Nature Knows and Psionic Success
God provides
New therapeutic targets for treating memory impairment in Down’s syndrome

Credit: CC0 Public Domain A team of researchers led by Dr. Victoria Puig from the Hospital del Mar Medical Research Institute (IMIM), which also involved the Centre for Genomic Regulation (CRG), has studied the neural basis of intellectual disability in mice with Down’s syndrome and has discovered that the neural networks of brain circuits relevant to memory and learning are over-activated and that the connectivity of these circuits is poor.
The researchers have also observed that neural activity during sleep is abnormal and probably interferes with memory consolidation . Additionally, the study identified biomarkers in brain rhythms that can predict memory deficits in the mice that are corrected by chronic treatment with a natural component of green tea, epigallocatechin gallate , which other studies have already shown to improve executive function in adults with Down’s syndrome.
“These results suggest that both hyperactivity of neuronal networks and deficiencies in the connectivity of specific brain circuits are possible dysfunctional mechanisms that contribute to memory deficits in Down’s syndrome, and therefore, offer new therapeutic possibilities for treating intellectual disability ,” explains Dr. Victoria Puig, researcher in the Integrated Pharmacology and Systems Neuroscience Research Group at the IMIM.
Researchers have recognised that epigallocatechin gallate corrects certain alterations at the molecular and cellular levels derived from the trisomy of chromosome 21 that are associated with cognitive deficits in Down’s syndrome. However, a dynamic description of the actions of epigallocatechin gallate on neural activity during distinct brain states was lacking. So this is the first investigation of mouse brain response to chronic treatment with epigallocatechin gallate at a functional level in trisomy conditions.
The study involved recording neuronal activity simultaneously in the prefrontal cortex and the hippocampus, two brain regions critical for learning and memory, in trisomic and non-trisomic mice during periods of rest while awake, asleep, and during the performance of a simple memory task. The data was collected before and after one month of treatment with epigallocatechin gallate, and the alterations in the activity of the neuronal networks in the two regions as well as the connectivity of the circuitry correlating with memory capacities were analyzed and found to have been corrected with the green tea extract.
According to Dr. Mara Dierssen from the Cellular and Systems Neurobiology lab at the CRG, “This study provides an in-depth description of the neurophysiological abnormalities present in different brain states in Down’s syndrome model mice and provides the keys for understanding the cellular mechanisms underlying the improved executive function observed in people with Down’s syndrome after chronic treatment with epigallocatechin gallate.”
Dr. Maria Alemany, first author of the paper and also a researcher in the IMIM’s Integrated Pharmacology and Neuroscience Systems research group, says, “The group is evaluating the effects of cognitive stimulation during brain development on the neuronal activity of mice with Down’s syndrome. This is important for understanding the cellular mechanisms of cognitive stimulation that are normally used in people to improve intellectual disability.”
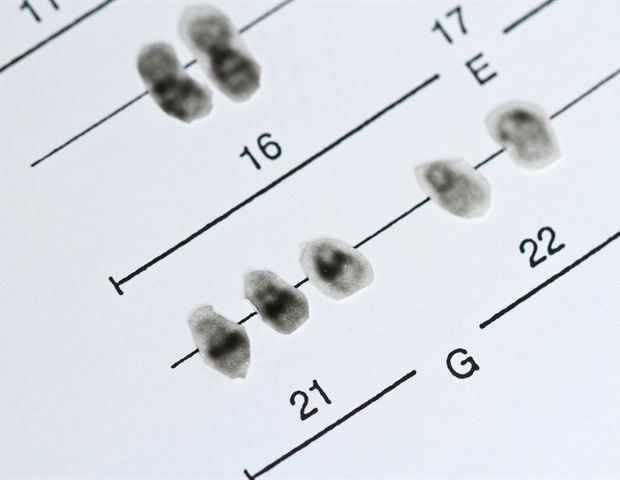
Down’s syndrome is a genetic alteration produced by the presence of an extra copy of chromosome 21, which is why this syndrome is also known as trisomy 21. It is the main cause of intellectual disability and the most common human genetic alteration. It is estimated that 34,000 people with Down’s syndrome live in Spain and that there are a total of 6 million people with the condition worldwide.
Provided by IMIM (Hospital del Mar Medical Research Institute)
New therapeutic possibilities for treating intellectual disability in Down syndrome
A team of researchers led by Dr. Victoria Puig from the Hospital del Mar Medical Research Institute (IMIM), which also involved the Centre for Genomic Regulation (CRG), has studied the neural basis of intellectual disability in mice with Down syndrome and has discovered that the neural networks of brain circuits relevant to memory and learning are over-activated and that the connectivity of these circuits is poor.
The researchers have also observed that neural activity during sleep is abnormal and probably interferes with memory consolidation.
The study has even identified biomarkers in brain rhythms that can predict memory deficits in the mice which are corrected by chronic treatment with a natural component of green tea, epigallocatechin gallate, which other studies have already shown to improve executive function in adults with Down syndrome. These results suggest that both hyperactivity of neuronal networks and deficiencies in the connectivity of specific brain circuits are possible dysfunctional mechanisms that contribute to memory deficits in Down syndrome and, therefore, offer new therapeutic possibilities for treating intellectual disability. Dr. Victoria Puig, Researcher, Integrated Pharmacology and Systems Neuroscience Research Group, IMIM To date, it had been recognized that epigallocatechin gallate corrects certain alterations at the molecular and cellular levels derived from the trisomy of chromosome 21 that are associated with cognitive deficits in Down syndrome.
However, a dynamic description of the actions of epigallocatechin gallate on neural activity during distinct brain states was lacking. This is, therefore, the first time that anyone has looked at how mouse brain responds to chronic treatment with epigallocatechin gallate at a functional level in trisomy conditions.
The study involved recording neuronal activity simultaneously in two brain regions critical for learning and memory, the prefrontal cortex and the hippocampus, in trisomic and non-trisomic mice during periods of rest while awake, asleep, and during the performance of a simple memory task.
The data was collected before and after one month of treatment with epigallocatechin gallate, and the alterations in the activity of the neuronal networks in the two regions as well as the connectivity of the circuitry correlating with memory capacities were analyzed and found to have been corrected with the green tea extract. This study provides an in-depth description of the neurophysiological abnormalities present in different brain states in Down syndrome model mice and provides the keys for understanding the cellular mechanisms underlying the improved executive function observed in people with Down syndrome after chronic treatment with epigallocatechin gallate. Dr. Mara Dierssen, Cellular and Systems Neurobiology Lab, Centre for Genomic Regulation Dr. Maria Alemany, first author of the paper and also a researcher in the IMIM’s Integrated Pharmacology and Neuroscience Systems research group, explains ” that the group is evaluating the effects of cognitive stimulation during brain development on the neuronal activity of mice with Down syndrome. This is important for understanding the cellular mechanisms of cognitive stimulation that are normally used in people to improve intellectual disability .”
Down syndrome is a genetic alteration produced by the presence of an extra copy of chromosome 21, which is why this syndrome is also known as trisomy 21. It is the main cause of intellectual disability and the most common human genetic alteration. It is estimated that 34,000 people with Down’s syndrome live in Spain and that there are a total of six million sufferers worldwide. This study provides an in-depth description of the neurophysiological abnormalities present in different brain states in Down syndrome model mice and provides the keys for understanding the cellular mechanisms underlying the improved executive function observed in people with Down syndrome after chronic treatment with epigallocatechin gallate. Dr. Mara Dierssen, Cellular and Systems Neurobiology Lab, Centre for Genomic Regulation
There Will Be 4 Identity Types in This Recovery. Which One Are You?

Become a conscious creator and feel motivated, focused and driven to achieve your goals.
Will be used in accordance with our Privacy Policy Opinions expressed by Entrepreneur contributors are their own.
The following article is based on excerpts from Ben Angel’s book, Unstoppable: A 90-Day Plan to Biohack Your Mind and Body for Success . Buy it now from Amazon | Barnes Noble | iBooks | IndieBound. And be sure to order The Unstoppable Journal , the only journal of its kind based on neuroscience , psychology , and biohacking to help you reach your goals.
Nearly half of adults in the United States reported that their mental health had been negatively impacted due to worry and stress over the coronavirus, according to the latest Kaiser Family Foundation poll. Adverse mental-health effects due to social isolation may be particularly pronounced among older adults and households with adolescents, as these groups are already at risk for depression or suicidal ideation.
The pandemic is likely to have both long- and short-term implications for mental health and substance use. Those with mental health concerns pre-pandemic, and those newly affected, will likely require mental health- and substance-use services. Keeping this in mind, you must know where you sit on the mental-health continuum to understand how it is affecting you physically. When people undergo traumatic stress either mentally or physically, it creates a pattern within the body that soon emanates into psychological and biological side effects. You can now track where you fall into this continuum by taking an Identity Quiz on how well you are coping with your current situation. We have been able to survey more than 50,000 entrepreneurs and found out 54 percent of them fall into the two lowest categories: The Guardian and The Defender.
There are four identity types in total: The Catalyst, The Synergist, The Guardian and The Defender. Your goal is to ensure your physical and psychological energy stays above a 50 percent charge, the state at which you become a conscious creator and feel motivated, focused, and driven to achieve your goals. When you fall below this state, you switch into a state of self-preservation mode where you run out of physical and emotional energy. This is where your fight-or-flight response is triggered and your brain prioritizes vital bodily functions over personal or career goals.
Below, you’re going to learn which identities we need to be most concerned about and what you can do to change your identity to help you through these harrowing times. The Defender
Operating at 0- 25 percent of their capacity. Traits of Defenders: Rely heavily on caffeine or other stimulants to make it through the day.
Food cravings of sugars and carbs.
Cognitive functions are in severe decline, like forgetting names, numbers or information; inability to make decisions.
Low levels of concentration.
Quick to exhaustion as brain doesn’t have the fuel it needs to focus.
Chronic digestive issues, joint pain, skin rashes and unexplainable brain fog and fatigue.
Insomnia.
Defenders are depressed, anxious and struggle to make it through the day. Many will blame this on a poor mental attitude and feel they are lazy. They are emotionally depleted and need love and support from others, including medical professionals, to help them get their health and their life back. Defenders must seek out medical and professional help immediately. The Guardian
Operating at 25-50 percent of their capacity. Traits of Guardians: Procrastination and criticism derail their efforts.
They can keep going, briefly relying on willpower.
They have goals, but they seem unattainable.
Self-doubt has laid its foundation.
Chronic stress.
Nutritional deficiencies taking their toll.
Less energy and focus.
Takes longer to recover from physical or emotional events.
They can endure for some time, but this constant state of fight or flight is taking its toll on many of their bodily and brain functions. It’s typically the first time in their life they can’t function as they used to, and many in the medical field will tell them it’s typical aging and prescribe a drug to help alleviate the symptoms without treating or accurately defining the cause. The Synergist
Operates at 50-75 percent of their capacity. Traits of Synergists: Learning to balance willpower with sustainable energy, though starting to find it harder to maintain willpower alone.
Energy levels tend to fluctuate throughout the day. Focus and concentration also varies throughout the day; unable to maintain constant energy. They have an inner understanding that rest helps to reset the body for long-term success. Relatively even moods. Deliberate and conscious creators. Not easily distracted. Can quickly slide back into a Guardian if they fail to look after their physical and emotional health. The Catalyst Operates at 75-100 percent of capacity. Traits of Catalysts: Greatly self-aware of how their brain and body works for peak performance. Abundance of psychological and physical energy to fuel them daily. Able to troubleshoot problems calmly and methodically. Able to pinpoint underlying issues and correct them successfully. Operates from the higher executive part of their brain. Strengthens their cognition through meditation, education, supplements and a healthy diet. Are society’s game changers, both locally and globally. Yes, we all can become The Catalyst, but it takes self-awareness and courage to dig deep into the root causation of your illnesses. Here are the first steps you should do to get yourself on the path to becoming unstoppable. 3 Steps to Become a Peak-Performing Catalyst If you scored as a Guardian or Defender, you mustn’t go on this health journey on your own. Finding a functional medicine doctor who specializes in chronic conditions will have the additional training needed to get to the root cause of your concerns. Following the steps below will aid in your knowledge of brain and body consciousness so you can increase your energy and build emotional and physical […]
Protecting a Most Precious Asset: GABA Proved to Fortify Cognitive Health in Human Trials

