Nature Knows and Psionic Success
God provides
Superfoods for the brain

Meal planning is one thing, deliberately including superfoods in our diet is another. One can be an economical activity while the other one can be considered an investment to our physical body, with the hope that it may serve us well for the many years to come.
For those who would like to enhance their ability to memorize things, start by incorporating brain-boosting foods into your diet. They not only help us retain more information, they can also be powerful antidotes to being forgetful (which comes with age). Make your own trail mix by incorporating brain-friendly superfoods such as nuts, seeds and dark chocolate. Superfoods have been around for a long time, although the word ‘superfoods’ has only been coined in the last decade or so to make it distinctly different from the rest.
Fish, wholegrain foods, dark leafy vegetables, berries are but a few food items that we can prepare more often to ensure our brain power is sustained.
For this week’s column, I’d like to focus on other superfoods such as matcha, dark chocolate and nuts and seeds — these are supplements we can easily add in to our daily lives.
Get the latest news delivered to your inbox
Sign up for The Manila Times newsletters
By signing up with an email address, I acknowledge that I have read and agree to the Terms of Service and Privacy Policy .
Matcha. Considered a natural nootropic (brain booster), matcha can help your brain work better by improving memory, focus, and motivation.
It also makes your brain healthier by increasing blood flow and giving it more energy and oxygen.
Try substituting one coffee cup to matcha latte, for example, and work your way towards replacing it altogether. You will get the same effect due to the caffeine properties of both drinks. Your brain will thank you for it.
Dark chocolate. The darker the chocolate, the better it is for your brain.
Studies show that consuming dark chocolates or cocoa that are high in flavanol can help improve the brain’s blood flow.
We have very good local brands of dark chocolate to eat as a snack. You can also opt to use this when making desserts or breakfasts.
Tablea is a great local product that we can use for this purpose and one example is oats champorado. Simply cook your oats in boiling water and milk, add tablea and your preferred sweetener and you’re good to go.
Nuts and seeds. Bring a handful of these in a small bag for a quick brain food snack. For those who like to prepare beforehand, making granola out of your nuts and seeds is a nice alternative to ensure you’re in tip top shape when utilizing brain power.
Simply combine your choice of nuts and seeds – think pumpkin seeds, flax seeds, pecans, walnuts – with some dried berries here and there for variety. Then add your sweetener of choice (agave is a good plant-based option) and bake in the oven for a couple of minutes.
Once cooled, you can crumble and eat as is or add in your yoghurt, oats or you may slice just like your typical granola bars. You can also make your own trail mix with this and add your dark chocolate bars.
These are examples of how we can supplement our nutrition with brain-friendly foods.
Happy cooking!
***
The author may be reached at kaycalpolugtu@gmail.com or follow her at Instagram @kaycalpolugtu and @aplateofbahaykubo.
President Ferdinand Marcos Jr. visits the Unilever Factory in General Trias, Cavite on Friday, Sept. 22, 2023. PHOTO BY KJ ROSALES/PPA POOL
President Ferdinand Marcos Jr. visits the Unilever Factory in General Trias, Cavite on Friday, Sept. 22, 2023. PHOTO BY KJ ROSALES/PPA POOL
President Ferdinand Marcos Jr. visits the Unilever Factory in General Trias, Cavite on Friday, Sept. 22, 2023. PHOTO BY KJ ROSALES/PPA POOL
President Ferdinand Marcos Jr. visits the Unilever Factory in General Trias, Cavite on Friday, Sept. 22, 2023. PHOTO BY KJ ROSALES/PPA POOL
The Seafarers Empowerment Advocates Network holds a roundtable with Filipino seafarers and other organizations on their Magna Carta at the Central United Methodist Church in Manila on Friday, Sept. 22, 2023, coinciding with National Seafarers’ Day. PHOTO BY J. GERARD SEGUIA
The Seafarers Empowerment Advocates Network holds a roundtable with Filipino seafarers and other organizations on their Magna Carta at the Central United Methodist Church in Manila on Friday, Sept. 22, 2023, coinciding with National Seafarers’ Day. PHOTO BY J. GERARD SEGUIA The Seafarers Empowerment Advocates Network holds a roundtable with Filipino seafarers and other organizations on their Magna Carta at the Central United Methodist Church in Manila on Friday, Sept. 22, 2023, coinciding with National Seafarers’ Day. PHOTO BY J. GERARD SEGUIA The Seafarers Empowerment Advocates Network holds a roundtable with Filipino seafarers and other organizations on their Magna Carta at the Central United Methodist Church in Manila on Friday, Sept. 22, 2023, coinciding with National Seafarers’ Day. PHOTO BY J. GERARD SEGUIA The Seafarers Empowerment Advocates Network holds a roundtable with Filipino seafarers and other organizations on their Magna Carta at the Central United Methodist Church in Manila on Friday, Sept. 22, 2023, coinciding with National Seafarers’ Day. PHOTO BY J. GERARD SEGUIA President Ferdinand Marcos Jr. delivers a message during the rice distribution at General Trias Sports Park in Cavite on Friday, Sept. 22, 2023. Over 1,200 members of 4Ps received one sack of rice each while 200 farmers received agricultural products. PHOTO BY RENE H. DILAN President Ferdinand Marcos Jr. delivers a message during the rice distribution at General Trias Sports Park in Cavite on Friday, Sept. 22, 2023. Over 1,200 members of 4Ps received one sack of rice each while 200 farmers received agricultural products. PHOTO BY RENE H. DILAN President Ferdinand Marcos Jr. delivers a message during the rice distribution at General Trias Sports Park in Cavite on Friday, Sept. 22, 2023. Over 1,200 members of 4Ps received one sack of rice each while 200 farmers […]
Brain’s Dual-Chemical Switch for Attention Revealed

Summary: Researchers have unveiled the brain’s chemical mechanism behind our attention span.
Historically, the neurotransmitter acetylcholine was considered the sole regulator of attention. Yet, this study shows that gamma-aminobutyric acid (GABA) collaborates with acetylcholine, toggling like a ‘switch’ in the brain’s claustrum region to filter essential information from noise.
This breakthrough can aid in therapies for concentration-related disorders.
Key Facts:
> Besides the known neurotransmitter acetylcholine, GABA also plays a crucial role in attention span regulation.
The claustrum acts as an attention-regulating hub where acetylcholine and GABA toggle the transfer of brain information.
This discovery might lead to enhanced treatments for attention disorders like ADHD and depression.
Source: NTU
A team of researchers from Nanyang Technological University, Singapore (NTU Singapore) has uncovered new clues about how chemicals released by brain cells regulate our attention span.
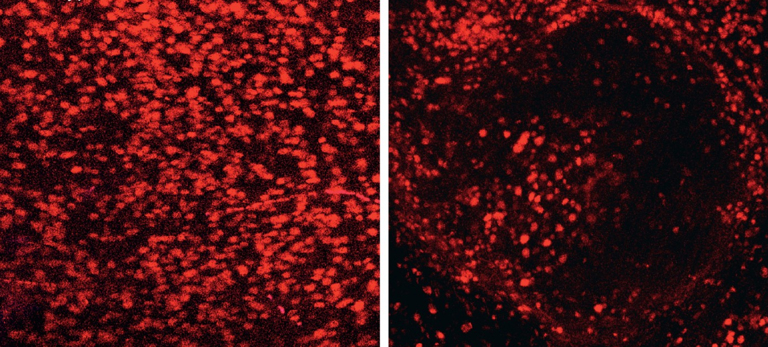
Findings from the study could pave the way for new therapies to treat neurological conditions associated with concentration difficulties, such as depression and attention-deficit hyperactivity disorder (ADHD). The opposing actions of the neurotransmitters (acetylcholine and GABA) on neurons in the claustrum enable brain signals to be encoded efficiently, allowing the brain to pay attention and ignore noise. Credit: Neuroscience News To communicate with one another, neurons in the brain and nervous system release chemicals called neurotransmitters that relay messages from one cell to another. Neurotransmitters are crucial for brain function and regulating all bodily functions, ranging from breathing and heart rate to reproduction.
These chemicals also coordinate cognitive processes that enable us to focus on important information within the constant barrage of stimuli the brain receives from the external environment, otherwise known as our attention span.
Researchers have long thought that our attention span was directed by only one neurotransmitter, acetylcholine, which excites neurons and causes them to fire electrical signals. However, recent work suggests that attention could require another neurotransmitter, gamma-aminobutyric acid (GABA), which inhibits neurons from receiving and sending messages.
In their study published in the Proceedings of the National Academy of Sciences (PNAS), the team demonstrated for the first time that GABA works together with acetylcholine in a precise sequence to regulate the transmission of signals from a part of the brain’s information processing network, called the claustrum.
Hidden deep in the brain, the claustrum is a thin sheet-like structure that receives and processes information from different parts of it. The claustrum helps to regulate concentration, but its exact role remains unknown.
Neurotransmitters toggle ‘like a switch’ to relay information
In lab experiments, the NTU scientists investigated how neurons in the claustrum in mice respond to acetylcholine and GABA produced by a part of the brain called the forebrain, that plays a central role in several brain functions.
The key technological advance that allowed the researchers to make this discovery is called optogenetics . Optogenetics uses light-sensitive proteins to selectively control the activity of specific types of neurons within the brain. In this case, the neurons within the forebrain that release acetylcholine and GABA were activated by light, allowing the team to measure the response of the claustrum to such a stimulus.
They discovered that two types of neurons in the claustrum, which send output signals to different parts of the brain, respond in opposing ways to acetylcholine and GABA. Neurons that extend to structures deep in the brain were excited by acetylcholine while neurons that extend to structures on the surface of the brain were inhibited by GABA.
Through this coordinated sequence of opposing actions, the two neurotransmitters toggle the transfer of information between the claustrum and the rest of the brain, like a switch. The study provides evidence that the neurotransmitters regulate a “microcircuit” in the brain, that allows the organ to differentiate important information from noise, helping a person pay attention.
The opposing actions of the neurotransmitters ( acetylcholine and GABA) on neurons in the claustrum enable brain signals to be encoded efficiently, allowing the brain to pay attention and ignore noise.
First author Mr Aditya Nair, former researcher at LKCMedicine and a current Ph.D. student at Caltech, said, “Our study advances our understanding of the claustrum’s role in directing attention span. Understanding how the claustrum regulates attention span at the cellular level also provides a window into other areas regulated by similar signalling pathways, such as arousal and learning.”
Lead investigator and neuroscientist Professor George Augustine from NTU’s Lee Kong Chian School of Medicine (LKCMedicine) said, “By understanding how acetylcholine and GABA work together to direct our attention, new and more effective therapies may be developed in the future to improve the attention span of patients with conditions such as ADHD and depression.”
Commenting as an independent expert, Dr Geoffrey Tan, Consultant (Psychiatry) Clinician-Scientist at the Institute of Mental Health Singapore, said, “Directing attention and multi-tasking are crucial cognitive processes for everyday functioning that require toggling between networks or circuits in the brain.
This study identifies a ‘switch’ in the claustrum that provides a mechanism by which acetylcholine may drive computations such as these. It is timely as we increasingly incorporate brain networks into how we think about cognition, psychiatric conditions and even interventions like mindfulness.”
The next steps for this project will be to determine how altering the dual-transmitter switch alters attention and brain disorders that affect attention, such as ADHD. It will also be important to determine whether the switch mechanism applies to other brain processes, such as arousal and learning. About this neuroscience research news
Author: Junn Loh Source: NTU Contact: Junn Loh – NTU Image: The image is credited to Neuroscience News Original Research: Open access. “ A functional logic for neurotransmitter corelease in the cholinergic forebrain pathway ” by Aditya Nair et al. PNAS Abstract A functional logic for neurotransmitter corelease in the cholinergic forebrain pathway The cholinergic system of the basal forebrain plays an integral part in behaviors ranging from attention to learning, partly by altering the impact of noise in neural populations.The circuit computations underlying cholinergic actions are confounded by recent findings that forebrain cholinergic neurons corelease both acetylcholine (ACh) and GABA.We have identified that corelease of ACh and GABA by […]
New brain biomarker predicts recovery from treatment-resistant depression

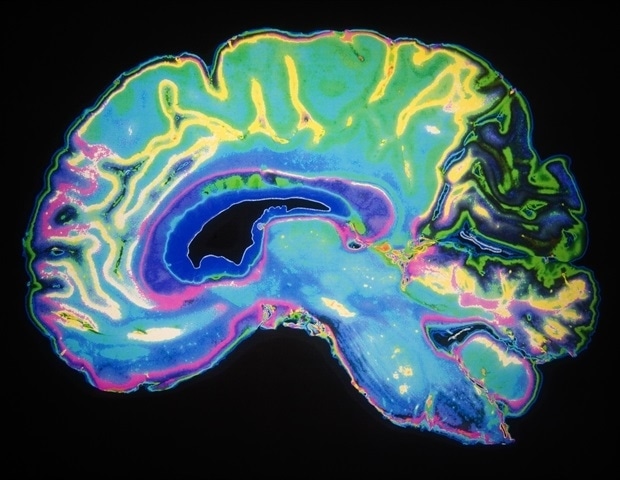
Using a novel deep brain stimulation (DBS) device capable of recording brain signals, researchers have identified a pattern of brain activity or “biomarker” related to clinical signs of recovery from treatment-resistant depression. The findings from this small study are an important step towards using brain data to understand a patient’s response to DBS treatment. The study was published in Nature and supported by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies ® Initiative, or The BRAIN Initiative ® .
