Nature Knows and Psionic Success
God provides
that can

Kids who play video games have better memory and better control over their motor skills than kids who don’t, according to a new study looking at adolescent brain function.
Video games might not be responsible for those differences — the study can’t say what the causes are — but the findings add to a bigger body of work showing gamers have better performance on some tests of brain function. That lends support to efforts to develop games that can treat cognitive problems .
“This study adds to our growing understanding of the associations between playing video games and brain development,” said Nora Volkow, director of the National Institute on Drug Abuse, in a statement .
The study used data from the Adolescent Brain Cognitive Development (ABCD) study , which launched in 2018 and is tracking brain development in thousands of children in the United States as they grow into adulthood. Participants periodically go through a battery of assessments, including brain imaging, cognitive tasks, mental health screenings, physical health exams, and other tests.
To study video games and cognition, the research team on this new study pulled from the first set of assessments in the ABCD study. It included data on 2,217 children who were nine and 10 years old. The ABCD study asked participants how many hours of video games they played on a typical weekday or weekend day. The research team divided the group into video gamers (kids who played at least 21 hours per week) and non-video gamers (kids who played no video games per week). Kids who only played occasionally weren’t included in the study. Then, the research team looked at the kids’ performance on tests that measure attention, impulse control, and memory.
The video gamers did better on the tests, the study found. They also had differences in brain activity patterns from the non-gamers — they had more activity in brain regions involved with attention and memory when they were performing the tests. Notably, there were no differences between the two groups on measures of mental health (more evidence rebutting widespread concerns that video games are bad for emotional well-being).
This study adds to a large body of work showing differences in the brains of gamers compared with non-gamers and hinting that gamers have an edge on certain types of brain function. Companies are trying to leverage those differences to develop video games that treat cognitive conditions. Akili Interactive, for example, has a prescription video game to treat ADHD , and DeepWell Digital Therapeutics wants to find the therapeutic value in existing games.
But despite all that work, it’s still not clear why there are differences between gamers and non-gamers in this age group. It could be that video games cause the improvements in cognition. It could also be that people who already have better attention for tasks like the ones in this study are more drawn to video games. There are many different types of video games, as well — this new study, for example, didn’t ask what games the gamers played.
“Large gaps in our knowledge on this topic persist,” wrote Kirk Welker, a neuroradiologist at the Mayo Clinic, in a commentary accompanying the study.
arents often worry about the harmful impacts of video games on their children, from mental health and social problems to missing out on exercise.

Parents often worry about the harmful impacts of video games on their children, from mental health and social problems to missing out on exercise.
But a large new US study published in JAMA Network Open on Monday indicates there may also be cognitive benefits associated with the popular pastime.
Lead author Bader Chaarani, an assistant professor of psychiatry at the University of Vermont, told AFP he was naturally drawn to the topic as a keen gamer himself with expertise in neuroimagery.
Prior research had focused on detrimental effects, linking gaming with depression and increased aggression.
These studies were however limited by their relatively small number of participants, particularly those involving brain imaging, said Charaani.
For the new research, Chaarani and colleagues analyzed data from the large and ongoing Adolescent Brain Cognitive Development (ABCD) Study, which is funded by the National Institutes of Health.
They looked at survey answers, cognitive test results, and brain images from around 2,000 nine- and ten-year-olds, who were separated into two groups: those who never played games, and those who played for three hours or more a day.
This threshold was chosen as it exceeds the American Academy of Pediatrics screen time guidelines of one or two hours of video games for older children.
– Impulses and memory –
Each group was assessed in two tasks.
The first involved seeing arrows pointing left or right, with the children asked to press left or right as fast as they could.
They were also told to not press anything if they saw a “stop” signal, to measure how well they could control their impulses.
In the second task, they were shown people’s faces, and then asked if a subsequent picture shown later on matched or not, in a test of their working memory.
After using statistical methods to control for variables that could skew results, such as parental income, IQ, and mental health symptoms, the team found the video gamers performed consistently better on both tasks.
As they performed the tasks, the children’s brains were scanned using functional magnetic resonance imaging (fMRI). Video gamers’ brains showed more activity in regions associated with attention and memory.
“The results raise the intriguing possibility that video gaming may provide a cognitive training experience with measurable neurocognitive effects,” the authors concluded in their paper.
Right now it’s not possible to know whether better cognitive performance drives more gaming, or is its result, said Chaarani.
The team hope to get a more clear answer as the study continues and they look again at the same children at older ages.
This will also help exclude other potential factors at play such as the children’s home environment, exercise and sleep quality.
Future studies could also benefit from knowing what genres of games the children were playing — though at age 10 children tend to favor action games like Fortnite or Assassin’s Creed.
“Of course, excessive use of screen time is bad for overall mental health and physical activity,” said Chaarani.
But he said the results showed video games might be a better use of screen time than watching videos on YouTube, which has no discernible cognitive effects.
ia/bgs
Brain discovery holds key to boosting body’s ability to fight Alzheimer’s, multiple sclerosis
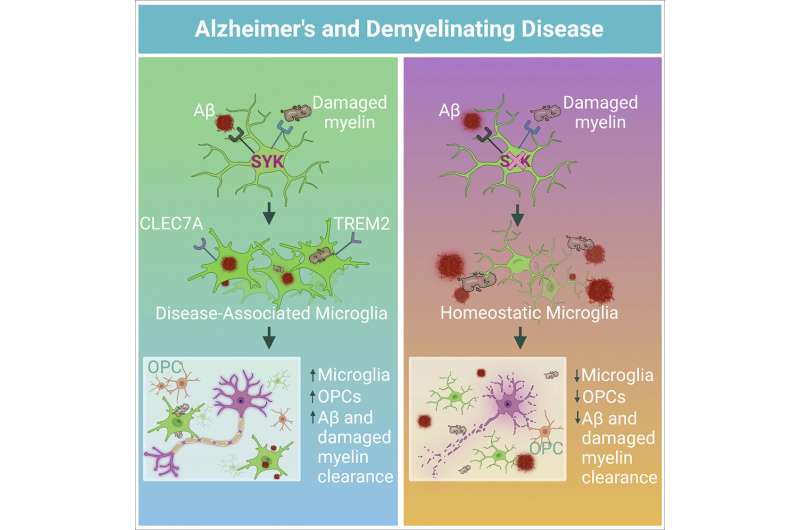
Graphical abstract. Credit: Cell (2022). DOI: 10.1016/j.cell.2022.09.030 UVA Health researchers have discovered a molecule in the brain responsible for orchestrating the immune system’s responses to Alzheimer’s disease and multiple sclerosis (MS), potentially allowing doctors to supercharge the body’s ability to fight those and other devastating neurological diseases.
The molecule the researchers identified, called a kinase, is crucial to both removing plaque buildup associated with Alzheimer’s and preventing the debris buildup that causes MS, the researchers found. It does this, the researchers showed, by directing the activity of brain cleaners called microglia. These immune cells were once largely ignored by scientists but have, in recent years, proved vital players in brain health.
UVA’s important new findings could one day let doctors augment the activity of microglia to treat or protect patients from Alzheimer’s, MS and other neurodegenerative diseases , the researchers report.
“Unfortunately, medical doctors do not currently possess effective treatments to target the root causes of most neurodegenerative diseases, such as Alzheimer’s, Parkinson’s or ALS [amyotrophic lateral sclerosis, commonly called Lou Gehrig’s disease]. In our studies, we have discovered a master controller of the cell type and processes that are required to protect the brain from these disorders,” said senior researcher John Lukens, Ph.D., of the University of Virginia School of Medicine and its Center for Brain Immunology and Glia (BIG), as well as the Carter Immunology Center and the UVA Brain Institute.
“Our work further shows that targeting this novel pathway provides a potent strategy to eliminate the toxic culprits that cause memory loss and impaired motor control in neurodegenerative disease.”
Toxic brain buildup
Many neurodegenerative diseases, including Alzheimer’s and MS, are thought to be caused by the brain’s inability to cleanse itself of toxic buildup. Recent advances in neuroscience research have shed light on the importance of microglia in removing harmful debris from the brain, but UVA’s new discovery offers practical insights into how this cleaning process occurs—and the dire consequences when it doesn’t.
Using a mouse model of Alzheimer’s disease, the UVA researchers found that a lack of the molecule they identified, spleen tyrosine kinase, triggered plaque buildup in the brain and caused the mice to suffer memory loss—like the symptoms seen in humans with Alzheimer’s. Further, the neuroscientists were able to reduce the plaque buildup by activating this molecule and microglia in the brain, suggesting a potential treatment approach for human patients, though that would require significantly more research and testing.
“Our work has described a critical element of microglial function during Alzheimer’s disease and MS,” said researcher Hannah Ennerfelt, the first author of a new scientific paper outlining the findings. “Understanding the underlying biology of these cells during neurodegeneration may allow for scientists and doctors to develop increasingly informed and effective therapeutic interventions.”
A lack of the molecule in a mouse model of MS, meanwhile, led to the buildup of damaged myelin, a protective coating on nerve cells. When myelin is damaged, the cells cannot transmit messages properly, causing MS symptoms such as mobility problems and muscle spasms. The UVA researchers conclude in a new scientific paper that the molecule they identified, abbreviated as SYK, is “critically involved” in the crucial removal of myelin debris.
“If boosting SYK activity in microglia can decrease the amount of myelin debris in MS lesions, developing new drugs to target SYK could stop the progression of MS and help to reverse the damage,” said Elizabeth L. Frost, Ph.D., a critical researcher on the project.