As life spans in industrialized nations increase, so does anxiety about the effects of cognitive decline on individuals, on society. New twin studies offer significant hope for strengthening the neurobiological environment, reversing that trend.
The market for brain health supplements in the United States, which has shown double-digit growth in the past several years, blares a message about the concerns of the health-conscious. They want to have agency over the state of their mental health as they age, as they do their physical health.
The benefits of the naturally-occurring amino acid neurotransmitter GABA [γ-Aminobutyric acid], found across a range of healthful foods, have never really been in doubt. It’s the reason that Pharma Foods International Co. Ltd., manufacturer of PharmaGABA TM and supplying partner of Mitsubishi International Food Ingredients Inc., has devoted decades of constant research and development to deriving it from natural sources, refining it, and making it bioavailable for daily intake.
Though its importance in moderating mood and enabling relaxation was traditionally recognized — the concept of harnessing and refining GABA in its pure form was based on observing its high concentration in fermented staples of ancient East Asian cuisine, such as kimchi — the modern world seeks authoritative evidence for GABA’s ability to bolster mental and emotional health.
This evidence arrived in the form of twin randomized, double-blind, placebo-controlled, parallel-group clinical studies involving the administration of 100 and 200 mg of GABA daily to two separate groups of 60 healthy adult subjects aged over 40.
The results of the studies show that over a 12-week period of daily administration of GABA, subjects performed significantly better on tests of their mental acuity, as well as surveying higher on indices evaluating quality of life, than subjects administered a placebo. Assessments using the Cognitrax and RBANS (Repeatable Battery for the Assessment of Neuropsychological Status) tests, which involve direct engagement of simple, everyday mental operations, were made at 4, 8, and 12 weeks. The results clearly show improvements in a host of cognitive areas, a palpable, calculable elevation of quality of life; and further, the studies attest unconditionally to the safety of daily supplemental GABA intake for healthy adults.
It has long been known that a decreased systemic level of GABA is associated with the presence of Parkinson’s disease, epilepsy, Huntington’s chorea, Alzheimer’s disease, and schizophrenia. Based on this knowledge, researchers sought connections between the presence of GABA and related conditions, including increased alpha and decreased beta wave production, mental alertness, and coordination; proving, first in animal models, that intake of GABA improved maze memory and avoidance learning among other neurobiological manifestations. These were the precursors to human trials.
Participants in this first human study showed significant improvement in visuospatial/construction faculty tests, involving spatial construction and coordination, and delayed memory, which is keyed to short-term attention and recall, in the 100 mg group. The most striking finding was that when intake was doubled to 200 mg, additional improvements were recorded in the crucial areas of non-verbal reasoning, working memory, and sustained attention. In both studies, quality of life, which is, of course, closely related to cognitive function, was shown to be identifiably higher with regular GABA intake, in the distinct areas of physical functioning, vitality, and mental health.
It needs to be noted that as far back as 2016, Pharma Foods responded to research from the University of California-Berkeley showing that non-REM sleep deficiency was associated with a higher buildup of toxic beta-amyloids in the brain — setting the stage for the onset of Alzheimer’s disease at an accelerated pace — with clinical proof that GABA reduced sleep latency while lengthening the successive deep, non-REM stage of sleep. In fact, the current study adds to a wealth of knowledge realized in previous clinical studies carried out over decades, indicating sweeping benefits that accompany the daily administration of supplemental GABA, including the ability to aid rigorous physical exercise and build muscular strength and endurance .
In Japan, the PharmaGABA TM brand has long held the confidence of health-conscious consumers. The world’s third largest economy also has the distinction of having the longest overall life expectancy. Factoring in its low birth rate and immigration, the complex matter of the “greying population” is always at the forefront of social discourse; discussions that inevitably include the assertion that longer life, without the internal resources to successfully live it, is unsustainable, both individually and nationally.
Pharma Foods was established in 1997 with its development of a proprietary process to derive GABA from an entirely natural source, the fermentation of Lactobacillus hilgardii . In PharmaGABA TM it produced a supplement of unequalled quality and over 80% purity. In fact, PharmaGABA is the only Self-Affirmed GRAS GABA product on the market today. In Japan, where an active, aging population is confronting the imperative of maintaining cognitive health throughout life, PharmaGABA commands over 80% of the market, with sales of the supplement in Japan and the U.S. increasing over 25% in the past year alone.
Our human condition calls for action now to preserve the vibrancy and value of our future, and the path is through healthy cognition and a mental and emotional disposition that allows us to meet every challenge vigorously and creatively. The current studies published by Pharma Foods International offer the promise that a naturally-occurring, naturally derived supplement, GABA, may lead the way.
8 Easy Ways to Instantly Boost Your Mood if You’re Social Distancing Alone

