address different issues. First-of-Their-Kind Wearables Capture Body Sounds to Continuously Monitor Health
The new devices developed by a team with Professor John Rogers were tested on a range of patients, from premature babies to the elderly. McCormick Faculty Named Among Global ‘Highly Cited Researchers’ for 2023
The list identifies researchers who showed significant influence by publishing highly cited papers. Are Consumers Ready for Robots at Their Doorstep?
Professor Amanda Stathopoulos found that consumers are more prepared for automated vehicle delivery than drones or robots. Get our news in your inbox.
Sign up for our newsletter.
Sign up
The Brain on Opioids: Metabolic Disruptions in Addiction

Source: Spixel/Shutterstock In recent years, the opioid epidemic has surged to alarming proportions, casting a shadow over communities worldwide. This crisis, fueled by an increase in the prescription of opioid medications and the illicit use of drugs like heroin, has led to a staggering rise in addiction , overdoses, and fatalities. The ramifications of this epidemic extend far beyond the individual, tearing at the fabric of families, overwhelming health care systems, and straining social services. Amidst this dire landscape, understanding the neural mechanisms underpinning opioid addiction is not just a scientific pursuit but a pressing necessity.
In a groundbreaking study published in the Journal of Psychiatry Neuroscience , Long Jin and colleagues have peeled back another layer in our understanding of heroin addiction, revealing its deep connections with cerebral metabolism. This research not only illuminates the complex neural underpinnings of addiction but also paves the way for innovative metabolic treatment strategies.
Heroin addiction, a relentless and often devastating condition, has long been associated with various brain network dysfunctions. However, this study delves into the metabolic aspect, examining how heroin dependence affects glucose metabolism and metabolic connectivity in the brain. The triple brain network—consisting of the default mode network (DMN), salience network (SN), and executive control network (ECN)—is the focal point of their investigation.
The research team conducted an integrated positron emission tomography/magnetic resonance imaging (PET/MRI) study on 36 individuals with heroin dependence and 30 healthy controls. Their findings were revealing: those with heroin dependence exhibited significant reductions in glucose metabolism in the bilateral anterior insula ( AI ) and inferior parietal lobule (IPL). Moreover, they observed a marked decrease in metabolic connectivity between the right AI and the left dorsolateral prefrontal cortex (DLPFC).
This study ties directly into the concept of brain energy. The brain, an energy-intensive organ, relies on efficient metabolic processes to function optimally. Disruptions in these metabolic pathways, as evidenced in heroin addiction, can lead to significant neural and cognitive impairments.
The findings from Jin et al.’s study underscore the importance of considering metabolic health in the brain when addressing addiction. Traditional treatments for heroin dependence primarily focus on managing withdrawal symptoms and preventing relapse . However, these findings suggest that targeting the underlying metabolic disturbances might be an additional, novel approach.
One promising avenue is the use of metabolic treatment strategies. These could include interventions designed to optimize brain metabolism, such as dietary modifications, supplements that support neuronal energy production, or medications that improve metabolic efficiency in the brain. For instance, since the study found a negative correlation between methadone dosage and glucose metabolism in specific brain regions, adjusting methadone treatment in conjunction with metabolic therapies might yield better outcomes. Although we don’t yet have data to confirm that these strategies might play a role in opioid addiction treatment, we do have some preliminary evidence that they might play a role in treating another addiction—alcoholism— from research conducted at the National Institute of Alcohol Abuse and Alcoholism, as described in this post .
As we continue to explore the intricate relationship between brain metabolism and mental health disorders, studies like these offer valuable insights. They not only deepen our understanding of conditions like heroin addiction but also open up new, more holistic treatment pathways. By integrating metabolic treatment strategies, we could potentially enhance cognitive control and reduce relapse rates in individuals struggling with addiction, offering a ray of hope in their journey toward recovery.
This holistic approach, aligning metabolic health with traditional psychiatric treatment, could revolutionize our approach to addiction and mental health care. It emphasizes the need for a comprehensive understanding of the brain’s energy needs and its impact on our mental well-being. As we continue to unravel the complexities of brain metabolism, we move closer to more effective, personalized treatments for those battling addiction, providing a more sustainable path to recovery and mental health.
Researchers identify brain center responsible for responses to rapid temperature change
We’ve all heard it: Put a frog in boiling water, and it will jump out. But put the same frog in lukewarm water and heat it gradually, and you’ll cook the frog. Often used as a metaphor for the unhurried and stubborn response many have to a slowly rising threat, the mechanisms underlying the urban myth have become a subject of scientific fascination.
This parable seems to have inspired new Northwestern University research, which identified a brain pathway responsible for rapid-threat detection.
“Animals are more likely to react to rapid rather than slow environmental change,” said lead author Marco Gallio, associate professor of neurobiology in Northwestern’s Weinberg College of Arts and Sciences. “In the present study, we identify a brain circuit in fruit flies that selectively responds to rapid thermal change, priming behavior for escape.”
The findings were published last week in the journal Nature Communications.
Gallio generally uses fruit flies to understand sensory circuits and the ways they create perceptions of the physical world. Using the fly as a model, the lab studies basic decision-making principles in an animal that has a fraction of the number of neurons (100,000) than humans have (roughly 100 billion). As a well-studied model organism for biological research, flies also are useful subjects because of the pre-existing tools to study fly neurons and behavior.
“There are often two types of responses to external stimuli in the brain: Some neurons respond to a stimulus like light or temperature with very persistent activity,” Gallio said. “Other neurons fire just at the beginning, like when a light turns on, and then their activity is gone. We’ve always wondered what the significance of these short-lived responses is.”
In visual stimuli, brains are wired to notice a large contrast between light and dark. Gallio said that the response intuitively also makes sense for the sense of touch: You don’t think about pressure when your hand is resting on a surface. Run your hand over something new, however, and you will detect subtle changes in texture. Gallio’s team wanted to see if the same was true for the sense of temperature.
To explore how flies respond to rapid change, the team used a high-resolution camera to observe flies navigating different temperature environments. When flies encounter a rapid heat front, they always produce a U-turn away from it.
The lab found flies always responded in cases of rapid temperature change, but not for slow change.
The team also identified a circuit in the fly brain that responds only to rapid temperature change (more than 0.2 degrees Celsius per second). Much like light-ON cells of the visual system, these neurons fired at the beginning of rapid heating and then went quiet.
“Our hypothesis was that these heat-ON responses may indeed correlate with the rate of temperature change,” said Jenna Jouandet, the study’s first author and a Ph.D. student in the Gallio Lab. “And therefore, may allow flies to anticipate dangerous thermal conditions and prepare to escape.”
Indeed, when the researchers experimentally inactivated those neurons, flies escaped less promptly.
To better understand how the activity of these neurons may be important for the behavior of the fly, the researchers collaborated with William Kath, applied math professor at Northwestern and deputy director of the new National Institute for Theory and Mathematics in Biology. Applied math Ph.D. student Richard Suhendra built a small computer model with two antennae and two wheels to demonstrate how adding a neuron that anticipates dangerous heat could improve the flexibility of the vehicle response. (Play with the model through a simple game on the Gallio Lab webpage.)
“The neurons that we initially discovered take input from the thermosensory neurons on the antennae and carry information to the higher brain,” Gallio said. “Flies are a great model to map brain circuits in that we were able to reconstruct the full circuit from sensory neurons all the way down to the centers that produce movement.”
Gallio explained that rapid changes are nearly always dangerous for a small fly.
“If the temperature is changing by half a degree per second — which is not that much — within 30 or 40 seconds, that fly could be dead,” Gallio said. “This system is an alarm bell that rings to prime an animal’s behavior for escape. We see the fly escape.”
Gallio hypothesizes that the results are broadly generalizable, especially because he sees it play out in humans, whether someone is entering a room that’s a different temperature or getting into a hot shower. He said these neurons seem to be able to sense something others do not — they seem to be able to anticipate the future.
The research reported in this publication was supported by the National Institutes of Health (grants R01NS086859, R21EY031849 and R21NS130554), a Pew Scholars Program in the Biomedical Sciences and a McKnight Technological Innovations in Neuroscience Awards. The research was supported in part through the computational resources provided for the Quest high performance computing facility at Northwestern University, which is jointly supported by the Office of the Provost, the Office for Research and Northwestern University Information Technology; the Training Grant in Circadian and Sleep Research (T32HL007909) and the National Science Foundation research training grant (DMS-1547394).
How smartphone addiction affects brain function and mental health

ISRAELI NEWS LIVE: Steven Ben-Nun interviewed by Mike Adams on Zionism, Palestine and Israel’s escalation Advertisement
Smartphone addiction has now become a global issue, thanks to the popularity of social media platforms and mobile games. While smartphones can make life easier in many ways, excessive use of smartphones and similar devices has been linked to many health issues.
According to a recent study published in Computers in Human Behavior , problematic smartphone use can cause cognitive impairments, poor sleep quality and depression . The study authors noted that although problematic smartphone use generally correlates with screen time, high screen time alone does not necessarily cause adverse effects. Smartphone use only becomes problematic when it starts to interfere with daily life.
In an article published in EXCLI Journal , Sehar Shoukat from the California Institute of Behavioral Neurosciences and Psychology discussed the dangers of problematic smartphone use and smartphone addiction. He noted that whenever a habit, such as checking or being active on social media, turns into an obligation, it quickly becomes an addiction. This addiction can easily endanger one’s well-being because of its negative influence on physical and psychological health . (Related: Study links smartphone use to heart attack and stroke risk .)
According to Shoukat, people who are “mobile addicted” are unable to cut back on their cell phone usage and often use their phones as a solution to boredom. They also get anxious or depressed when their phones are out of their reach. These negative feelings and attitude, coupled with a dependency on smartphones and other gadgets, could increase a person’s risk of developing anxiety disorders and clinical depression.