Although the approach is still experimental, clinical research shows that DBS can be used safely and effectively to treat cases of depression in which symptoms have not improved with antidepressant medications, referred to as treatment-resistant depression. People receiving DBS undergo surgery to have a thin metal electrode implanted into specific brain areas to deliver electrical impulses that modulate brain activity. How exactly DBS improves symptoms in people with depression is not well-understood, which has made it difficult for researchers to objectively track patients’ response to treatment and adjust as needed.
The small study enrolled 10 adults with treatment-resistant depression, all of whom underwent DBS therapy for six months. Each participant received the same stimulation dose to begin and then stimulation levels were increased once or twice. Later, researchers used artificial intelligence (AI) tools to analyze collected brain data from six patients and observed a common brain activity signature or biomarker that correlated with patients self-reporting feeling symptoms of depression or stable as they recovered. In one patient, researchers identified the biomarker and were retrospectively able to predict that a patient would fall back into a major depressive episode four weeks before clinical interviews showed they were at risk of a relapse occurring. This study demonstrates how new technology and a data-driven approach can refine DBS therapy for severe depression, which can be debilitating. It’s this type of collaborative work made possible by the BRAIN Initiative that moves promising therapies closer to clinical use.” John Ngai, Ph.D., Director of the BRAIN Initiative In the study, patients received DBS targeting the subcallosal cingulate cortex (SCC), a brain region that regulates emotional behavior and is involved in feelings of sadness. DBS of the SCC is an emerging therapy that can provide stable, long-term relief from depressive symptoms for years. However, using DBS to treat depression remains challenging because each patient’s path to stable recovery looks different. Clinicians also must rely on subjective self-reports from patient interviews and psychiatric rating scales to track symptoms, which can fluctuate over time. This makes it hard to distinguish between normal mood variations and more serious situations requiring a tweak in stimulation. In addition, changes in symptoms in response to DBS can take weeks or months to occur, making it difficult to tell how well the therapy is working.
“This biomarker suggests that brain signals can be used to help understand a patient’s response to DBS treatment and adjust the treatment accordingly,” said Joshua A. Gordon, M.D., Ph.D., director of NIH’s National Institute of Mental Health. “The findings mark a major advance in translating a therapy into practice.”
The patients in the study responded well to DBS therapy; after six months, 90% showed a significant improvement in depression symptoms, and 70% were in remission or no longer depressed. This high response rate was a unique opportunity to look back and examine how each patient’s brain responded differently to the stimulation during treatment.
Christopher Rozell, Ph.D., Julian T. Hightower Chair and professor of electrical and computer engineering at Georgia Tech in Atlanta, and his colleagues used a technique called explainable artificial intelligence to understand these subtle changes in brain activity. The algorithm used brain data to distinguish between depressive versus stable recovery states and was able to explain what activity changes in the brain were the main drivers of this transition. Importantly, the biomarker also distinguished between normal day-to-day transient mood changes and sustained worsening symptoms. This algorithm could provide clinicians with an early warning signal that a patient is moving toward a highly depressive state and requires a DBS adjustment and extra clinical care.
“Nine out of 10 patients in the study got better, providing a perfect opportunity to use a novel technology to track the trajectory of their recovery,” said Helen Mayberg, M.D., director of the Nash Family Center for Advanced Circuit Therapeutics at Icahn Mount Sinai in New York City and co-senior author of the study. “Our goal is to identify an objective, neurological signal to help clinicians decide when, or when not, to make a DBS adjustment.”
“We showed that by using a scalable procedure with single electrodes in the same brain region and informed clinical management, we can get people better,” said Dr. Rozell, co-senior author of the study. “This study also gives us an amazing scientific platform to understand the variation between patients, which is key to treating complex psychiatric disorders like treatment-resistant depression.”
Next, the team analyzed data from MRI brain scans collected from patients before surgery. The results revealed structural and functional abnormalities in the specific brain network targeted by the DBS therapy. More severe white matter deficits were related to longer recovery times.
Researchers also used AI tools to analyze changes in facial expression extracted from videos of participant interviews. In a clinical setting, a patient’s facial expression can reflect the severity of their depression symptoms, a change that psychiatrists likely pick up on in routine clinical evaluations. They found patterns in individual patient expressions that coincided with their transition from illness to stable recovery. This could serve as an additional tool and new behavioral marker to track recovery in DBS therapy. More research is needed to determine whether the video analysis can reliably predict current and future disease states.
Both the observed facial expression changes and anatomical deficits correlated with cognitive states captured by the biomarker, supporting the use of this biomarker in managing DBS therapy for depression.
The research team, including Drs. Mayberg and Rozell, and Patricio Riva-Posse, M.D., at Emory University School of Medicine in Atlanta, is now confirming their findings in a second cohort […]
Brain stimulation could boost maths ability – study

Using electrodes to ‘excite’ certain areas of the brain could help people who struggle with maths enjoy the subject more, a study has suggested (Alamy/PA) Using electrodes to “excite” certain areas of the brain could help people who struggle with maths enjoy the subject more, a study has suggested.
A team spanning the universities of Surrey and Oxford , Loughborough University , and Radboud University in the Netherlands investigated the impact of neurostimulation on learning.
High-frequency random noise stimulation, also known as tRNS, works by sending a mild electrical current to the brain through two electrodes on the scalp. Previously, we have shown that a person’s ability to learn is associated with neuronal excitation in their brains
Roi Cohen Kadosh, a professor of cognitive neuroscience and head of the School of Psychology at the University of Surrey led the project. Recommended
Charity boss speaks out over ‘traumatic’ encounter with royal aide
Ukraine war’s heaviest fight rages in east – follow live
He said: “ Learning is key to everything we do in life – from developing new skills, such as driving a car, to learning how to code. Our brains are constantly absorbing and acquiring new knowledge.
“Previously, we have shown that a person’s ability to learn is associated with neuronal excitation in their brains. What we wanted to discover in this case is if our novel stimulation protocol could boost, in other words excite, this activity and improve mathematical skills.”
Some 102 people were recruited for the study – published in the journal Plos Biology – with their mathematical skills assessed beforehand.
They were split into four groups, including a learning group and an ‘overlearning’ group – in which people practised sums “beyond the point of mastery” – while being exposed to high-frequency random electrical noise stimulation.
The other two groups were exposed to a placebo, which researchers said was similar to real stimulation but without significant electrical currents.
Access unlimited streaming of movies and TV shows with Amazon Prime Video
Sign up now for a 30-day free trial
Sign up
Brain activity was measured via an electroencephalogram (EEG) recording at the beginning and end of the stimulation. This discovery could not only pave the way for a more tailored approach in a person’s learning journey but also shed light on the optimal timing and duration of its application
The team found the ability of those whose brains were less “excited” by maths during the assessment had improved post-stimulation.
There was no change in those who performed well in the initial assessment, nor in those included in the placebo groups.
Prof Cohen Kadosh added: “What we have found is how this promising neurostimulation works and under which conditions the stimulation protocol is most effective. Recommended
Reported sighting of Daniel Khalife ‘could be very significant’ – police chief
Timeline of events around hunt for terror suspect Daniel Khalife
Police name man who died in custody after being held for murder of missing woman
“This discovery could not only pave the way for a more tailored approach in a person’s learning journey but also shed light on the optimal timing and duration of its application.”
Dr Nienke van Bueren from Radboud University, who led the study under Prof Cohen Kadosh’s supervision, said: “These findings highlight that individuals with lower brain excitability may be more receptive to electrical noise stimulation, leading to enhanced learning outcomes, while those with high brain excitability might not experience the same benefits in their mathematical abilities.”
A mouse with 100,000 human neurons in its brain illuminates the enigma of Alzheimer’s
When a person gets older and begins to lose his or her memory, even to forget the names of their loved ones, it is already too late. Alzheimer’s has been quietly destroying the brain for years. If you could open the skull, you would see dead neurons and accumulations of two characteristic proteins: amyloid and tau. The disease threatens to wipe out civilization in the coming decades — there are 10 million new cases of dementia every year — but the scientific community still has no idea what causes it. An international team, including Spanish neuroscientist Amaia Arranz, has introduced 100,000 human neurons into the brains of mice to try to investigate in vivo what happens during the advance of Alzheimer’s disease. The authors have observed how the cells perish and have managed to avoid this neuronal death with a simple oral treatment. Their breakthrough was published Thursday in the journal Science .
Mice are not susceptible to Alzheimer’s, but the researchers genetically modified them to suffer from an accumulation of the amyloid protein. By introducing human neurons into the brains of these rodents, the scientists were able to identify the exact mechanism of neuronal destruction: activation of the MEG3 gene induces necroptosis, a genetically programmed cell death, which is also present in cancer. A drug approved for the treatment of leukemia, ponatinib, and another for melanoma, dabrafenib, prevented neuronal death in these mice. The anti-inflammatory necrosulfonamide achieves the same effect. “There are still no drugs that cure or help alleviate the symptoms of Alzheimer’s disease. This study could help to find therapies that prevent the loss of neuronal cells,” says Arranz of the Achúcarro Basque Center for Neuroscience in Bilbao.
The work was carried out in the laboratory of Belgian biologist Bart De Strooper, of the VIB-KU Leuven Center for Brain & Disease Research (CBD). Arranz and fellow scientist Ira Espuny participated at the CBD in 2017 in the development of the first mouse with human neurons that recreated something similar to Alzheimer’s. The new study has gone a step further by implanting both human and mouse neurons in the rodents. The human neurons immediately showed the hallmarks of the disease: tau and amyloid proteins and cell death. The mouse neurons, on the other hand, remained intact. In the authors’ opinion, these results reveal “a human-specific vulnerability to Alzheimer’s disease .”
The brain of a mouse is the size of a pea, weighs half a gram and contains about 70 million neurons. Arranz explains that the 100,000 implanted human neurons remain in a very specific region. “The mouse brain is still a mouse brain, with a little piece where there are human cells. We are not going to create monsters or Frankensteins,” says the neuroscientist. Her research center is named after Nicolás Achúcarro, a Spanish physician who was working in Munich in Alois Alzheimer’s laboratory when the German neurologist described a new disease in 1906, based on the case of a 50-year-old woman with memory loss issues. More than a century later, mankind continues to ignore the causes of Alzheimer’s disease.
Biologist Estela Area Gómez won last year’s Oskar Fischer Prize for postulating a hypothesis that links neuronal death in Alzheimer’s disease to failures in cholesterol metabolism. In her opinion, the scientific community has been stuck for decades on a false premise: that deposits of amyloid and tau proteins are responsible for dementia. The researcher recalls that the Colombian neurologist Francisco Lopera found two people with an aggressive genetic mutation that condemned them to suffer early Alzheimer’s , but they remained healthy for years due to other protective mutations. “Those patients had a lot of amyloid plaques. In other words, it has been shown that it is not the amyloid plaques that lead to the disease,” says Gómez, of the Margarita Salas Center for Biological Research in Madrid.
Gómez is skeptical about the conclusions of the new study, in which she did not participate. “These mice, at a technical level, are wonderful, but I have serious doubts as to whether they really reflect what happens in humans,” she says. “It’s like if you want to make a mouse that models a covid infection and, instead of infecting it with the cause — the coronavirus — you decide you’re just going to induce an increase in fever. What you’re doing is mirroring the symptoms of the disease in the mouse, but not the disease per se.”
Two years ago, the United States authorized aducanumab , touted as the first drug to attack the presumed causes of Alzheimer’s disease. The drug — developed by the U.S. pharmaceutical company Biogen and priced at about $42,500 euros per patient per year — eliminates the amyloid proteins that accumulate between neurons. The European Medicines Agency, however, has refused to approve aducanumab because it found no evidence of its efficacy.
“My question is how long are we going to continue investing all our efforts in eliminating amyloid plaques, when we are seeing that there are people with three, four or five times more amyloid plaques than an Alzheimer’s patient and they have no cognitive defects,” says Gómez. The biologist recalls that carrying the APOE4 gene multiplies the risk of suffering from Alzheimer’s and is related to cholesterol metabolism. “Nature is shouting at us that the failure of cholesterol metabolism in neurons is one of the causes, if not the main cause, of Alzheimer’s.”