“This is an especially promising option given that most of the currently available drugs for MS treatment dampen adaptive immunity. These immunosuppressive drugs lead to susceptibility to infection and higher risk of potentially fatal side effects like progressive multifocal leukoencephalopathy. Additionally, some forms of MS do not have a strong involvement of the immune system, and therefore there are currently very limited treatment options for those patients.”
“Targeting SYK in microglia,” she noted, “would circumvent multiple limitations of present-day therapeutics for MS.”
Based on their promising results, the researchers report that targeting the molecule to stimulate the brain’s immune activity could offer a way to treat not just Alzheimer’s and MS but a “spectrum” of neurodegenerative diseases.
“These findings are especially exciting because they point to a treatment avenue in which we could alter the behavior of these native brain cells, microglia, to behave in a more neuroprotective way,” said researcher Coco Holliday, a UVA undergraduate working in the Lukens lab. “It could potentially be applied to a variety of different neurological diseases that all share the problem of a buildup of toxic waste in the brain. It’s been a very exciting project to be a part of.”
The research was published in Cell .
Provided by University of Virginia
Molecule That Puts Brain Cells Into “Boost Mode” Identified
Scientists at Oregon Health & Science University have identified a long-sought gene-encoded protein that enables the brain to communicate a broad range of signals across gaps between neurons, known as synapses.
Known as synaptotagmin-3, or SYT3, the protein helps to replenish the supply of chemical neurotransmitters that carry signals between neurons.
“When brain cells are active, they release neurotransmitters to communicate with their neighbors,” said senior author Skyler Jackman, Ph.D., assistant scientist in the OHSU Vollum Institute . “If a cell is very active it can exhaust its supply of neurotransmitters, which can cause a breakdown of communication and brain disfunction.
“It turns out that cells have a boost mode that replenishes their supply of neurotransmitters, but until now, we didn’t know the molecule that was responsible. We found that SYT3 is directly responsible for that neurotransmitter boost,” he said. “This gives us new insight about how brains can break down and fail to process information properly.”
Researchers generated “knock-out” mice that did not have the SYT3 gene. They found that those mice lacked the more robust level of synaptic transmission, compared with control mice that had the gene.
Notably, mutations of the SYT3 gene have been implicated in human cases of epilepsy and autism spectrum disorder. The research published today suggests the possibility of developing gene therapies or pharmaceutical approaches targeting SYT3, Jackman said.
“Imbalances in neurotransmitter release are the underlying causes for many neurological disorders,” said lead author Dennis Weingarten, Ph.D., a postdoctoral researcher in the Jackman lab. In the future, he said, “understanding these molecular switches — such as SYT3 — is a crucial step for us to combat these diseases.”
Jackman’s lab specializes in the study of synaptic transmission. The human brain contains hundreds of trillions of synapses. Discovering the molecules that endow these specialized structures with their unique properties is essential for understanding brain function and neurological disorders.
“Synaptic transmission is fundamental for sensing our surroundings, making decisions and nearly every other feature of our inner world,” Jackman said.
Reference: Weingarten DJ, Shrestha A, Juda-Nelson K, Kissiwaa SA, Spruston E, Jackman SL. Fast resupply of synaptic vesicles requires synaptotagmin-3. Nature . 2022. doi: 10.1038/s41586-022-05337-1
This article has been republished from the following materials. Note: material may have been edited for length and content. For further information, please contact the cited source.
Advertisement
Vitamin C deficiency linked to metabolic syndrome

( Natural News ) A recent study revealed that vitamin C deficiency is linked to metabolic syndrome, a finding that could have powerful implications in improving the health of a significant portion of the American population.
Around 40 percent of Americans currently have metabolic syndrome, which is the term for a group of risk factors that raise their risk of developing serious health conditions such as diabetes, stroke and heart disease. Those who have metabolic syndrome have three or more of the following risk factors: high blood pressure, low levels of HDL cholesterol, extra fat around the waist, high triglycerides and high blood sugar levels.
This phenomenon is largely due to Americans’ poor diets, which are often rich in toxic types of fats and processed sugars. This leads to chronic low-grade inflammation that can eventually lead to the development of metabolic syndrome. The same poor eating habits that can cause metabolic syndrome also create imbalances in the gut microbiome, and this impaired gut function creates additional toxins in your blood that causes the depletion of vitamin C . This has a knock-on effect on vitamin E, a vitamin that vitamin C protects.
Unfortunately, the depletion of these two essential antioxidants only makes the situation worse for people with metabolic syndrome as it leaves them without two important vitamins that help defend the body from the oxidative stress that damages cells. It’s a dangerous cycle; those who have metabolic syndrome are already at a higher risk of heart problems and diabetes, and the fact that they have a weaker immune system due to a vitamin C deficiency only makes their risk even greater. What does this mean for people who have metabolic syndrome?
If you have metabolic syndrome, this study indicates that increasing your consumption of vitamin C could go a long way toward improving your health. However, consuming the recommended amount of vitamin C is not likely to be enough as a study suggests that those with metabolic syndrome need even more vitamin C than the average person. In other words, people who have metabolic syndrome might consume the same amount of vitamin C as other people but because their condition depletes the body of this vitamin, their levels will remain lower.
Increasing your vitamin C intake can benefit your health in many ways because this powerhouse antioxidant helps keep your immune system in check. Maintaining a healthy level of this vitamin can help your body fight infections, heal wounds and neutralize some of the toxins that you may have been exposed to. It also helps your body to make hormones and chemical messengers needed for the functioning of your brain and nerves.
Unfortunately, because vitamin C is a water-soluble vitamin, it is not well stored by the body. Instead, your body just absorbs what it needs at the time, while the rest gets washed away in your urine. This means you need to take it daily, either through the food you eat or supplements.
Many people associate vitamin C with orange juice, and it is true that many citrus fruits are high in this important vitamin. However, it is preferable to eat the whole fruit if you are looking to increase your intake instead of getting it from juice. Kiwis, guavas, grapefruit and strawberries also are good sources of vitamin C. Breakfast is a good time to add fruits rich in vitamin C to your daily routine.
When it comes to vegetables, bell peppers are an excellent source of this vitamin, particularly red and yellow peppers. You will also find vitamin C in cruciferous vegetables such as cauliflower, broccoli, Brussels sprouts and cabbage. Supplements are available for those who struggle to get enough vitamin C from food sources.
Upping your vitamin C intake is a very easy way to improve your overall health and reduce your risk of disease , and being proactive about it could make an impact on the many Americans who have metabolic syndrome.
Sources for this article include:
TheEpochTimes.com
Lobelia: A Snake’s Worst Nightmare

Have you ever been bitten by a venomous serpent? Ever wondered if you would live to tell about it? You don’t have to be a snake handler to know that venom is not something to play around with. Unfortunately, not everyone knows just how to tackle this issue when the occasion arises. Today, let me introduce what might be a lifesaver and a snake’s worst nightmare – Lobelia. Slick and Sly
They slither upon the rocks with stealth and, when convenient, make deserted holes their hideout, that is, until they can surprise their next unsuspecting prey. Yep, snakes!
These reptiles don’t necessarily have the best reputation of being cute and cuddly. Quite the contrary! Certain snakes can get lethally ugly, with nearly half of the 3200 species being venomous. ( 1 ).
According to the World Health Organization: “Snakebite envenoming is a potentially life-threatening disease caused by toxins in the bite of a venomous snake. Envenoming can also be caused by having venom sprayed into the eyes by certain species of snakes that have the ability to spit venom as a defense measure.” ( 2 ) How could you possibly find the relief you need to meet such an emergency? Thankfully, we have an answer offered to us courtesy of nature. Anti-Ophidian – Don’t Bite The Dust
Lobelia, also referred to as pukeweed, accounts for over 300 different species around the world. The one most often utilized for its medicinal ability is Lobelia inflata . While all parts of this plant can be used for medicinal purposes, the seeds are the most potent. The United Plant Savers state that its “very limited wild harvest is permissible when no other alternative will do.” (Gladstar & Hirsch. Planting the Future . 2000)
So what makes this weed so special? The central nervous system activities of this unique herb is thanks to its Piperidine alkaloids, the primary alkaloids of the 52 discovered to date. You may be wondering, what does this have to do with snake bites ?
First, snake antivenom is currently the only standard practice for snake bites, but there are increasing challenges with this route. These include price, cold storage, and diagnostic tools. So an available alternative would be good. ( 4 )
Then we have venom phospholipase A2 (PLA2). This enzyme, largely present in the poison of snakes, is responsible for its toxic effects. Natural herbal PLA2-inhibitors, such as Lobelia, may demonstrate efficacy as novel alternatives to antivenom serum. ( 5 )
The research conducted “showed significant antimicrobial, analgesic and anti-venom properties… Taken together this study validates the strong pharmacological properties of Lobelia nicotianaefolia , which was traditionally used to treat pain and snake bite.” ( 6 )
Now, here’s the cool part. PLA2 has an affinity to attach to the nicotinic acetylcholine (nACh) receptor sites in our brains. ( 7 ) A key hallmark of envenomation is the loss of taste and smell that can persist from months to years. ( 8 ) The activation of these nACh receptors by nicotine is linked directly to the restored function of taste receptors and the olfactory pathway ( 9 ). Thankfully, Lobelia contains properties which can mimic nicotine’s activating ability.
“Animal studies suggest alkaloids of this type may cross the blood-brain barrier, similar to nicotine, and promote the release of neurotransmitters dopamine and norepinephrine….. Lobelien binds to nicotinic acetylcholine receptor sites, promoting release of epinephrine and norepinephrine release, and acts as an antispasmodic bronchodilator.” ( 10 ) Then Is Lobelia A Smoker’s Best Friend?