Photo credit: Hearst Owned Photo credit: Hearst Owned How do you prevent being alone from turning into feeling lonely —especially during a pandemic ? Science tells us that the key is reaching for small things that might spark happiness by creating a flood of feel-good chemicals in your body. “It’s okay to give ourselves time and space to cry, complain, or be angry at a time like this,” says Miami-based mental health counselor Raquel Espinel Suarez. “But remember to set a timer—literally—so that there’s a hard end to any wallowing. Once it dings, do something that will trigger happiness, bring back a pleasant memory, or make you smile.”
Although happiness generators are often deeply personal, there are certain crowd-pleasing actions that have been scientifically proven to release endorphins and dopamine, the hormones that kickstart happiness. Here, your to-do list for getting chipper—even when you’re feeling anything but. EAT SOMETHING
Turns out the greatest comfort food is actually… all food. According to a 2017 study from the Academy of Finland, the simple act of eating releases endorphins. Whether you’re digging into a delicious pizza or virtuously sipping a flavorless nutritional drink, your brain becomes flooded with its own natural opioids, creating pleasurable feelings. Additional research shows that chowing down releases dopamine not once, but twice—first as we’re consuming the food, and again once the nourishment hits our stomachs. That being said, there are specific foods that can up the ante on feeling blissful. Those include:
Chocolate. Everyone’s favorite indulgence has been shown to release endorphins, dopamine, and serotonin, creating an antidepressant effect—and that’s particularly true of dark chocolate. But to reap the benefits, you only need a square or two…not an Easter basket ‘s worth.
Spicy foods. If your motto is the hotter the better, you may already be familiar with the feel-good flood in your body that occurs after eating chili peppers. Research shows that the burning in your mouth after ingesting capsaicin (the natural chemical that makes peppers hot) is actually a sensation, not a taste—and the scorching it creates sends an SOS signal to your brain to relieve the pain ASAP. That’s when endorphins rush to the rescue as your body’s way of blocking the pain and making you feel good.
6 ways to get your stress hormones under control, this week
Right now, no matter who you are or what you do, it’s a safe bet that you’re probably more stressed than usual. You’re certainly not alone. The COVID-19 outbreak — and all that’s come with it — has most of us on edge.
“The uncertainty about the future, loss of control and financial strain are all contributing to elevated stress levels at this time,” explains naturopath Belinda Kirkpatrick. “There’s also the worry about how elderly relatives and loved ones are coping, and some people feel like they’ve lost their freedom and connection to others. All of these factors combined with the fear of actually getting COVID-19 are keeping cortisol levels — your body’s primary stress hormone — uncomfortably high.”
Dr Jaime Lee, a medical doctor and founder of workplace wellness company Health Quotient, adds that the coronavirus crisis meets all the requirements for elevated cortisol.
“Research has identified three factors that universally lead to stress — uncertainty, loss of control and lack of information,” she explains. “In the current situation, all these factors are met, so stress is impacting everyone on some level.”
Like what you see? Sign up to our bodyandsoul.com.au newsletter for more stories like this. Why cortisol matters
Since it’s commonly used to describe your stress levels, cortisol tends to get a bad rap. Produced by your adrenal glands — which sit on top of your kidneys — cortisol is actually essential to the proper functioning of your entire body.
“Cortisol is important for regulating your blood-sugar levels, sleep-wake cycles, inflammation and blood pressure,” notes Kirkpatrick.
“It also helps you exercise, grow, perform and react quickly to a perceived danger,”adds Dr Lee. “Cortisol acts on almost every tissue in the body, from your immune system, metabolism and brain through to your bones and intestines.”
When functioning normally, a spike in cortisol may occur when your brain perceives a threat — like a car racing towards you — and this primes your body for fight or flight. “If you experience shock or danger, a surge of cortisol will increase sugar in the bloodstream to help you survive and react to the stress,” explains Kirkpatrick. “It also alters immune function and suppresses digestive function to allow you to respond quickly.”
And that’s the real kicker. Although most people aren’t exposed to physical life-or-death threats on the regular, your brain reacts the same way to modern-day threats like snarky emails or news of a worldwide pandemic. “Your stress response can be triggered by any perceived threat, whether it’s physical, biological, chemical or psychological,” says Dr Lee.“To facilitate fight or flight, your heart needs to pump faster, blood needs to be diverted from the internal organs to large muscle groups and your brain needs to focus on the threat, so your sex drive and digestion decreases.”
While this may be useful in certain cases— like when you actually need to dodge a speeding car — living with sustained levels of elevated cortisol means your body can’t function the way it’s supposed to. Too much of a good thing
According to Dr Lee, your body is able to maintain a state of equilibrium when a stress response is a one-off. However, constant stress triggered by news headlines, struggling to juggle homeschooling with working from home and worrying about loved ones day in and day out creates a string of red flags for your brain, keeping your cortisol levels raised.
“If cortisol is chronically elevated, it can result in fatigue, sugar cravings, weight gain, muscle weakness, difficulty sleeping and lowered immunity,” Kirkpatrick says.
Dr Lee adds: “The real danger occurs when your stress response is triggered over and over again without a natural resolution. This overexposure has a significant impact on many of the body’s functions and can have long-term effects such as an increased risk of heart disease, stroke, diabetes, high blood pressure, anxiety, depression, sleep problems, decreased libido and fertility, acne and memory impairment.”
It’s a scary list of complications, but the good news is you have the power to turn it around. Plus, as Kirkpatrick notes, some people may even be experiencing lower cortisol levels during the pandemic because their usual life is more stressful.
“For people who usually burn the candle at both ends, work hard, have a busy social life and are used to running on adrenaline, you may find that slowing down and living in isolation is helping to restore your adrenal glands and reduce your cortisol levels.” A balancing act
In times of low stress, your cortisol levels should spike in the morning (to help you wake up) and then slowly decline during the day, eventually plummeting just before bed (which helps you sleep). According to Dr Lee, it can take three to four hours for your cortisol levels to return to normal after a stress response (like an argument or high-stakes meeting), but Kirkpatrick notes if your levels have been high for some time, it can take up to six months to balance them out.
There are ways to stop your cortisol from peaking in the first place, try these to get you started… 1. Make friends with herbs
If you’re feeling stressed or anxious, Kirkpatrick suggests taking a supplement containing withania (also known as ashwagandha). This herb has been used for centuries in Ayurvedic medicine, and it’s been proven to reduce stress levels and improve your mood and memory. Holy basil is another one to add to your list — research shows that it can help your mind cope with all kinds of stress, whether it be chemical, physical or emotional, and it can also improve feelings of anxiety and depression. Kirkpatrick tips that licorice tea is another great adrenal support. Aim for one to two cups most days, unless you have high blood pressure. 2. Get creative
“Use this time in isolation to slow down and rediscover an old hobby, like cooking, board games or puzzles — one of the ultimate mindful activities,” says Kirkpatrick. Studies also show that engaging in any form of art-making can have a positive influence on stress levels no matter […]
Researchers Developing Fanny Pack Exoskeleton To Improve Walking In Children With Cerebral Palsy
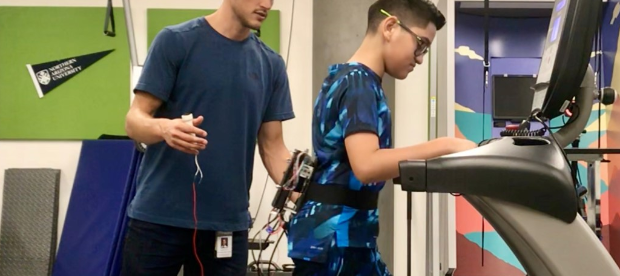
Benjamin Conner, a researcher at the University of Arizona, and his team are working on developing new ways children with Cerebral Palsy can train their brains to learn effective ways to walk, ultimately allowing them to be a lot more independent as they grow older and move into adulthood.
The fanny pack powered exoskeleton, that’s worn on the waist, consists of motors and steel cables that are attached to a pulley at the ankle. As a child walks, the motors are able to help with the movement by increasing or decreasing resistance. This serves a variety of purposes – first, it serves as an assistive feature designed to make walking easier for kids with Cerebral Palsy. The exoskeleton works in tandem with the muscles and helps with a more normal and natural walking pattern. Second, it also acts as a therapeutic intervention and helps with retraining the brain to adapt to a more natural walking movement. In this mode, the exoskeleton is designed to not assist, and makes walking a bit difficult for the children by adding resistance. The harder the children push, the more resistance the exoskeleton adds. This helps children with CP to build muscle memory and strengthen their muscles, ultimately training their brain to adapt to a more steady walking pattern.
Current treatment for people with CP includes muscle or nerve injections, oral relaxants, physical therapy and orthopedic surgery. This exoskeleton will work to supplement these methods. It is still being developed in the College of Medicine’s lab and the team hopes to make it commercially available to families in the future.
Read the source link for more information on this exoskeleton.
Source: Ktar News , University of Arizona
Image Gallery:
New therapeutic targets for treating memory impairment in Down syndrome

Barcelona, 4th May, 2020. A team of researchers led by Dr. Victoria Puig from the Hospital del Mar Medical Research Institute (IMIM), which also involved the Centre for Genomic Regulation (CRG), has studied the neural basis of intellectual disability in mice with Down syndrome and has discovered that the neural networks of brain circuits relevant to memory and learning are over-activated and that the connectivity of these circuits is poor.
The researchers have also observed that neural activity during sleep is abnormal and probably interferes with memory consolidation. The study has even identified biomarkers in brain rhythms that can predict memory deficits in the mice which are corrected by chronic treatment with a natural component of green tea, epigallocatechin gallate, which other studies have already shown to improve executive function in adults with Down syndrome.
“These results suggest that both hyperactivity of neuronal networks and deficiencies in the connectivity of specific brain circuits are possible dysfunctional mechanisms that contribute to memory deficits in Down syndrome and, therefore, offer new therapeutic possibilities for treating intellectual disability,” explains Dr. Victoria Puig, researcher in the Integrated Pharmacology and Systems Neuroscience Research Group at the IMIM.
To date, it had been recognised that epigallocatechin gallate corrects certain alterations at the molecular and cellular levels derived from the trisomy of chromosome 21 that are associated with cognitive deficits in Down syndrome. However, a dynamic description of the actions of epigallocatechin gallate on neural activity during distinct brain states was lacking. This is, therefore, the first time that anyone has looked at how mouse brain responds to chronic treatment with epigallocatechin gallate at a functional level in trisomy conditions.
The study involved recording neuronal activity simultaneously in two brain regions critical for learning and memory, the prefrontal cortex and the hippocampus, in trisomic and non-trisomic mice during periods of rest while awake, asleep, and during the performance of a simple memory task. The data was collected before and after one month of treatment with epigallocatechin gallate, and the alterations in the activity of the neuronal networks in the two regions as well as the connectivity of the circuitry correlating with memory capacities were analysed and found to have been corrected with the green tea extract.
According to Dr. Mara Dierssen from the Cellular and Systems Neurobiology lab at the CRG, “This study provides an in-depth description of the neurophysiological abnormalities present in different brain states in Down syndrome model mice and provides the keys for understanding the cellular mechanisms underlying the improved executive function observed in people with Down syndrome after chronic treatment with epigallocatechin gallate”. (De la Torre R et al. Lancet Neurology del 2016 doi: 10.1016/S1474-4422(16)30034-5)
Dr. Maria Alemany, first author of the paper and also a researcher in the IMIM’s Integrated Pharmacology and Neuroscience Systems research group, explains “that the group is evaluating the effects of cognitive stimulation during brain development on the neuronal activity of mice with Down syndrome. This is important for understanding the cellular mechanisms of cognitive stimulation that are normally used in people to improve intellectual disability”.
Down syndrome is a genetic alteration produced by the presence of an extra copy of chromosome 21, which is why this syndrome is also known as trisomy 21. It is the main cause of intellectual disability and the most common human genetic alteration. It is estimated that 34,000 people with Down’s syndrome live in Spain and that there are a total of six million sufferers worldwide.
According to Dr. Mara Dierssen from the Cellular and Systems Neurobiology lab at the CRG, “This study provides an in-depth description of the neurophysiological abnormalities present in different brain states in Down syndrome model mice and provides the keys for understanding the cellular mechanisms underlying the improved executive function observed in people with Down syndrome after chronic treatment with epigallocatechin gallate”. (De la Torre R et al. Lancet Neurology del 2016 doi: 10.1016/S1474-4422(16)30034-5)
###
Reference article
Maria Alemany-González, Thomas Gener, Pau Nebot Marta Vilademunt, Mara Dierssen, M. Victoria Puig. Prefrontal-hippocampal functional connectivity encodes recognition memory and is impaired in intellectual disability. PNAS .
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.
What dreams may come: Why you’re having more vivid dreams during the pandemic