“When cell phone use becomes an addiction, the behavior becomes stressful,” said Shoukat, quoting a research on cell phone use and human behavior. Negative effects of smartphone addiction on mental health
Several studies have explored the psychological effects of excessive smartphone usage and social media addiction. While social media platforms like Facebook and X (formerly Twitter) can be accessed using laptops or desktop computers, smartphone apps appear to be the most common gateways for social media users, especially young adults.
In a study published in the American Journal of Preventive Medicine , researchers recruited 1,787 Americans aged 19 to 32 years to examine the link between social media use and perceived social isolation. They found that participants who spent the highest amount of time on social media felt more socially isolated than their counterparts who were less active online.
Individuals who frequently checked social media were also 2.7 times more likely to develop depression than those who did so less frequently. Those who spent the highest amount of time on social media had a 1.7 higher risk of depression, indicating that too much social interactions online could have a detrimental effect on mental health.
In a similar study from Canada, researchers recruited 750 young adults and asked them to complete a survey about their relationship with social media and the sacrifices they were willing to make to remain socially active online. Nearly half of the participants admitted to checking their socials more than nine times a day, while more than half reported spending over an hour on social media every day.
Not surprisingly, those addicted to social media were willing to make more compromises to maintain their online access than those who didn’t care much about their socials. About 40 percent said they were willing to give up caffeine, alcohol and video games if it meant being able to stay active on social media. Almost 10 percent were prepared to give up a year of their life, while five percent were willing to trade off five years of their life. About three percent preferred losing 10 years of their life over quitting social media.
This study shows the alarming hold social media has on many young people and how social media/smartphone addiction could be just as dangerous and life-threatening as other forms of addiction. (Related: Mental health in the digital age: 7 Ways to control your smartphone use .) Negative effects of smartphone addiction on brain health
Aside from having a negative impact on mental health, smartphone addiction can also influence the brain in an unfavorable way. Earlier studies have found that excessive use of the internet and modern devices can bring about alterations in your brain’s neural architecture and function . For instance, regularly interacting with your phone’s touchscreen has been found to trigger changes in the neural circuitry of cortical regions associated with sensory and motor processing of the hand and thumb.
Research also suggests that excessive internet usage has a detrimental effect on children’s attention, with many educators noting that “today’s digital technologies are creating an easily distracted generation.” In a study published in PNAS , researchers investigated the sustained impact of media multi-tasking – a behavioral pattern that involves interacting with multiple inputs simultaneously – on cognitive function.
They found that despite the constant practice heavy media multi-tasking individuals have (i.e., responding to notifications and prompts and navigating various hyperlinks), they still performed worse on task-switching tests than individuals who spend less time on the internet. The researchers attributed this poor task-switching ability to an “increased susceptibility to distraction from irrelevant environmental stimuli.”
Subsequent brain imaging studies have corroborated this theory. Heavy media multi-taking individuals tend to show greater activity in the right prefrontal regions of their brains , which are normally activated in response to distractor stimuli. This means that people who spend an inordinate amount of time on the internet require more effort to maintain their concentration on one thing and not give in to distracting stimuli.
Another seminal study, this time by Japanese researchers, also found that longer smartphone usage is associated with lower cognitive function and reduced volume in several areas of the brain. After following a large sample of children for years, the researchers observed a decrease in verbal intelligence among those who frequently used the internet. They also noted a reduced increase in regional gray and white matter volumes in brain areas associated with attention, emotion, executive functions, language processing […]
New Studies of Brain Activity Explain Benefits of Electroconvulsive Therapy

Why this controversial treatment works is a century-old mystery; scientists from UC San Diego may have solved it
EEG headsets like the one shown here help measure electrical activity in the brain. Patients who receive electroconvulsive therapy experience slowing in brain activity after treatment. Photo credit: Ulrichw/Pixabay Article Content
Electroconvulsive therapy (ECT), formerly known as electroshock therapy, involves inducing a brief seizure in the brain using controlled doses of electricity. While ECT is highly effective for certain mental illnesses, particularly depression, the reasons for its efficacy have long puzzled the fields of psychiatry and neuroscience.
Now, researchers from University of California San Diego may have an answer. In two new studies published November 16, 2023 in Translational Psychiatry, they propose a new hypothesis that ECT alleviates depression symptoms by increasing aperiodic activity, a type of electrical activity in the brain that doesn’t follow a consistent pattern and is generally considered to be the brain’s background noise.
“We’re solving a puzzle that’s stumped scientists and doctors since electroconvulsive therapy was first developed nearly a century ago,” said first author Sydney Smith, a PhD candidate in the Voytek Lab at UC San Diego. “On top of that, we’re also helping to demystify one of the most effective, yet stigmatized treatments for severe depression.”
Electroconvulsive therapy has a great track record, but a bad reputation. The therapy is effective in up to 80% of patients who receive the treatment, most often for depression but occasionally for bipolar disorder or schizophrenia. However, despite this high success rate, electroconvulsive therapy is frequently associated with frightening images of people receiving painful, high voltage shocks.
“A lot of people are surprised to learn that we still use electroconvulsive therapy, but the modern procedure uses highly controlled dosages of electricity and is done under anesthesia,” said Smith. “It really doesn’t look like what you see in movies or television.”
While generally safe and effective, ECT does have drawbacks, including temporary confusion and cognitive impairment. It also requires multiple outpatient visits, which can present a barrier to some people who might otherwise benefit from the treatment. Sydney Smith, PhD candidate in the Voytek Lab at UC San Diego Bradley Voytek, PhD is a professor in the department of Cognitive Science at UC San Diego and senior author on the new study, which helps explain the benefits of electroconvulsive therapy. Photo by: UC San Diego Health Sciences “One of the reasons ECT isn’t more popular is that for a lot of people, it’s easier and more convenient to just take a pill,” said senior author Bradley Voytek , PhD, professor of cognitive science at UC San Diego. “However, in people for whom medications don’t work, electroconvulsive therapy can be life-saving. Understanding how it works will help us discover ways to increase the benefits while minimizing side effects.”
The researchers used electroencephalography (EEG) scans to study the brain activity of patients who received ECT therapy for depression. They also looked at another similar form of treatment called magnetic seizure therapy, which induces a seizure with magnets instead of electrodes. Both therapies showed increased aperiodic activity levels in patients’ brains post-treatment.
“Aperiodic activity is like the brain’s background noise, and for years scientists treated it that way and didn’t pay much attention to it,” said Smith. “However, we’re now seeing that this activity actually has an important role in the brain, and we think electroconvulsive therapy helps restore this function in people with depression.”
One of the functions of aperiodic activity in the brain is helping control how neurons turn on and off. Our neurons are constantly going through cycles of excitation and inhibition that correspond with different mental states. Aperiodic activity helps boost inhibitory activity in the brain, effectively slowing it down.
“Something we see regularly in the EEG scans of people who receive electroconvulsive or magnetic seizure therapy is a slowing pattern in the brain’s electrical activity,” said Smith. “This pattern has gone unexplained for many years, but accounting for the inhibitory effects of aperiodic activity helps explain it. It also suggests that these two forms of therapy are causing similar effects in the brain.”
While these findings establish a link between aperiodic activity and ECT benefits, the researchers stress the need for further investigation to leverage these insights in clinical applications. They are currently exploring the possibility of using aperiodic activity as a metric of treatment effectiveness in other depression treatments, such as medications.
“At the end of the day, what’s most important to patients and to doctors is that the treatment works, which in the case of ECT, it does,” said Voytek. “However, it’s our job as scientists to dig into what’s really going on in the brain during these treatments, and continuing to answer those questions will help us find ways to make these treatments even more effective while reducing negative effects.”
Co-authors of the first study include: David Printz, Maryam Soltani and Celene Gonzalez at UC San Diego, Vincent Ma at Los Angeles General Medical Center and Angela Chapman at University of Iowa.
The first study was supported, in part, by National Institute of General Medicine Science (grant R01GM134363-01) and the Veterans Medical Research Foundation.
Full link to second study: https://doi.org/10.1038/s41398-023-02631-y
Co-authors of the second study include: Eena L. Kosik, Quirine van Engen, Jordan Kohn, Zafiris J. Daskalakis and Itay Hadas at UC San Diego, Aron T. Hill at Deakin University and Reza Zomorrodi and Daniel M. Blumberger at University of Toronto.
The second study was supported, in part, by National Institute of General Medicine Science (grant R01GM134363-01).
Disclosures: Zafiris J. Daskalakis has received research and equipment in kind support for an investigator-initiated study through Brainsway Inc. and Magventure Inc. and industry-initiated trials through Magnus Inc. He also currently serves on the scientific advisory board for Brainsway Inc. Bradley Voytek, PhD
A small molecule blocks aversive memory formation, providing a potential treatment target for depression
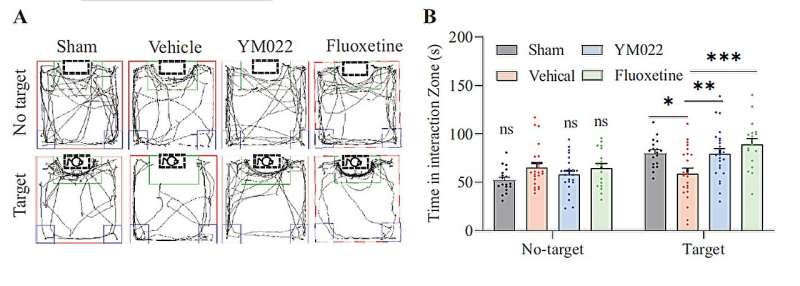
The YM022-treated mice (diagram A, second from right) spent significantly more time in the social interaction zone (framed with a green line) than the control group when the aggressive mouse was placed in the acrylic cage. The findings indicate that the treated mice exhibited less social avoidance and depressive-like behaviour induced by the previous attack. Credit: Zhang, X. et al., source: https://www.nature.com/articles/s41380-023-02127-7 Depression is one of the most common mental illnesses in the world, but current anti-depressants have yet to meet the needs of many patients. Neuroscientists from City University of Hong Kong (CityU) recently discovered a small molecule that can effectively alleviate stress-induced depressive symptoms in mice by preventing aversive memory formation with a lower dosage, offering a new direction for developing anti-depressants in the future.