The short answer? Yes! Lobelia has a history of use by the Native American peoples. For instance, the Cherokee burned it for use as a natural insecticide. Others used it for skin and respiratory diseases, as well as a psychedelic. (Hamel. Cherokee Plants and Their Uses . 1975)
The practice of smoking the herb to bring lung relief led to its common name, “Indian Tobacco” ( 12 ). In fact, renowned herbalists such as Jethro Kloss and John Christopher firmly believed that there was no other herb even half as effective or fast-acting to clear and clean the airways. Its dual-direction ability allows it to act as a respiratory stimulant in small amounts, while at larger amounts it contributes to a sedative and purgative effect. This makes lobelia highly indicated in cases of spasmodic asthma, pneumonia, bronchitis, cough, or vomiting (to remove poisoning). ( 13 )
What’s more, the alkaloid lobeline has a chemical structure identical to nicotine. And lobelia exhibits a successful history of both reducing the urge to smoke while also clearing nicotine from the lungs. ( 14 )
This did not last, however, due to the 1993 decision by the FDA to ban the use of lobelia for such use, and Canada has made it strictly for prescription by licensed dealers only. ( 15 ) Currently, though legal, the United States (USDA) does not classify this herb as a food, and it is excluded from obtaining GRAS status. All this despite the fact that no deaths have been linked to its use. ( 16 ) The “Thinking Herb”
And lobelia offers further benefits. Dr. John Christopher labeled it the “thinking herb” due to its uncanny ability to identify those areas of the body that need help and then swiftly alleviate the issue. ( 17 )
More than this, it will enhance every other herbal constituent you combine with it, making those herbs more effective, especially for the nerves. Specifically, Lobelia proves an excellent neuroprotective agent, as it is a viable solution for Parkinson’s Disease and drug abuse. ( 18 , 19 )
Researchers isolated a constituent of lobelia called beta-amyrin palmitate; then they showed this compound to have mechanisms that improve depressive episodes. ( 20 , 21 ) Research further reveals that the working memory of in ADHD adults can also be enhanced. ( 22 ) Lobeline “significantly increased the brain GABA level” in mice with drug-induced seizures, and thus, scientists consider this as a possible remedy for epileptic seizures. ( 23 ). Use Caution
Please note that after a certain threshold of […]
Gut Microbiome Plays a Role in Lifestyle’s Effects on Dementia Risk
Summary: The microbiome of the gut may influence how exercise and diet affect overall brain health and the risk of developing dementia.
Source: Baycrest
The gut microbiome may play a role in how diet and exercise affect brain health and dementia risk, suggests a recent Baycrest study. This knowledge could help scientists and clinicians optimize strategies to prevent dementia.
Lifestyle interventions to reduce dementia risk often include diet and exercise, which are known to affect the gut microbiome – the community of bacteria and other microorganisms that live in our gut.
“We know that imbalances in the microbiome are associated with impaired cognition,” says Noah Koblinsky, lead author of the study, Exercise Physiologist and Project Coordinator at Baycrest’s Rotman Research Institute (RRI).
“However, we don’t know much about the role of the microbiome when we use lifestyle interventions, such as diet and exercise, to support brain health. Can we tailor lifestyle interventions to specifically target the gut microbiome, and will this help to optimize their effects on cognition? In this review study, we aimed to address this gap in knowledge.”
To this end, Koblinsky and his team reviewed all of the existing research on diet and exercise interventions that looked at both the microbiome and brain health.
The study was published in the Journals of Gerontology: Series A .
They found that the gut microbiome does appear to play a role in how diet and exercise affect brain health, though more research is needed to fully understand how.
Diet studies showed a large impact of diet on the microbiome, with foods associated with a Mediterranean-style eating pattern (for example, fibre and healthy fats) appearing to have the greatest benefit to a healthy gut microbiome and brain.
One study of 1,200 older adults looked at the impact of diet on both cognition and the microbiome. Half of the participants were asked to follow a Mediterranean-style diet for 12 months, while the other half were not.
Those in the Mediterranean diet group showed significant improvements in cognition. As well, those who followed the diet more closely had healthier microbiomes associated with better brain health.
In another study, researchers used antibiotics to “kill off” the gut microbiome in a sample of rats. They then gave those rats microbiome (fecal) transplants from rats that had either been fed an unhealthy diet or a healthy diet. The rats that received the transplant from the unhealthy diet group showed worse memory performance, as well as inflammation in the intestines and brain.
These findings support the idea that the microbiome plays a role in the way diet impacts brain health.
The researchers found fewer studies looking at exercise. However, those that did suggest that starting exercise, specifically aerobic exercise, can lead to changes in the gut microbiome and brain health at the same time. They found that the gut microbiome does appear to play a role in how diet and exercise affect brain health, though more research is needed to fully understand how. Image is in the public domain This area of research is still in its infancy, and the majority of the studies that the researchers reviewed looked at rodents and singular dietary components (for example, fibre) rather than whole diet patterns (like the Mediterranean diet). Overall, the researchers found a clear need for more studies on whole diet and exercise interventions looking at both the microbiome and brain health, particularly in older adults at risk of dementia.
The researchers are now launching a diet and exercise randomized controlled trial and are looking to secure funding to include analysis of microbiome changes.
“By better understanding how changes to the gut microbiome affect the relationship between lifestyle and brain health, we can strengthen existing lifestyle interventions and create new strategies to reduce dementia risk, helping older adults everywhere age fearlessly,” says Dr. Nicole Anderson, Senior Scientist at the RRI, Associate Scientific Director of Baycrest’s Kimel Family Centre for Brain Health and Wellness, and the senior author on this study.
Funding: This research was supported by a grant from the Canadian Consortium on Neurodegeneration in Aging (CCNA), which is supported by the Canadian Institutes of Health Research (CIHR) with funding from several partners. About this microbiome, lifestyle, and dementia research news
Author: Sophie Boisvert-Hearn
Source: Baycrest
Contact: Sophie Boisvert-Hearn – Baycrest
Image: The image is in the public domain
Original Research: Open access.
“ The Role of the Gut Microbiome in Diet and Exercise Effects on Cognition: A Review of the Intervention Literature ” by Noah Koblinsky et al. Journals of Gerontology Series A
Abstract
The Role of the Gut Microbiome in Diet and Exercise Effects on Cognition: A Review of the Intervention Literature
Interest in the gut–brain axis and its implications for neurodegenerative diseases, such as Alzheimer’s disease and related dementias, is growing. Microbial imbalances in the gastrointestinal tract, which are associated with impaired cognition, may represent a therapeutic target for lowering dementia risk.
Multicomponent lifestyle interventions are a promising dementia risk reduction strategy and most often include diet and exercise, behaviors that are also known to modulate the gut microbiome.A better understanding of the role of the gut microbiome in diet and exercise effects on cognition may help to optimize these lifestyle interventions.The purpose of this review is to summarize findings from diet and exercise interventions that have investigated cognitive changes via effects on the microbiome. We aim to discuss the underlying mechanisms, highlight current gaps in the field, and provide new research directions.There is evidence mainly from rodent studies supporting the notion that microbiota changes mediate the effects of diet and exercise on cognition, with potential mechanisms including end-product metabolites and regulation of local and systemic inflammation.The field lacks whole diet and exercise interventions, especially those involving human participants. It is further limited by heterogeneous rodent models, outcome assessments, and the absence of proper mediation analyses.Trials including older adults with dementia risk factors, factorial designs of diet and exercise, and pre and post measures of microbiota, end-product metabolites, and inflammation would help to elucidate and potentially leverage the role of the microbiome […]
Brain development in grandchildren could be affected by what their grandmother eats

GALVESTON, Texas (KXAN) – The University of Texas Medical Branch conducted a study recently that found brain development in grandchildren could be affected by what their grandmother eats.
The study was performed on mice by UTMB. Research found that adverse effects of maternal high-fat diet on brain development and related disorders, including autism spectrum disorder, could carry over to a second generation of descendants, according to a press release about the study, which was published on Tuesday in Cell Reports .
It builds on findings from a previous study done by Shelly A. Buffington, assistant professor in the Department of Neurobiology and faculty in the Sealy Center for Microbiome Research at UTMB, demonstrating the effects of maternal high-fat diet on offspring brain plasticity and social behavior published in Cell in 2016 .
“Our study focused on the impact of high-fat diet exposure in the maternal lineage on behavioral outcomes associated with neurodevelopmental disorders in descendant generations,” Buffington said. “Remarkably, we found that a high fat grandmaternal diet has the potential to impact neurodevelopment and long-term behavioral outcomes across multiple descendant generations.”
In the current study, researchers compared gut microbial richness across three generations of mice. The grandmothers were fed either a control or high-fat diet.
Diet-driven loss of microbial richness observed in the grandmaternal females, and their first-generation offspring, was partially recovered by the second descendant generation, yet social deficits akin to those in the first descendant generation remained evident in the second.
“These data suggested that disruption of the maternal gut microbiome, instead of that of the juvenile offspring, could be the culprit underlying abnormal social behavior in the descendant generations,” said study co-first author and recent UTMB Neuroscience Graduate Program doctoral graduate, Claudia Di Gesù.
Di Gesù also suggested that preconception, prenatal, and postnatal supplementation with probiotics could one day be incorporated into a comprehensive regimen. A regimen including micronutrient, folic acid, and vitamin D dietary supplementation, physical activity, and cognitive behavior approaches to help improve long-term health outcomes in both the mother and her child, and, potentially, her children’s children.