De Strooper founded the prestigious Dementia Research Institute in the UK in 2016, where he directed the work of over 800 scientists until last year. The Belgian is one of the world’s leading experts on Alzheimer’s. His study suggests that understanding the molecular intricacies of neuronal resistance in mice to the disease will illuminate the path to protecting the human brain.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Brain inspires more robust AI
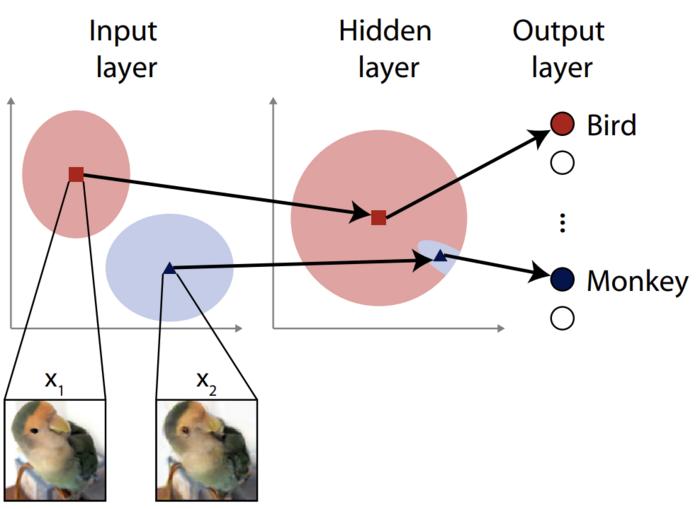
image: To our eyes the input images x1 and x2 look the same, but hidden features nudge a typical neural network to classify this bird image as a monkey by mistake. It’s said the images are distant at the input space, but close in the hidden-layer space. The researchers aimed to close this exploit. view more Credit: ©2023 Ohki & Ukita CC-BY Most artificially intelligent systems are based on neural networks, algorithms inspired by biological neurons found in the brain. These networks can consist of multiple layers, with inputs coming in one side and outputs going out of the other. The outputs can be used to make automatic decisions, for example, in driverless cars. Attacks to mislead a neural network can involve exploiting vulnerabilities in the input layers, but typically only the initial input layer is considered when engineering a defense. For the first time, researchers augmented a neural network’s inner layers with a process involving random noise to improve its resilience.
Artificial intelligence (AI) has become a relatively common thing; chances are you have a smartphone with an AI assistant or you use a search engine powered by AI. While it’s a broad term that can include many different ways to essentially process information and sometimes make decisions, AI systems are often built using artificial neural networks (ANN) analogous to those of the brain. And like the brain, ANNs can sometimes get confused, either by accident or by the deliberate actions of a third party. Think of something like an optical illusion — it might make you feel like you are looking at one thing when you are really looking at another.
The difference between things that confuse an ANN and things that might confuse us, however, is that some visual input could appear perfectly normal, or at least might be understandable to us, but may nevertheless be interpreted as something completely different by an ANN.
A trivial example might be an image-classifying system mistaking a cat for a dog, but a more serious example could be a driverless car mistaking a stop signal for a right-of-way sign. And it’s not just the already controversial example of driverless cars; there are medical diagnostic systems, and many other sensitive applications that take inputs and inform, or even make, decisions that can affect people.
As inputs aren’t necessarily visual, it’s not always easy to analyze why a system might have made a mistake at a glance. Attackers trying to disrupt a system based on ANNs can take advantage of this, subtly altering an anticipated input pattern so that it will be misinterpreted, and the system will behave wrongly, perhaps even problematically. There are some defense techniques for attacks like these, but they have limitations. Recent graduate Jumpei Ukita and Professor Kenichi Ohki from the Department of Physiology at the University of Tokyo Graduate School of Medicine devised and tested a new way to improve ANN defense.
“Neural networks typically comprise layers of virtual neurons. The first layers will often be responsible for analyzing inputs by identifying the elements that correspond to a certain input,” said Ohki. “An attacker might supply an image with artifacts that trick the network into misclassifying it. A typical defense for such an attack might be to deliberately introduce some noise into this first layer. This sounds counterintuitive that it might help, but by doing so, it allows for greater adaptations to a visual scene or other set of inputs. However, this method is not always so effective and we thought we could improve the matter by looking beyond the input layer to further inside the network.”
Ukita and Ohki aren’t just computer scientists. They have also studied the human brain, and this inspired them to use a phenomenon they knew about there in an ANN. This was to add noise not only to the input layer, but to deeper layers as well. This is typically avoided as it’s feared that it will impact the effectiveness of the network under normal conditions. But the duo found this not to be the case, and instead the noise promoted greater adaptability in their test ANN, which reduced its susceptibility to simulated adversarial attacks.
“Our first step was to devise a hypothetical method of attack that strikes deeper than the input layer. Such an attack would need to withstand the resilience of a network with a standard noise defense on its input layer. We call these feature-space adversarial examples,” said Ukita. “These attacks work by supplying an input intentionally far from, rather than near to, the input that an ANN can correctly classify. But the trick is to present subtly misleading artifacts to the deeper layers instead. Once we demonstrated the danger from such an attack, we injected random noise into the deeper hidden layers of the network to boost their adaptability and therefore defensive capability. We are happy to report it works.”
While the new idea does prove robust, the team wishes to develop it further to make it even more effective against anticipated attacks, as well as other kinds of attacks they have not yet tested it against. At present, the defense only works on this specific kind of attack.
“Future attackers might try to consider attacks that can escape the feature-space noise we considered in this research,” said Ukita. “Indeed, attack and defense are two sides of the same coin; it’s an arms race that neither side will back down from, so we need to continually iterate, improve and innovate new ideas in order to protect the systems we use every day.”
###
Journal article: Jumpei Ukita and Kenichi Ohki. “Adversarial attacks and defenses using feature-space stochasticity ”, Neural Networks , DOI: 10.1016/j.neunet.2023.08.022
Funding:
This work was supported by Brain Mapping by Integrated Neurotechnologies for Disease Studies (Brain/MINDS) from Japan Agency for Medical Research and Development (AMED) (14533320, JP16dm0207034, JP20dm0207048 to K.O.); CREST-JST (JPMJCR22P1 to K.O.); Institute for AI and Beyond (to K.O.); JSPS KAKENHI (25221001, 19H05642, 20H05917, to K.O.); Takeda Science Foundation (to J.U.); and Masayoshi Son Foundation (to J.U.).
Departmental links:
Ohki Lab – https://physiol1.m.u-tokyo.ac.jp/ern24596/en/
[…]
France suspends iPhone 12 sales over concerns of high electromagnetic radiation emissions

Advertisement
France’s National Frequency Agency (ANFR) has ordered Apple to halt sales of the iPhone 12 on the French market following recent tests showing that the phone model is emitting electromagnetic waves exceeding levels acceptable to the country’s regulatory limits .
The move gives Apple 15 days to correct the issue and bring the iPhone 12’s specific absorption rate (SAR) within acceptable levels. The ANFR has urged the tech giant to implement all available means quickly to remedy the malfunction before a full recall of the copies already sold begins. (Related: Apple warns users with medical devices to keep iPhones away from body because they emit EMF .)
The ANFR monitors public exposure to electromagnetic waves using SAR – the measurement that determines electromagnetic waves transported and absorbed by the human body when a phone is in a pocket or in the hand – with the limit placed at four watts per kilogram (w/kg).
The agency recently tested 141 phones, including the iPhone 12, and found that the iPhone 12 exceeded the limit with a reading of 5.74 w/kg and ordered Apple to quickly fix the issue, which could possibly be achieved through a simple software update.
” The rule is the same for everyone , including the digital giants,” said French Minister of Digital and Telecommunications Jean-Noel Barrot. French newspaper Le Parisien even noted that French officials are willing to recall every single iPhone 12 in France, including units that have already been sold.
Barrot said a software update would be sufficient to fix the radiation issues linked to the iPhone model , which the company has been selling since 2020. “Apple is expected to respond within two weeks. If they fail to do so, I am prepared to order a recall of all iPhone 12s in circulation,” he added.
The European Union (EU) has set safety limits for SAR values linked to exposure to mobile phones, which could increase the risk of some forms of cancer according to scientific studies. In 2020, France widened regulations requiring retailers to display the radiation value of products on packaging beyond cellphones, including tablets and other electronic devices.
Barrot assured users that the European standard for electromagnetic emissions is 10 times lower than the levels that scientific studies have established as consequential for users.
The French watchdog ANFR will now pass on its data findings to regulators in other EU member countries
“In practical terms, this decision could ‘snowball’ the restrictive measures,” Barrot said.
ANFR agents have been instructed to ensure that the iPhone 12 is no longer offered for sale through any distribution channel in France. EMFs in radio frequency range pose danger to human health
The International Agency for Research on Cancer (IARC) has classified non-ionizing EMFs in the radio frequency range as Group 2B – a possible human carcinogen . These fields are produced by electronic products, like Bluetooth devices, cellphones, computers, smart devices, smart meters, tablets and wireless routers.
The current IARC evaluation from 2011 pointed to a possible link between RF radiation and cancer in people – particularly glioma, a malignant type of brain cancer. This conclusion means that there could be some risk.
Some researchers feel there’s already enough evidence of harm from long-term, low-level exposure to non-ionizing radiation that the IARC should upgrade the classification to a Group 1 – a known carcinogen.
In a multicenter study published in the International Journal of Epidemiology , researchers followed cancer rates and cellphone use in more than 5,000 people in 13 countries and found a “loose connection” between the highest rate of exposure and glioma – which were more often found on the same side of the head people used to speak on the cellphone.
Another review of more than two dozen studies on low-frequency EMFs published in the Journal of Chemical Neuroanatomy suggested that these energy fields may cause neurological and psychiatric problems in people.
That being said, the best approach is to be aware that EMFs exist and be smart about your exposure. Experts say this is a developing field of research that will undoubtedly expand as the use of wireless devices and labor-saving machines increases.
Radiation.news has more on the dangers of smartphones.
Watch the following video on the dangers of smartphone radiation . Screen radiation Combined with Cell phone radiation is like morphine and Marijuana ararwana
This is a modal window.
No compatible source was found for this media.
This video is from the EMF Safety Co channel on Brighteon.com . More related stories:
Radio signals from mobile phone towers could lead ALIENS to Earth .
SGT Report: 5G towers, smart phones and mRNA injections are inextricably connected .
“Substantial scientific evidence” shows that RF radiation from mobile phones causes cancer . Sources include: Barrons.com TheMessenger.com Reuters.com IARC.WHO.int PubMed.NCBI.NLM.NIH.gov 1 PubMed.NCBI.NLM.NIH.gov 2 Brighteon.com
Unhealthy pathobiome in the brain could cause some forms of Alzheimer’s and related dementias
The human microbiome includes the genetic material of more than 100 trillion tiny microorganisms – fungi, yeast, bacteria, and even viruses, most of which hang out in our gastrointestinal tract to serve as guardians of our health. But when a healthy microbiome gives way to an imbalance -; a “pathobiome” -; any number of health problems can occur -; from rheumatoid arthritis, to bacterial vaginosis. New data published this month in the journal Frontiers in Cellular and Infection Microbiology , from researchers at Drexel’s College of Medicine, gives more evidence to the possibility that developing a pathobiome in the brain could cause some forms of Alzheimer’s and related dementias.
When biomes turn unhealthy, either by invasion of outside pathogens, or a major change in the relative numbers of the microbial species present, a dysbiosis, or imbalance in the microbiota, occurs. This dysbiosis can alter human metabolism and cause inflammation, which has been linked to the tissue damage seen in ulcerative colitis, rheumatoid arthritis and many other chronic inflammatory diseases.
Studying 130 samples from the donated brains of 32 people – 16 with Alzheimer’s and 16 age-matched controls without the disease, the Drexel researchers found bacterial flora in all the brains-; but the Alzheimer’s brains showed profoundly different bacterial profiles compared to their age-matched controls.
The group used full-length 16s ribosomal RNA gene sequencing, a technique that can detect any and all bacterial species present in a sample. In this process, the researchers pinpointed disease-specific sets of bacteria in almost all of the Alzheimer’s-affected brains, suggesting these groups of bacteria are strong predictors of the disease.
The authors detected five brain microbiomes, four that are hypothesized to be present at different times in the evolution of the Alzheimer’s-afflicted brains. The authors said it is likely that the observed Alzheimer’s microbiomes evolve to become more pathogenic as the disease progresses with the later stages characterized as a pathobiome. The authors hypothesize that the brain begins with a healthy biome, but as the disease develops, the healthy biome is supplanted as a new set of microbes replace the original healthy ones with the eventual emergence of the Alzheimer’s pathobiome.