“Depression affects millions of individuals worldwide, necessitating more effective treatments. Conventional methods, such as drug therapy with delayed onset of action and psychotherapy, have limitations in yielding satisfactory results for many patients. A pioneering advancement in treatment is urgently needed,” said Professor He Jufang, Wong Chun Hong Chair Professor in Translational Neuroscience at CityU.
Previous research found that stress leads to neural plasticity changes in brain’s valence-coding systems (“valence” refers to the degree to which something is pleasurable or aversive), which are strongly associated with depression, post-traumatic stress disorders and anxiety disorders.
Also, some studies revealed that depression is correlated with the hyperactivated amygdala. “However, the neural mechanism that mediates depression in amygdala is still poorly understood,” said Professor He.
Over the years, Professor He’s research group has focused on memory formation and encoding studies. Previously, they discovered that cholecystokinin (CCK), a key neuromodulator, is crucial for inducing long-term potentiation (LTP)—a lasting increase in communication strength between neurons—to enable memory formation.
They also found that the CCK and CCK-B receptors (CCKBR is one of three known types of CCK receptors in the central nervous system) mediate neuroplasticity, as well as visual and sound associative memory formation, in the auditory cortex, and trace fear memory formation in the amygdala.
Other studies have found that CCKBR antagonist (which blocks the binding of the CCK and CCK-B receptors, thus inhibiting the effect of the binding) exhibited an anti-depressant effect in mice.
So Professor He’s group hypothesized that CCK might facilitate aversive memory formation by enabling LTP in the basolateral amygdala (BLA)—a brain region involved in processing emotional memories and thought to be dysregulated in depression, thus enhancing the development of depression.
In their latest study, they tested this hypothesis using various experimental methods, including in vitro electrophysiological recording, optogenetic manipulation, drug manipulation and behavioral analysis of mice, to examine the critical role of CCK and CCKBR in depression. They found that a CCKBR antagonist called YM022 had an anti-depressant-like effect by blocking neuroplasticity-caused aversive memory formation in mice.
The study was published in Molecular Psychiatry , titled “Cholecystokinin B Receptor Antagonists for the Treatment of Depression via Blocking Long-term Potentiation in the Basolateral Amygdala.”
The results of the in-vitro recording in the BLA showed that the YM022 significantly suppressed neuroplasticity. The neuroplasticity induction rate reached 72.3% in the control group; but it was only 10.2% in the drug-treated group.
Moreover, the team underwent a series of behavioral tests to determine the antagonist’s efficacy. The results showed that depressive behaviors in mice treated with a CCKBR antagonist was reduced.
“Remarkably, the YM022 shows anxiolytic effects with a dose of 3.0 ug/kg, which is 3,000 times lower than the required dosage of current antidepressants,” said Professor He.
“These results indicate that CCKBR is a potential target for depression treatment, and that the selected antagonist, YM022, may be a good anti-depressant candidate due to its extremely small effective dose. This paves the way for targeted drug development that specifically addresses the abnormalities observed in the basolateral amygdala.”
Next, the research team will focus on the precise mechanisms and potential side effects of CCKBR antagonists to set the stage for future clinical trials involving human subjects.
Provided by City University of Hong Kong
Using a neuromonitoring platform to improve care for traumatic brain injuries

UC’s neurocritical care team monitors metrics like blood flow, pressure, oxygen and glucose levels in the brain in real time and monitors trends and spikes over longer periods of time for patients with severe traumatic brain injuries. Credit: Andrew Higley/UC Marketing + Brand. Tracking heart rate, blood pressure and oxygen levels is a standard practice to give doctors valuable information on patients’ heart and lung health over time and guide treatment decisions.
The University of Cincinnati Gardner Neuroscience Institute’s Brandon Foreman, MD, said there is a need for similar tracking of data on patients’ brain health for those with severe brain injuries. UC experts have pioneered a comprehensive platform for this practice known as multimodal neuromonitoring (MNM), despite a lack of standard practice among others in the field.
Foreman, along with an international panel of colleagues and experts in MNM, recently published survey results in the journal Critical Care Medicine identifying areas of consensus and needs for further research to develop a standard practice for comprehensively monitoring brain health in the intensive care unit . MNM basics
Foreman said measurements like blood flow, pressure, oxygen and glucose levels in the brain give actionable information when treating patients with severe brain trauma.
“We can give people oxygen, we can give people glucose, we can reduce pressure inside the skull,” said Foreman, associate professor of neurology and associate director of neurocritical care research in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine and a UC Health physician. “Multimodal brain monitoring is all about getting those measurements that give us the same comprehensive view of the brain that we normally get from the vital signs that help monitor the heart and lungs.”
Many of these brain metrics require neurosurgeons to place advanced catheters in patients’ brains, so MNM typically only occurs in academic institutions where there are available technologies and surgeons with this expertise.
At UC, MNM efforts are focused on patients with traumatic brain injuries. Led by Laura Ngwenya, MD, director of the UCGNI Neurotrauma Center, neurosurgeons are trained to place brain monitors directly into the brain at bedside early after patients come to the intensive care unit. The neurocritical team has developed a unique and comprehensive system where all of the brain measurements are then aggregated into a single platform to help inform their medical decisions.
“We decided if we’re going to put something in your head, we probably should do it in the most comprehensive way possible because this is not a benign thing to do,” Foreman said. “There’s no one else that monitors the brain to the degree that we do. There’s nowhere else that does this.”
Foreman said he can remotely monitor patient data on the platform from anywhere at any time, and the platform also helps the team track changes over longer periods of time.
“If a patient is in the ICU at 2 a.m., I can pull up everything that’s happening in real time and help the team there at the bedside make a decision,” he said. “We also implemented this strategy so over time we see how the brain injury is evolving—how this person’s brain is really working or not working. That helps direct the team in terms of the things that they want to do to address problems at the bedside.” Next steps
Foreman said survey results from 35 experts in MNM across the country found agreement that the practice of MNM can help care teams make better treatment decisions, including choosing not to intervene when doing so could be harmful. Having more comprehensive data allows for personalized care based on each patient’s individual needs.
The experts agreed MNM is best used for the “sickest of the sick” patients, like those with traumatic brain injuries and severe strokes, but there is currently not enough data to determine other patient populations that may benefit from MNM. Most survey participants also agreed that MNM is a distinct specialty that will require specific training and expertise rather than just involving buying a high-tech piece of equipment and plugging it in.
“I think there’s a movement toward this being its own entity, something that you would train on as a separate skill, that you’d deploy as a separate line of service,” Foreman said.
All of the data and best equipment in the world is worthless if it doesn’t lead to better treatment for patients, so Foreman said an important step of standardizing MNM will be to prove its usefulness. But how MNM is used depends on how the data is interpreted by experts in order to provide clinical care teams with the right information for decision making. Foreman and the UC neurocritical care team’s pioneering approach has now been adopted at several academic centers across the US.
This year, Rudy Luna, MD, a first-year neurology resident at UC, presented research at the American Academy of Neurology conference that found “a significant shift toward improvement in clinical outcome” for patients with daily reporting and interpretation of MNM data. Foreman said the team is writing a more comprehensive analysis that he hopes to publish in the coming months that confirms the usefulness of MNM to improve the outcome of patients at UC with severe traumatic brain injuries.
Provided by University of Cincinnati
Brain Pathway for Rapid Threat Response Found

Summary: A new study identifies a brain pathway responsible for rapid-threat detection, inspired by the “boiling frog” metaphor. Fruit flies were used as a model to understand how animals respond to rapid environmental changes.
The study reveals that flies exhibit escape behavior in response to rapid temperature changes, guided by a specific circuit in their brain.
These findings shed light on the significance of short-lived neural responses and suggest that the ability to anticipate and respond to swift changes is crucial for survival.
Key Facts:
> The study used fruit flies, with a fraction of the neurons humans have, as a model to investigate rapid-threat detection.
Flies respond with escape behavior when exposed to rapid temperature changes but do not react to slow changes.
A circuit in the fly brain responds only to rapid temperature change, influencing escape responses and survival.
Source: Northwestern University
We’ve all heard it: Put a frog in boiling water, and it will jump out. But put the same frog in lukewarm water and heat it gradually, and you’ll cook the frog. Often used as a metaphor for the unhurried and stubborn response many have to a slowly rising threat, the mechanisms underlying the urban myth have become a subject of scientific fascination.
This parable seems to have inspired new Northwestern University research, which identified a brain pathway responsible for rapid-threat detection. Indeed, when the researchers experimentally inactivated those neurons, flies escaped less promptly. Credit: Neuroscience News “Animals are more likely to react to rapid rather than slow environmental change,” said lead author Marco Gallio, associate professor of neurobiology in Northwestern’s Weinberg College of Arts and Sciences. “In the present study, we identify a brain circuit in fruit flies that selectively responds to rapid thermal change, priming behavior for escape.”
The findings were published last week in the journal Nature Communications.
Gallio generally uses fruit flies to understand sensory circuits and the ways they create perceptions of the physical world. Using the fly as a model, the lab studies basic decision-making principles in an animal that has a fraction of the number of neurons (100,000) than humans have (roughly 100 billion). As a well-studied model organism for biological research, flies also are useful subjects because of the pre-existing tools to study fly neurons and behavior.