Other UTMB co-authors include former Buffington Lab postdoctoral scholar Robert Fultz and research associate Ian Bolding. Researchers from Baylor College of Medicine and the University of Palermo also contributed to the study.
Copyright 2022 Nexstar Media Inc. All rights reserved. This material may not be published, broadcast, rewritten, or redistributed.
For the latest news, weather, sports, and streaming video, head to KXAN Austin.
Omega-3 Linked to Improved Brain Structure and Cognition at Midlife

Eating cold-water fish and other sources of omega-3 fatty acids may preserve brain health and enhance cognition in middle age, according to new research. Holy mackerel! Could eating salmon, tuna, cod, herring, or sardines keep our brains healthy and our thinking agile in middle age? New research on omega-3 fatty acids makes this connection.
New evidence indicates that eating food that contains omega-3 fatty acids, such as cold-water fish, may preserve brain health and enhance cognition in middle age.
According to new research, having at least some omega-3s in red blood cells was associated with better brain structure and cognitive function among healthy study volunteers in their 40s and 50s. The study was published online on October 5 in Neurology , the medical journal of the American Academy of Neurology. Faculty of The University of Texas Health Science Center at San Antonio (UT Health San Antonio) and other investigators of the Framingham Heart Study conducted the analysis. Omega-3 fatty acids (omega-3s) are present in certain foods such as flaxseed and fish, as well as dietary supplements such as fish oil. Several different omega-3s exist, but the majority of scientific research focuses on three: alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA contains 18 carbon atoms, whereas EPA and DHA are considered “long-chain” (LC) omega-3s because EPA contains 20 carbons and DHA contains 22. “Studies have looked at this association in older populations. The new contribution here is that, even at younger ages, if you have a diet that includes some omega-3 fatty acids, you are already protecting your brain for most of the indicators of brain aging that we see at middle age,” said Claudia Satizabal, PhD, lead author of the study. She is an assistant professor of population health sciences with the Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases at UT Health San Antonio.
Salmon is an excellent source of omega-3 fatty acids.
Volunteers for the study had an average age was 46. The research team examined the relation of red blood cell omega-3 fatty acid concentrations with MRI and cognitive markers of brain aging. Scientists also studied the effect of omega-3 red blood cell concentrations in participants who carried APOE4, a genetic variation linked to a higher risk of Alzheimer’s disease.
The study of 2,183 dementia- and stroke-free participants found that: Higher omega-3 index was associated with larger hippocampal volumes. The hippocampus, a structure in the brain, plays a major role in learning and memory.
Consuming more omega-3s was associated with better abstract reasoning, or the ability to understand complex concepts using logical thinking.
APOE4 carriers with a higher omega-3 index had less small-vessel disease. The APOE4 gene is associated with cardiovascular disease and vascular dementia.
Scientists used a technique called gas chromatography to measure docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) concentrations from red blood cells. The omega-3 index was calculated as DHA plus EPA. Flaxseed (linseed), soybean, and canola oils are examples of plant oils that contain ALA. Walnuts and chia seeds also contain ALA. The amount of omega-3 in fish varies greatly.Cold-water fatty fish, such as salmon, mackerel, tuna, herring, and sardines, contain high amounts of LC omega-3s, while fish with a lower fat content—such as bass, tilapia, and cod—as well as shellfish contain lower levels. Beef is very low in omega-3s. However, beef from grass-fed cows contains somewhat higher levels of omega-3s, mainly as ALA, than that from grain-fed cows. Some foods, such as certain brands of eggs, milk, yogurt, juices, and soy beverages, are fortified with DHA and other omega-3s. “Omega-3 fatty acids such as EPA and DHA are key micronutrients that enhance and protect the brain,” said Debora Melo van Lent, PhD, study coauthor. She is a postdoctoral research fellow at the Biggs Institute. “Our study is one of the first to observe this effect in a younger population. More studies in this age group are needed.”
The researchers divided participants into those who had very little omega-3 red blood cell concentration and those who had at least a little more. “We saw the worst outcomes in the people who had the lowest consumption of omega-3s,” Satizabal said. “So, that is something interesting. Although the more omega-3 the more benefits for the brain, you just need to eat some to see benefits.”
Scientists don’t know how DHA and EPA protect the brain. One theory is that, because those fatty acids are needed in the membrane of neurons, when they are replaced with other types of fatty acids, that’s when neurons (nerve cells) become unstable. Another explanation may have to deal with the anti-inflammatory properties of DHA and EPA. “It’s complex. We don’t understand everything yet, but we show that, somehow, if you increase your consumption of omega-3s even by a little bit, you are protecting your brain,” Satizabal said.
It’s encouraging that DHA and EPA also protected APOE4 carriers’ brain health. “It’s genetics, so you can’t change it,” Melo van Lent said, referring to the vulnerability of this risk group. “So, if there is a modifiable risk factor that can outweigh genetic predisposition, that’s a big gain.”
Reference: “Association of Red Blood Cell Omega-3 Fatty Acids With MRI Markers and Cognitive Function in Midlife: The Framingham Heart Study” by Claudia L. Satizabal, Jayandra Jung Himali, Alexa S. Beiser, Vasan Ramachandran, Debora Melo van Lent, Dibya Himali, Hugo J. Aparicio, Pauline Maillard, Charles S. DeCarli, William Harris and Sudha Seshadri, 5 October 2022, Neurology .
DOI: 10.1212/WNL.0000000000201296
Study links omega-3s to improved brain structure, cognition at midlife

Credit: CC0 Public Domain Eating cold-water fish and other sources of omega-3 fatty acids may preserve brain health and enhance cognition in middle age, new evidence indicates.
Having at least some omega-3s in red blood cells was associated with better brain structure and cognitive function among healthy study volunteers in their 40s and 50s, according to research published online Oct. 5 in Neurology . Faculty of The University of Texas Health Science Center at San Antonio (UT Health San Antonio) and other investigators of the Framingham Heart Study conducted the analysis.
“Studies have looked at this association in older populations. The new contribution here is that, even at younger ages, if you have a diet that includes some omega-3 fatty acids, you are already protecting your brain for most of the indicators of brain aging that we see at middle age ,” said Claudia Satizabal, Ph.D., assistant professor of population health sciences with the Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases at UT Health San Antonio. Satizabal is the lead author of the study.
Volunteers’ average age was 46. The team looked at the relation of red blood cell omega-3 fatty acid concentrations with MRI and cognitive markers of brain aging. Researchers also studied the effect of omega-3 red blood cell concentrations in volunteers who carried APOE4, a genetic variation linked to higher risk of Alzheimer’s disease.
The study of 2,183 dementia- and stroke-free participants found that: Higher omega-3 index was associated with larger hippocampal volumes. The hippocampus, a structure in the brain, plays a major role in learning and memory.
Consuming more omega-3s was associated with better abstract reasoning, or the ability to understand complex concepts using logical thinking.
APOE4 carriers with a higher omega-3 index had less small-vessel disease. The APOE4 gene is associated with cardiovascular disease and vascular dementia.
Researchers used a technique called gas chromatography to measure docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) concentrations from red blood cells. The omega-3 index was calculated as DHA plus EPA.
“Omega-3 fatty acids such as EPA and DHA are key micronutrients that enhance and protect the brain,” said study coauthor Debora Melo van Lent, Ph.D., postdoctoral research fellow at the Biggs Institute. “Our study is one of the first to observe this effect in a younger population. More studies in this age group are needed.”
The team divided participants into those who had very little omega-3 red blood cell concentration and those who had at least a little and more. “We saw the worst outcomes in the people who had the lowest consumption of omega-3s,” Satizabal said. “So, that is something interesting. Although the more omega-3 the more benefits for the brain, you just need to eat some to see benefits.”
Researchers don’t know how DHA and EPA protect the brain. One theory is that, because those fatty acids are needed in the membrane of neurons, when they are replaced with other types of fatty acids , that’s when neurons (nerve cells) become unstable. Another explanation may have to deal with the anti-inflammatory properties of DHA and EPA. “It’s complex. We don’t understand everything yet, but we show that, somehow, if you increase your consumption of omega-3s even by a little bit, you are protecting your brain,” Satizabal said.
It’s encouraging that DHA and EPA also protected APOE4 carriers’ brain health . “It’s genetics, so you can’t change it,” Melo van Lent said, referring to the vulnerability of this risk group. “So, if there is a modifiable risk factor that can outweigh genetic predisposition, that’s a big gain.”
Provided by University of Texas Health Science Center at San Antonio
Neurodegenerative Diseases, Novel Treatments
Saskia Sivananthan, chief research officer at the Alzheimer Society of Canada, said recently that if not much changes to the current trends, the number of people with dementia and the number of people caring for them “is going to be enormous. By investing in addressing modifiable risk factors that improve brain health, we can start changing and shifting some of those numbers down.”
Don’t bet on it. Unfortunately, the experts at the ASC appear to speak only to like-minded old-school scientists largely unaware of the research on neurodegenerative disorders being conducted outside their bubble. According to the Alzheimer Society report, “Navigating the Path Forward for Dementia in Canada,” “Certain risk factors like age and genetics are not modifiable.” While we all age, though, how we age is modifiable. We all know people who look and act 10 years younger than their chronological age and vice versa. Being active, having many interests, eating a proper diet , sleeping well, visiting your doctor for yearly check-ups, and not neglecting your oral hygiene are just some of the things we can all do to age well.