An interesting side effect of the coronavirus pandemic is the number of people who say they are having vivid dreams.
Many are turning to blogs and social media to describe their experiences.
https://twitter.com/SiouxsieW/status/1247983766179434496
While such dreams can be confusing or distressing, dreaming is normal and considered helpful in processing our waking situation, which for many people is far from normal at the moment. While we are sleeping
Adults are recommended to sleep for seven to nine hours to maintain optimal health and well-being.
When we sleep we go through different stages which cycle throughout the night.
This includes light and deep sleep and a period known as rapid eye movement (REM) sleep, which features more prominently in the second half of the night.
As the name implies, during REM sleep the eyes move rapidly. Dreams can occur within all sleep stages but REM sleep is considered responsible for highly emotive and visual dreams.
We typically have several REM dream periods a night, yet we do not necessarily remember the experiences and content.
Researchers have identified that REM sleep has unique properties that help us regulate our mood, performance and cognitive functioning.
Some say dreams act like a defence mechanism for our mental health, by giving us a simulated opportunity to work through our fears and to rehearse for stressful real-life events.
This global pandemic and associated restrictions may have impacts on how and when we sleep. This has positive effects for some and negative effects for others. Both situations can lead to heightened recollection of dreams. Disrupted sleep and dreams
During this pandemic, studies from China and the UK show many people are reporting a heightened state of anxiety and are having shorter or more disturbed sleep.
Ruminating about the pandemic, either directly or via the media, just before going to bed can work against our need to relax and get a good night’s sleep. It may also provide fodder for dreams.
When we are sleep deprived, the pressure for REM sleep increases and so at the next sleep opportunity a so-called rebound in REM sleep occurs. During this time dreams are reportedly more vivid and emotional than usual. More time in bed
Other studies indicate that people may be sleeping more and moving less during the pandemic.
If you’re working and learning from home on flexible schedules without the usual commute it means you avoid the morning rush and don’t need to get up so early.
Heightened dream recall has been associated with having a longer sleep as well as waking more naturally from a state of REM sleep.
If you’re at home with other people you have a captive audience and time to exchange dream stories in the morning. The act of sharing dreams reinforces our memory of them. It might also prepare us to remember more on subsequent nights.
This has likely created a spike in dream recall and interest during this time. The pandemic concerns
Dreaming can help us to cope mentally with our waking situation as well as simply reflect realities and concerns.
In this time of heightened alert and changing social norms, our brains have much more to process during sleep and dreaming. More stressful dream content is to be expected if we feel anxious or stressed in relation to the pandemic, or our working or family situations.
Hence more reports of dreams containing fear, embarrassment, social taboos, occupational stress, grief and loss, unreachable family, as well as more literal dreams around contamination or disease are being recorded.
https://twitter.com/DoubleEph/status/1251080859924541440
An increase in unusual or vivid dreams and nightmares is not surprising.
Such experiences have been reported before at times associated with sudden change, anxiety or trauma, such as the aftermath of the terrorist attacks in the US in 2001, or natural disasters or war.Those with an anxiety disorder or experiencing the trauma first-hand are highly likely also to experience changes to dreams.But such changes are also reported by those witnessing events like the 9/11 attacks second-hand or via the media. Problems solved in dreams One theory on dreams is they serve to process the emotional demands of the day, to commit experiences to memory, solve problems, adapt and learn.This is achieved through the reactivation of particular brain areas during REM sleep and the consolidation of neural connections.During REM the areas of the brain responsible for emotions, memory, behaviour and vision are reactivated (as opposed to those required for logical thinking, reasoning and movement, which remain in a state of rest).The activity and connections made during dreaming are considered to be guided by the dreamer’s waking activities, exposures and stressors.The neural activity has been proposed to synthesise learning and memory.The actual dream experience is more a by-product of this activity, which we assemble into a more logical narrative when the remainder of the brain attempts to catch up and reason with the activity on waking. Please … go to sleep If disrupted sleep and dreams are problematic or distressing for you, consider how your sleep schedule and behaviour has changed with the pandemic. Maybe seek advice for supporting your sleep and well-being during this time.My colleagues and I at the Sleep/Wake Research Centre have produced several information sheets on sleep during the pandemic.We are also conducting a survey concerning the sleep of people living in New Zealand. This explores factors affecting sleep during the pandemic, and participants can comment on their dreaming. For the latest updates on the coronavirus, visit here . Rosie Gibson , Research Officer, Sleep/Wake Research Centre, College of Health, Massey University This article is republished from The Conversation under a Creative Commons license. Read the original article .
Coronavirus: Why you’re having weird dreams during isolation
Many are turning to blogs and social media to describe their experiences. Had an awful anxiety dream this morning. I was trying to buy a train ticket to get to Ms13. I couldn’t get the machine to work (it was like a pinball machine). Then the person at the desk booked me a 6 hour coach trip instead & wouldn’t change it. Woke with my heart pounding! — Dr Siouxsie Wiles (@SiouxsieW) April 8, 2020 While such dreams can be confusing or distressing, dreaming is normal and considered helpful in processing our waking situation, which for many people is far from normal at the moment.
WHILE WE ARE SLEEPING
Adults are recommended to sleep for seven to nine hours to maintain optimal health and well-being.
When we sleep we go through different stages which cycle throughout the night. This includes light and deep sleep and a period known as rapid eye movement (REM) sleep, which features more prominently in the second half of the night. As the name implies, during REM sleep the eyes move rapidly.
Dreams can occur within all sleep stages but REM sleep is considered responsible for highly emotive and visual dreams.
We typically have several REM dream periods a night, yet we do not necessarily remember the experiences and content. Researchers have identified that REM sleep has unique properties that help us regulate our mood, performance and cognitive functioning.
Some say dreams act like a defence mechanism for our mental health, by giving us a simulated opportunity to work through our fears and to rehearse for stressful real-life events.
This global pandemic and associated restrictions may have impacts on how and when we sleep. This has positive effects for some and negative effects for others. Both situations can lead to heightened recollection of dreams.
DISRUPTED SLEEP AND DREAMS
During this pandemic, studies from China and the UK show many people are reporting a heightened state of anxiety and are having shorter or more disturbed sleep.
Ruminating about the pandemic, either directly or via the media, just before going to bed can work against our need to relax and get a good night’s sleep. It may also provide fodder for dreams.
When we are sleep deprived, the pressure for REM sleep increases and so at the next sleep opportunity a so-called rebound in REM sleep occurs. During this time dreams are reportedly more vivid and emotional than usual.
Looking for things to pass the time? The best shows to watch, the funniest videos, the best hacks and home workouts? Find it all at our Life (goes on) in Lockdown section
MORE TIME IN BED
Other studies indicate that people may be sleeping more and moving less during the pandemic.
If you’re working and learning from home on flexible schedules without the usual commute it means you avoid the morning rush and don’t need to get up so early.
Heightened dream recall has been associated with having a longer sleep as well as waking more naturally from a state of REM sleep.
If you’re at home with other people you have a captive audience and time to exchange dream stories in the morning. The act of sharing dreams reinforces our memory of them. It might also prepare us to remember more on subsequent nights.
This has likely created a spike in dream recall and interest during this time.
THE PANDEMIC CONCERNS
Dreaming can help us to cope mentally with our waking situation as well as simply reflect realities and concerns.
In this time of heightened alert and changing social norms, our brains have much more to process during sleep and dreaming. More stressful dream content is to be expected if we feel anxious or stressed in relation to the pandemic, or our working or family situations.
Hence more reports of dreams containing fear, embarrassment, social taboos, occupational stress, grief and loss, unreachable family, as well as more literal dreams around contamination or disease are being recorded. Today’s #CoronaDreams – Was jogging with my brother @theboxsurfer and then we saw what looked like a dead tiger hit by a car. Went close and then it jumped up and started chasing us. We ran into a nearby park only to find it filled with lions, tigers and ligers. Sigh — tyro (@DoubleEph) April 17, 2020 Had my first #CoronaDreams last night.
It was a sequence of maze-like events trying to get from PointA to PointB in the real-world (note: that’s my usual stress dream) but now there’s the added feature of trying to avoid all the UNmasked ppl in my path 😳😤😭 — Kate Ertmann 💪🏼🌊⬆ (@GOK8) April 25, 2020 I’ve been having the weirdest dreams lately… like REALLY weird! A mix of old normal, new normal, work, old social life, puzzles and walks… one dream even featured @patel4witham holding a course on how to build a house… Anyone else or just me? 🤔😫😂 #coronadreams pic.twitter.com/2lpfxm29Ym — Charlotte Sullivan (@CharlotteSulli) April 22, 2020 An increase in unusual or vivid dreams and nightmares is not surprising. Such experiences have been reported before at times associated with sudden change, anxiety or trauma, such as the aftermath of the terrorist attacks in the US in 2001, or natural disasters or war.
Those with an anxiety disorder or experiencing the trauma first-hand are highly likely also to experience changes to dreams.
But such changes are also reported by those witnessing events like the 9/11 attacks second-hand or via the media.
PROBLEMS SOLVED IN DREAMS One theory on dreams is they serve to process the emotional demands of the day, to commit experiences to memory, solve problems, adapt and learn.This is achieved through the reactivation of particular brain areas during REM sleep and the consolidation of neural connections.During REM the areas of the brain responsible for emotions, memory, behaviour and vision are reactivated (as opposed to those required for logical thinking, reasoning and movement, which remain in a state of rest).The activity and connections made during dreaming are considered to be guided by the dreamer’s waking activities, exposures and stressors.The neural activity has been proposed to synthesise learning and […]
Aromatherapy can be used to improve symptoms like depression, stress, and pain in post-partum women