Samples from both sets of brain samples were drawn from the frontal and temporal lobes and entorhinal cortex. Based on the random distribution of microbiomes requiring delivery all over the brain, the results were consistent with failure in one or more of the brain’s networks; however it too soon to tell if the observed distribution patterns result from a leaky blood-brain barrier, the brain’s glymphatic system, or synaptonemal transmission that allowed bacteria, including Cutibacterium acnes (formerly called Proprionibacterium acnes ), Methylobacterium, Bacillus, Caulobacter, Delftia, and Variovora to enter the brain. In Alzheimer’s brain samples, the researchers noted, these pathogenic bacteria appeared to have overpowered and replaced Comamonas sp. bacteria, which are associated with a dementia-free brain. Perhaps destruction of the Comamonas bacteria, part of a healthy brain microbiome, is the first sign of impending dementia. We’re now coming up with the questions to guide future studies, but the hypotheses are many. The culprit could be bacteria or something else – like fungi, parasites, or viruses – at the same time.” Garth D. Ehrlich, PhD, professor in the College of Medicine, senior author of the paper When a patient has Alzheimer’s, they experience inflammation in the brain characterized by deposits of amyloid beta which are formed by an increase in the production of the Aβ peptide (an antimicrobial peptide, which is part of the innate immune response) resulting in amyloid plaques in the brain. Similarly, Alzheimer’s is characterized by tau protein tangles found with the cells which are characterized by abnormal phosphorylation which ultimately lead to the destruction of synapses and neurons, but which have also been demonstrated to help stop the spread of pathogens in the brain.
These protein-oriented pathologies – known as the “amyloid cascade hypothesis”-; have been the main focus of Alzheimer’s research for decades. Recently, studies are challenging that model by suggesting a role for bacteria, fungi and viruses, and immune system and brain inflammation, which some researchers call the “pathogen hypothesis.”
“Multiple studies have now shown the presence of bacteria in Alzheimer’s-afflicted brains,” said Jeffrey Lapides, PhD, an adjunct associate professor in the College of Medicine, and a senior author of the study. “Perhaps plaques, whose constituents have anti-microbial properties in vitro, aren’t the direct cause of Alzheimer’s, but instead are a response to bacteria in the brain – some benign, some pathogenic, perhaps causing damage that has not yet resulted in cognitive deficits, making them part of the pathobiome.”
This unique set of bacteria found in the Alzheimer’s-afflicted brains are also commonly found in brains afflicted with the neurodegenerative disease amyotrophic lateral sclerosis, or ALS — suggesting that this set of bacteria may contribute to more than one neurological illness.
The next step for this research, according to the authors, is to study the possible contributions of other microbes and figure out what happened, physiologically, in the brain to make this microbiome change over time.
“The development of Alzheimer’s and other dementias is complex and likely involves the interaction of many systems,” said Ehrlich. “I’m a believer in the more infections you get in the brain, the higher your risk of Alzheimer’s. There are many pathogens that likely increase the risk. This pathobiome is not the whole answer, but it’s a piece of the puzzle.”
The exact location of the problematic bacteria within the brain is also an open question, according to the team. Researchers need to know more precisely where the bacteria are to better understand the role they are playing. The authors found that when an unhealthy pathobiome is located in the frontal lobe, the likelihood of Alzheimer’s disease being present is very high. It’s less likely to develop in the temporal lobe.
Despite the many unknowns, the authors said this is a significant step forward for studying the microbiome. The strength of our work is also to combine a breakthrough sequencing technology and the most advanced and innovative statistical approaches. Microbiome data analysis is notoriously challenging without […]
Here’s how essential oils help relieve depression symptoms

Advertisement
Aromatherapy is the practice of using essential oils – potent plant extracts that possess beneficial properties – to promote well-being and treat various health issues. This holistic treatment has been around for centuries and can be traced back to the time of the ancient Egyptians .
Today, aromatherapy is still used as an adjunct therapy in clinical practice . Clinical trials have shown that certain essential oils can be used as natural remedies for minor complaints like insomnia, nausea, loss of appetite, headaches and post-operative pain, as well as mental health-related issues like anxiety, stress and depression. (Related: Natural remedies: Treating headaches with essential oils .) Physical and cognitive symptoms of depression
Depression is a mood disorder characterized by a persistent feeling of sadness that could last for weeks or months . This condition manifests itself as a combination of cognitive and physical symptoms that greatly impact a person’s quality of life and ability to perform everyday tasks. Depression is said to affect more than 300 million people around the world and, if left untreated, could be life-threatening.
According to the National Institute of Mental Health, over 18 million American adults suffer from a depressive illness in any given year. Major depression (clinical depression), the most common and severe form of depression , is the psychiatric diagnosis most commonly associated with suicide. Research suggests that the risk of suicide among people with major depression is about 20 times that of the general population.
Common physical symptoms of depression include: Tiredness or fatigue
Insomnia or sleeping more than usual
Increased or decreased appetite
Slow speech or movements
Unexplained pain or headaches
Low libido
Constipation or diarrhea
Cognitive decline is also common among people who suffer from depression. This decline usually affects executive functioning, which encompasses a person’s ability to plan, solve problems and make decisions. Aside from executive dysfunction, other cognitive symptoms of depression include reduced attention and concentration, lower processing speed, impaired learning and poor memory. The science behind aromatherapy
Today, the first-line treatment for depression is antidepressants. Pharmaceutical companies have developed a wide variety of antidepressants to address the different symptoms of depression. However, many patients end up looking for alternatives because of the suboptimal effectiveness of these medications and the unpleasant side effects they can cause .
One of the alternatives people with depression often turn to is aromatherapy. This complementary and alternative medicine (CAM) has been shown to help alleviate symptoms of depression. In a systematic review published in the journal Evidence-Based Complementary and Alternative Medicine , researchers looked at the results of 12 randomized controlled trials and concluded that aromatherapy is an effective treatment option for relieving depression symptoms .
According to the review, aromatherapy can be administered in two ways: Individuals suffering from depression can either inhale essential oils directly or have the oils massaged on their skin. When essential oils are inhaled, their beneficial components can easily enter the bloodstream through the blood capillary network in the nose and the bronchi in the lungs.
One of the main organs targeted by essential oils is the brain. Research shows that the active components of essential oils can stimulate parts of the brain through the olfactory epithelium. Located behind the nostrils, this thin tissue is composed of neurons and supporting cells that line about half of your nasal cavity. The most important cells in the olfactory epithelium are the olfactory receptor neurons, which help transmit olfactory information to the brain.
When you inhale essential oils, their chemical components stimulate olfactory receptor neurons, which then transmit signals to your limbic system and hypothalamus. The limbic system is the part of your brain involved in emotional and behavioral responses , while the hypothalamus is the part of your brain that produces hormones responsible for controlling your body temperature, heart rate, hunger, mood, sleep and thirst.
Once the signals reach your olfactory cortex — the part of your brain concerned with the sense of smell — they trigger the release of specific brain chemicals, or neurotransmitters, like serotonin. Serotonin is a natural mood booster that is linked to feelings of happiness. Research shows that serotonin acts on different brain regions and affects a range of functions and behaviors , such as memory, fear, digestion, sleep, breathing, body temperature and stress response. Treating depression with aromatherapy
Studies at the Monell Chemical Senses Center in Philadelphia suggest that specific odors can change your mood and emotions , and these changes correlate to measurable physiological variations such as changes to your blood pressure, heart rate and body temperature. Studies also reveal that odors provide cues that trigger memory, and these memories are “more evocative and emotionally intense” than any memory triggered by other types of sensory cues.
By triggering memory associations and influencing specific parts of your brain that regulate physiological and emotional changes, aromatherapy can help relieve cognitive and physical symptoms of depression .
Here are four of the best essential oils for relieving depression symptoms , according to science: Lavender essential oil
In a study published in the journal Phytomedicine , researchers found that lavender oil in capsule form (Silexan) is just as effective at relieving generalized anxiety disorder — a common trigger of depression — as Ativan, an anti-anxiety drug. They also noted that lavender oil showed no sedative effects and was well-tolerated by participants, making it a safe natural alternative to commonly prescribed depressant medications.
Aside from anxiety, lavender oil can also help with panic attacks and general nervousness and is particularly helpful for postpartum depression . It is also a good natural remedy for restlessness, depression, anxiety and sleep disturbances that accompany post-traumatic stress disorder . Bergamot essential oil
According to a study published in the journal Neuroimmunomodulation , citrus fragrance not only helps restore homeostatic balance to the body, it could also normalize neuroendocrine hormone levels and immune function in people suffering from depression. These effects are extremely beneficial for the treatment of depression as dysregulation of neuroendocrine and immune function is associated with psychosomatic or psychiatric disorders like depression.
Among citrus oils, bergamot essential […]
Could a breakdown in the brain’s networks allow infections to contribute to Alzheimer’s disease?
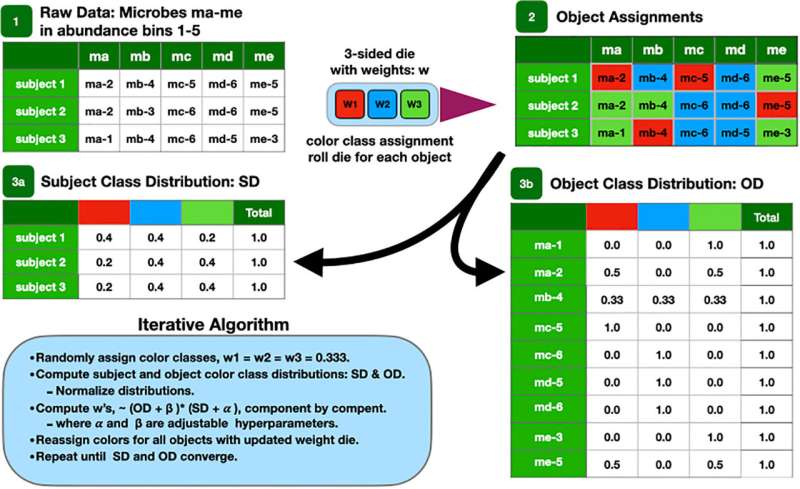
Cartoon of the LDA algorithm. Credit: Frontiers in Cellular and Infection Microbiology (2023). DOI: 10.3389/fcimb.2023.1123228 The human microbiome includes the genetic material of more than 100 trillion tiny microorganisms—fungi, yeast, bacteria, and even viruses, most of which hang out in our gastrointestinal tract to serve as guardians of our health. But when a healthy microbiome gives way to an imbalance—a “pathobiome”—any number of health problems can occur—from rheumatoid arthritis, to bacterial vaginosis.
New data published this month in the journal Frontiers in Cellular and Infection Microbiology , from researchers at Drexel’s College of Medicine, gives more evidence to the possibility that developing a pathobiome in the brain could cause some forms of Alzheimer’s and related dementias.
When biomes turn unhealthy, either by invasion of outside pathogens, or a major change in the relative numbers of the microbial species present, a dysbiosis, or imbalance in the microbiota, occurs. This dysbiosis can alter human metabolism and cause inflammation, which has been linked to the tissue damage seen in ulcerative colitis, rheumatoid arthritis and many other chronic inflammatory diseases .
Studying 130 samples from the donated brains of 32 people—16 with Alzheimer’s and 16 age-matched controls without the disease—the Drexel researchers found bacterial flora in all the brains, but the Alzheimer’s brains showed profoundly different bacterial profiles compared to their age-matched controls.
The group used full-length 16s ribosomal RNA gene sequencing, a technique that can detect any and all bacterial species present in a sample. In this process, the researchers pinpointed disease-specific sets of bacteria in almost all of the Alzheimer’s-affected brains, suggesting these groups of bacteria are strong predictors of the disease.
The authors detected five brain microbiomes, four that are hypothesized to be present at different times in the evolution of the Alzheimer’s-afflicted brains. The authors said it is likely that the observed Alzheimer’s microbiomes evolve to become more pathogenic as the disease progresses with the later stages characterized as a pathobiome.
The authors hypothesize that the brain begins with a healthy biome, but as the disease develops, the healthy biome is supplanted as a new set of microbes replace the original healthy ones with the eventual emergence of the Alzheimer’s pathobiome.
Samples from both sets of brain samples were drawn from the frontal and temporal lobes and entorhinal cortex. Based on the random distribution of microbiomes requiring delivery all over the brain, the results were consistent with failure in one or more of the brain’s networks; however it is too soon to tell if the observed distribution patterns result from a leaky blood-brain barrier, the brain’s glymphatic system, or synaptonemal transmission that allowed bacteria, including Cutibacterium acnes (formerly called Proprionibacterium acnes), Methylobacterium, Bacillus, Caulobacter, Delftia, and Variovora to enter the brain.
In Alzheimer’s brain samples, the researchers noted, these pathogenic bacteria appeared to have overpowered and replaced Comamonas sp. bacteria, which are associated with a dementia-free brain.