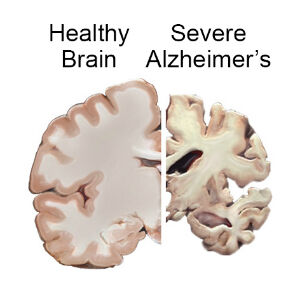
There is also some really exciting new research about rejuvenation. A study from the University of California-San Francisco showed that exposure of an aged animal to young blood can counteract and reverse pre-existing effects of brain aging by rejuvenating synaptic plasticity and improving cognitive function. This reminds me of the grotesque practice most commonly attributed to the historical figure of Elizabeth Bathory, a Hungarian countess and serial killer who lived from 1560 to 1614. Bathory believed that she could maintain eternal youth and beauty by bathing in the blood of virgins. Macabre, yes, but perhaps she was onto something? Healthy Brain and Severe AD Brain Tal Iram, a young neuroscientist at Stanford University, infused, instead of blood, cerebrospinal fluid taken from young mice into old mice. For comparison, a separate group of old mice was infused with artificial cerebrospinal fluid. A few weeks later, the mice were exposed to cues — a tone and a flashing light — that they had earlier learned to associate with shocks to their feet. The animals that had received the young cerebrospinal fluid infusion tended to freeze for longer, suggesting that they had preserved stronger memories of the original foot shock.
The ASC report mentions social isolation as a risk factor, but does not discuss the connection between social isolation and the bacteria in our guts, commonly referred to as the gut microbiome , a focus of much research all over the globe. For example, scientists from University of California-La Jolla found that loneliness was associated with a lack of diversity in the gut microbiome. On the other hand, wisdom and compassion were associated with a diverse microbiome. Conversely, the researchers said that social support, compassion, and wisdom might confer protection against loneliness-related instability of the gut microbiome. The relationship between loneliness and microbial diversity was particularly strong in older adults.
Healthy, diverse gut microflora may buffer the negative effects of chronic stress or help shape social behaviors that promote either wisdom or loneliness. It is possible that loneliness may result in decreased stability of the gut microbiome and, consequently, reduced resistance and resilience to stress-related disruptions, leading to inflammation and disease.
Other surprising new research from Stanford shows that the buildup of neurofibrillary tangles of tau protein inside neurons in Alzheimer’s, Parkinson’s, and other brain diseases, which has been assumed to be the primary culprit, actually occurs in all aging cells, not just brain cells. Protein aggregation may be a universal phenomenon in aging cells and could be involved in many more diseases of aging than was suspected. Their discovery points to a new way of thinking about what goes wrong in cells as they age and, potentially, to new ways of preventing some unwelcome consequences of aging.
In the Alzheimer’s brain, abnormal levels of beta-amyloid protein, a naturally occurring protein, clump together to form plaques that collect between neurons and disrupt cell function. Pharmaceutical companies and neuroscientists have spent millions of hours and billions of dollars trying to clear the brain of these amyloid plaques.
Now a new study in the journal PLOS Biology, by John Mamo of Curtin University in Bentley, Australia, found that amyloid protein made in the liver, when transported to the brain, may be a significant contributor to neurodegeneration in the brain. Consequently, it seems logical to assume that the liver may play an important role in the onset or progression of the disease. Has anyone at the Alzheimer Society heard about this?
The “Navigating the Path Forward for Dementia in Canada” report advises us to get six-to-eight hours of quality sleep at night. Good advice. But what if you can’t? A majority of elderly people suffer from insomnia . The reason may be hiding in their gut. Diana Rogulja, an assistant professor of neurobiology at Harvard Medical School, recently discovered how sleep deprivation causes death in fruit flies and mice. Lethal changes occur not in the brain but in the gut by way of a preponderance of reactive oxygen species (ROS), free radicals . If ROS are not swept up by antioxidant enzymes, they may cause damage to DNA, RNA, and proteins, and may lead to cell death.
In conclusion, it appears that there are many avenues open to improve the lives of people suffering from neurodegenerative disorders and, in the long run, to prevent these from occurring in the first place. Unfortunately, many scientists dealing with neurodegenerative diseases are too deeply invested in the current model to initiate change. The message needs to reach the public directly for real transformation. Pressure for reform must come from both inside and outside medicine.
References
Vaccaro, A., Dor, Y. K.., & Rogulja, D. et al., (2020). Sleep loss can cause death through accumulation of reactive oxygen species in the gut. Cell, 181(6), 1307-1328.
Nguyen, T. T., Zhang, X… & Jeste, D. V.et al., (2021). Association of loneliness and wisdom with gut microbial diversity and composition: an exploratory study. Frontiers in psychiatry, 395.
Lam, V., Takechi, R., Hackett, M. […]
‘Superagers’ with sharp memories in their 80s have larger neurons

So-called superagers maintain an exceptionally sharp memory into their eighties and above “Superagers” – people aged 80 or over with exceptionally good memories – may have larger than expected neurons in a region of the brain that is critical for memory .
With age , most people experience a gradual decline to their memory, but some maintain a remarkable ability to recall past events into their eighties or older, on par with people 20 to 30 years younger.
Alongside a decline in memory, our brains naturally shrink with age, with previous studies suggesting this occurs less with superagers.
Now, researchers have shown that superagers may have larger than expected neurons in their entorhinal cortex, a component of the brain’s memory system.
Tamar Gefen at Northwestern University in Illinois and her colleagues imaged brains donated by six superagers who died at an average age of 91. The six individuals previously took part in ongoing research into superagers .
These images were compared with seven people who died at an average age of 89 and a further six people who died at an average of 49, all of whom had memories that would be considered normal for their age.
Among the superagers, their entorhinal cortex neurons were around 10 per cent larger than those of the people who died at a similar age with a to-be-expected memory.
The superagers’ neurons were even around 5 per cent larger than the people who died 40 years younger, suggesting that larger than average neurons may contribute to an exceptional memory at age 80 or over.
The superagers also had substantially fewer protein clumps called tau tangles inside their neurons than their counterparts who died at a similar age. An abnormal build-up of tau has been suggested as a cause of Alzheimer’s disease .
“I am not yet sure why larger neurons are associated with preserved memory other than that they are more resistant to tau tangles,” says Gefen. “One other hypothesis is that they are more structurally sound and can generate more optimal [neural connections].”
“[The overall study] adds to the growing evidence that superagers differ from typical adults on multiple levels of the brain,” says Alexandra Touroutoglou at Harvard Medical School.
“The sample size here is relatively small, but that’s understandable. Superagers are a rare group, so finding a good number of them in a postmortem brain study is difficult,“ she says.
According to Joseph Andreano , also at Harvard Medical School, other brain regions linked to cognition have been shown to differ in size in superagers compared with people with a to-be-expected memory. It is unclear whether neuron size in the entorhinal cortex specifically accounts for enhanced memory, he says.
Study: Regular consumption of blueberries can reverse cognitive decline among the elderly

( Natural News ) Blueberries are full of beneficial antioxidants. According to a study published in the journal Nutritional Neuroscience , eating wild blueberries regularly can help reverse cognitive decline among the elderly .
While conducting the study, researchers from the University of North Carolina (UNC) discovered that elderly Americans who were already suffering from “demonstrable cognitive issues” experienced incredible benefits from consuming blueberries each day.
In many cases, the brain health of the study participants reached the same levels as those with no known history of cognitive decline. This is important because there are no mainstream cures for dementia .
Blueberries are a popular “superfood,” with impressive antioxidant properties. The berries also contain different vitamins and minerals linked to brain health and reductions in heart disease and cancer risk.
A one-cup serving (about 148 grams) of blueberries provides 24 percent of your daily intake of vitamin C, 36 percent of vitamin K, 25 percent of manganese and 14 percent of dietary fiber. Cognitive function and blueberry consumption
For the study, researchers gathered data from 86 elderly adults between the ages of 65 and 80.
The volunteers all self-reported cognitive issues. Another 43 people in the same age range but without reported brain issues took part in the study as the control group.
After an initial screening to determine cognitive functioning at the start of the study, participants were split into two groups: One group added wild blueberry powder to their diets while the other added a placebo. (Related: Anthocyanins in fruits like blueberries can boost brain and heart health .)
Dr. Carol Cheatham, lead researcher and an associate professor of psychology and neuroscience at UNC, said that they specifically used wild blueberries from Maine for the study because the phytochemicals they contain can fight skin cancer, pests and other elements in the harsh northeastern environment. Blueberries can reverse cognitive decline
When people consume berries, the protective benefits of the fruits’ phytochemical content are transferred to humans. The study showed that the phytochemicals in wild blueberries can boost brain health .
For the study, the volunteers mixed blueberry powder into their food every day. Six months later, they were screened for cognitive health again.
The researchers discovered that the mental processing speed of participants who consumed the blueberries daily greatly recovered after the study period.
On average, their mental processing was restored to the point that they had the same processing speed as the control group who reported no cognitive decline.
Processing speed refers to the brain’s ability to store and recall information. The researchers explained that processing speed is key to all brain functions, and this improvement points to an “overall jump in brain health.”
The study was relatively small, but Cheatham believes that her team has found a natural and effective solution to the cognitive issues affecting millions of Americans.
Cheatham herself incorporates blueberries into her regular diet by mixing at least two cups of berries into a breakfast smoothie.
You can also boost your brain health by consuming blueberries every day. Even amounts much smaller than Cheatham’s daily intake can still be effective. Boost your brain health with these tasty blueberry recipes
Try these amazing recipes featuring antioxidant-rich blueberries to boost your brain health.
Healthy blueberry and oatmeal muffins
This recipe pairs blueberries with fiber-rich oatmeal .