“There are often two types of responses to external stimuli in the brain: Some neurons respond to a stimulus like light or temperature with very persistent activity,” Gallio said.
“Other neurons fire just at the beginning, like when a light turns on, and then their activity is gone. We’ve always wondered what the significance of these short-lived responses is.”
In visual stimuli, brains are wired to notice a large contrast between light and dark. Gallio said that the response intuitively also makes sense for the sense of touch: You don’t think about pressure when your hand is resting on a surface. Run your hand over something new, however, and you will detect subtle changes in texture. Gallio’s team wanted to see if the same was true for the sense of temperature.
To explore how flies respond to rapid change, the team used a high-resolution camera to observe flies navigating different temperature environments. When flies encounter a rapid heat front, they always produce a U-turn away from it.
The lab found flies always responded in cases of rapid temperature change, but not for slow change.
The team also identified a circuit in the fly brain that responds only to rapid temperature change (more than 0.2 degrees Celsius per second). Much like light-ON cells of the visual system, these neurons fired at the beginning of rapid heating and then went quiet.
“Our hypothesis was that these heat-ON responses may indeed correlate with the rate of temperature change,” said Jenna Jouandet, the study’s first author and a Ph.D. student in the Gallio Lab. “And therefore, may allow flies to anticipate dangerous thermal conditions and prepare to escape.”
Indeed, when the researchers experimentally inactivated those neurons, flies escaped less promptly.
To better understand how the activity of these neurons may be important for the behavior of the fly, the researchers collaborated with William Kath, applied math professor at Northwestern and deputy director of the new National Institute for Theory and Mathematics in Biology.
Applied math Ph.D. student Richard Suhendra built a small computer model with two antennae and two wheels to demonstrate how adding a neuron that anticipates dangerous heat could improve the flexibility of the vehicle response. (Play with the model through a simple game on the Gallio Lab webpage .)
“The neurons that we initially discovered take input from the thermosensory neurons on the antennae and carry information to the higher brain,” Gallio said. “Flies are a great model to map brain circuits in that we were able to reconstruct the full circuit from sensory neurons all the way down to the centers that produce movement.”
Gallio explained that rapid changes are nearly always dangerous for a small fly.
“If the temperature is changing by half a degree per second — which is not that much — within 30 or 40 seconds, that fly could be dead,” Gallio said. “This system is an alarm bell that rings to prime an animal’s behavior for escape. We see the fly escape.”
Gallio hypothesizes that the results are broadly generalizable, especially because he sees it play out in humans, whether someone is entering a room that’s a different temperature or getting into a hot shower. He said these neurons seem to be able to sense something others do not — they seem to be able to anticipate the future. Funding: The research reported in this publication was supported by the National Institutes of Health (grants R01NS086859, R21EY031849 and R21NS130554), a Pew Scholars Program in the Biomedical Sciences and a McKnight Technological Innovations in Neuroscience Awards. The research was supported in part through the computational resources provided for the Quest high performance computing facility at Northwestern University, which is jointly supported by the Office of the Provost, the Office for Research and Northwestern University Information Technology; the Training Grant in Circadian and Sleep […]
Learn How to Be Happy Alone With These 16 Expert Tips

Video player poster image Whether you lead a solitary life or are simply feeling lonely, figuring out how to be happy alone goes a long way toward bolstering mental health. Even though everyone gets lonely sometimes, learning how to appreciate some me-time can take your days from okay to great. But, it’s important to remember that it’s okay to not be okay sometimes.
Meet the Experts: Dana Klisanin, Ph.D. , psychologist and CEO of Evolutionary Guidance Media R&D; Patrick Porter, Ph.D., neuroscience expert and founder of BrainTap ; Jeff Temple, Ph.D. , licensed psychologist and founding director of the Center for Violence Prevention at University of Texas Medical Branch; Brad Thomas, Ph.D. , NYC-based therapist and licensed clinical psychologist; Jeff Yoo, L.M.F.T. at Moment of Clarity Mental Health Center .
“Being happy in life and with self begins with our choices as adults and how we perceive our contributions to the world,” says Jeff Yoo, L.M.F.T. at Moment of Clarity Mental Health Center . Ahead, mental health experts explain tips for being happy alone, how to ask for help when you need it, and what it is to be alone versus feeling lonely. Alone vs. lonely
Being alone is a physical state where you are not in the company of others, whereas feeling lonely is an emotional state of feeling isolated, regardless of whether you’re physically alone or with others, says Patrick Porter, Ph.D., neuroscience expert and founder of BrainTap . “One can be alone without feeling lonely, and conversely, one can feel lonely in a crowd,” he says. Understanding this difference is crucial, as it impacts how you approach your own mental and emotional well-being.
Aloneness can be a neutral state, says Brad Thomas, Ph.D. , NYC-based therapist and licensed clinical psychologist. “People can be happy being by themselves, and there are other times when they desire to be emotionally connected to others,” he says. Still, we want to keep our eye on these feelings to determine to what extent we are feeling loneliness and how distressing it can be, he adds.
Aloneness can be an enriching experience—giving us the chance to learn more about ourselves and the world around us, says Dana Klisanin, Ph.D. , psychologist and CEO of Evolutionary Guidance Media R&D. “Loneliness can arise when we feel that we have no one to share our experiences with or no one who understands us,” she says. How to be happy alone short-term
In our society, there is a stigma around being alone or feeling lonely that we can flip on its head, says Thomas. “We can take some of the power away from that stigmatization and look at it healthier,” he says. There are many advantages to being alone, like having the time to focus on yourself. “That is taking the power in your hands and understanding what you desire, independent of other people’s reactions,” Thomas explains.
When it comes to things you can start doing right now to be happy alone, experts suggest: Question the narrative
First of all, ask yourself if you are really “unhappy alone” or have you been taught to think you should be unhappy if you are alone, says Klisanin. “Our narratives define us. If your ‘story’ isn’t working, you have permission to change it,” she says. Take a moment for mindfulness
Spend five to 10 minutes each day meditating to center yourself. Focus on your breathing and the present moment, suggests Porter. Accepting solitude as an opportunity rather than a hindrance can shift one’s perspective, adds Klisanin. Get active
Even a 20-minute walk outside can boost endorphin levels, elevating your mood and well-being, says Porter. “Avoid sitting for prolonged periods; our research shows that just two hours of sitting can reduce oxygen in the brain by 10%. Make it a point to get up and move around,” he adds. Take a tech break
Take a break from being on your computer and technology when you can, says Thomas. “Putting away your devices allows you to check in with yourself to see what you desire.” Engage in creative activities
These can be therapeutic and stimulate your brain, says Porter. Whether it’s painting, journaling , gardening , or learning to play a musical instrument, a new hobby can provide a sense of fulfillment and self-expression, says Klisanin. Get inspired
Watching short motivational videos or reading inspirational quotes can uplift your spirits, says Porter—so time to watch some Ted Talks! Practice self-care and grounding
Pamper yourself, whether it’s taking a warm bath or enjoying your favorite healthy snack, says Porter. “Additionally, spend some time outside grounding yourself to release excess energy. Walk on grass barefoot or with leather shoes to achieve a zero point energy state; our research indicates that the average person has up to three volts of disruptive energy flowing through their body,” he adds. How to be happy alone long-term
The more you practice and get into the habit of being alone, the more you’ll understand your path of self-understanding and discovery, says Thomas. With time, “you’ll be able to tolerate so much more ambiguity because you know yourself well,” he says. Experts explain the best tips for figuring out how to be happy alone long-term. Build a routine
A stable routine helps your brain recognize patterns, making you feel more in control and happier, says Porter. “Incorporate a consistent sleep schedule into this routine. Going to bed and waking up at the same time helps regulate your body’s clock and improves your overall well-being,” he says. Set goals
Whether they are short- or long-term, goals give you a sense of purpose, says Porter. “Challenge yourself to tackle new things; this keeps your mind sharp and invokes the beginner’s mindset, which is fantastic for discovering happiness,” he says. Keep your mind sharp
Learning something new is not just rewarding; it enhances brain function, says Porter. “Continuously challenging yourself with new skills not only boosts your self-esteem but also keeps your cognitive abilities in […]
Can gene expression predict if a brain tumor is likely to grow back?

Credit: Anna Shvets from Pexels Doctors often prescribe radiation along with surgery to treat a brain tumor called meningioma that originates in the protective membranes surrounding the brain. But side effects from radiation can be serious, including memory loss and cognitive decline, so it’s important to know which patients really need it.
Now, researchers at UC San Francisco and Northwestern Medicine, in collaboration with 10 other medical centers, have found a highly accurate way to predict the best treatment for patients based on patterns of gene expression—which genes are turned on and off—in their tumors.
Screening tumors using this new approach could change the course of treatment for nearly 1 in 3 people with meningioma, the most common form of brain tumor diagnosed in 42,000 Americans each year. Unlike other brain tumors , meningiomas occur most often in female, Black and elderly patients .
In a paper appearing in Nature Medicine , the team concluded that just 1 in 5 patients with low-grade tumors (those less likely to regrow) may need radiation , while around 2 in 5 with higher-grade tumors may be better off without radiation, based on the results of the new gene-expression test.
“There’s been a lot of controversy in the field in terms of who should receive radiotherapy and who shouldn’t,” said David Raleigh, MD, Ph.D., a radiation oncologist in the UCSF Brain Tumor Center and a senior author of the study, along with Stephen Magill, MD, Ph.D., assistant professor of neurological surgery at Northwestern University Feinberg School of Medicine. “Our biomarker takes the guessing game out of this and shows us which patients are likely to benefit from radiotherapy and which may get toxicity and possibly no benefit from radiation.” From microscopes to molecules
Because meningiomas grow slowly, a patient may be unaware of their tumor until they start to experience neurological symptoms like numbness, vision loss or personality changes. There are no pharmaceutical treatments, so doctors rely on surgery to remove the tumor and radiation to prevent it from growing back. Doctors treat these tumors based on guidance from the World Health Organization, which stages them according to severity.