“Perhaps destruction of the Comamonas bacteria, part of a healthy brain microbiome, is the first sign of impending dementia,” said Garth D. Ehrlich, Ph.D., a professor in the College of Medicine, who was a senior author of the paper. “We’re now coming up with the questions to guide future studies, but the hypotheses are many. The culprit could be bacteria or something else—like fungi, parasites, or viruses—at the same time.”
When a patient has Alzheimer’s, they experience inflammation in the brain characterized by deposits of amyloid beta which are formed by an increase in the production of the Aβ peptide (an antimicrobial peptide, which is part of the innate immune response) resulting in amyloid plaques in the brain.
Similarly, Alzheimer’s is characterized by tau protein tangles found with the cells which are characterized by abnormal phosphorylation which ultimately lead to the destruction of synapses and neurons, but which have also been demonstrated to help stop the spread of pathogens in the brain.
These protein-oriented pathologies—known as the “amyloid cascade hypothesis”— have been the main focus of Alzheimer’s research for decades. Recently, studies are challenging that model by suggesting a role for bacteria, fungi and viruses, and immune system and brain inflammation, which some researchers call the “pathogen hypothesis.”
“Multiple studies have now shown the presence of bacteria in Alzheimer’s-afflicted brains,” said Jeffrey Lapides, Ph.D., an adjunct associate professor in the College of Medicine, and a senior author of the study. “Perhaps plaques, whose constituents have anti-microbial properties in vitro, aren’t the direct cause of Alzheimer’s, but instead are a response to bacteria in the brain—some benign, some pathogenic, perhaps causing damage that has not yet resulted in cognitive deficits, making them part of the pathobiome.”
This unique set of bacteria found in the Alzheimer’s-afflicted brains are also commonly found in brains afflicted with the neurodegenerative disease amyotrophic lateral sclerosis , or ALS—suggesting that this set of bacteria may contribute to more than one neurological illness.
The next step for this research, according to the authors, is to study the possible contributions of other microbes and figure out what happened, physiologically, in the brain to make this microbiome change over time.
“The development of Alzheimer’s and other dementias is complex and likely involves the interaction of many systems,” said Ehrlich. “I’m a believer in the more infections you get in the brain, the higher your risk of Alzheimer’s. There are many pathogens that likely increase the risk. This pathobiome is not the whole answer, but it’s a piece of the puzzle.”
The exact location of the problematic bacteria within the brain is also an open question, according to the team. Researchers need to know more precisely where the bacteria are to better understand the role they are playing. The authors found that when an unhealthy pathobiome is located in the frontal lobe, the likelihood of Alzheimer’s disease being present is very high. It’s less likely to develop in the temporal lobe.
Despite the many unknowns, the authors said this is a significant step forward for studying the microbiome.
“The strength of our work is also to combine a breakthrough sequencing technology and the most advanced and innovative statistical approaches,” said lead author Yves Moné, Ph.D., a research associate in the College […]
Aromatherapy May Lead to a 226% Boost in Cognition

Certain aromas can help build better brains—and memories—during sleep.
Smell is directly linked to memory.
Scents may offer a safe and possibly beneficial option to boost brain health.
Source: Palo Cech/ Pexels You know those small vials of fragrant oils sometimes placed on a hotel pillow to calm a guest and improve sleep? Well, science says they work, even suggesting certain aromas can help build better brains—and memories—during sleep.
Researchers writing in a July 2023 issue of Frontiers in Neuroscience contend “ olfactory enrichment”—inhaling pleasant fragrances during sleep—influences brain function in ways that significantly improve cognition and boost memory . How Scientists Conducted the Study
Of 43 study participants—all healthy men and women between the ages of 60 and 85—20 underwent two hours of aromatherapy nightly. Seven different fragrant oils were dispersed through a room diffuser on a rotating basis—a different one each night—for a period of six months. When compared to the control group, the 20 volunteers registered a whopping 226 percent increase in cognitive capacity as measured by a word list test commonly used to evaluate memory.
The exact protocol is as follows: Participants provided an odorant diffuser made by Diffuser World
Provided seven essential oils: rose, orange, eucalyptus, lemon, peppermint, rosemary, lavender
Participants were asked to turn on the diffuser before bedtime—producing scent for two hours
Rotate through different scents each night
Continue nightly for six months
While this study was conducted in older adults aged 60-85, with no cognitive issues at all, there is some chance this may help younger groups as well. At a minimum, the side effects, or risks of sleeping with scented aromas, are quite minimal.
The finding supports past studies, including a 2021 report in the journal Geriatric Nursing indicating olfactory stimulation could prove a “simple and convenient new intervention for alleviating, maintaining [and managing] cognitive function and [behavior and psychological symptoms] in older adults with dementia .”
So, why is the sense of smell so critical to cognition, emotion , and general neural function? Smell Directly Linked to Memory
Unlike the other senses, such as eyesight and hearing, the olfactory nerves are linked directly to a white matter pathway in the brain—the uncinate fasciculus—which plays a significant role in learning and memory encoding. It is part of the brain’s limbic system, which governs emotions and behavior.
It is this pathway that deteriorates due to aging and the development of neurodegenerative disorders like Alzheimer’s and Parkinson’s disease, authors of the July 2023 journal article state. In fact, the sense of smell is much like the canary in the cave, where the bird’s sensitivity to adverse conditions and resulting death, is a warning to miners to get out quickly. Loss of smell can prove a warning of the onset of some 70 different neurological disorders or neural infections. Traumatic brain injuries can also modify or interfere with olfactory discrimination .
The researchers were quick to point out that olfactory stimulation does not directly affect areas of the brain responsible for controlling sleep. However, they say the use of natural fragrances can deepen slow-wave sleep. Slow-wave sleep is considered “the most restful portion of the sleep cycles,” study authors write. “Odorants enhance normal sleep, and…also improve abnormal sleep at a magnitude similar to that of sleep medications.”
Meanwhile, the National Sleep Foundation says that smell can affect “how long it takes to fall asleep, [as well as] overall sleep quality and quantity. Distinct scents may promote better sleep, help people wake up in the morning, or even [potentially] influence dreams and memory formation during sleep.”
Key components of what is defined as “quality sleep” include duration, continuity (number of times one awakens during the night), and amount of beneficial slow wave (deep) sleep, which is important in enhancing memory, strengthening the immune system, repairing bone and tissue, and regenerating cells. Lavender Most Studied, But Other Oils Also Beneficial
The most studied fragrance for improving sleep has been lavender, but past reports also cite the appealing effects of natural oils like jasmine, rose, and Roman chamomile, which reportedly is effective in easing anxiety and depression , and even cedarwood. All of these are extracts derived from plants.
In a 2021 article published in Complementary Therapies in Medicine , authors review 30 aromatherapy studies and conclude the use of fragrant oils has a “statistically significant” effect on improving sleep quality and reducing “ stress , pain, anxiety, depression, and fatigue.” Indeed, aromatherapy also appears effective for controlling cases of acute insomnia , they state. And now, of course, the latest study indicates the smell of these oils can make the user smarter in terms of cognition, recall, and judgment.
The therapeutic effects of natural fragrances are not a new concept. Pedanius Discorides, a Greek physician considered the father of pharmacognosy, discussed the medicinal properties of natural plant oils in his book De Materia Medica , written in the first century. Later, in the 12th century, Saint Hildegard, a German Benedictine abbess, composer, philosopher, and medical writer, used distilled lavender for healing purposes. Finding the Best Way to Use Fragrances
Having a scientifically approved approach to enhancing sleep quality, while building cognition and memory, through the use of natural fragrances could benefit tens of thousands of Americans. Impaired sleep is reaching epidemic proportions in the United States. The National Sleep Foundation estimates more than a third of adults fail to sleep the required number of hours. The Centers for Disease Control and Prevention says the number is closer to 35 percent.
Chronic insomnia and other forms of sleep deprivation are linked to a variety of physical, mental, and psychological symptoms. These include mood shifts and increased irritability, concentration and attention problems, failures in judgment and executive decision-making , physiological changes, such as impairments in brain function and hormone production, reduced immunity protection from disease, overstimulated appetite and weight gain, higher risk for diabetes and various dementias, an overactive nervous system , chronic fatigue—even earlier death. This list includes a range of psychiatric disorders, including elevated anxiety, depression, and obsessive compulsiveness.
As the […]
Fundamental Biology Overturned: New Discovery Challenges Long-Held Views on “The Second Brain”

The enteric nervous system (ENS), often called the second brain, plays a crucial role in digestion, immunity, and communication with the brain. Researchers have discovered that ENS development continues after birth and includes neurons derived from mesoderm, challenging long-held scientific beliefs and opening avenues for potential new treatments for aging and gastrointestinal diseases. Discoveries may pave the way for improved therapies for gastrointestinal issues.
Following your gut. Losing your appetite. A gutsy move. Though we often consider the gut as merely a digestive tool, these common expressions reflect the central role the gut plays in a much wider range of essential functions.
The entire digestive tract is lined by the enteric nervous system (ENS), a vast network of millions of neurons and glial cells—the two primary cell types also found in the central nervous system. While often called the second brain, the ENS not only generates the same neurotransmitters but actually predates the evolution of the central nervous system in the brain.
The functions of the ENS are crucial to life and extend far beyond digestion, as it regulates immunity, gut secretions, and enables complex, bi-directional communication between the gut and the brain. This is why a happy gut co-exists with a happy brain, and why digestive issues can lead to changes in mood and behavior.
Since the mid-20 th century, scientists have believed that the ENS is derived from the neural crest before birth and remains unchanged after. Now, in a paper published in the journal eLife , researchers at Beth Israel Deaconess Medical Center (BIDMC) present a completely new paradigm describing a developmental pathway by which ENS development continues after birth in mice and human tissue samples.
This discovery overturns decades of scientific dogma on the fundamental biology of neuroscience and of ENS, by showing evidence for the first time of a non-ectodermal and a mesodermal origin for large numbers of enteric neurons born after birth. The findings show the relevance of these neurons to the maturation and aging of the ENS in health and disease.
“These results indicate for the first time that the mesoderm is an important source of neurons in the second largest nervous system of the body,” said Subhash Kulkarni, Ph.D., a staff scientist at BIDMC and an assistant professor in the Division of Medical Sciences at Harvard Medical School. “How we mature and how we age is central to our understanding of health and disease in our rapidly aging population. The increasing proportion of neurons of mesodermal lineage is a natural consequence of maturation and aging; further, this lineage can be expected to have distinct vulnerabilities to disease.”
Using transgenic mice models, high-resolution microscopy, and genetic analyses, Kulkarni and colleagues analyzed the ENS neuronal populations in adult mice and human tissues. Using mice models, the team found that while the early post-natal ENS cells were from the expected neural crest lineage, that pattern changed rapidly as the animal matured. Kulkarni and colleagues documented the arrival and continual expansion of a novel population of enteric neurons that were derived from the mesoderm—the same lineage that gives rise to the muscle and heart cells.
This newly discovered population of mesoderm-derived neurons expanded with age, such that they comprised a third of all enteric neurons in adolescent mice, half of all enteric neurons in adult mice, and then eventually outnumbered the original neural crest-derived population of enteric neurons in aging mice.
By assessing the molecular signature of these neurons, the team identified new cellular markers that were used to identify this population of mesoderm-derived neurons in human gut tissue. These markers also provided pharmacological targets, which the researchers used to not only manipulate the proportions of the mesodermal neurons in adolescent mice but also reduce their dominant proportions in the aging mouse gut to cure age-associated slowing of gut movement.
“We can now work to understand how these findings can be translated into human systems to provide a disease-modifying cure to aging patients whose chief complaint often includes diseases of the GI tract,” added Kulkarni. “By reversing one of the biggest dogmas of neuroscience, we are now in uncharted territory and, at the same time, have a huge opportunity to understand this hidden basic, translational, and clinical biology of neurons. The newly discovered lineage of neurons presents us with potential new drug targets that could help large populations of patients.”
Reference: “Age-associated changes in lineage composition of the enteric nervous system regulate gut health and disease” by Subhash Kulkarni, Monalee Saha, Jared Slosberg, Alpana Singh, Sushma Nagaraj, Laren Becker, Chengxiu Zhang, Alicia Bukowski, Zhuolun Wang, Guosheng Liu, Jenna Leser, Mithra Kumar, Shriya Bakhshi, Matthew Anderson, Mark Lewandoski, Elizabeth Vincent, Loyal A. Goff and Pankaj Jay Pasricha, 7 August 2023, eLife .
DOI: 10.7554/eLife.88051.1
Co-authors included Monalee Saha, Jared Slosberg, Alpana Singh, Sushma Nagaraj, Chengxiu Zhang, Alicia Bukowski, Zhuolun Wang, Guosheng Liu, Jenna Leser, Mithra Kumar, Shriya Bakhshi, Elizabeth Vincent, and Loyal A. Goff of Johns Hopkins University School of Medicine; Laren Becker and of Stanford University School of Medicine; Matthew Anderson and Mark Lewandoski of Center for Cancer Research, National Cancer Institute; and Pankaj Jay Pasricha of the Mayo Clinic.