Ingredients for 12 servings: 1 1/5 Cups whole wheat pastry flour
1 Cup fresh or frozen blueberries
1 Cup oats
1 Cup vanilla almond milk , unsweetened
1/2 Cup coconut oil
1/2 Cup honey 1 Teaspoon baking powder 1/2 Teaspoon baking soda 1/2 Teaspoon cinnamon 1/2 Teaspoon salt 1 Teaspoon vanilla extract 1 Large egg Preparation: > Mix the dry ingredients in a large bowl: Flour, oats, baking powder, baking soda, cinnamon and salt. Whisk the wet ingredients in a medium bowl: Coconut oil, egg, honey, vanilla and almond milk. Pour the mixture with the wet ingredients into the bowl of dry ingredients and mix until just combined. Do not overmix. Set the mixture aside for 10 minutes. Preheat the oven to 350 F and line the muffin tin with liners while the mixture is set aside. Mix in the blueberries and divide the batter evenly among the muffin tin holes. Sprinkle the tops of the muffins with more oats for garnish. Bake the muffins for 20 to 25 minutes, flipping the pan around the ten-minute mark to bake all muffins evenly. The muffins are done when you insert a toothpick into the center of the muffins and it comes out clean without any batter on it. Let the muffins cool for 10 minutes and transfer them to a cooling rack to finish cooling. No-bake vegan blueberry breakfast bars These vegan blueberry bars don’t need to be baked and they’re perfect for a quick and tasty breakfast or snack. Ingredients for 16 servings: 1 1/5 Cups 100 percent pure, uncontaminated, rolled oats (certified gluten-free) 1 Cup almond butter 3/4 Cup whole almonds 1/2 Heaping cup dried blueberries ½ cup pistachios 1/3 Cup ground flaxseed 1/3 Cup pepitas 1/3 Cup pure maple syrup or honey 1/3 Cup walnuts 1/4 Cup sunflower seeds 1/4 Cup unsweetened apple sauce Preparation: > Line an 8″x 8″ or similar size baking pan with parchment or wax paper until the paper hangs over the edges. Combine the oats, almonds, blueberries, pistachios, ground flaxseed, walnuts, pepitas and sunflower seeds in a large bowl and mix to combine. Add the maple syrup or honey and apple sauce to the large bowl, then mix again to combine. Add the almond butter to the combined ingredients in the bowl and mix until combined. Place the batter in the prepared pan. Press down firmly with the palm of your hands or use a mini-roller. Distribute the mixture as evenly as possible. Leave the pan in the freezer for at least one hour. Remove the pan from the freezer. Carefully lift the frozen slab from the pan using the excess along the edges. Set the slab down and gently peel the paper away. Slice the slab diagonally into eight long bars, […]
Music on the brain: Listening can influence our brain’s activity

Enlarge People have long tried to use music as a tool to improve their abilities. Soldiers chanted songs when marching into battle, sailors sang songs on long voyages, and cloth makers sang when weaving. But do we have any evidence that music makes a difference for any of our activities?
We’ve only recently started to ask that question scientifically. It began with the Mozart effect, which seemed to link classical music to improved mental performance. Named after the famous composer, it was shorthand for the apparent boost in IQ tests that people listening to his music experienced. But the phenomenon turned out not to be real. “Background music was thought to help with work. [It was] found to be the noise stopping the person from being distracted,” says Professor Concetta Tomaino, executive director and co-founder of the Institute for Music and Neurologic Function.
However, research into music and its effects on human abilities continued and eventually resulted in the discovery of an effect called brain entrainment, which appears capable of improving memory, focus, sleep, and physical activity. Making waves
The technique involves manipulating some of the waves of activity that are part of normal brain behavior. We’ve discovered five types of brain waves: alpha, beta, theta, delta, and gamma. David Sonnenschein, founder of iQsonics, a company that is developing tools for autistic children, says that alpha waves mark resting states and that beta waves are for waking consciousness. However, their effects also overlap; Tomaino says that “Gamma and beta waves help with attention and theta and delta waves help with sleep.”
In theory, you can tune difference in music frequency to boost the activity of any one of these brain waves. “In essence, brain entrainment is the production of specific brain patterns from certain types of music that has specific phase difference,” says Sonnenschein, whose tools for autistic children are based on the idea. Brain entrainment works by having a person listen to music with two different frequencies using headphones. “You can have music at 408 Hz and music at 400 Hz—this creates a difference,” Sonnenschein said, “and that difference is the frequency of brain waves you produce in the brain.”
Beyond these frequency effects, the exact benefits of different types of music are still hotly debated. Some researchers suspect that brain entrainment has a very large effect regardless of the type of music. This group includes Adam Shea-Hewett, who has worked on using music to improve human abilities for nearly two decades and is co-founder of Evoked Response, a company that provides music it claims improves individual capabilities.
However, there are others, such as Mari Tervaniemi, research director at the Centre of Excellence in Music, Mind, Body, and Brain at the University of Helsinki, who differ. “In most cases, it is the favorite music which is beneficial—beneficial to changing the emotional state. Positive emotions can then also contribute to improving cognition. It depends on the music that person likes,” she told Ars. However, she does caution that there are very few studies on South America or Africa, so any cultural differences in how music is appreciated remain unexplored.
There is evidence that the music itself matters. A study with 50 volunteers used brain entrainment that stimulated theta brainwaves but used different means of doing so: either white noise or music. A simple memory test showed that those listening to music saw a much greater boost in performance. Lots of questions
However, everyone we talked to agreed that music has an effect. But how large is this effect, and how long does it last? That is a question researchers have been struggling with for quite some time.
Research indicates that the effects can be wide-ranging, from improving memory to increasing attention. However, these effects do not last forever. Both Tervaniemi and Tomaino say that you can use it for one or two sessions throughout the day. More than this and you would adapt to the music, limiting its effect.
There is some data on how long changes last following exposure to music. Music produced by Evoked Response has been shown to increase focus in an attention-based task, and the effect seemed to last well after the music was shut off. “We don’t know how long the effects last, but an improvement was seen compared to those without music after two hours from the session,” says Shea-Hewett. Evoked Response and others have found similar timing when music was used to influence memory, physical activity, and attention—effects last for one to two hours after the music listening phase.
Another study looking into the effects on sleep showed that individuals who listened to music as they fell asleep saw an increase in their slow wave oscillations (brain waves of a certain frequency), which occur during the later hours of sleep and are essential for memory consolidation. The group that also used the specially crafted music showed a doubling in their time spent in deep sleep and over a halving in the time taken to fall asleep. Self-medication?
While many people are excited about the prospects of using music to boost everyday performance, others have tested it for its therapeutic value. “Many studies in this area are normally focused on people with pathological conditions such as Alzheimer’s disease, insomnia, and attention deficit hyperactivity disorder,” says Tomaino. “For example, music has been shown to improve memory of dementia patients or focus for people with ADHD.” But the greatest effect is on those with Parkinson’s disease, which is marked by uncontrollable movements. “Training with music can lead to a recovery of movement, and the effects are seen instantly.”
Given that listening to music has a long history and is deeply ingrained in many cultures, it’s tempting to view these results as a clear benefit. But the benefit is unlikely to be uniform. For example, there are people who suffer from amusia. “These people do not detect musical pitch and so will not get an effect from music,” Tervaniemi told Ars. Amusia may be as common as dyslexia and is currently poorly studied. We also don’t […]
Brain-zapping cap appears to boost memory for at least 1 month, early research finds

A cap embedded with electrodes that deliver small electric zaps to the brain appeared to boost memory in a group of older adults for at least one month, according to a new study.
The researchers say the technology, the results of which were published Monday in the journal Nature Neuroscience , could one day be used as an at-home intervention for people at risk of dementia to improve memory, when diet and other lifestyle changes alone aren’t enough.
Though both the study’s authors and outside experts say that more work is needed before people could go out and use such a device, there’s an air of excitement around the results.
The findings are “quite remarkable,” said Dr. Gregory Worrell, a neurologist at the Mayo Clinic in Rochester, Minnesota, who was not involved in the research.
“Memory dysfunction is such a common comorbidity of neurologic and psychiatric disease, so these kinds of results could have really wide-ranging applications,” he said.
As people begin to live longer, the approach could become an important tool to protect or even enhance memory in older adults, said senior study author Robert Reinhart, a neuroscientist at Boston University.
More than 16 million people in the U.S., many over the age of 65, have some form of cognitive impairment, according to the Centers for Disease Control and Prevention .
“It’s an unfortunate fact of life that as we age we all become a little more forgetful,” Reinhart said. “Memory deficits impair our activities of daily living, planning, decision making, cognition, learning, and that can generally have a negative effect of diminishing quality of life.” A brain-zapping cap
The new study included 150 people ages 65 to 88 who did not have a diagnosed neurological disorder .
Using the cap, the researchers delivered a weak electrical current to participants’ brains while asking them to recall five lists of 20 words. The process was done for 20 minutes on four consecutive days. Forty people in the study received a placebo treatment — they wore the cap but didn’t receive the electrical stimulation.
The study found that memory performance improved by approximately 50% to 65% in participants who received the four-day intervention. That translated to participants recalling four to six more words, on average, as compared to the group of people receiving the placebo stimulation, according to the researchers.
“This is not a small effect,” Worrell said.
The study also found that the intervention was capable of boosting both working memory and long-term memory. Both types of memory are important — the former helps store information for seconds and minutes, like when you need to remember a phone number. Long-term memory is important for storing information over days, months or years.