Pathologists currently classify meningiomas by looking at them under a microscope for features that indicate whether they may grow back, a system that is very good but not perfect. Patients with Grade 1 tumors don’t usually receive radiation treatment if their tumors can be removed completely during surgery. Yet approximately 20% of the time, the tumors recur.
Those with Grade 2 and 3 tumors, which are much more aggressive and more likely to grow back after surgery, are often treated with radiation after surgery. It has been unclear how many of these patients, particularly those with Grade 2 tumors, actually need radiation treatment.
Raleigh, along with Magill and lead author William Chen, MD, decided to look at classifying tumors according to which of their genes are turned on and off, thereby offering clues to how aggressive they might be.
“Gene-expression tests like this, that analyze a small number of genes at a time, are widely available for breast, prostate and some other cancers, and they’ve proven to be a very accurate and inexpensive alternative to other types of tests,” said Chen. How to turn guesses into answers
Raleigh and Chen and their multidisciplinary team suspected that gene expression could more accurately point out the patients who would be helped by radiotherapy. Using samples from 1,856 meningioma patients at 12 medical centers in the U.S., Europe and Hong Kong, Raleigh’s team came up with a set of 34 genes whose gene expression patterns had the potential to predict whether a tumor would return.
One-fifth of the Grade 1 tumors—the same number that grow back after surgery—expressed the patterns that Raleigh’s team found could predict a tumor’s regrowth. This fraction of patients may benefit from radiation. The researchers also found that two-fifths of patients with Grade 2 and 3 tumors did not have a recurrence, and this, too, could be predicted by the tumor’s gene expression.
“When to proceed with additional surgery, radiotherapy or simply to observe a small residual meningioma is not always clear,” said Magill. “This test adds information that can let us tailor our surgical and radiation approach to provide the best outcome for each patient and maximize both quality and quantity of life.”
The team’s next step is to test the approach in two clinical trials currently being developed.
More information: William C. Chen et al, Targeted gene expression profiling predicts meningioma outcomes and radiotherapy responses, Nature Medicine (2023). DOI: 10.1038/s41591-023-02586-z
Provided by University of California, San Francisco
New study reveals potential link between oral contraceptives and riskier behaviors in women

Advertisement
A new study has revealed a potential link between oral contraceptive (OC) use and alterations in the brain structure of women that may influence emotions, anxiety, fear, decision-making and impulse control.
The study, published in the journal Frontiers in Endocrinology , examined 139 women aged 23 to 35 who were either currently using OC, had stopped taking them or had never used them, along with 41 men for comparison. The research found that those on OC had thinner regions in their frontal lobe compared to those who had never taken or had stopped.
According to Alexandra Brouillard, the lead author and researcher at the Université du Québec à Montréal , the thinning in the ventromedial prefrontal cortex, a brain region associated with emotion regulation, suggests that women taking OCs might experience lower inhibitions, take more risks and exhibit reduced fear responses.
The researchers used MRIs to analyze gray matter volume and cortical thickness in brain regions associated with information processing, emotion regulation, memory retention and decision-making. The research found that women generally have more gray matter in parts of the brain linked to learning and self-control than men.
However, women currently using OCs experience thinning in the brain region responsible for processing risk and fear. This reduction in thickness may lead to issues in self-control, social behavior and impulsiveness, potentially affecting the amygdala, which is responsible for regulating emotions. (Related: Birth control pills can raise the risk of depression by up to 80% .)
Despite this, Brouillard warned against making direct connections between these brain changes and riskier behaviors, stressing the need for further investigation into potential behavioral implications.
“The objective of our work is not to counter the use of COCs, but it is important to be aware that the pill can have an effect on the brain . Our aim is to increase scientific interest in women’s health and raise awareness about the early prescription of COCs and brain development, a highly unknown topic,” explained Brouillard. Hidden dangers of birth control pills doctors won’t tell you
In a blog post written by certified wellness health coach, nutritional consultant and detox specialist Sarah Ding for her website Juicing-for-Health.com , she discussed the hidden dangers of birth control pills that doctors don’t want their patients to know.
Ding wrote that contrary to the popular belief that birth control pills are inherently safe, the reality is quite different.
“Many women take birth control pills without being aware of the serious health implications of these pills. Doctors prescribe pills to young ladies from the age of 16, some to help them regulate their menstruation, and reduce pre-menstruation symptoms, acne, and other hormonal problems. Often there is no question about their lifestyle and diet, much less the underlying reasons why these young ladies have this problem in the first place!”
Birth control pills come with a range of side effects that are often downplayed during medical consultations, with the only obligatory check being a blood pressure measurement.
Despite the convenience they offer in preventing pregnancy, immediate side effects akin to those experienced during pregnancy, such as weight gain, breast tenderness, mood swings, nausea and a decrease in libido, can catch many women off guard.
However, these initial effects are just the tip of the iceberg.
Long-term use of contraceptives has been linked to a myriad of more serious side effects, including yeast overgrowth and infection, irregular bleeding, missed periods, elevated blood pressure, spotting between periods, no ovulation, fluid retention and lower bone density.
Shockingly, the list extends to potentially severe conditions like an increased risk of liver and gallbladder diseases and the development of liver tumors and gallstones.
Ding also shared how she suffered from the adverse effects of these contraceptives. “I wish my doctor had told me about the dangers of birth control pills when I started taking them decades ago. Until today, I still suffer from the damage that birth control pills have caused to my liver.”
Learn more about the adverse side effects of contraceptives at DangerousMedicine.com .
Watch the video below to learn more about the dangerous side effects of birth control . This is a modal window.
No compatible source was found for this media.
This video is from the Tammy Cuthbert Garcia channel on Brighteon.com . More related stories:
Birth control pills found to increase the likelihood of ischemic stroke in women .
Birth control vaccine that may leave women permanently sterile now in clinical trials .
Canadian government to spend $4.3M on abortions and birth control to manage indigenous populations .
FDA approves first OTC birth control pill in the U.S. despite concerns about data on its proper use .
Washington state spends millions of taxpayer dollars buying three-year supply of abortion pills . Sources include: NYPost.com DailyMail.co.uk Juicing-for-Health.com
What makes us human? Scientists uncover clues behind brain evolution

Graduate student Emre Caglayan (left) and lead scientist Genevieve Konopka stand in their lab at the Pickens Biomedical Building on the campus of UT Southwestern, Tuesday, Oct. 17, 2023, in Dallas. (ElÃas Valverde II/The Dallas Morning News/TNS) ElÃas Valverde II
The human brain is three times bigger than a chimp’s and more spherical than a Neanderthal’s. Within a maze of bumps and grooves, neurons converse in distinct patterns that give humans unique cognitive abilities.
Scientists haven’t fully deciphered those patterns. But researchers at UT Southwestern Medical Center are determined to solve the molecular mystery of what makes us human.
In a study published in the journal Nature, they compared brain cell types and activities among humans, chimpanzees and rhesus monkeys. Human brains had more of a kind of cell that may help them adapt based on new experience and heal from injury. Certain human neurons also had more of a gene that affects language development.
Genevieve Konopka, whose lab ran the study, has long investigated the molecular mechanisms that lead to brain disease. Understanding the human brain’s inner workings, she said, may help researchers develop therapies to treat conditions like Alzheimer’s and schizophrenia.
The brain’s support crew
Our brains set us apart from other primates. Humans communicate in languages that chimps can’t speak and devise systems of government and religion that don’t exist in the animal kingdom.
Though scientists have compared the cell types and genes in the brains of humans and other primates, they still lack a complete knowledge of how the human brain came to be over millions of years of evolution.
Konopka’s inquiry into brain evolution stemmed from her study of brain disease. In 2019, she compared brain tissue in people with and without schizophrenia and found differences in cells called oligodendrocytes. These cells act like the brain’s support crew, producing insulation that wraps around neurons and helps them send signals faster.
Konopka also saw a difference in oligodendrocytes between human and chimp brains. She realized this support crew could play an important role in both brain disease and human brain evolution.
Konopka wasn’t able to pursue her research further because of technological limits. But in recent years brain studies got a boost from single-cell technology, which allows scientists to capture each cell in a piece of brain tissue and examine the activity of different genes.
Using this technology, Konopka focused on a part of the brain located in what’s called the posterior cingulate cortex. This part is implicated in schizophrenia and is associated with the way we think about ourselves. Konopka said her lab is the first to apply single-cell technology to this region of the brain.
Her lab compared oligodendrocyte amounts and gene activity in human, chimp and rhesus monkey brain tissue. In another experiment, they compared human DNA with genetic information from two ancient human populations: Neanderthals and Denisovans.
Waiting in the wings
Konopka thought her lab would find more oligodendrocytes in human brain tissue compared to that of chimps and rhesus monkeys.
Instead, she found a human-specific increase and gene activity changes in pre-oligodendrocytes: brain cells that haven’t yet evolved to perform their mature functions.
At first, Konopka thought it was a mistake. But after confirming the result, she said, it began to make sense. More pre-oligodendrocytes may help the human brain adapt in response to change or injury, she explained. Having more of these cells may allow us to continue learning into adulthood.
Her lab also found that a gene called FOXP2, which is associated with language development in humans, had higher expression in two types of human neurons. Konopka said the human-specific increase could contribute to the language of human thoughts.