The microscopy was performed on the Ross Imaging Core at the Hopkins Conte Digestive Disease Center at the Johns Hopkins University (P30DK089502) using the Olympus FV 3000rs (procured with the NIH-NIDDK S10 OD025244 grant). The 10X Genomics Chromium processing for scRNAseq was performed at the GRCF Core and the sequencing was performed at the CIDR core at the Johns Hopkins University. This work was supported through a grant from the Ludwig Foundation, a grant from the NIA (R01AG066768), a pilot award from the Hopkins Digestive Diseases Basic & Translational Research Core Center grant (P30DK089502), a pilot award from the Diacomp initiative through Augusta University; a Johns Hopkins Catalyst Award; the Maryland Genetics, Epidemiology, and Medicine training program sponsored by the Burroughs Welcome Fund; the Hopkins Conte Digestive Disease Center at the Johns Hopkins University (P30DK089502); NIDDK (R01DK080920); the Maryland Stem Cell Research Foundation (MSCRF130005), and a grant from the AMOS family.
Zebrafish study unravels how the brain orchestrates motion
The zebrafish brain, though simpler than its human counterpart, is a complex network of neurons that engage in a ceaseless dance of electrical activity. What if this neural ballet could reveal the secrets of how brains, including our own, control movement? A zebrafish study led by researchers at the Champalimaud Foundation offers a new lens through which to view the activity of neural populations, and to understand how the brain orchestrates motion. Why we have a brain
“The brain’s primary function is movement”, explains Claudia Feierstein, lead author of the study published today in Current Biology . “Plants don’t need a brain because they don’t move. Yet, even for something as seemingly simple as eye movements, the brain’s role remains largely enigmatic. Our goal is to illuminate this ‘black box’ of motion and to decode how neural activity controls eye and body movements, using zebrafish as our model organism”.
With their tiny transparent bodies, zebrafish have become the darlings of neuroscience, offering a unique window into brain function. Eye movement is a circuit that’s conserved across species, including humans. If we can understand how it works in zebrafish, we can start to understand better how human brains do movement”. Claudia Feierstein, lead author of the study Zebrafish, like humans, possess an innate ability to stabilize their vision and position in response to movement. When the world around them spins, their eyes and body move in tandem to maintain stability. This is akin to us steadying our gaze on a fixed point while on a merry-go-round.
But how does the brain coordinate this behavior? Previous research by the team had shown that different parts of the zebrafish brain were associated with different types of movements. However, the precise relationship between these brain areas and the actual behavior remained unclear. “While we know that neurons are involved in detecting visual stimuli (the input) and controlling muscles (the output), we remain in the dark about the processing in between”, remarks Feierstein. Complicating matters is the plethora of stimuli to which neurons respond and the staggering amount of data captured by whole-brain imaging studies. “When you have tens of thousands of neurons and 100 different possible behaviors that they could encode, it’s not trivial to understand what is going on”.
As Michael Orger, one of the two senior authors, elaborates, “When you look at the activity of individual neurons, you find that they can respond to multiple behavioral variables. This makes it challenging to pinpoint what exactly is driving their activity”. This leads to a complex interplay between neurons and behavior, where individual neurons can be involved in multiple types of movements. A new analytical approach
To tackle this challenge, the researchers initially used a statistical method known as linear regression to explore the relationship between behavioral variables and neuronal activity. However, they quickly realized that examining neurons one by one did not provide a clear understanding of the overall picture. It was like trying to understand a grand-scale dance performance featuring hundreds of dancers by only watching one dancer’s moves. “We started by looking at individual neurons but soon realized that we needed to understand the ensemble, the whole dance troupe if you will”, says Feierstein. “So we incorporated what’s known as a ‘dimensionality reduction’ step in our analysis to get a zoomed-out view of what the population of neurons is doing”.
As Christian Machens, the study’s other senior author, points out, “We wanted to know: how does the overall activity that we measure relate to behavior? How can we boil down the activity of tens of thousands of neurons to its essential features? It took a considerable amount of time to develop the analytical approach for this. But once we managed to overcome these challenges, we could finally ask: how does the overall activity of these neurons relate to specific behaviors, like eye movement or swimming?”.
In the study, zebrafish were embedded in agarose, a gel-like substance, to keep them in a fixed position so that the researchers could image the brain. The agarose near their eyes and tails was removed to allow for movement. “We then put images on a screen below the zebrafish and recorded brain activity with a fluorescent dye through a microscope”, describes Feierstein. Unveiling the brain’s choreography
By applying their analytical approach to a region of the zebrafish brain called the hindbrain, the researchers were able to condense the cacophony of neuronal activity into two main ‘features’, or patterns of activity, that corresponded to specific types of movements, and are presumably generated by separate circuits in the zebrafish hindbrain.
The first circuit they found is primarily concerned with eye movements, specifically the rotation of the eyes, either clockwise or anti-clockwise. Imagine a fish seeing something spin around in its environment. To keep a stable view of this spinning object, the fish’s eyes also rotate, and its tail may move. Essentially, this circuit helps the fish adjust its eyes to keep a constant and stable image of what it’s seeing. As Feierstein elucidates, “It’s like the brain’s way of saying, ‘Okay, the world is spinning around me, I need to move my eyes to keep track of it'”. Moreover, the researchers discovered that neurons associated with leftward and rightward rotation were anatomically segregated in the left and right hemispheres of the brain, respectively.
The second circuit is more involved in what researchers call ‘vergence’ and tail movement. Vergence is the ability of the eyes to move in opposite directions – both eyes moving towards or away from the nose – in response to stimuli. This circuit comes into play when the fish perceives a stimulus moving from back to front. Feeling as though it’s drifting backward, the fish swims forward to stabilize its position. At the same time, its eyes converge to maintain a stable image. Consequently, this circuit helps the fish adjust its body and eye movements to stay in a stable position.
As Orger summarises, “One brain circuit is primarily concerned with eye movements, particularly rotation, to maintain a stable image on the […]
Pitt neuroscientists create first non-human primate model of hereditary Alzheimer’s in marmosets
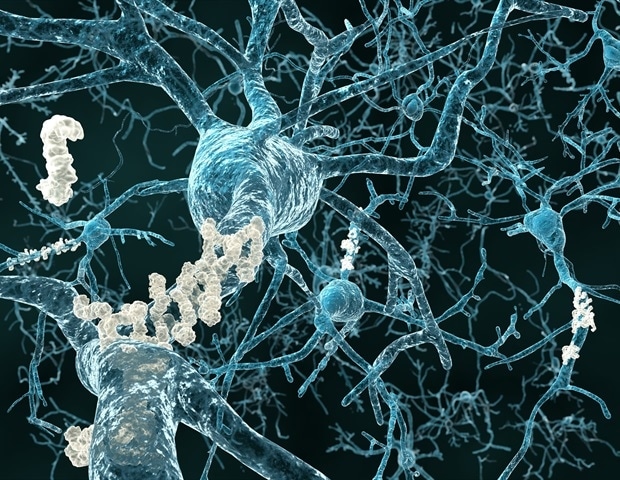
To reimagine existing preclinical trials for Alzheimer’s disease, University of Pittsburgh School of Medicine neuroscientists created the first non-human primate model of hereditary Alzheimer’s in marmoset monkeys, outlining their approach in Alzheimer’s & Dementia: Translational Research & Clinical Interventions .
Researchers are now working on characterizing and validating genetic, molecular, functional and cognitive features of aging and Alzheimer’s disease in marmosets that harbor mutations in the same gene that is linked to early-onset disease in humans. Scientists hope to accelerate the pace of the drug discovery pipeline and rebuild the foundation for future translational studies while overcoming limitations inherent to existing preclinical models. We are ambitious about finding a cure for Alzheimer’s disease. We are establishing a process for rigorous, minimally invasive standardized testing of the marmoset model of Alzheimer’s disease and openly sharing data.” Afonso Silva, Ph.D., senior author, professor of neurobiology at Pitt Marmoset families are better matched to mimic the genetically diverse human population than a colony of inbred rodents. And because marmosets’ life spans are shorter than those of other non-human primates, researchers can comprehensively study their aging within a relatively short period of time.
If allowed to age naturally, marmosets will spontaneously develop aggregates of toxic amyloid beta and tau indicative of Alzheimer’s-like pathology in the brain. To create marmosets with inheritable predisposition to Alzheimer’s disease, researchers introduced a series of mutations in the PSEN1 gene using the Crispr/Cas9 gene engineering system. These same mutations cause early onset Alzheimer’s disease in humans.
Presenilin-1, the protein encoded by PSEN1, plays a key role in generating amyloid tangles, and, just like human patients, marmosets with a mutation in the PSEN1 gene start developing Alzheimer’s-like pathologies during adolescence.
In establishing the model, the team is applying a bench-to-bedside approach to marmosets as though they were human patients. To characterize and validate the new model, researchers are employing a battery of non-invasive tests, including behavioral studies, longitudinal analysis of blood biomarkers, and regular PET scans to assess brain function and pathological changes in the brain tissue. The tests are designed to map out and compare the aging trajectory between healthy controls and animals genetically predisposed to early-onset Alzheimer’s and correlate progressive changes in the levels of amyloid and tau to changes in cognition.
Researchers also plan to look into other factors that accompany disease progression, including brain-blood barrier permeability, vascular stiffness and metabolism, as well as analyze changes in gene expression profiles over time by regularly sampling skin cells.
“We need new models to understand underlying biological processes behind normal and pathological aging,” said lead and corresponding author Stacey Rizzo, Ph.D., associate professor of neurobiology and deputy director for preclinical research at Pitt’s Aging Institute. “Tracking the animals from birth in a well-controlled way would allow us to hypothesize on how molecular and genetic changes translate to pathophysiological consequences in the brain and devise ways to stop them from getting to the point of no return.”
In 2022, Rizzo and Silva received a five-year, $32.5 million grant from the National Institutes of Health to conduct this project.
Additional authors of the study are Gregg Homanics, Ph.D., David Schaeffer, Ph.D., Lauren Schaeffer, M.S., Jung Eun Park, M.S., Ph.D., Julia Oluoch, Tingting Zhang, Ph.D., Takeshi Murai, Ph.D., Sang Ho Choi, Ph.D., Hasi Huhe, Ph.D., Julia Kofler, M.D., and Peter Strick, Ph.D., all of Pitt, as well as collaborators from The Jackson Laboratory, Emory University, University of California Santa Cruz and Sage Bionetworks.
This work is supported by the National Institutes of Health, National Institute on Aging (grant U19AG074866) and UPMC-ITTC IPA 2019 NO.16 grant. Support from DSF Charitable Foundation Grant 1805R01 provided resources to enable this research.
Source:
University of Pittsburgh
Journal reference:
Sukoff Rizzo, S. J., et al. (2023) Bridging the rodent to human translational gap: Marmosets as model systems for the study of Alzheimer’s disease . Alzheimer’s & Dementia Translational Research & Clinical Interventions . doi.org/10.1002/trc2.12417 .
Study Suggests Melatonin Could Have A Huge Positive Effect on Memory Function

Experts recommend that adults sleep at least 7 hours every night. Unfortunately, a lot of people don’t meet up with this requirement as they struggle with falling or staying asleep. Many people in this category have insomnia, the most common sleep disorder known to man. According to the Center for Disease Control (CDC), such people made up more than ¼ of the American adult population as of 2020.
From sleep hygiene to healthy dieting, mindfulness, yoga, physical activity, and therapeutic approaches, there are many recommended coping strategies for insomnia. However, the one that seems to be gaining the most attention recently is melatonin supplements. The brain produces melatonin in response to darkness, and the supplements help to increase the levels of melatonin hormones in the bloodstream. Taking these supplements helps to regulate the body’s circadian rhythm (sleep-wake cycle) by sending signals to the body that it’s time to take a nap.
However, more than just helping to manage insomnia, new findings show that melatonin may also have memory-enhancing effects. The study was motivated by concerns that melatonin could be harmful to the brain after some users felt groggy when they woke up. Furthermore, research from Japan also indicates that these advantages can be noticed on a microscopic scale.
Tokyo’s Sophia University scientists critically examined melatonin, N1-acetyl-5-methoxyquinuramine (AMK), melatonin’s biological metabolite, and ramelteon, with the aim of determining their effects on memory function. While AMK biologically metabolizes melatonin, ramelteon activates and binds the melanin receptor. The results showed that melatonin and its derivatives were able to trigger microscopic changes in mouse brains.
Since phosphorylation is necessary for forming both short and long-term memories, the researchers also included protein extracellular signal-regulated kinase (ERK), calcium/calmodulin-dependent kinase IIα (CaMKIIα), CaMKIIβ, CaMKIV, and the cAMP-response element binding protein (CREB), in their study.