( Natural News ) The volatile oils present in plants have long been used to treat common human ailments. The earliest records of their use date as far back as the time of the Ancient Egyptians, who were credited with inventing the first ever method of extraction for these precious oils. Today, these natural products are known as essential oils and are commonly used in an alternative or complementary therapy known as aromatherapy.
Highly volatile and concentrated, essential oils got their name because early scientists believed them to be the essence of their plant sources’ odor and flavor . These oils are also rich in active and aromatic plant compounds that give them various medicinal properties. Essential oils are now widely used for their antimicrobial, antioxidant, brain-stimulating and mood-lifting effects, which have all been proven by science.
In a recent study, a team of American and Iranian researchers investigated whether aromatherapy could improve the symptoms experienced by women after childbirth . Some of the most common ones include pain, anxiety, mood swings, difficulty sleeping and a long-lasting form of depression called postpartum depression. The researchers discussed their findings in an article published in the journal Complementary Therapies in Clinical Practice . The benefits of aromatherapy for new mothers
According to the researchers, aromatherapy is a popular method used to manage the symptoms of various physiologic processes and diseases. For their study, they searched international databases like PubMed, Google Scholar, Web of Science, and Scopus for randomized controlled trials and quasi-experimental studies on the use of aromatherapy to reduce postpartum symptoms.
The researchers reported finding 34 studies in total, 17 of which met their criteria and were included in their review. The studies involved a total of 1,400 women who used a variety of aromatherapy. The researchers found that the results of these studies all pointed to aromatherapy improving common postpartum-related issues, such as depression , stress, pain, anxiety and fatigue.
Based on these findings, the researchers concluded that aromatherapy has therapeutic effects that can help women during the postpartum period . However, they also advised caution when using essential oils as safety concerns were not addressed in any of the studies. The history and various applications of aromatherapy
While the origin of aromatherapy has not been linked to a particular place or region, archaeological findings have revealed that one of the first distillation machines for extracting essential oils was developed in Ancient Egypt. The early Egyptians used cedarwood, clove , cinammon, nutmeg and myrrh essential oils to embalm the dead . They also mixed these oils with herbs to make fragrances.
Similarly, the Ancient Greeks created perfumes and medicines using essential oils. Hippocrates, known as the “father of medicine,” is believed to have used aromatherapy for healing. But while the earliest records of their medicinal use all came from the western world, the practice of using aromatic oils to enhance the mood is said to have originated in China.
The term “aromatherapy” was first coined in 1937 by a French chemist named Rene-Maurice Gattefosse, who discovered that some essential oils can promote skin healing. Gatterfosse, who was said to have used lavender oil to cure his burn wounds, developed an interest in essential oils afterward. During World War II, a French surgeon named Jean Valnet was also reported to have used essential oils to help heal the wounds of soldiers.
Today, essential oils and their applications have evolved considerably. No longer limited to just topical use, essential oils are now also inhaled to stimulate the olfactory system and influence the limbic system – a set of structures in the brain that process emotions and memory . This allows essential oils to influence a person’s heart rate , blood pressure, breathing, stress levels and even hormonal balance.
Here are some conditions that can be treated with aromatherapy : Alopecia
Circulatory problems
Depression
Fatigue
Headaches
Insomnia
Menstrual problems
Menopausal problems
Muscular aches
Negative feelings (e.g., agitation, anxiety, stress)
Pain and localized aches
Aromatherapy is a natural treatment that can be used to manage postpartum symptoms, as well as other mood-related issues. To learn more about its other uses and benefits, visit Naturopathy.news .
Sources include:
Why You’re Having More Vivid Dreams During The Pandemic
An interesting side effect of the coronavirus pandemic is the number of people who say they are having vivid dreams
While such dreams can be confusing or distressing, dreaming is normal and considered helpful in processing our waking situation, which for many people is far from normal at the moment.
Adults are recommended to sleep for seven to nine hours to maintain optimal health and well-being.
When we sleep we go through different stages which cycle throughout the night. This includes light and deep sleep and a period known as rapid eye movement (REM) sleep, which features more prominently in the second half of the night. As the name implies, during REM sleep the eyes move rapidly.
Dreams can occur within all sleep stages but REM sleep is considered responsible for highly emotive and visual dreams.
We typically have several REM dream periods a night, yet we do not necessarily remember the experiences and content. Researchers have identified that REM sleep has unique properties that help us regulate our mood, performance and cognitive functioning.
Some say dreams act like a defence mechanism for our mental health , by giving us a simulated opportunity to work through our fears and to rehearse for stressful real-life events.
This global pandemic and associated restrictions may have impacts on how and when we sleep . This has positive effects for some and negative effects for others. Both situations can lead to heightened recollection of dreams.
During this pandemic, studies from China and the UK show many people are reporting a heightened state of anxiety and are having shorter or more disturbed sleep .
Ruminating about the pandemic, either directly or via the media, just before going to bed can work against our need to relax and get a good night’s sleep. It may also provide fodder for dreams. When we are sleep deprived, the pressure for REM sleep increases and so at the next sleep opportunity a so-called rebound in REM sleep occurs. During this time dreams are reportedly more vivid and emotional than usual.
Other studies indicate that people may be sleeping more and moving less during the pandemic.
If you’re working and learning from home on flexible schedules without the usual commute it means you avoid the morning rush and don’t need to get up so early. Heightened dream recall has been associated with having a longer sleep as well as waking more naturally from a state of REM sleep.
If you’re at home with other people you have a captive audience and time to exchange dream stories in the morning. The act of sharing dreams reinforces our memory of them. It might also prepare us to remember more on subsequent nights.
This has likely created a spike in dream recall and interest during this time.
Dreaming can help us to cope mentally with our waking situation as well as simply reflect realities and concerns.
In this time of heightened alert and changing social norms, our brains have much more to process during sleep and dreaming. More stressful dream content is to be expected if we feel anxious or stressed in relation to the pandemic, or our working or family situations.
Hence more reports of dreams containing fear, embarrassment, social taboos, occupational stress, grief and loss, unreachable family, as well as more literal dreams around contamination or disease are being recorded .
An increase in unusual or vivid dreams and nightmares is not surprising. Such experiences have been reported before at times associated with sudden change, anxiety or trauma, such as the aftermath of the terrorist attacks in the US in 2001, or natural disasters or war.
Those with an anxiety disorder or experiencing the trauma first-hand are highly likely also to experience changes to dreams. But such changes are also reported by those witnessing events like the 9/11 attacks second-hand or via the media. One theory on dreams is they serve to process the emotional demands of the day, to commit experiences to memory, solve problems, adapt and learn. This is achieved through the reactivation of particular brain areas during REM sleep and the consolidation of neural connections.
During REM the areas of the brain responsible for emotions, memory, behaviour and vision are reactivated (as opposed to those required for logical thinking, reasoning and movement, which remain in a state of rest).
The activity and connections made during dreaming are considered to be guided by the dreamer’s waking activities, exposures and stressors.
The neural activity has been proposed to synthesise learning and memory. The actual dream experience is more a by-product of this activity, which we assemble into a more logical narrative when the remainder of the brain attempts to catch up and reason with the activity on waking.
If disrupted sleep and dreams are problematic or distressing for you, consider how your sleep schedule and behaviour has changed with the pandemic. Maybe seek advice for supporting your sleep and well-being during this time.
My colleagues and I at the Sleep/Wake Research Centre have produced several information sheets on sleep during the pandemic.
We are also conducting a survey concerning the sleep of people living in New Zealand. This explores factors affecting sleep during the pandemic, and participants can comment on their dreaming.
How Not Only To Live Longer, But Healthier, According to Global Experts

If you want to increase your “healthspan” as well as your lifespan, you need to take simple daily actions involving physical activity, nutrition and social connection. That was the message from experts at the International Federation on Ageing’s (IFA) 14th global conference, Towards a Decade of Healthy Ageing – From Evidence to Action, held in Toronto this August. The panel discussion, Associations Between Physical Activity and Healthy Ageing, offered some strategies. “If we’re expecting a slow and depressing decline, that has a real affect on our health. It’s a self-fulfilling prophecy.” Focus on enjoying life
Although exercise was the focus of the session, several presenters touched on other aspects of healthy aging. For example, psychotherapist Nicole Christina, the Syracuse, NY-based producer of the Zestful Aging podcast , talked about attitude, social interaction and healthy eating as well as exercise.
Christina, who interviews thought leaders on healthy aging, advocates “balance and pleasure” rather than a focus on “eating clean.” When it comes to food, “there’s so much to worry about,” she said. “There’s gluten, fat, carbs, GMOs, antioxidants, organics, probiotics… Are my vegetables seasonal? Microbio friendly? Were they picked by fair trade workers [and] under what conditions? Do they have a carbon footprint?” In her view, “if you are going to be so stressed about [whether] your kale is clean and organic, you might [as well] just have a sandwich.”
Christina also applies this philosophy to physical activity. “Exercise is not supposed to be a punishment for eating…. It shouldn’t feel like a chore because our bodies are made to move. They enjoy moving and we feel better when we move.”
As well, she asked audience members to look at their attitudes about aging. “If we’re expecting a slow and depressing decline, that has a real effect on our health. It’s a self-fulfilling prophecy,” she said, adding that research shows that people with a positive attitude live seven and a half years longer. In addition, she stressed the need for social connection because “being alone is not only uncomfortable, it’s lethal.” Instead, she advises us “to find our tribe where we feel we feel a sense of belonging.” Nurturing close connections with others is critical in healthy aging. Photo: Flickr/Creative Commons, Jeremy Bronson. Find the doctor within
Christina wasn’t the only presenter to broach the importance of social connection to older adults. Hui-Chuan Hsu, a researcher in gerontology, told the audience that saying hello to five persons and chatting for at least five minutes each day was part of the homework for participants in Taiwan’s Integrated Self-healing Enhancement Program (SEP).
In addition to promoting social connection, the health promotion program for older adults focuses on exercise and nutrition education and asks participants to draw on their natural healing power. “You can empower yourself, you can make yourself stronger, you can make yourself happier,” Hsu said, noting that program participants show increased muscle strength, reduced blood pressure and increased walking speed.
Stimulate brain and body
The session also featured another health promotion program, Healthy Ageing Promotion Program for You (HAPPY), geared to vulnerable seniors. We wanted to build cognitive reserve and delay frailty in residents who are “slipping down the ladder,” said associate professor Reshma Merchant, division head of geriatric medicine at National University Hospital in Singapore.
The program was developed after a study conducted by Merchant showed more than a third of older adults in Bukit Panjang in western Singapore were on the verge of becoming frail, putting them at higher risk for developing a disability.
HAPPY features dual-task exercises to train participants physically and mentally. For example, participants may be asked to memorize cards and then tap different body parts while marching on the spot. Early results show that HAPPY participants experience less depression and anxiety and improved physical function and cognition. Tai chi can help with balance and prevent falls. Photo: Flickr/Creative Commons, Derek Barrett. Dance and move
There’s also evidence that dancing improves cognition, according to Dr. Sandra Hirst, an associate professor in nursing at the University of Calgary, who performed a broad review of creative aging through dance/movement approaches . This project was sparked after witnessing the dramatic improvement in memory and conversational ability of an 84-year-old, long-term care resident after dancing with his wife.
Dr. Hirst also pointed out that the review showed that movement activities like tai chi reduce falls and increase mobility, flexibility and balance. “When you think about walking up and down stairs, when you’re thinking about getting out of the bathtub, when you think about walking through a side gate, changes in balance become extremely important,” she explained.
The fifth presenter was Christina Bosch-Farré, who discussed preliminary findings from the Survey of Healthy, Aging and Retirement in Europe (SHARE), which studied more than 50,000 older adults. She noted that low educational level, lack of employment and low income were associated with an inactive and unhealthy lifestyle.
Speaking of unhealthy lifestyles, Hui-Chuan Hsu pointed out that between 50 to 75 percent of chronic disease is a result of our way of living. “We increase our lifespan, but our healthy span doesn’t increase that much,” she said.
5 Ways to Keep Your Brain Healthy During the Pandemic