The lab also identified hundreds of genes that may function differently in humans, Neanderthals and Denisovans. These differences shed light on how the human brain evolved over the last 300,000 to 500,000 years, Konopka said.
Konopka’s research adds to the field by not only investigating which genes exist in different brain cells, but also how active they are, according to Doug Broadfield, an associate professor of cell biology at the University of Miami Miller School of Medicine.
“What’s new about this study is that it’s … created a new field of brain evolution,” said Broadfield, who was not involved with the research, “where instead of focusing on the structure of the brain, now we can look at the genetic activity of the brain.”
Konopka hopes to next use single-cell technology to examine brain tissue from people with brain disorders, including schizophrenia.
“We just wanted to set the table, if you will, for future studies looking at brain disease,” she said.
Adithi Ramakrishnan is a science reporting fellow at The Dallas Morning News. Her fellowship is supported by the University of Texas at Dallas. The News makes all editorial decisions.
Can Electronic Brain Training Games Relieve “Brain Fog” from Long Covid?
Media Contact:
Sophia Friesen
Manager, Science Communications, University of Utah Health
sophia.friesen@hsc.utah.edu
A collection of cognitive symptoms referred to as “brain fog” occur in up to 10-30% of people who have been infected with the virus that causes COVID-19. But currently there are no treatments for the confusion, fuzzy thinking, and forgetfulness that can last for weeks or months, sometimes interfering with daily life.
Researchers at University of Utah Health are testing whether a non-invasive “brain training” tool that resembles a video game can alleviate these symptoms. They are recruiting up to 200 participants aged 18 and older who feel their cognitive function has worsened after having COVID-19. Clinical trial participants will try a potential treatment in the convenience of their own home for a 10-week study period with a follow-up visit after 90 days. Study coaches will provide support through virtual visits.
The trial, called RECOVER-NEURO, is part of the National Institutes of Health Researching COVID to Enhance Recovery (RECOVER) Initiative . Call 801-230-2285 to learn more or enroll.
Study participants will be offered an online intervention called BrainHQ. Although it may look like a game, it is more like a mental workout, according to Sarah Shizuko Morimoto, PsyD , the principal investigator of RECOVER-NEURO and an associate professor of population health sciences at U of U Health. BrainHQ is a suite of computerized games/exercises that train different cognitive functions such as attention, memory, processing speed, and navigation. The games provide rewards for correct answers, and participants can track their learning curves. As the participant practices, the games adapt to their individual abilities. And as they improve, the games get harder, maximizing the brain’s learning potential.
Cognitive computerized remediation technologies like BrainHQ have already shown promise. Preliminary research led by Morimoto, who develops digital interventions for mental health, revealed that similar activities enhance cognitive function and alleviate symptoms in older adults with treatment-resistant depression. Sarah Shizuko Morimoto, PsyD, is the principal investigator of the RECOVER-NEURO study. Some study participants will test if adding a second non-invasive method increases effectiveness of BrainHQ. The interventions include: BrainHQ: Participants will complete online BrainHQ activities designed to improve memory, attention, and brain processing speed—the time it takes to understand and respond to information.
BrainHQ and PASC Cognitive Recovery (PASC CoRe): Participants in this intervention group will meet virtually with trained study staff to plan and manage personal goals, learn mindfulness skills to focus attention on goal-oriented tasks, and develop strategies to manage mental tiredness.
BrainHQ and Transcranial Direct Current Stimulation (tDCS): tDCS is a safe, non-invasive form of brain stimulation that may “boost” cognitive training outcomes and brain health. Participants in this intervention group will wear a headset connected to the tDCS device while they complete the cognitive activities. The tDCS device will be programmed to deliver a mild electrical current to specific parts of the brain to increase activity during BrainHQ activities.
Non-invasive methods such as these are attractive because they avoid risks associated with medication-based symptom management, Morimoto says. “Over the last year, experts across the country have been meeting to evaluate every suggested treatment for long COVID,” she says. The study’s design was developed with input from experts in neurology, immunology, rehabilitation, psychology, and neuroscience, in collaboration with long COVID patient advocates.
“These experts have decided that the best interventions to test are the ones that are both safe and have data to support their use,” Morimoto says. “We are excited to be able to offer this cutting-edge treatment to patients suffering from long COVID at no cost.”
She adds that the clinical trial may reveal a treatment and provide insights into underlying causes of brain fog. Data captured from the clinical trial could pinpoint which cognitive functions become impaired, identify neural circuits responsible for these deficits, and assess the potential to reshape these circuits for improving cognitive capabilities. That knowledge can be used as the basis for further research, ultimately leading to better treatments and preventive measures.
Find additional RECOVER clinical trials for long COVID at trials.recovercovid.org .
# # #
About RECOVER : The National Institutes of Health Researching COVID to Enhance Recovery (NIH RECOVER) Initiative is a $1.15 billion effort, including support through the American Rescue Plan Act of 2021, that seeks to identify how people recuperate from COVID-19 who are at risk for developing post-acute sequelae of SARS-CoV-2 (PASC). Researchers are also working with patients, clinicians, and communities across the United States to identify strategies to prevent and treat the long-term effects of COVID-19, including long COVID. For more information, please visit recovercovid.org . About University of Utah Health
University of Utah Health is the state’s only academic health care system, providing leading-edge and compassionate care for a referral area that encompasses 10 percent of the US, including Idaho, Wyoming, Montana, and much of Nevada. A hub for health sciences research and education in the region, U of U Health has a $522 million research enterprise and trains the majority of Utah’s physicians, and more than 1,670 scientists and 1,460 health care providers each year at its Colleges of Health, Nursing, and Pharmacy and Schools of Dentistry and Medicine. With more than 20,000 employees, the system includes 12 community clinics and five hospitals: University Hospital, Huntsman Mental Health Institute, Huntsman Cancer Hospital, University Orthopaedic Center, and the Craig H. Neilsen Rehabilitation Hospital. For 14 straight years, U of U Health has ranked among the top 10 US academic medical centers in the rigorous Vizient Quality and Accountability Study.
Online brain training games seen to improve cognition in small MS trial
PhD student used BrainHQ program in thesis work on computerized training Share this article:
Share article via email A person is shown talking with a doctor who’s sitting at a desk and entering information into a computer. The use of a computer-based program called BrainHQ led to significantly improved scores on cognitive tests among people with multiple sclerosis (MS), according to data from a small clinical trial in Nebraska.
The study was led by Samantha Jack, PhD, as part of work she did as a graduate student at the University of Nebraska. Jack published the findings in a PhD thesis titled “ Effect of Computerized Cognitive Training in Persons with Multiple Sclerosis .”
“With the continued development of computerized cognitive testing and computerized cognitive training, clinicians hopefully will start incorporating cognitive performance into their regular discussions with patients,” Jack wrote.
“As the field of MS continues to evolve, my hope is that these convenient options will help make cognition a priority,” she added.
Recommended Reading Benefits seen for patients using online brain training games
Cognitive difficulties, such as trouble with memory and attention, are a common symptom of MS . The mechanisms leading to cognitive impairment in MS patients are not fully understood, but such problems are believed to arise primarily due to lesions and shrinkage of specific brain areas.
A number of strategies have been shown to help ease or reverse cognitive decline in MS patients. These include cognitive rehabilitation programs, exercise, and medications.
BrainHQ is a computer-based system of games that are designed to exercise cognitive faculties. A free version is available to try online, or consumers can subscribe for greater access. An annual subscription is $96 per person, or a monthly subscription is available for $14.
To fulfill some of her degree requirements, Jack, along with colleagues, conducted a small clinical trial to test whether the games in BrainHQ could help with cognitive issues in people with MS.
The study included 52 adults with relapsing-remitting MS , who were mostly white and female individuals, had mild to moderate disability, and had been living with MS for a mean of 8.3 years.
The participants were divided into two groups. One group had training with the BrainHQ system for 30 minutes three times weekly for six weeks, using games designed to improve attention, processing speed, and memory. The other patients played casual online games through the BrainHQ portal at the same time schedule.
Before and after the intervention, the participants underwent an assessment of cognitive function called the Brief International Cognitive Assessment for MS, or BICAMS.
This test includes three measures of cognition. The Symbol Digit Modalities Test (SDMT) assesses attention and processing speed, while the Brief Visuospatial Memory Test – Revised (BVMT-R) tests memory. The California Verbal Learning Test 2nd Edition (CVLT-II) evaluates both verbal learning and memory.
The results showed that BICAMS scores improved significantly more for patients who underwent the BrainHQ training, compared with the control group that played casual games. This study provides evidence that computerized cognitive training with BrainHQ is a valuable option for [people with] MS suffering from cognitive decline. A statistically significant improvement with BrainHQ was seen for all three subscores on the BICAMS. A particularly strong effect was seen for the CVLT-II, with an average improvement of more than nine points in the BrainHQ group, compared with less than one point in the control group.
“This study provides evidence that computerized cognitive training with BrainHQ is a valuable option for [people with] MS suffering from cognitive decline,” Jack concluded.
She added that this type of computer-based intervention “is convenient for the patient because they can do it at home when they have time and not at a specific time with a neuropsychologist.”
Jack noted, as a study limitation, that there were “very few males and very few non-Caucasian subjects.”
“While MS is more common in Caucasians and females, future studies should try to enroll a more diverse population. Furthermore, future studies should include subjects over age 60 to determine if the BrainHQ program can improve their cognitive functioning,” the researcher wrote.
The BrainHQ system is sold by Posit Science, which was not involved in this study. Henry Mahncke, PhD, the company’s CEO, said “these are very exciting results from independent researchers,” in a Posit Science press release .
“We hope this spurs not just further research, but targeted chronic care improvement programs at leading medical centers and health plans to help patients in need,” Mahncke said.