In the words of Atsuhiko Chiba, the study’s lead author, “Our study aimed to investigate the effects of melatonin, ramelteon, and N1-acetyl-5-methoxyquinuramine (AMK) on the relative phosphorylation levels of memory-related proteins in order to explore candidate signaling pathways associated with the receptor- and nonreceptor-mediated memory-enhancing effects of melatonin.”
Speaking on the result of the study, he said it suggests that “melatonin is involved in promoting the formation of long-term object recognition memory by modulating the phosphorylation levels of memory-related proteins such as ERK, CaMKIIs, and CREB in both receptor-mediated and nonreceptor-mediated signaling pathways.”
In other words, melatonin plays a significant role in improving or creating long-term memory. This is good news for the older population as their memories generally decline as they age. The team believes that further research may lead to the formulation of melatonin-based treatments for people with age-related memory concerns.
An article published on the “Clinical Aspects of Melatonin Intervention in Alzheimer’s Disease Progression” in PubMed Central agrees with the need for further study on this subject. “Although there is evidence to postulate melatonin as a useful ad-on therapeutic tool in MCI, larger double-blind multicenter studies are urgently needed to further explore and investigate the potential and usefulness of melatonin as an antidementia drug. Its apparent usefulness in symptomatic treatment, concerning sleep, sundowning or cognitive impairment, even in a progressed state, further underlines the need for such decisive studies,” it reads.
Trying to Train Your Brain Faster? Knowing This Might Help With That
Credit: Andriy Onufriyenko / Getty Images Are you working really hard to learn something? Remember this counterintuitive fact, and you might improve your learning curve. Full Transcript
SUBSCRIBE: Apple | Spotify
Hi Science, Quickly listeners. This is Jeff DelViscio, executive producer of the show.
The whole podcast team is out in the field, so while we’re away, we’re bringing back a few amazing oldies from the archive.
Today we dive into your brain during bouts of intense learning…maybe that happens to you when you listen to this podcast? Perhaps?
Producer Karen Hopkin brings us a study that looked at brain training…and how rest might be the key to training your brain even faster.
The episode was first aired on July 21, 2021 –when we were still called 60-Second Science. Ah, memories.
Enjoy!
—
Karen Hopkin : This is Scientific American’s 60-Second Science. I’m Karen Hopkin.
They say that practice makes perfect.
[CLIP: Piano sounds]
Hopkin : But sometimes the best practice is not on a keyboard …
[CLIP: Piano sounds]
Hopkin : It’s all in your head. Because a new study shows that the brain takes advantage of the rest periods during practice to review new skills, a mechanism that facilitates learning. The work appears in the journal Cell Reports . [Ethan R. Buch et al., Consolidation of human skill linked to waking hippocampo-neocortical replay ]
Leonardo Cohen : A lot of the skills we learn in life are sequences of individual actions.
Hopkin : Leonardo Cohen of the National Institute of Neurological Disorders and Stroke , or NINDS.
Cohen : For example, playing a piece of piano music requires pressing individual keys in the correct sequence with very precise timing.
[CLIP: Piano music]
Hopkin : That level of virtuosity requires a ton of practice and a lot of repetition. But Cohen says it also requires a certain amount of rest.
Cohen : We know from previous research that interspersing rest with practice during training is advantageous for learning a new skill. In fact, we recently showed that virtually all early skill learning is evidenced during rest rather than during the actual practice.
Hopkin : It’s during those intermittent breaks that the brain starts to sew together the individual movements that make up a seamless piece.
[CLIP: Piano music]
Hopkin : The question then becomes: How? To find out, Cohen and his colleagues turned to an imaging technique called magnetoencephalography , or MEG.
Ethan Buch : The unique advantage of MEG is that it allows us to observe neural activity across the entire brain with millisecond time resolution, which is crucial for investigating very fast widespread brain dynamics.
Hopkin : Ethan Buch , Cohen’s colleague at NINDS. They and their team had 30 volunteers sit inside an MEG scanner. And they asked them to type the sequence 41324 on a keyboard as quickly and accurately as possible.[CLIP: Sounds of typing] Hopkin : The participants would type for 10 seconds, then rest for 10 seconds, then repeat while the researchers monitored their neural activity. Buch : And what we found was really quite interesting. So we actually found that the brain kept replaying much faster versions of the practice activity patterns over and over again during rest. Hopkin : So a sequence that might take one second for fingers to type …[CLIP: Sounds of typing] Hopkin : … would take just 50 milliseconds for the brain to replay.[CLIP: Sounds of typing] Buch : That’s an impressive 20-fold compression. Hopkin : The regions most active were those involved in controlling movement and representing sequences. And the more often the brain repeated the sequence, the faster the subject improved. Buch : When the participants were beginning to learn the skill, they were initially typing about five to six repetitions of the sequence during each 10 seconds of practice. But during rest, the brain replayed about 25 repetitions of the sequence, and that’s a fivefold increase over the same amount of time. Hopkin : That lightning-quick neural rehearsal supercharges learning and memory. Buch : It’s as if the brain actively exploits these rest periods to amplify the effects of practice and rapidly consolidate the skill memory. And this actually appears to be this skill-binding mechanism that we were looking for. Hopkin : So next time you sit down to practice …[CLIP: Piano music] Hopkin : Give yourself a break—or a lot of little breaks. Your brain, and your audience, will thank you.[CLIP: Piano music] Hopkin: For Scientific American’s 60-Second Science, I’m Karen Hopkin. SUBSCRIBE: Apple | Spotify [ The above text is a transcript of this podcast .] Rights & Permissions ABOUT THE AUTHOR(S) Karen Hopkin is a freelance science writer in Somerville, Mass. She holds a doctorate in biochemistry and is a contributor to Scientific American ‘s 60-Second Science podcasts. Recent Articles by Karen Hopkin Parrot Babies Babble Just like Us The Scientific Secret to Soothing Fussy Babies Why Your Dog Might Think You’re a Bonehead
Here are 10 kiwifruit benefits you shouldn’t miss out on

Advertisement
With its jade-green flesh, tiny black seeds and naturally sweet taste, the humble little kiwifruit makes a great addition to a healthy diet.
Kiwifruit, which is widely cultivated in New Zealand, California, Italy, Chile, France and Greece, is known for its wealth of essential nutrients, antioxidants and other beneficial plant compounds. The well-documented health benefits of this superfruit are definitely something you shouldn’t miss out on. (Related: 8 Science-backed health benefits of eating kiwi .) All types of kiwifruit are nutrient-dense
Kiwifruit is a great source of 20 vitamins, including vitamins A, B3 (niacin), B9 (folate), C (ascorbic acid), E and K, and minerals like copper, magnesium and potassium.
They also contain an array of other nutrients, notably nutritionally relevant levels of dietary fiber as well as a wide range of antioxidants, bioactive enzymes and phytonutrients that provide functional and metabolic benefits.
Although traditional kiwifruit has green flesh, there are a few different types of equally delicious kiwifruit varieties, such as the golden kiwifruit, which has yellow flesh and is sweeter than the green variety.
Unlike green kiwifruit, you can eat a golden kiwifruit just as you would an apple. Eating the golden kiwifruit’s skin is a great way to increase the amount of fiber you get from the fruit from two to four grams per serving. Kiwifruit can support healthy immune function
Kiwifruit is known for having the highest vitamin C content among commonly eaten fruits, providing 290 percent of the Daily Value (DV) for vitamin C per serving.
Currently, the recommended DV for vitamin C for children aged 4 and above and adults is 60 milligrams (mg) regardless of gender, according to the Institute of Medicine . Vitamin C helps strengthen the immune system, aids in collagen production and wound healing, and acts as an antioxidant that protects cells from free radical damage. Kiwifruit can boost digestion
According to a study published in the European Journal of Nutrition , kiwifruit offers digestive benefits not only for healthy individuals but also for people who suffer from constipation and other gastrointestinal disorders, including symptoms of irritable bowel syndrome.
The fiber in kiwifruit is said to have great water retention capacity, which can help improve stool consistency and support regular bowel movement. Eating fiber-rich kiwifruit can also bring about favorable changes in the composition of your gut microbiota that favors the production of beneficial metabolites. In addition, studies show that the predominant enzyme in kiwifruit, actinidin, can support healthy digestion . Kiwifruit can reduce your risk of developing cancer
According to a review of clinical and cell culture studies, adding kiwifruit to a healthy diet is an excellent way to fight or prevent cancer , particularly colorectal cancer. This is because kiwifruit contains plenty of active components that have direct and indirect anticancer activities.
Research suggests that the direct anticancer effects of kiwifruit involve the reduction of oxidative damage to DNA, which is mediated by ascorbic acid (vitamin C). Meanwhile, the indirect anticancer effects of kiwifruit can be attributed to its ability to improve digestion and support bowel regularity, which helps reduce one’s risk of colorectal cancer. Kiwifruit has cardioprotective properties
A study published in Advances in Food and Nutrition Research reported that kiwifruit can help prevent cardiovascular disease (CVD). In fact, studies show that eating two or three kiwifruits a day can help reduce platelet hyperreactivity and lowers blood cholesterol as well as blood pressure.
Platelet hyperreactivity can increase your risk of heart disease because platelets can stick to blood vessel walls and contribute to plaque buildup – a condition known as atherosclerosis. Aside from CVD, platelet hyperreactivity has also been associated with sickle cell disease, inflammatory bowel disease , rheumatoid arthritis, diabetes, Alzheimer’s disease and cancer. Kiwifruit helps keep your bones strong
One kiwifruit contains 31 percent of your daily recommended intake of vitamin K, which helps improve bone mineral density . Maintaining optimal bone mineral density is important for preventing osteoporosis and osteoarthritis, especially among older adults. Kiwifruit can help you maintain younger-looking skin
Kiwifruit contains high amounts of vitamin E, an antioxidant that can protect your skin from damage caused by ultraviolet B rays from the sun. Vitamin E can also help prevent lipid peroxidation and collagen cross-linking — two events that have been linked to premature skin aging. Kiwifruit promotes good-quality sleep
Kiwifruit contains many medicinally useful compounds, some of which can help with sleep disorders. For instance, kiwifruit is a rich source of the amino acid tryptophan , which is a precursor to serotonin and melatonin. Serotonin is a brain chemical that influences mood, cognition and sleep , while the hormone melatonin also plays a role in your sleep-wake cycle.
In a study published in the Asia Pacific Journal of Clinical Nutrition , Taiwanese researchers found that participants with self-reported sleep disturbances who ate two kiwifruits one hour before bedtime experienced significant improvements in sleep duration and overall sleep quality , suggesting that kiwifruit has potent sleep-promoting properties. Kiwifruit can support eye health
Kiwifruit contains high amounts of two carotenoids, namely, lutein and zeaxanthin. These antioxidants are abundantly present in eye tissue and help protect your eyes from oxidative damage. Studies show that lutein and zeaxanthin can also help delay the progression, or even reduce your risk , of chronic eye diseases.
According to Drs. Sherri Nordstrom Stastny and Julie Garden-Robinson from North Dakota State University , one cup of kiwifruit contains 220 micrograms of lutein and zeaxanthin, which can help rebuild your macula and prevent age-related macular degeneration .
Additionally, a cup of sliced kiwifruit contains 167 mg of vitamin C, which is twice the amount you can get from an orange. Researchers recommend consuming vitamin C-rich foods to maintain healthy vision because vitamin C and other antioxidants help repair damaged cells and promote the growth of new cells.
A cup of kiwifruit can also provide about 20 percent of the recommended daily intake for copper, which is important for maintaining a healthy nervous system. This is important for improving the function of your retina , which houses the nerves that convert images […]
Fireflies, brain cells, dancers: new synchronisation research shows nature’s perfect timing is all about connections

This is the case in the brain, for example, where there is a complex network structure of connections between different regions.Real complex systems like this, where there is no central guiding signal and oscillators are connected in a complex network, are very robust to damage and adaptable to change, and can more easily scale to different sizes.Stronger sync comes from more wandering walks One drawback of such complicated systems is for scientists, as they are mathematically difficult to come to grips with.
Representative Image Image Credit: pixabay.com Getting in sync can be exhilarating when you’re dancing in rhythm with other people or clapping along in an audience. Fireflies too know the joy of synchronisation, timing their flashes together to create a larger display to attract mates.
Synchronisation is important at a more basic level in our bodies, too. Our heart cells all beat together (at least when things are going well), and synchronised electrical waves can help coordinate brain regions – but too much synchronisation of brain cells is what happens in an epileptic seizure. This is a modal window.
No compatible source was found for this media.
Sync most often emerges spontaneously rather than through following the lead of some central timekeeper. How does this happen? What is it about a system that determines whether sync will emerge, and how strong it will be? In new research published in Proceedings of the National Academy of Sciences, we show how the strength of synchronisation in a network depends on the structure of the connections between its members – whether they be brain cells, fireflies, or groups of dancers.