man sits on floor as he meditates Is your brain feeling … foggy? You’re not just imagining it. “Keeping busy with regular activities and spending time with others are both key to brain health and lowering your risk of dementia — and they’re also things most of us are lacking right now,” says psychiatrist Gary Small, director of the UCLA Longevity Center. The good news is there is plenty you can do during this pandemic to keep your brain neurons firing. Here are five things to try. Stay active
Exercise won’t just keep your heart healthy and your weight down as you face lots of time inside — it helps your brain stay in shape, too. “We know that regular aerobic exercise boosts blood flow to your brain, and also increases the size of your hippocampus, the part of your brain that’s involved in verbal memory and learning,” explains geriatrician Zaldy Tan, medical director of the UCLA Alzheimer’s and Dementia Care Program. His own study, among others, helped uncover the link: “When we performed MRI scans of over 2,000 people over age 60, we found that the more active they were, the bigger their hippocampus,” he says. “Even better, the protective effects were highest in those over age 75, which suggests that it’s never too late to start.”
You don’t need much exercise to see benefits. Walking or cycling just three times a week appears to improve thinking skills after six months in formerly sedentary people over age 55, according to a recent study published in the medical journal Neurology. A heart-healthy diet adds even more benefits: People who followed the DASH (dietary approaches to stop hypertension) diet, an eating plan rich in fruits, veggies, whole grains, lean protein and low-fat dairy, fared even better.
Besides getting in a regular walk (or two) during the day, limit sitting as much as possible to preserve your brain health. Adults ages 45 to 75 who sit for anywhere from three to seven hours each day have a substantial thinning of their medial temporal lobe, which is where the brain forms new memories, according to a 2018 study. “This is one of the types of changes that precede dementia,” says study coauthor Small.
And don’t forget resistance training , if you can squeeze it in, Small adds. A 2019 study found that lab rats who “weight trained” (meaning they were trained to climb a 3-foot-high ladder with dumbbells attached) three times a week performed much better on memory tests after five weeks than a control group. “It seems to help reduce some of the brain inflammation associated with dementia,” Small says. Target stress
Stress itself is toxic to brain cells. “It kills them off and shrinks both the prefrontal cortex and the hippocampus, both areas of the brain responsible for memory and learning,” says psychiatrist Majid Fotuhi, an affiliate staff member at the Johns Hopkins University School of Medicine. A review of studies published in April 2018, which followed almost 30,000 people for at least 10 years, found that people who reported “clinically significant anxiety” were more likely to develop dementia later in life.
Practicing mindfulness techniques such as meditation or yoga may help fend off anxiety’s toll on the brain. One UCLA study found that people over age 55 who enrolled in a 12-week program consisting of an hour of a type of meditative yoga once a week as well as 20 minutes of at-home meditation had significant improvements in both verbal memory (the ability to remember word lists) and visual-spatial memory (the ability to find and remember locations). Fotuhi says meditation and yoga “appear to enhance production of brain-derived neurotrophic factor, a protein that stimulates connections between your brain neurons.”
Even if Downward-Facing Dog isn’t your thing, you can reap similar benefits by just adding deep breathing exercises into your daily routine five to 10 minutes a day, Fotuhi says. Limit anxiety and sleep medications
It may be tempting to pop a Xanax or ask your physician for a prescription of sleep meds during these stressful times. But try to avoid doing so if you can, says Small. People who take a benzodiazepine — drugs such as diazepam (Valium), lorazepam (Ativan) or alprazolam (Xanax) — regularly are about 50 percent more likely to develop Alzheimer’s, according to a review published in the Journal of Clinical Neurology last year.
Another recent study published in the Journal of the American Geriatric Society found a link between long-term use of the sleeping pill zolpidem (Ambien) and Alzheimer’s. The same holds true for over-the-counter sleep aids such as diphenhydramine or doxylamine (Unisom). These medications, found in the “PM” versions of Tylenol, Aleve and Advil as well as allergy meds such as Zyrtec and Benadryl, are anticholinergics, a type of drug that has been linked to lower cognitive ability and possibly even dementia in elderly adults, according to a study published in JAMA Neurology.
Sleep itself is important for brain health, because it gives your body a chance to clean out all the waste, such as beta-amyloid plaques that raise risk of developing dementia, Small says. But rather than relying on meds, you’re better off practicing good sleep habits such as cutting out all caffeine after lunch, staying away from electronic devices for a couple of hours before bed, and maintaining regular sleep and wake times every day. Stay connected as much as possible
Social isolation is a major risk factor for dementia, says Small. If you normally enjoy activities such as a book club or game night, try to arrange them virtually . “My wife and I play the card game hearts online with our friends a couple times a week,” Small says. Or use the Zoom conferencing platform to create a virtual party where you can hang out with close family and friends. One landmark University of Michigan study found that just 10 minutes of talking to another person can help boost memory and cognitive performance.
You can also try connecting a little more deeply on social media; if you […]
6 popular supplements that could boost your immune functions

The current COVID-19 pandemic gives us a good opportunity to pay attention to our immune system, which can influence how our body responds if we are exposed to the disease.
Our daily lifestyle habits can strongly affect our immune system. Among these habits, eating healthy foods to get sufficient nutrients is very important.
A newly published study from the University of Southampton and elsewhere shows that a healthy diet with nutritional supplements could support your body to fight COVID-19.
The team suggests that supplements are a safe, effective, and low-cost way to support an optimal immune system where the diet does not provide enough of certain vitamins and minerals
Here we introduce 6 popular nutritional supplements for different purposes and different groups of people. These supplements aim to boost your daily immune functions and make your body stronger.
> Supplements for immune functions, memory ability, and liver health
This type of supplement could boost the immune system, promote memory and liver health, and relieve stress.
Genius Mushroom can deliver an organic wellness formula unlike any other: Enhance mental clarity, immune function, natural energy, and more.
It increases immune support to another level with reishi mushroom extract. This mushroom extract has been used for centuries to help people avoid the common cold. It also can improve mood and potentially act as a detoxifying liver cleanse.
In addition, Lions Mane provides a safe alternative to highly questionable nootropics and smart drugs hitting the market nowadays. It could boost memory functions.
start=”2″> Supplements for immune functions, weight management, and glucose metabolism
This type of supplement not only supports your immune system but also boosts your glucose metabolism and helps with healthy weight management.
Amazing Nutrition Berberine Plus is a product that provides these health benefits and also promotes your heart and gut health.
The capsules feature berberine hydrochloride, a form that has been widely studied and may be absorbed more easily by the body.
In addition, the product is free of shellfish, eggs, fish, peanuts, milk, wheat, soy, and tree nuts, and it is a great choice for people with dietary sensitivities or diet preferences.
start=”3″> Supplements for immune functions, muscle recovery, and endurance
This type of supplement could boost the immune system whiling improving muscle recovery and endurance.
OPTIMUM NUTRITION ZMA is a zinc and magnesium supplement for immune support and muscle functions.
It contains high-quality forms of zinc, magnesium, and vitamin B6. The supplement can support greater nutritional needs to fuel your active lifestyle and fill gaps in your micronutrient intake.
start=”4″> Supplements for men’s immune functions
This type of supplement focuses on men’s immune functions and support men’s daily nutrient needs.
GNC Mega Men provides 20 vitamins and minerals, including Vitamin A, Vitamin C, Vitamin B-6, and Vitamin B-12.
It offers key nutrients for men’s health, antioxidants, brain health, heart health, and immune health, plus antioxidants. In addition, selenium, lycopene, and vitamin E can support prostate health.
start=”5″> Supplements for women’s immune functions
This type of supplement focuses on women’s immune functions and supports women’s daily nutrient needs.
One A Day Women’s 50+ offers a wide variety of key nutrients in an easy to take, daily tablet.It may help support your healthy brain function with B vitamins and may help promote bone health, joint health, heart health, eye health, immune health, and physical energy. start=”6″> Supplements for vegans and vegetarians Carnivora Vegi-Caps is a supplement that helps reduce fatigue, strengthen, and support your immune system.It can help destroy toxins In your body, boost health and wellness, increase energy levels, reduce fatigue, improve mental clarity, maintain your white blood cells, improve heart health, and supercharge your immune system.It selectively targets and eliminates abnormal cells and waste products, called “free radicals”, in your body without harm to a single normal cell.It contains 17 nutrients, naturally occurring in the plant, working together to support the body’s natural healing process. We have affiliate partnerships and get a share of the revenue from your purchase. Source: Amazon .
Green tea, turmeric and more: 12 Supplements and herbs that can naturally relieve pain caused by arthritis

( Natural News ) Arthritis refers to a group of degenerative conditions that target the joints and the tissues that surround the joints. Common types of arthritis include osteoarthritis, rheumatoid arthritis and gout. Although each type is influenced by unique factors, arthritis is generally characterized by pain, stiffness and inflammation in the hands, hips and knees. Medicinal herbs, vitamins and supplements for arthritis
Fortunately, there are several herbs, vitamins and supplements that work to control inflammation and reduce joint pain. Here are 12 natural remedies that you can use to treat arthritis :
> Glucosamine – Glucosamine is a natural chemical compound found inside the body that provides structural support to cartilage, the rubbery tissue that cushions bones at the joint to prevent friction. As a supplement, it helps fortify worn cartilage in older adults with arthritis. Additionally, glucosamine supplements help curb inflammation.
Omega-3 fatty acids – Omega-3 fatty acids can inhibit the production of molecules linked to inflammation, like eicosanoids and cytokines. Most fatty fishes like salmon and tuna are excellent sources of omega-3 fatty acids, so be sure to add them to a balanced diet.
Green tea – This popular herbal drink contains epigallocatechin-3-gallate (EGCG), a unique plant compound with anti-inflammatory properties. It is also rich in polyphenols that can minimize swollen joints and reduce the likelihood of arthritis flare-ups.
Vitamin D – Vitamin D, an essential micronutrient, is also known to play an important role in the prevention of inflammatory conditions like arthritis. In particular, low vitamin D levels are closely associated with joint pain. Take vitamin D supplements to prevent severe arthritis flare-ups and ease inflammation.
S-adenosylmethionine (SAM-e) – SAM-e is a compound in the body that supports hormone production and regulation, but it also acts as a natural painkiller. When taken as a supplement, SAM-e also stimulates the growth of cartilage and increases levels of serotonin, an important chemical and neurotransmitter in the brain that inhibits pain perception.
Capsaicin – Capsaicin is the main active compound in chili peppers. Besides the spiciness, capsaicin is also known for its antioxidant compounds that act as natural painkillers. It is available as supplements or as topical creams and gels. For arthritis, it’s best to use topical capsaicin to minimize pain quickly.
Turmeric – This popular Indian spice is commonly used to treat various inflammatory conditions thanks to curcumin , its main active compound. Curcumin also helps reduce pain, especially in individuals with osteoarthritis and rheumatoid arthritis. (Related: Curcumin enhances bioavailability of green tea flavonoids .)
Avocado/soybean unsaponifiables (ASU) – ASU is a vegetable extract that works to block inflammatory chemicals and prevent the deterioration of cartilage. ASU also helps repair damaged connective tissues around joints affected by rheumatoid arthritis.
Cat’s claw – Cat’s claw, a tropical vine native to Central and South America, has antioxidant and anti-inflammatory effects against rheumatoid arthritis. It also helps fight joint pain and ward off potential flare-ups.
Fish oil – Fish oil is harvested from the tissues of fatty fishes. If you don’t like to eat fish, then you can take fish oil supplements to avoid a deficiency in essential omega-3 fatty acids that help ease inflammation.
Gamma-linolenic acid – Classified as an omega-6 fatty acid, GLA is a fatty substance found in various plant-based foods and healthy oils. It is believed to fight inflammation, relieve stiff joints and reduce pain linked to rheumatoid arthritis .
Ginger – Like turmeric, ginger is a popular go-to remedy for various inflammatory ailments. Its strong antioxidant compounds are especially potent against stiffness and joint pain caused by rheumatoid arthritis and osteoarthritis . Ginger can also keep an arthritis flare-up at bay and minimize pain when it does occur.
Painful arthritis flare-ups can hinder daily activities. Although there is currently no cure for arthritis , the various natural medicines above can help ease swollen joints and minimize pain.
Sources include:
Efforts to Legalize Psychedelics is Quickly Picking Up Momentum