Print This Page
Researchers highlight benefits of sharing human brain data
Credit: Unsplash/CC0 Public Domain In recent years, the scientific community has seen a push for more findable, accessible, interoperable, and reusable (FAIR) neurophysiology data sharing. While certain measures have been put in place by institutions such as the National Institute of Health (NIH) to promote more FAIR data sharing, some researchers remain hesitant and unwilling to share their data beyond minimum requirements due to multiple disincentives.
In a new Neuron article , a team of researchers, led by co-authors Dr. Vasiliki Rahimzadeh, assistant professor at the Center for Medical Ethics and Health Policy at Baylor College of Medicine, and Dr. Kathryn Maxson Jones, assistant professor of history of technology at Purdue University and formerly a Senior Research Assistant in the Center for Medical Ethics and Health Policy at Baylor during the time of the study, profile three successful instances of data sharing from the NIH BRAIN Initiative Research Opportunities in Humans (ROH) Consortium to highlight the benefits of FAIR data sharing.
“This group is focused on how to maximize the scientific utility of human neuronal data through broad and secure data sharing,” explains Rahimzadeh. “While there has been a lot of attention paid to scientific benefits of data sharing, such as researchers being able to learn from others and expand their own work, far less has been paid to the professional and other social benefits . These value propositions are important for incentivizing researchers to share data more often beyond what is required as a condition of their funding.”
The paper showcases examples of successful data sharing from research groups at the University of Pennsylvania, Cedars-Sinai Medical Center, and Harvard Medical School and Massachusetts General Hospital involving intracranial electrophysiology data from patients. When shared, the data in question was de-identified to protect patient privacy, reformatted into standardized file types and uploaded to institutional or NIH archival databases, where it has been and is being reused for new research, education, training and tool development opportunities.
Rahimzadeh said that by sharing data, the research groups discussed in the paper were able to not only open new doors for collaboration with other groups, but to also support replicability studies that overall enhance scientific rigor.
“The benefits to users include expanding both the diversity and volume of datasets available for research and being able to combine multiple datasets together to find new associations or conduct subgroup analyses that previously might have been infeasible,” she said. “For producers of data, there are benefits of supporting new scientific collaborations and contributing to professional development of trainees who will continue a culture of data sharing.”
Rahimzadeh added that by sharing their data, investigators increase the visibility of their labs, reduce redundancies in similar research studies and benefit from others identifying errors in code or analysis that might otherwise have remained undetected.
“Many pressing research questions about the brain and nervous systems today require analyses of data that are more voluminous and multi-faceted than any single laboratory can reasonably be expected to produce. This makes sharing data all the more important. Additionally, sharing data has had tangible benefits in other fields of life science, such as genomics,” said Dr. Maxson Jones, the co-lead author on the paper, who is now at Purdue University. “Our paper shows that investing in the labor of sharing data in standardized formats comes with its own payoffs.”
Other authors contributing to the paper include Mary A. Majumder, Michael J. Kahana, Ueli Rutishauser, Jie Zheng, Angelique C. Paulk, Sydney S. Cash, Ziv M. Williams, Michael S. Beauchamp, Jennifer L. Collinger, Nader Pouratian, Amy L. McGuire and Sameer A. Sheth. The authors are affiliated with Baylor College of Medicine, Purdue University, the University of Pennsylvania, Cedars-Sinai Medical Center, Boston Children’s Hospital, Massachusetts General Hospital, the University of Pittsburgh and U.T. Southwestern Medical Center.
Provided by Baylor College of Medicine
Brain implant may enable communication from thoughts alone
A speech prosthetic developed by a collaborative team of Duke neuroscientists, neurosurgeons, and engineers can translate a person’s brain signals into what they’re trying to say.
Appearing Nov. 6 in the journal Nature Communications , the new technology might one day help people unable to talk due to neurological disorders regain the ability to communicate through a brain-computer interface.
“There are many patients who suffer from debilitating motor disorders, like ALS (amyotrophic lateral sclerosis) or locked-in syndrome, that can impair their ability to speak,” said Gregory Cogan, Ph.D., a professor of neurology at Duke University’s School of Medicine and one of the lead researchers involved in the project. “But the current tools available to allow them to communicate are generally very slow and cumbersome.”
Imagine listening to an audiobook at half-speed. That’s the best speech decoding rate currently available, which clocks in at about 78 words per minute. People, however, speak around 150 words per minute.
The lag between spoken and decoded speech rates is partially due the relatively few brain activity sensors that can be fused onto a paper-thin piece of material that lays atop the surface of the brain. Fewer sensors provide less decipherable information to decode.
To improve on past limitations, Cogan teamed up with fellow Duke Institute for Brain Sciences faculty member Jonathan Viventi, Ph.D., whose biomedical engineering lab specializes in making high-density, ultra-thin, and flexible brain sensors.
For this project, Viventi and his team packed an impressive 256 microscopic brain sensors onto a postage stamp-sized piece of flexible, medical-grade plastic. Neurons just a grain of sand apart can have wildly different activity patterns when coordinating speech, so it’s necessary to distinguish signals from neighboring brain cells to help make accurate predictions about intended speech.
After fabricating the new implant, Cogan and Viventi teamed up with several Duke University Hospital neurosurgeons, including Derek Southwell, M.D., Ph.D., Nandan Lad, M.D., Ph.D., and Allan Friedman, M.D., who helped recruit four patients to test the implants. The experiment required the researchers to place the device temporarily in patients who were undergoing brain surgery for some other condition, such as treating Parkinson’s disease or having a tumor removed. Time was limited for Cogan and his team to test drive their device in the OR.
“I like to compare it to a NASCAR pit crew,” Cogan said. “We don’t want to add any extra time to the operating procedure, so we had to be in and out within 15 minutes. As soon as the surgeon and the medical team said ‘Go!’ we rushed into action and the patient performed the task.”
The task was a simple listen-and-repeat activity. Participants heard a series of nonsense words, like “ava,” “kug,” or “vip,” and then spoke each one aloud. The device recorded activity from each patient’s speech motor cortex as it coordinated nearly 100 muscles that move the lips, tongue, jaw, and larynx.
Afterwards, Suseendrakumar Duraivel, the first author of the new report and a biomedical engineering graduate student at Duke, took the neural and speech data from the surgery suite and fed it into a machine learning algorithm to see how accurately it could predict what sound was being made, based only on the brain activity recordings.
For some sounds and participants, like /g/ in the word “gak,” the decoder got it right 84% of the time when it was the first sound in a string of three that made up a given nonsense word.
Accuracy dropped, though, as the decoder parsed out sounds in the middle or at the end of a nonsense word. It also struggled if two sounds were similar, like /p/ and /b/.
Overall, the decoder was accurate 40% of the time. That may seem like a humble test score, but it was quite impressive given that similar brain-to-speech technical feats require hours or days-worth of data to draw from. The speech decoding algorithm Duraivel used, however, was working with only 90 seconds of spoken data from the 15-minute test.
Duraivel and his mentors are excited about making a cordless version of the device with a recent $2.4M grant from the National Institutes of Health.
“We’re now developing the same kind of recording devices, but without any wires,” Cogan said. “You’d be able to move around, and you wouldn’t have to be tied to an electrical outlet, which is really exciting.”
While their work is encouraging, there’s still a long way to go for Viventi and Cogan’s speech prosthetic to hit the shelves anytime soon.
“We’re at the point where it’s still much slower than natural speech,” Viventi said in a recent Duke Magazine piece about the technology, “but you can see the trajectory where you might be able to get there.”
This work was supported by grants from the National Institutes for Health (R01DC019498, UL1TR002553), Department of Defense (W81XWH-21-0538), Klingenstein-Simons Foundation, and an Incubator Award from the Duke Institute for Brain Sciences.
America’s Real Drug Problem: Potato Chips and Donuts Match Cocaine in Addictiveness
Photo by Tim Samuel: https://www.pexels.com/photo/woman-drinking-fresh-lemonade-at-table-with-junk-food-6697265/ Clear Facts:
Fatty and sugar-rich foods, like potato chips and donuts, rival the addictiveness of nicotine and cocaine.
An alarming 14% of adults and 12% of children are addicted to ultra-processed foods.
Ultra-processed foods trigger dopamine levels akin to addictive substances.
Americans might be hooked on more than just their daily cup of joe. According to recent shocking research, the very foods that grace our pantries and fridges are as addictive as some illicit drugs.
Published in the British Medical Journal, the study’s grim findings underscore that roughly 14% of adults and 12% of children are in the grips of ultra-processed foods. These aren’t just any foods. We’re talking about those saturated with refined sugars, artificial flavors, and unhealthy fats – items such as ice cream, potato chips, sugary cereals, and the like. So, what’s the scientific reasoning? These edibles closely mirror the dopamine spike in our brains triggered by hard-hitting substances like nicotine and even alcohol. Not just comparable, but they also surpass the addictiveness of drugs like heroin.
Florida’s addiction specialist Dr. Daniel Bober provided a stark perspective: “What really makes this dangerous is this addiction we have to ultra-processed foods. And these are foods that contain chemicals, emulsifiers, artificial colors. They also contain refined sugars and just the right amount of salt, sugar, and fat to be highly reinforced, which can lead some people to engage in compulsive eating.”
Considering the obesity epidemic, it’s no wonder experts are drawing parallels between the hazardous nature of these foods and illegal narcotics such as cocaine.
Bober drives the point home: “We want a hit, and we want it fast. Whether it’s from cocaine, food, shopping, it all has one thing in common. And that is using compulsive behavior to deal with uncomfortable feelings like loneliness, depression, isolation. It’s something we need to look at because it’s part of our culture.”