The people with the worst cognitive function coming into the experiment showed the most improvement during the intervention and one month later, the researchers said, adding that that may lay the groundwork for a clinical trial for people with Alzheimer’s disease .
Reinhart noted that the research is still in its early stages. Additional studies are still needed to determine whether these effects can last beyond one month, as well as whether these methods can enhance memory performance in people with impaired cognition due to neurodegenerative disorders like Alzheimer’s.
Get the Morning Rundown
Get a head start on the morning’s top stories.
This site is protected by recaptcha Privacy Policy | Terms of Service
The technology also has limitations. The approach cannot correct for the death of brain cells, something common among people with these disorders, said Shrey Grover, a doctoral student in Reinhart’s lab and the lead author of the study.
However, it’s not the first time researchers have shown that zapping the brain can temporarily improve memory. Worrell, of the Mayo Clinic, published a study in 2018 that found low-intensity electrical stimulation to a specific area appeared to improve verbal short-term memory. Overall, he acknowledged, that previous research on the topic has been a mixed bag.
Dr. Michael Fox, a Harvard Medical School neurologist who was not involved in the research, said the promise of being able to put on a cap 20 minutes a day and enhance cognitive function gets “people excited.”
Still, Fox said he wonders what sort of adverse effects, if any, the method could have on the mind.
Feeling forgetful? How stress may affect memory
April 12, 202203:37
“If someone is above the age of 65 and their No. 1 problem is memory, this could still be something that helps and this might be OK if it comes at the expense of some other function that doesn’t bother them,” he said.
The study’s authors said that they did not observe any serious adverse effects over the course of the study.Grover said participants often experienced itching and a tingling sensation shortly before and after using the helmet. Some people experienced a slight “poking sensation” on their scalp, he said, but they generally found the sensation very manageable. Wide use one day? Many researchers in the field expect that the technology could one day be used widely to help those experiencing cognitive impairment.The technology used in the helmet is relatively cheap and noninvasive, Worrell said, meaning people could one day possibly use the device at home.There are already similar devices sold at brick-and-mortar stores and online retailers, like Amazon, he said, but none have been approved by the Food and Drug Administration for memory improvement and may not work as advertised.Grover said the approach could be administered outside of a doctor’s office and combined with existing therapies.But aside from its potential clinical use, Reinhart said that if the approach becomes available to the wider public, he could see people using it the same way they use caffeine to increase arousal .“You can imagine a future potentially where people are using stimulation,” he said. “I think people are just overwhelmingly interested in augmenting their ability to provide a kind of cutting-edge advantage.”Worrell agreed. “It is more expensive than a cup of coffee, but it is really not incredibly expensive,” he said. Follow NBC HEALTH on Twitter & Facebook .
Modern humans generate more brain neurons than Neanderthals
The question of what makes modern humans unique has long been a driving force for researchers. Comparisons with our closest relatives, the Neanderthals, therefore provide fascinating insights. The increase in brain size, and in neuron production during brain development, are considered to be major factors for the increased cognitive abilities that occurred during human evolution. However, while both Neanderthals and modern humans develop brains of similar size, very little is known about whether modern human and Neanderthal brains may have differed in terms of their neuron production during development.
Researchers from the Max Planck Institute of Molecular Cell Biology and Genetics (MPI-CBG) in Dresden now show that the modern human variant of the protein TKTL1, which differs by only a single amino acid from the Neanderthal variant, increases one type of brain progenitor cells, called basal radial glia, in the modern human brain. Basal radial glial cells generate the majority of the neurons in the developing neocortex, a part of the brain that is crucial for many cognitive abilities. As TKTL1 activity is particularly high in the frontal lobe of the fetal human brain, the researchers conclude that this single human-specific amino acid substitution in TKTL1 underlies a greater neuron production in the developing frontal lobe of the neocortex in modern humans than Neanderthals.
Only a small number of proteins have differences in the sequence of their amino acids — the building blocks of proteins — between modern humans and our extinct relatives, the Neanderthals and Denisovans. The biological significance of these differences for the development of the modern human brain is largely unknown. In fact, both, modern humans and Neanderthals, feature a brain, and notably a neocortex, of similar size, but whether this similar neocortex size implies a similar number of neurons remains unclear. The latest study of the research group of Wieland Huttner, one of the founding directors of the Max Planck Institute of Molecular Cell Biology and Genetics (MPI-CBG) in Dresden, carried out in collaboration with Svante Pääbo, director at the Max Planck Institute for Evolutionary Anthropology in Leipzig, and Pauline Wimberger of the University Hospital Dresden and their colleagues, addresses just this question. The researchers focus on one of these proteins that presents a single amino acid change in essentially all modern humans compared to Neanderthals, the protein transketolase-like 1 (TKTL1). Specifically, in modern humans TKTL1 contains an arginine at the sequence position in question, whereas in Neanderthal TKTL1 it is the related amino acid lysine. In the fetal human neocortex, TKTL1 is found in neocortical progenitor cells, the cells from which all cortical neurons derive. Notably, the level of TKTL1 is highest in the progenitor cells of the frontal lobe.
Modern human TKTL1, but not Neanderthal TKTL1, leads to more neurons in embryonic mouse neocortex
Anneline Pinson, the lead author of the study and researcher in the group of Wieland Huttner, set out to investigate the significance of this one amino acid change for neocortex development. Anneline and her colleagues introduced either the modern human or the Neanderthal variant of TKTL1 into the neocortex of mouse embryos. They observed that basal radial glial cells, the type of neocortical progenitors thought to be the driving force for a bigger brain, increased with the modern human variant of TKTL1 but not with the Neanderthal variant. As a consequence, the brains of mouse embryos with the modern human TKTL1 contained more neurons.
More neurons in the frontal lobe of modern humans
After this, the researchers explored the relevance of these effects for human brain development. To this end, they replaced the arginine in modern human TKTL1 with the lysine characteristic of Neanderthal TKTL1, using human brain organoids — miniature organ-like structures that can be grown from human stem cells in cell culture dishes in the lab and that mimic aspects of early human brain development. “We found that with the Neanderthal-type of amino acid in TKTL1, fewer basal radial glial cells were produced than with the modern human-type and, as a consequence, also fewer neurons,” says Anneline Pinson. “This shows us that even though we do not know how many neurons the Neanderthal brain had, we can assume that modern humans have more neurons in the frontal lobe of the brain, where TKTL1 activity is highest, than Neanderthals.” The researchers also found that modern human TKTL1 acts through changes in metabolism, specifically a stimulation of the pentose phosphate pathway followed by increased fatty acid synthesis. In this way, modern human TKTL1 is thought to increase the synthesis of certain membrane lipids needed to generate the long process of basal radial glial cells that stimulates their proliferation and, therefore, to increase neuron production.
“This study implies that the production of neurons in the neocortex during fetal development is greater in modern humans than it was in Neanderthals, in particular in the frontal lobe,” summarizes Wieland Huttner, who supervised the study. “It is tempting to speculate that this promoted modern human cognitive abilities associated with the frontal lobe.”
Story Source:
Materials provided by Max Planck Institute of Molecular Cell Biology and Genetics (MPI-CBG) . Note: Content may be edited for style and length.
Journal Reference :
> Anneline Pinson, Lei Xing, Takashi Namba, Nereo Kalebic, Jula Peters, Christina Eugster Oegema, Sofia Traikov, Katrin Reppe, Stephan Riesenberg, Tomislav Maricic, Razvan Derihaci, Pauline Wimberger, Svante Pääbo, Wieland B. Huttner. Human TKTL1 implies greater neurogenesis in frontal neocortex of modern humans than Neanderthals . Science , 2022; 377 (6611) DOI: 10.1126/science.abl6422
Brain stimulation can improve the memory of older people
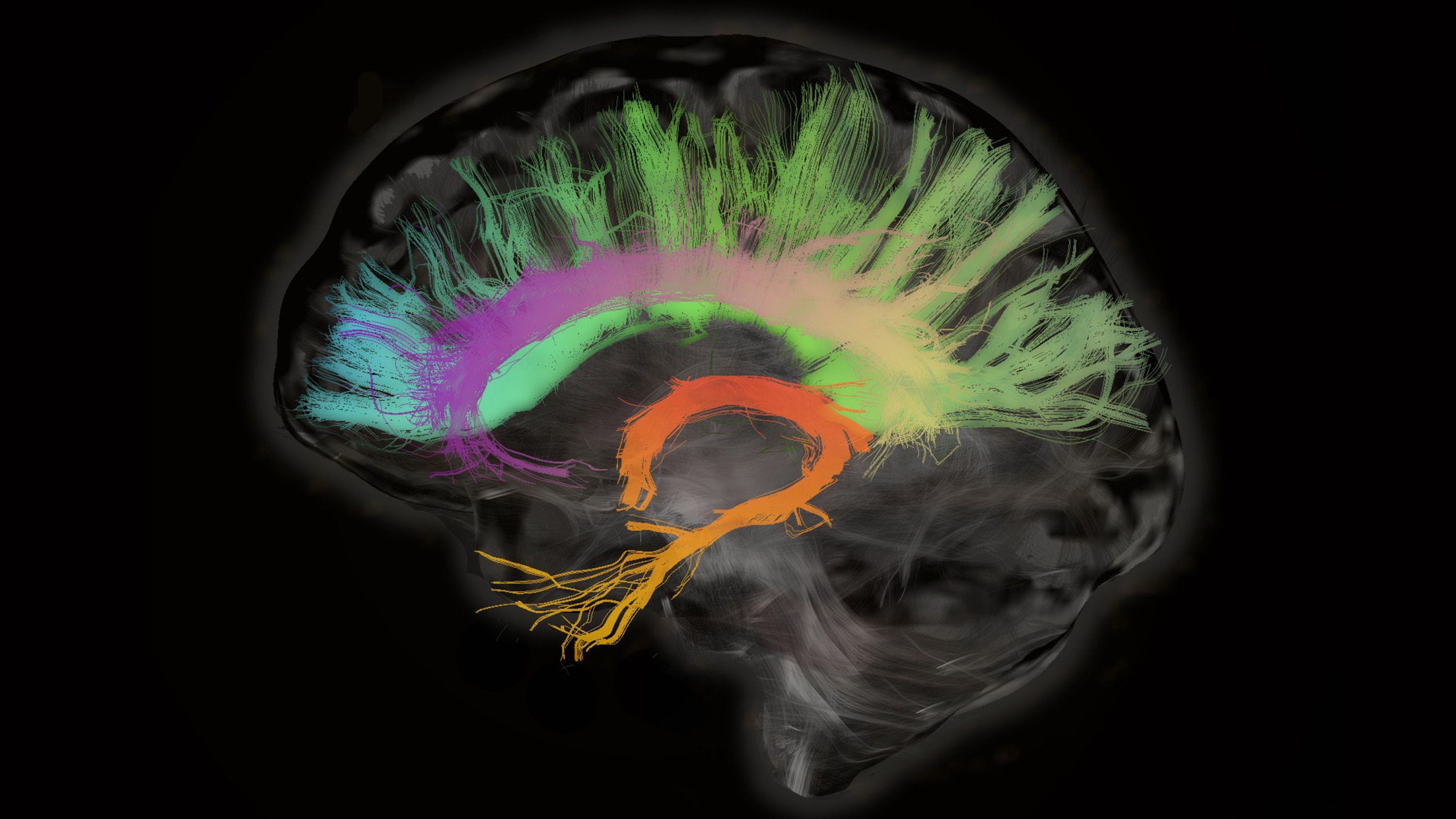
Many of us will struggle to remember things as we get older. A gentle form of brain stimulation might help, according to new research. The approach appears to boost the memories of older people and help them remember lists of words.