Denver, Oakland, and Santa Cruz voted to decriminalize mushrooms. Washington, D.C. just took a major step toward adding legalization to the Nov. 2020 ballot. Chicago city leaders passed a resolution supporting scientific and medicinal research, with a goal of decriminalization. Vermont lawmakers filed a bill to decriminalize it, as well. Even Oregon is pushing to legalize psilocybin mushrooms for therapeutic purposes.
All thanks to reports that show psychedelics have therapeutic benefits. For example, researchers at New York University found psilocybin mushrooms caused a “rapid and sustained” reduction in anxiety and depression in patients with cancer, as reported by the Financial Post. Researchers from the University of California David found that micro-dosing with psychedelic drugs for a prolonged period of time showed promise. “Our study demonstrates that psychedelics can produce beneficial behavioral effects without drastically altering perception, which is a critical step towards producing viable medicines inspired by these compounds,” said David Olson of UC Davis, as quoted by Esquire.
A report titled Psychedelic-Assisted Psychotherapy: A Paradigm Shift in Psychiatric Research and Development found that such treatments have ““positive long-term mental health consequences, rather than daily neurochemical corrections in brain dysfunctions,” meaning they may help treat conditions better than pharmaceuticals, as noted by Leafly.
Some of the issues that psychedelics may be able to assist with include substance dependency, PTSD, depression, anxiety, obsessive compulsive disorder, and chronic pain. There’s so much interest, COMPASS Pathways just raised $80 million to push its psilocybin therapy into Phase 3 development to help folks with treatment-resistant depression. The company received FDA Breakthrough Therapy designation for its program of psilocybin therapy in treatment-resistant depression in 2018, as highlighted in a recent press release. As the growth story unfolds, some of the companies to keep an eye on include The Yield Growth Corp. (CSE:BOSS)(OTC:BOSQF), GW Pharmaceuticals (NASDAQ:GWPH), Champignon Brands Inc. (OTC:SHRMF)(CSE:SHRM), Mind Medicine Inc. (OTC:MMEDF) , and Johnson & Johnson (NYSE:JNJ).
The Yield Growth Corp. (CSE:BOSS)(OTCQB:BOSQF) BREAKING NEWS : The Yield Growth Corp. announced it has changed the name of its majority owned subsidiary to NeonMind Biosciences Inc. from Flourish Mushroom Labs Inc., a company engaged in research and development of potentially therapeutic uses of psychedelic mushrooms and development of functional mushroom products.
NeonMind was inspired by the potential therapeutic effects of psychedelic mushrooms, which have been shown to increase sensory processing and brain connectivity characterized by increased synchronization of sensory brain regions, as found in a recent study called “Psilocybin induces time-dependent changes in global functional connectivity”, according to psypost.org.
The NeonMind name is meant to reflect that connectedness, by bringing together “Neon,” representing brilliance, brightness, and radiance with “Mind,” as our intellect, consciousness, power and soul.
NeonMind has filed a U.S. provisional patent application to protect intellectual property relating to the use of psychedelic mushrooms to activate the mind to achieve better body health, including:
– losing weight;
– reducing food cravings;
– counteracting compulsive overeating;
– improving quality of diet by empowering the mind to select lower calorie foods;
– increasing metabolism;
– treating diabetes;
– regulating blood glucose; and
– reducing susceptibility to cardiovascular disease, high blood pressure, diabetes mellitus and other illnesses associated with obesity
The company is developing plans for clinical trials to further its research into potentially therapeutic benefits of compounds found in psychedelic mushrooms.
The company also intends to launch functional mushroom based products under the NeonMind brand, and has designed initial packaging concepts and filed trademark applications for NeonMind in Canada and the U.S. It aims to be a leader in the fast-growing functional foods market by offering high-quality mushroom-infused products that support immune, cognitive, memory and other brain functions.
Other related developments from around the markets include:
GW Pharmaceuticals (NASDAQ:GWPH), a biopharmaceutical company focused on discovering, developing and commercializing novel therapeutics from its proprietary cannabinoid product platform, will announce on May 11th, 2020 its financial results for the first quarter ending March 31st, 2020. GW will also host a conference call the same day at 4:30 p.m. ET. Conference call information will be provided in the financial results press release. A replay of the call will also be available through the Company’s website.
Champignon Brands Inc. (OTC:SHRMF)(CSE:SHRM) announced its placement in an editorial published by NetworkNewsWire. “The expansion of the functional food and drinks sector has created a new opportunity. While cannabis and CBD have taken these consumables beyond the traditional active ingredients of alcohol and caffeine, this diversification of the market has opened up consumers to new possibilities. Among those possibilities is the use of natural ingredients found in mushrooms.”
Mind Medicine Inc. (OTC:MMEDF) in collaboration with University Hospital Basel’s Liechti Laboratory , has discovered and filed a patent application in the United States (preserving all worldwide rights) for a neutralizer technology intended to shorten and stop the effects of an LSD trip during a therapy session. This discovery, when further developed, may act as the ‘off-switch’ to an LSD trip. MindMed is the leading psychedelic pharmaceutical company and the Liechti Laboratory is the leading research center focused on the pharmacology of psychedelic substances. This is the latest discovery based on surprising experimental results from work and collaboration conducted at the lab. The invention may help reduce the acute effects of a psychedelic drug and help shorten the hallucinogenic effects when required by a patient or medical professional. One of the many fears and stigmas associated with psychedelics are rare occurrences of ‘bad trips.’ MindMed is seeking to equip therapists and other medical professionals with the resources and technology to better control the effects of dosing LSD in a clinical setting to improve the patient experience and patient outcomes. This advancement paves the way for greater therapeutic applications of LSD and shorter-acting psychedelic therapy treatments. MindMed believes this technology, when further developed, may one day be marketed as an added feature to shorten a therapy session and stop a session if the patient is not comfortable.
Johnson & Johnson (NYSE:JNJ) announced that U.S. District Judge Freda L. Wolfson , chief judge of the District of New Jersey, who is […]
Why Your Immune System Declines as You Age — and 5 Things to Do About It

Every cold and flu season, and especially now during the novel coronavirus outbreak , we’re reminded that older adults tend to be hit harder by viral infections and other illnesses. That’s mostly because, as we age, our immune systems start to weaken. Cooking more regularly at home and staying active are two ways to help slow immunosenescence. This gradual decline in immunity, known as immunosenescence, is one reason why older adults are at increased risk of health issues — from chronic diseases (such as heart disease and cancer) to dangerous complications (such as pneumonia) from illnesses like COVID-19. Immunosenescence even makes protective vaccinations, like the flu shot , less effective in older people, according to Harvard Health Publishing .
And while scientists agree that part of this process is natural and inevitable, studies suggest that there is also a lot that older adults can do to preserve and strengthen their immune systems.
Here’s what’s happening with the body’s natural defenses over time, and how we can protect ourselves well into our golden years.
Some of the most obvious signs of aging are physical: As we get older, we develop wrinkles as our skin loses its elasticity and we go gray as our hair loses its pigment. Some signs are mental: Memory loss becomes more common and some people develop degenerative brain diseases like dementia.
At the same time, something similar but less obvious is happening to the body’s aging immune system.
“It’s the same with every organ in the body,” says Nir Barzilai, MD , director of the Institute for Aging Research at the Albert Einstein College of Medicine. “Things begin to break down, and the body can’t repair it as quickly and completely as it once could.”
To a certain extent, that’s just a normal part of aging, says Jessica Lee, MD , assistant professor of geriatrics and palliative medicine at the University of Texas Health McGovern Medical School. “Unfortunately, the body just doesn’t produce immune cells the way it used to at a younger age,” she says.
B and T cells — two types of white blood cells that make antibodies to fight off outside pathogens — are produced less frequently in older adults, Lee says. “They’re also potentially of a lower quality,” she adds, “which makes it difficult for the body to mount an immune response when it’s attacked by something like a virus or bacteria.”
On top of that, levels of inflammation in the body tend to rise as we get older, as well — a phenomenon known as inflammaging, according to a July 2018 review in Nature Reviews Endocrinology .
“When we get an infection and we get a fever, that’s inflammation,” Barzilai says. “But if our inflammatory response is too high in these situations, it can be very dangerous.”
Yes, a decrease in immunity over the years is normal. “But I don’t want to sound like it’s all doom and gloom, and it’s just too bad if you’re old because there are ways you can boost your immunity to help offset that natural decline that comes with age,” Lee says. “Aging is a modifiable condition. It’s flexible — and if you can lower your biological age, you’re going to be better protected against viruses and other threats.” Barzilai agrees, adding that there are really two types of aging: chronological, which keeps track of a person’s actual age, and biological, which takes into account how healthy people are compared with their peers.
“Aging is a modifiable condition,” says Barzilai. “It’s flexible — and if you can lower your biological age , you’re going to be better protected against viruses and other threats.”
Here are a few ways to do just that. Not only will these strategies help you feel younger, but they’ll do the same for your immune system as well.
1. Get Plenty of Vitamins and Minerals From Whole Foods
Eating a healthy diet rich in antioxidants, fiber and other important nutrients is one of the best ways to strengthen your immunity at any age, says Lee — but it’s especially important for older adults who are starting to lose those natural defenses.
“I recommend eating as many fruits and vegetables and whole foods as possible, and trying to avoid processed foods that are high in sugar and fat,” she says.
One nutrient older adults shouldn’t skimp on is zinc. Zinc deficiency is common in older adults, according to a 2012 review in Aging and Disease , and has been linked to impaired immune function and an increased risk of infection.
Shellfish, eggs, soy products, legumes and whole grains are all good sources of zinc . You can also get zinc from dairy sources such as milk, cheese and low-fat yogurt.
Or, you might consider taking a daily zinc supplement — but only do this under a doctor’s supervision, since too much zinc could also harm the immune system, per the Aging and Disease study.
Older adults might benefit from taking a vitamin D supplement, as well. The body depends on vitamin D to regulate the immune system, according to a December 2018 review in the Journal of Aging and Gerontology , and many older adults don’t get enough from sun exposure and diet alone.
Adults up to age 70 should get 600 IU of vitamin D daily and adults 70 and older get 800 IU a day, per the National Institutes of Health . Finding a type of workout you love and sticking to it can help support your immune system. 2. Exercise Regularly
A September 2013 literature review in the journal Maturitas notes that exercise has been shown to increase both the number and function of immune-system cells in older people, as well as reduce inflammation.
Only certain types of exercise have been studied in clinical trials. For example, a study in the March 2018 journal Aging Cell observed that older adults who cycled regularly had levels of T cells in their blood similar to young adults who weren’t involved in regular exercise.
And a 2012 study in the Journal of Sports Medicine & Doping Studies observed that a six-month […]
Can Zapping the Brain Boost Memory?