The authors of the study echoed this sentiment, noting: “Ultra-processed foods high in refined carbohydrates and added fats are highly rewarding, appealing, and consumed compulsively and may be addictive. Understanding of these foods as addictive could lead to novel approaches in the realm of social justice, clinical care, and policy approaches.”
We want to know what you think! Share your thoughts in the comments below.
Source
Feeling Lonely? Experts Share 16 Tips on How to Be Happy Alone

16 Expert Tips on How to Be Happy Alonekate_sept2004 – Getty Images [table-of-contents] stripped
Whether you lead a solitary life or are simply feeling lonely, figuring out how to be happy alone goes a long way toward bolstering mental health. Even though everyone gets lonely sometimes, learning how to appreciate some me-time can take your days from okay to great. But, it’s important to remember that it’s okay to not be okay sometimes.
Meet the Experts: Dana Klisanin, Ph.D. , psychologist and CEO of Evolutionary Guidance Media R&D Patrick Porter, Ph.D., neuroscience expert and founder of BrainTap ; Jeff Temple, Ph.D. , licensed psychologist and founding director of the Center for Violence Prevention at University of Texas Medical Branch; Brad Thomas, Ph.D. , NYC-based therapist and licensed clinical psychologist; Jeff Yoo, L.M.F.T. at Moment of Clarity Mental Health Center .
“Being happy in life and with self begins with our choices as adults and how we perceive our contributions to the world,” says Jeff Yoo, L.M.F.T. at Moment of Clarity Mental Health Center . Ahead, mental health experts explain tips for being happy alone, how to ask for help when you need it, and what it is to be alone versus feeling lonely. Alone vs. lonely
Being alone is a physical state where you are not in the company of others, whereas feeling lonely is an emotional state of feeling isolated, regardless of whether you’re physically alone or with others, says Patrick Porter, Ph.D., neuroscience expert and founder of BrainTap . “One can be alone without feeling lonely, and conversely, one can feel lonely in a crowd,” he says. Understanding this difference is crucial, as it impacts how you approach your own mental and emotional well-being.
Aloneness can be a neutral state, says Brad Thomas, Ph.D. , NYC-based therapist and licensed clinical psychologist. “People can be happy being by themselves, and there are other times when they desire to be emotionally connected to others,” he says. Still, we want to keep our eye on these feelings to determine to what extent we are feeling loneliness and how distressing it can be, he adds.
Aloneness can be an enriching experience—giving us the chance to learn more about ourselves and the world around us, says Dana Klisanin, Ph.D. , psychologist and CEO of Evolutionary Guidance Media R&D. “Loneliness can arise when we feel that we have no one to share our experiences with or no one who understands us,” she says. How to be happy alone short-term
In our society, there is a stigma around being alone or feeling lonely that we can flip on its head, says Thomas. “We can take some of the power away from that stigmatization and look at it healthier,” he says. There are many advantages to being alone, like having the time to focus on yourself. “That is taking the power in your hands and understanding what you desire, independent of other people’s reactions,” Thomas explains.
When it comes to things you can start doing right now to be happy alone, experts suggest: Question the narrative
First of all, ask yourself if you are really “unhappy alone” or have you been taught to think you should be unhappy if you are alone, says Klisanin. “Our narratives define us. If your ‘story’ isn’t working, you have permission to change it,” she says. Take a moment for mindfulness
Spend five to 10 minutes each day meditating to center yourself. Focus on your breathing and the present moment, suggests Porter. Accepting solitude as an opportunity rather than a hindrance can shift one’s perspective, adds Klisanin. Get active
Even a 20-minute walk outside can boost endorphin levels, elevating your mood and well-being, says Porter. “Avoid sitting for prolonged periods; our research shows that just two hours of sitting can reduce oxygen in the brain by 10%. Make it a point to get up and move around,” he adds. Take a tech break
Take a break from being on your computer and technology when you can, says Thomas. “Putting away your devices allows you to check in with yourself to see what you desire.” Engage in creative activities
These can be therapeutic and stimulate your brain, says Porter. Whether it’s painting, journaling , gardening , or learning to play a musical instrument, a new hobby can provide a sense of fulfillment and self-expression, says Klisanin. Get inspired
Watching short motivational videos or reading inspirational quotes can uplift your spirits, says Porter—so time to watch some Ted Talks!
Advertisement Practice self-care and grounding
Pamper yourself, whether it’s taking a warm bath or enjoying your favorite healthy snack, says Porter. “Additionally, spend some time outside grounding yourself to release excess energy. Walk on grass barefoot or with leather shoes to achieve a zero point energy state; our research indicates that the average person has up to three volts of disruptive energy flowing through their body,” he adds. How to be happy alone long-term
The more you practice and get into the habit of being alone, the more you’ll understand your path of self-understanding and discovery, says Thomas. With time, “you’ll be able to tolerate so much more ambiguity because you know yourself well,” he says. Experts explain the best tips for figuring out how to be happy alone long-term. Build a routine
A stable routine helps your brain recognize patterns, making you feel more in control and happier, says Porter. “Incorporate a consistent sleep schedule into this routine. Going to bed and waking up at the same time helps regulate your body’s clock and improves your overall well-being,” he says. Set goals
Whether they are short- or long-term, goals give you a sense of purpose, says Porter. “Challenge yourself to tackle new things; this keeps your mind sharp and invokes the beginner’s mindset, which is fantastic for discovering happiness,” he says. Keep your mind sharp
Learning something new is not just rewarding; it enhances brain function, says Porter. “Continuously challenging yourself with new skills not only boosts your self-esteem […]
Your brain remembers what your fingers used to do
New CU Boulder research demonstrates that, with practice, older adults can regain manual dexterity that may have seemed lost
Despite what ads for wrinkle cream would have us believe, there’s no magic reversal for aging. As the years pass, a certain amount of change is inevitable but not, it turns out, inexorable.
Fingers that feel less nimble in doing the normal tasks of life—buttoning a shirt, writing a list—are not doomed to stay that way, new research shows . It also demonstrates that, to some extent, age is just a number.
Researchers in the University of Colorado Boulder Department of Integrative Physiology —first author Sajjad Daneshgar and Taylor Tvrdy , both PhD students, and Professor Roger Enoka —worked with more than two dozen study participants ages 60 to 83 to understand whether manual dexterity can improve with time. Sajjad Daneshgar, a PhD student in the CU Boulder Department of Integrative Physiology, conducted research that found manual dexterity can improve with practice in older age. Over six sessions, participants completed a pegboard exercise multiple times, and after the sixth session, data showed that the average time it took to complete the pegboard had decreased for all participants.
“We saw that in older adults, training can improve hand function to a level it was at in middle age,” Daneshgar says. “In a way, practicing helped them go back a decade or two. Most people believe that aging has many negative challenges in terms of function in the hands, but this study shows that what you achieved in the past can really help you as you get older.”
Simple puzzle, complex process
For the study, Daneshgar and his research colleagues recruited right-handed older adults with no history of neurological disease. After an initial familiarization session and evaluation session, participants completed a grooved pegboard test 25 times in each of six sessions.
The test required participants to fit small, keyhole-shaped metal pegs into 25 holes on a board as quickly as possible. The keyholes had different orientations on the board, so participants not only had to manipulate the pegs with their fingers to get them situated correctly, but then fit them correctly.
“At first glance, this looks like a simple puzzle or game, but it’s actually a very complex process,” Daneshgar says. “Your mind is controlling your physical function—and we’re doing a lot more studies on this physical function and what’s going on in the muscles, in the nervous system—and we’re seeing that cognition of the mind, how you learn things, is connected to the muscles and how dexterous you are.”
For example, one of the study participants was a 67-year-old woman who played the piano in her youth. While the average time to complete the pegboard was between 40 and 50 seconds, she could do it in 36—a time faster than some of the researchers could achieve.
“Even though she wasn’t regularly playing the piano during the study, that tells us that perhaps the memory your brain has of controlling those muscles still exists,” Daneshgar says. “Some activities that people do—playing a musical instrument, rock climbing—can be very beneficial for manual dexterity, and even if they’re done earlier in life, the brain may remember controlling those muscles.” During the research, study participants fit small, keyhole-shaped metal pegs into 25 holes on a board as quickly as possible. Practice leads to improvement
However, those who reach their later years without a longtime history of guitar-playing or bouldering shouldn’t despair. Wherever study participants started at baseline—even if their initial times for completing the pegboard were comparatively slow—each saw improvement in their times by the sixth session.
“Manual dexterity can be improved by the brain,” Daneshgar says. “It’s not just at the level of the fingers. Signals from the brain are controlling function and practicing aids learning. This study shows that, as far as function in the limbs and hands, learning in terms of muscle training never ends. Whatever level you’re at, you can go back to this training and practicing to see improvement in function.”
Another important outcome from the research is demonstrating that categorizing people’s performance based on chronological age during their later years may not be the best way to understand manual dexterity.
“Whatever you learned in the past is going to be a main player in performance in older age,” Daneshgar says. “Of course, not all people in older age are going to have the same performance, but people who had better practice in the past can, in older age, practice and get to a place where they perform better than middle-age adults.
“But we also showed that practice helps everybody. It doesn’t matter if you have particular experience earlier in life, practice helps all people to do better with no exception.”
Manual dexterity is one of the National Institutes of Health Toolbox biomarkers of neurological health and motor function across the span of life. Daneshgar notes that the research demonstrates manual dexterity is not something that must inevitably worsen over time. With practice, the brain can remember what the fingers once did.
“Manual dexterity relates to our ability to button a shirt or hold a pen,” Daneshgar says. “These are the activities of daily life that we want to be able to do throughout our lives, and they’re abilities that we don’t need to lose.”
Did you enjoy this article? Subcribe to our newsletter. Passionate about integrative physiology? Show your support. Image of wind turbines Next crime commission should focus on domestic-violence research, expert says