The technique can be adapted to improve either long-term or short-term memory, and the benefits appear to last for at least a month. It’s the first time this type of brain stimulation has been shown to have such long-lasting effects on human memory, say the researchers behind the work.
“This was a very short intervention which produced both an immediate effect and a very durable one,” says Marom Bikson, a neural engineer at the City College of New York, who was not involved in the study. “More research is needed, but if this works out it could be in every doctor’s office … and it could eventually be something that people use at home.” Electric brains
“It’s an uncomfortable fact of life that as we age, we all become a little bit forgetful,” says Rob Reinhart, a neuroscientist at Boston University, who led the work. Reinhart studies brain networks for functions like cognition, attention, and memory—and how they seem to decline with age and as a result of some disorders.
Brain cells communicate with each other using electrical pulses, and brain networks and regions have their own pulses of electrical activity. Growing evidence suggests that applying electrical stimulation to these networks can change the way they work, potentially strengthening connections between brain regions.
To find out if this approach could improve memory, Reinhart and his colleagues turned to a form of brain stimulation called transcranial alternating current stimulation. tACS, as it’s known, allows gentle pulses of electricity to the skull via electrodes embedded in what is essentially a swimming cap.
Although the approach delivers electricity to regions of the brain, the doses are too low to trigger brain cells to fire. Instead, tACS modulates the way cells fire, says Reinhart. He prefers to describe his use of tACS as brain modulation rather than brain stimulation. “They’re noninvasive, safe, extremely weak levels of alternating current,” he says.
The team used a modern, high-definition form of tACS, which allows researchers to target small regions of the brain. The group chose to focus on two regions of the brain that are known to be involved in memory: part of the prefrontal cortex at the front of the brain, which is involved in long-term memory, and the inferior parietal lobe, a region toward the back of the brain thought to be involved in short-term memory.
Each of these two brain regions has its own characteristic pattern of electrical pulses of activity, or brain waves. In the first experiment, Reinhart and his colleagues delivered pulses of activity to match the natural rhythms of each region—high frequencies for the prefrontal cortex and low frequencies for the parietal lobe. Tingling, itching, and warming
The team recruited 60 volunteers, all between the ages of 65 and 88, who were divided into three groups. In a task, each person was read a list of 20 words and had to recall them later. While they were performing this task, a third of the group had the prefrontal cortex of their brain modulated, and another third had their parietal lobes targeted. The remaining third wore a cap of electrodes but didn’t receive any stimulation.
Those who did receive brain stimulation did not feel anything dramatic, says Reinhart. “When the current is running, you feel like a mild tingling or itching or poking or warming sensation,” he says.
The 20-minute session was repeated for four consecutive days. Over those four days, people who received brain stimulation improved in their ability to remember words. There was no such improvement among those who weren’t stimulated.
And the type of memory improvement depended on which brain regions had been stimulated. Those who had the front of their brains stimulated were better at remembering the first words in the list, suggesting their long-term memory had improved. Those who had their parietal lobes stimulated saw improvements in their short-term memory.
By the end of the four days, those who’d had their brains stimulated improved their performance by around 50 to 65% and remembered around four to six extra words from the list of 20, on average, says Reinhart. “It’s very impressive,” says Roi Cohen Kadosh, a cognitive neuroscientist at the University of Surrey, who was not involved in the study.
“We can watch the memory improvements accumulate … with each passing day,” says Reinhart, who, along his colleagues, published the findings in the journal Nature Neuroscience on Monday.
The greatest improvements were among those who had the worst cognitive function at the start of the study. This suggests that the technique might one day be helpful for people with memory disorders such as Alzheimer’s disease or other dementias, says Reinhart.
When Reinhart’s team swapped the frequencies, targeting the front of the brain with low frequencies and the back of the brain with high ones, there was no improvement in either short- or long-term memory. This suggests that the type of stimulation must match the natural brain waves in order to work.
Reinhart and his colleagues only checked in on their volunteers a month after they did the experiment, and they don’t know if the improvements lasted beyond that point. And while the study found that the volunteers were better at remembering words from a list, Reinhart doesn’t know if their memories improved more generally, or if the stimulation improved their lives in any way.
“The effects are really specific, and not something that would benefit someone who would want to improve their memory [more generally],” says Cohen Kadosh. He points out that people who want to remember things for an exam, for example, don’t just want to remember the first and last things they read—they need to remember everything. “We need to see if there is really an effect … in everyday life functions,” he says. Bikson agrees this is a valid concern—some “brain training” games promise to boost […]
How Nature Nurtures the Brain

A new study investigates how a walk outdoors has positive effects on the brain.
Living in cities can increase one’s risk of developing anxiety, depression, and schizophrenia.
A new study investigated the brain processes underlying the positive effects on stress of taking a walk in a forest.
The results of the study showed that a walk in the forest reduces activity in the amygdala and benefits mental health.
Life in a large city can be incredibly stressful . Psychological research has shown that people who live in cities may have an increased risk for depression , anxiety , and schizophrenia compared to people living in more rural areas. In contrast, many people perceive hiking and spending time in nature as stress-relieving and calming. What has been largely unclear so far, however, is the question of how specifically spending time in nature affects our brain function to reduce stress. The positive effects of nature on mental well-being
A new study, published in the journal Molecular Psychiatry ( Sudimac et al., 2022 ), focused on precisely this question. In the study, entitled “How nature nurtures: Amygdala activity decreases as the result of a one-hour walk in nature,” a research team led by Sonja Sudimac from the Max Planck Institute for Human Development in Berlin investigated how stress-related brain regions reacted to a one-hour walk in an urban environment—a busy street in Berlin—compared to a natural environment; in this case, a forest.
The researchers used a neuroscientific technique called functional magnetic resonance imaging (fMRI) to measure brain activation in 63 healthy volunteers in two groups: walking in nature or walking in an urban environment. In both groups, brain activation was measured before and after the walk, using two different tasks in the MRI scanner. The first fMRI task was a fearful-faces task designed to activate anxiety-related brain networks, and the second fMRI task was a social-stress task designed to activate stress-related brain networks.
In the fearful-faces task, volunteers watched faces with fearful and neutral expressions while lying in the scanner. The so-called MIST (Montreal Imaging Stress Task) was used as the social stress task. In the MIST, volunteers have to solve very complicated mathematical tasks designed to be beyond their abilities, while they get compared to a fake “average.” The fake average the volunteers see is always better than their own performance, so that they may feel stressed since they perform so badly. Amygdala activity is reduced after a walk in nature
The scientists found very similar results in both the fearful faces and the stress test. For the group of volunteers that walked for one hour in an urban environment, there were no changes in the activation of fear or stress-related networks between the two scans. In contrast, for the group of volunteers that walked for one hour in nature, there was a decrease in activity in one specific brain area for both fMRI tasks after the walk: the amygdala; in particular, the right amygdala.
The amygdala is a group of neuronal nuclei within the temporal lobe of the brain and has been shown to be a key structure in the processing of fear and stress. In particular, when people are stressed out, their brains tend to switch to more amygdala-driven networks. The finding that amygdala activity reduces after a walk in nature, therefore, led the scientists to conclude that a walk in nature can help restore us from the negative effects of stress. This finding has powerful implications as it suggests that taking time off and hiking in the woods can have a protective effect on the development of many psychological disorders for which stress is often a major influence factor.
So what can you do the next time you feel stressed out? Take a hike in the woods, and you should feel a little less frazzled.