The science of sync Scientists originally became interested in sync to understand the inner workings of natural systems. We have also become interested in designing sync as a desired behaviour in human-made systems such as power grids (to keep them in phase).
Mathematicians can analyse sync by treating the individuals in the system as “coupled oscillators”. An oscillator is something that periodically repeats the same pattern of activity, like the sequence of steps in a repetitive dance, and coupled oscillators are ones that can influence each other’s behaviour.
It can be useful to measure whether a system of oscillators can synchronise their actions, and how strong that synchronisation would be. Strength of synchronisation means how well the sync can recover from disturbances.
Take a group dance, for example. A disturbance might be one person starting to get some steps wrong. The person might quickly recover by watching their friends, they might throw their friends off for a few steps before everyone recovers, or in the worst case it might just cause chaos.
Synced systems are strong but hard to unravel Two factors make it difficult to determine how strong the synchronisation in a set of coupled oscillators could be.
First, it’s rare for a single oscillator to be in charge and telling everyone else what to do. In our dance example, that means there’s neither music nor lead dancers to set the tempo.
And second, usually each oscillator is only connected to a few others in the system. So each dancer can only see and react to a few others, and everyone is taking their cues from a completely different set of dancers. This is the case in the brain, for example, where there is a complex network structure of connections between different regions.
Real complex systems like this, where there is no central guiding signal and oscillators are connected in a complex network, are very robust to damage and adaptable to change, and can more easily scale to different sizes.
Stronger sync comes from more wandering walks One drawback of such complicated systems is for scientists, as they are mathematically difficult to come to grips with. However, our new research has made a significant advance on this front.
We have shown how the network structure connecting a set of oscillators controls how well they can synchronise. The quality of sync depends on “walks” on a network, which are sequences of hops between connected oscillators or nodes.
Our maths examines what are called “paired walks”. If you start at one node and take two walks with randomly chosen next hops for a specific number of hops, the two walks might end up at the same node (these are convergent walks) or at different nodes (divergent walks).
We found that the more often paired walks on a network were convergent rather than divergent, the worse the synchronisation on the network would be. When more paired walks are convergent, disturbances tend to be reinforced.
In our dancing example, one person making the wrong steps might lead some neighbours astray, who may then lead some of their neighbours astray and so on.
These chains of potential disturbances are like walks on the network. When those disturbances propagate through multiple neighbours and then converge on one person, that person is going to be much more likely to copy the out-of-sync moves than if only one of their neighbours was offbeat.
Social networks, power grids and beyond So networks with many convergent walks are prone to poorer synchronisation. This is good news for the brain avoiding epilepsy, as its highly modular structure brings a high proportion of convergent walks.
We can see this reflected in the echo chamber phenomenon in social media. Tightly coupled subgroups reinforcing their own messages can synchronise themselves well, but may fall far out of step with the wider population.
Our results bring a new understanding to how synchronisation functions in different natural network structures. It opens new opportunities in terms of designing network structures or interventions on networks, either to aid synchronisation (in power grids, say) or to avoid synchronisation (say in the brain).
More widely, it represents a major step forward in our understanding of how the structure of complex networks affects their behaviour and capabilities. (The Conversation) Real complex systems like this, where there is no central guiding signal and oscillators are connected in a complex network, are very robust to damage and adaptable to change, and can more easily scale to different sizes.
(This story has not been edited by […]
Brain food: MIND diet leads to ‘short-term’ improvements in cognitive health
Food used in MIND diet. (credit: RUSH University) CHICAGO — The popular Mediterranean-DASH Intervention for Neurodegenerative Delay diet, better known as the MIND diet, specifically focuses on foods and nutrients beneficial for brain health. Now, a new study shows the diet is reaping benefits with a “short-term” impact on cognition.
Despite the positive short-term outcome, results from a three-year clinical trial may not be as remarkable as previously observed in MIND diet studies .
“The benefits within the new study’s three-year clinical trial weren’t as impressive as we’ve seen with the MIND diet observational studies in the past, but there were improvements in cognition in the short-term, consistent with the longer-term observational data,” says Dr. Lisa Barnes, the study’s lead author and associate director of the Alzheimer’s Disease Research Center at RUSH University Medical Center, in a university release .
The findings show no significant statistical difference in cognitive changes between participants on the MIND diet and those on a control diet. Both groups aimed to reduce their daily caloric intake by 250 kilocalories. Noticeable cognitive improvements, though, were detected in the study’s initial two years.
“What we saw was improvement in cognition in both groups, but the MIND diet intervention group had a slightly better improvement in cognition, although not significantly better,” notes Dr. Barnes. “Both groups lost approximately 5 kilograms over three years, suggesting that it could have been weight loss that benefited cognition in this trial.”
This trial was significant, being the first-of-its-kind to explore the effects of a diet believed to boost brain health on cognitive ability decline in a large group of individuals 65 years and older without any cognitive impairment. Over the past six years, U.S. News & World Report has consistently ranked the MIND diet among the top five diets.
The MIND diet is a blend of the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets. These diets are known to reduce the risk of various cardiovascular issues , like hypertension and diabetes. The MIND diet centers on foods and nutrients beneficial for brain health, and prior research indicated it could decelerate cognitive decline and substantially reduce Alzheimer’s disease risk , even without strict adherence. (© NDABCREATIVITY – stock.adobe.com) The trial involved 604 participants who were overweight, ate suboptimal diets, and had a family history of Alzheimer’s disease. It examined two different dietary interventions, both with the goal of a 250-calorie reduction per day for weight loss.
Due to the intensive support and monitoring each group received from dietitians, discerning significant differences between the groups in this relatively short timeframe proved challenging.
“By the end of the study, the average weight loss was approximately 5.5 percent of initial body weight for all participants, exceeding the study target of 3 percent, the amount recognized as clinically significant to prevent or improve adverse health outcomes,” says Jennifer Ventrelle, assistant professor in the Departments of Preventive Medicine and Clinical Nutrition and lead dietitian on the MIND diet trial at RUSH.
The improved MIND scores at the study’s conclusion indicate both groups likely experienced cognitive benefits , though further research is required to confirm these findings.
“The average MIND score at the end of three years for the MIND group was 11.0 and 8.3 for the control group, placing both groups in a therapeutic range to slow cognitive decline and lower a risk for Alzheimer’s disease, according to previous studies,” explains Ventrelle. “The significant weight loss and improved MIND scores suggest that the control group also improved their diet and may suggest that following the MIND diet at a score of at least 8.3, coupled with at least a 250 calorie reduction to produce weight loss, may improve cognition.”
The MIND diet includes 14 dietary components, with nine recommended “brain-healthy food groups” such as chicken, fish, green vegetables, berries, and nuts. On the contrary, it advises against five unhealthy groups, including red meat and pastries .
“Randomized trials are gold standards for establishing a cause-and-effect relationship between diet and incidence of Alzheimer’s disease,” says Barnes. “These individuals were healthy at the start of the trial and had no cognitive impairment, and their cognition got slightly better over time. Why there was no difference between the two diet groups at the end of the trial could be a result of many factors including that the control group had a relatively healthy diet. Moving forward, we will look at specific food groups and their associations with biomarkers that were measured in the blood to see if certain nutrients and food groups are more important than others since the two groups were pretty healthy from a dietary perspective at the start.”
The study is published in the journal New England Journal of Medicine . You might also be interested in:
Weight Loss News Heart Health News Diet News Astronomy News Food News Food News Society & Culture News Français Longer Life News
Study: Microplastics accumulate in the brain and cause behavioral changes associated with dementia
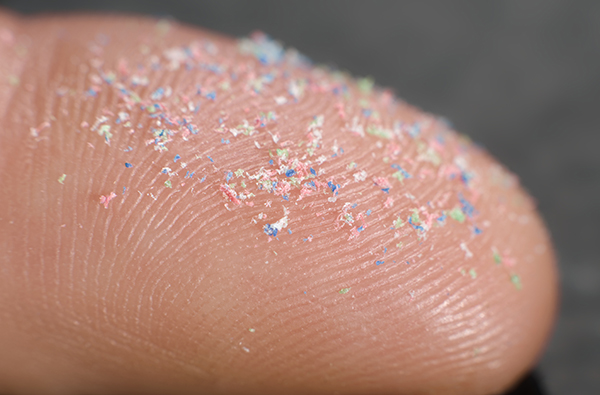
Advertisement
Plastics, especially microplastics, are some of the most common pollutants on Earth. They can be found in the air, in water systems and even in food chains worldwide.
The prevalence of microplastics in the environment is well documented, along with their negative impacts on marine life. However, only a handful of studies have examined their potential health impacts on mammals.
This inspired Jaime Ross, a professor from the University of Rhode Island (URI), to conduct a study on the effects of microplastic exposure .
The study was published in the International Journal of Molecular Science . Microplastics and brain health
Ross and her colleagues analyzed the neurobehavioral effects of, and inflammatory response to, microplastic exposure, as well as the accumulation of microplastics in tissues, including the brain.
Upon examining data from animal studies, the researchers discovered that the infiltration of microplastics is just as far-reaching in the body as it is in the environment. Microplastics exposure was also linked to behavioral changes, especially in older animal subjects. (Related: Report reveals recycling plastic releases toxic “chemical cocktail” into the environment .)
For the study, the researchers exposed young and old mice to different levels of microplastics via their drinking water for three weeks. The results showed that microplastic exposure induces behavioral changes and alterations in immune markers in liver and brain tissues.
After being exposed to microplastics, the research team noticed that the mice began to move and behave peculiarly, exhibiting behaviors similar to those caused by dementia in humans. The results were more profound among older mice.
Ross said this was “striking” because even though they didn’t use high doses of microplastics, the exposure still caused significant changes in only a short period.
Experts still don’t fully understand the life cycle of microplastics in the human body.
Ross said she and her fellow researchers aimed to answer the following questions in their study: As you age, does it make you more susceptible to systemic inflammation from microplastics?
Can your body get rid of microplastics easily?
Do your cells respond differently to these toxins?
Microplastics accumulate in all organs
To understand the physiological systems that may be contributing to the behavioral changes they observed in mice, the researchers analyzed how widespread the microplastic exposure was by dissecting several major tissues, such as the brain, gastrointestinal tract, heart, kidney, liver, lungs and spleen.
They found that the particles had started to bioaccumulate in every organ, including the brain, and even in bodily waste. Because the microplastics got inside the animals’ bodies through their drinking water, Ross and her colleagues expected to find microplastics in the gastrointestinal tract as well as in the liver and kidneys.
Ross noted that the presence of microplastics in the heart and lungs indicates that they spread beyond the digestive system and potentially undergo systemic circulation. This is dangerous because the blood-brain barrier is supposed to be “difficult to permeate.”
The blood-brain barrier is “a protective mechanism against viruses and bacteria,” but microplastics were able to infiltrate it. The particles were found deep in the brain tissue. Brain infiltration by microplastics may cause a decrease in glial fibrillary acidic protein (GFAP), which supports many cell processes in the brain.
Ross warned that a decrease in GFAP is linked to the early stages of certain neurodegenerative diseases, such as Alzheimer’s disease, and depression.
The researchers were also surprised to learn that microplastics could induce altered GFAP signaling.
Ross plans to continue investigate this further in future studies. “We want to understand how plastics may change the ability of the brain to maintain its homeostasis or how exposure may lead to neurological disorders and diseases, such as Alzheimer’s disease,” said Ross. Tips to reduce exposure to microplastics
Microplastics are minuscule and they are everywhere, making it hard to avoid them.
Protect your brain health and overall well-being by following these tips on how to reduce your exposure to microplastics : Do not purchase ready-to-heat products such as boil-in-the-bag rice .
Don’t buy fruit sealed in plastic.
Avoid heating anything in plastic. Avoid consuming food or beverages that have come into contact with plastic. Avoid food-grade nylon used for food packaging and as liners in slow cookers. If possible, drink filtered tap water over bottled water. When buying clothes or furnishings, choose more natural fabrics. If you’re buying carpet, look for something made of wool, not polyester. While natural fibers are usually more expensive, you can save some money with second-hand carpets. Avoid food like fruits and vegetables wrapped in plastic and drink filtered tap water to reduce your exposure to harmful microplastics.Visit Microplastics.news to learn more about the many dangers of microplastics.Watch the video below to learn more about a study on microplastics discovered in human blood . Study: Microplastics Discovered In Human Blood For The First TimeThis is a modal window.No compatible source was found for this media.This video is from the InfoWars channel on Brighteon.com . More related stories: Microplastics alter the shape of human lung cells, warn scientists . National survey: Microplastic pollution around Great Britain’s coastline a hundred times worse than previously reported . Study: Plastic pollution in some lakes is WORSE than the most contaminated parts of the oceans . Sources include: ScienceDaily.com TheGuardian.com Brighteon.com