ABOVE: © HUMM
What if you could boost your brain’s processing capabilities simply by sticking electrodes onto your head and flipping a switch? Berkeley, California–based neurotechnology company Humm has developed a device that it claims serves that purpose. Their “ bioelectric memory patch ” is designed to enhance working memory—the type of short-term memory required to temporarily hold and process information—by noninvasively stimulating the brain.
In recent years, neurotechnology companies have unveiled direct-to-consumer (DTC) brain stimulation devices that promise a range of benefits, including enhancing athletic performance , increasing concentration , and reducing depression . Humm’s memory patch, which resembles a large, rectangular Band-Aid, is one such product. Users can stick the device to their forehead and toggle a switch to activate it. Electrodes within the patch generate transcranial alternating current stimulation (tACS), a method of noninvasively zapping the brain with oscillating waves of electricity. The company recommends 15 minutes of stimulation to give users up to “90 minutes of boosted learning” immediately after using the device. The product is set for public release in 2021.
Over the last year or so, Humm has generated much excitement among investors, consumers, and some members of the scientific community. In addition to raising several million dollars in venture capital funding , the company has drawn interest both from academic research labs and from the United States military. According to Humm cofounder and CEO Iain McIntyre , the US Air Force has ordered approximately 1,000 patches to use in a study at their training academy that is set to start later this year.
Despite the hype, however, some scientists say that the jury is still out on whether noninvasively stimulating the brain with electricity can have a meaningful effect on cognition. Unlike the more powerful method of transcranial magnetic stimulation, electrical stimulation doesn’t generate a clear sign that the stimulation is influencing the brain, such as an immediately observable muscle twitch.
Humm’s device builds on years of research suggesting that methods of transcranial electrical stimulation (tES)—including tACS and transcranial direct current stimulation (tDCS), which uses a constant rather than an alternating current—can boost memory, attention, and other cognitive processes by influencing natural rhythms in brain activity. In one of the most recent studies , for example, a pair of scientists at Boston University demonstrated that it was possible to reverse age-related working memory deficits in older adults by modulating brain rhythms with tACS. POWER STRIP: This electrode-containing patch could boost working memory, according to Humm, the California-based company that makes it. A few years ago, the Humm team decided to test the efficacy of their product in a randomized, placebo-controlled trial. After recruiting 36 healthy adults between 17 and 56 years old, they split the participants into two groups. One group was given tACS at 6 hertz ( previous studies suggested that brain rhythms important for cognitive tasks oscillate at this frequency) for 15 minutes and the other received a sham stimulation, where electricity was applied for a brief, 60-second period, then turned off for the rest of the session. All subjects engaged in the Corsi block-tapping test, a working-memory task that involves recalling the order in which a series of squares appeared on a screen, while they underwent tACS or sham stimulation, in addition to before and after. Participants were also asked to rate how likely the stimulation was to improve their performance, both prior to and following the experiment.
This study found that tACS-treated participants performed approximately 20 percent better than their sham-treated counterparts—and that expectations regarding their performance did not influence results. “I was surprised that they got such a large effect size,” says Ted Zanto , a University of California, San Francisco, neuroscientist and a scientific advisor to Humm who helped design the study. “In a lot of research labs using different devices, they oftentimes don’t see quite such a large effect.” The findings from the study, which was completed in 2018, are available in a white paper on the company’s website.
“It was a properly designed study . . . and what they found was a statistically significant difference between the two experimental groups,” says Anli Liu , a neurologist at NYU School of Medicine who isn’t involved with the company. “That being said, I think statistical significance doesn’t necessarily mean clinical significance.” Liu points out that the 20 percent difference in performance between the two groups was driven by members of the tACS group being able to recall six items, while the control group remembered only five. In addition, she adds that it remains to be seen if similar improvements can be seen with other working memory tasks. The company is accepting online registrations for early access to its patch. Other scientists share Liu’s skepticism. Because the company didn’t report whether or not their memory patch generated any changes in the brain, it is unclear whether it actually alters brain rhythms, says Joel Voss , a neuroscientist at Northwestern University who has no affiliation with the company. “It’s important if you want to validate a device to show that it’s actually engaging the hypothesized neural structure and changing its function in the way that you predicted.” Otherwise, Voss adds, the effects could be due to “extraneous, nonspecific influences,” such as placebo or indirect influences on the peripheral nervous system. For example, stimulating the nerves on your skin might make you alert, which may in turn make you more attentive to the task at hand.
On top of that, it remains unclear how much electricity actually enters the brain with tES, according to Voss. He adds that results from several studies indicate that not enough electricity gets into the brain with this technique to have a meaningful impact on function. For example, in one 2019 Nature Communications paper, a group of researchers reported that tACS stimulation could increase a tremor in individuals whose hands already shook and trigger it in healthy individuals asked to hold a tiny weight up with one finger. But this effect disappeared when they applied a topical anesthetic to the […]
Boosting the brain with physical activity

Apr 30, 2020 at 2:11 PM
Physical activity is well-known for its benefits related to weight control, reduced risk of cardiovascular disease, and elevated blood glucose levels. Increasing data is accumulating, however, about the effect it has on our brains.
For most people, concerns about brain health often do not surface until later in life as they begin to experience changes associated with the aging process. Brain health actually begins shortly after conception. Research indicates that a number of factors can affect brain size and activity, including exposure to physical activity.
The development of the brain and central nervous system appears to occur in stages, one building upon another. The process can be stimulated by physical activity. A woman who is physically active before and during pregnancy has the opportunity to affect better brain performance in her child.
Stimulation of the brain from physical activity is especially important during the years of growth and development. It helps to create new neurons and connections within the brain and nervous system.
The Physical Activity Guidelines Advisory Committee Scientific Report 2018 (from the U.S. Department of Health and Human Services) noted the connection between physical activity and better brain cognition. They noted benefits such as better processing speed, memory, and higher executive functions (reasoning, planning, organizing, problem-solving, etc.) with higher levels of physical activity.
The Guidelines establish recommendations for physical activity beginning at age three.
They suggest that 3-5 year olds be active throughout the day. The goal for 6-17 year olds is > 60 minutes of moderate to vigorous activity daily with vigorous activity occurring at least three times a week. They should also do activities that strengthen muscles and bones several times a week.
Adults should try for 150-300 minutes of moderate or 75-150 minutes of vigorous cardiovascular exercise each week. They should also do moderate to vigorous muscle strengthening exercises at least twice a week. Older adults and those with disabilities should stay as active as they can with cardio and strength activities based on their health status.
Unfortunately, only a small percentage of individuals in all age categories achieve these goals. For the adolescent period, for example, which is when the brain and nervous system are maturing, statistically only about 20% fulfill the physical activity recommendations.
In children and teens, studies indicate that higher levels of physical activity are associated with better test scores, greater learning, improved reading skills, and greater understanding. The subjects of math and reading have the strongest connection. More specifically, cardiovascular activity seems to help with attention, planning, working memory, and inhibitory control.
Ongoing studies are investigating the reasons for the connections between physical activity and better brain health and numerous possibilities exist. A key player appears to be something called “brain-derived neurotrophic factor” (BDNF) that is stimulated by physical activity. This substance is important for the survival, growth, and maintenance of neurons in circuits related to emotional and cognitive function.
BDNF can also improve brain plasticity (the ability to adapt to changing conditions) and can enhance the strength of neural networks related to learning and memory. The extent of the response by BDNF is based on the intensity, duration, frequency, and type of physical activity.
Stress can decrease the BDNF response, which can interfere with the creation of new brain cells and potentially impair learning, memory, and overall brain performance. The good news is that physical activity is a great stress-buster.
Increased heart rate can maximize blood flow (nutrients, oxygen) to brain tissues to allow for optimal performance. Physical activity can also counter the oxidative stress and inflammation caused by obesity, elevated blood glucose, and high blood lipids that can impede blood flow to the brain.
Related to quality of life, physical activity can reduce levels of anxiety and depression, while improving overall mood and emotional well-being. It can also increase the effectiveness of anti-depressant medications.
For middle-age and older adults, physical activity can delay brain aging, improve cognitive processes, can be analgesic for pain, and can improve mood. The natural course of aging decreases blood flow to the brain by about 5% a year. Physical activity can help to maximize the flow.
The Alzheimer’s Association suggests that physical activity can reduce the risk of both vascular dementia and Alzheimer’s disease. Persons with type 2 diabetes are at greater risk for Alzheimer’s as it can increase inflammatory and oxidative/metabolic changes that can lead to cognitive decline due to damage to neurological tissues. Persons with diabetes should establish a lifetime of physical activity as soon as they are diagnosed.
In persons with established brain-associated conditions such as Parkinson’s disease, multiple sclerosis, stroke, and dementia, physical activity can improve functioning. This means being able to sustain independence in activities of daily living and better quality of life for a longer period of time.
Brain health, then, is not just a concern for the older years of life. It is a life-long process that starts at the early stages of growth and development, progresses through childhood and adolescence, and continues through the adult years. Physical activity is a controllable factor that can enhance the brain and nervous system so that it is functioning optimally.
Pam Stuppy, MS, RD, CSSD, LD is a registered, licensed dietitian with nutrition counseling offices in York, ME and Portsmouth, NH. She has also been the nutritionist for Phillips Exeter Academy, presents workshops nationally, and is Board Certified as a Specialist in Sports Dietetics. (See www.pamstuppynutrition.com for more nutrition information, some healthy cooking tips, and recipe ideas).
