Nature Knows and Psionic Success
God provides
Waking Up Tired? Try This Natural Sleep Supplement

If melatonin makes you groggy, GABA could be a good alternative. Sleep is essential to all aspects of our well-being, from our mood and brain functions to our immune system , heart health and more. Despite how important a good night’s sleep is, many Americans struggle with insomnia . If you’ve tried nighttime yoga , journaling , melatonin and every other sleep remedy in the book, and you still can’t seem to knock out at night, there’s a supplement you might consider trying.
Enter gamma-aminobutyric acid or GABA. It’s an amino acid, naturally found in the body, that promotes a calming effect. GABA is often taken as a dietary supplement, but it has a track record showing that it may be a good sleep aid alternative to melatonin. It affects only the early sleep stages and leaves you feeling more awake in the morning as a result (some people say popular sleep supplements like melatonin make them groggy ). Although there’s limited research, small studies have yielded positive results showing that GABA may be worth a shot if you’re struggling to fall asleep .
Here’s what we know about GABA, tips on taking it and why it might be a viable sleep aid to consider.
For more help getting quality rest, try these seven natural sleep aids for insomnia , and here’s how to create the perfect environment for sleep .
Best Mattress of 2024 What is GABA?
GABA is a neurotransmitter naturally found in the brain and some foods like tomatoes and soybeans. It’s an inhibitory neurotransmitter that blocks chemical signals in the central nervous system and reduces brain activity. GABA can help promote calmness in the body and helps regulate nerve cell hyperactivity when feeling fearful, anxious or stressed.
It’s sold without a prescription as a dietary supplement, but GABA’s effects may also benefit those who struggle to fall asleep. Taking GABA for sleep
Taken alone or with other natural sleep aids, GABA supplements help address anxiety, stress and an overactive brain , three main offenders that make it difficult to fall asleep. Its calming effect puts the mind in a relaxed state, so you’re in the right headspace to drift off to sleep.
Low GABA levels have actually been linked to sleep deprivation, as one study found participants with insomnia had 30% lower levels of GABA in their systems. Another small-scale study by Frontiers in Neuroscience involving middle-aged adults found that taking 300 mg of GABA before bed for at least a week can reduce sleep latency (the amount of time it takes to fall asleep).
There’s no concrete evidence showing GABA helps sleep efficiency (quality of sleep and slow wave sleep), but the study’s results showed it may promote sleepiness as it affects early sleep stages. Another benefit is that it won’t leave you feeling drowsy the following morning like other over-the-counter medications such as ZzzQuil or prescription sleep medications. A rendering of the molecular structure of GABA. Tips for taking GABA to aid sleep
1. GABA can be taken as a supplement or powder in your food .
2. Take GABA 30 to 60 minutes before bed for the best results (as shown by studies).
3. Follow the dosage instructions and track the amount and how often you take GABA.
4. Use a sleep journal to document your sleep quality so you can identify patterns and possible side effects while tracking GABA’s effectiveness.
5. GABA is naturally found in fermented foods like kimchi, sourdough, sake and mulberry beer.
6 . Always talk to your doctor before taking GABA or any new supplements. Is it safe to take GABA every night?
According to the Sleep Foundation, there are no serious side effects when taking GABA in small doses from sleep or dietary supplements, although some consumers have reported feeling abdominal pain or headaches. High levels of GABA in the brain are linked to daytime drowsiness, and a small number of people report drowsiness after taking GABA.
People at a higher risk of having a negative reaction to GABA include: Pregnant people
People under 18 years old
Those who take prescriptions for high blood pressure
Those who take anti-seizure medications
Other benefits of GABA: stress and anxiety relief
While research is still limited, more data supporting GABA as a stress and anxiety reliever continues to emerge. Relieving anxiety and stress before bed isn’t to be taken lightly, as it can significantly impact sleep latency and overall sleep quality . One study from 2012 showed that after 30 minutes of taking GABA, it helped ease stress in participants.
Low levels of GABA can result in anxiety and depression and are prevalent in individuals with mental health conditions .
There’s a high dose of GABA in the supplement Chlorella as the neurotransmitter has been shown to lower blood pressure .
As you should with any new supplement, consult your doctor before taking GABA, especially when taken in combination with other medications or prescriptions.The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives. Mattress Buying Guides
Scientists say sleep resets brain connections—but only for first few hours
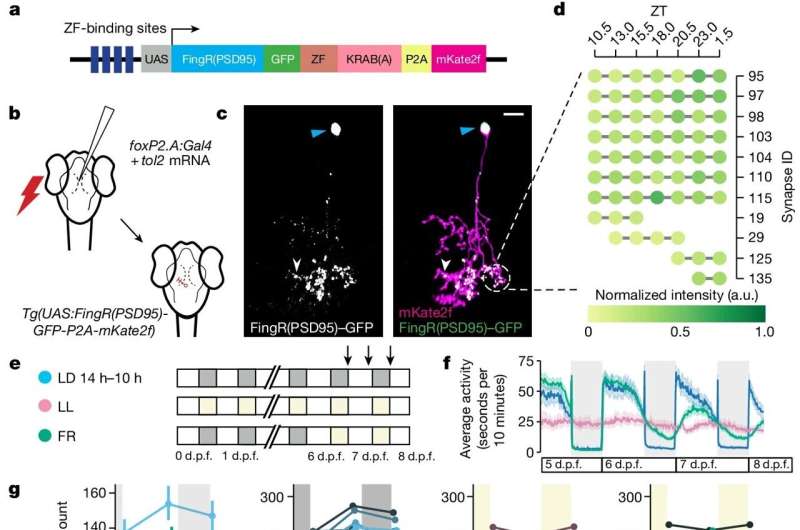
Single-neuron synapse tracking across day–night cycles reveals diverse dynamics. Credit: Nature (2024). DOI: 10.1038/s41586-024-07367-3 During sleep, the brain weakens the new connections between neurons that had been forged while awake—but only during the first half of a night’s sleep, according to a new study in fish by UCL scientists.
The researchers say their findings, published in Nature , provide insight into the role of sleep, but still leave an open question around what function the latter half of a night’s sleep serves.
The researchers say the study supports the Synaptic Homeostasis Hypothesis, a key theory on the purpose of sleep which proposes that sleeping acts as a reset for the brain.
Lead author Professor Jason Rihel (UCL Cell & Developmental Biology) said, “When we are awake, the connections between brain cells get stronger and more complex. If this activity were to continue unabated, it would be energetically unsustainable. Too many active connections between brain cells could prevent new connections from being made the following day.
“While the function of sleep remains mysterious, it may be serving as an ‘off-line’ period when those connections can be weakened across the brain, in preparation for us to learn new things the following day.”
For the study, the scientists used optically translucent zebrafish, with genes enabling synapses (structures that communicate between brain cells) to be easily imaged. The research team monitored the fish over several sleep-wake cycles .
The researchers found that brain cells gain more connections during waking hours, and then lose them during sleep. They found that this was dependent on how much sleep pressure (need for sleep) the animal had built up before being allowed to rest; if the scientists deprived the fish from sleeping for a few extra hours, the connections continued to increase until the animal was able to sleep.
Professor Rihel added, “If the patterns we observed hold true in humans, our findings suggest that this remodeling of synapses might be less effective during a mid-day nap, when sleep pressure is still low, rather than at night, when we really need the sleep.”
The researchers also found that these rearrangements of connections between neurons mostly happened in the first half of the animal’s nightly sleep. This mirrors the pattern of slow-wave activity, which is part of the sleep cycle that is strongest at the beginning of the night.
First author Dr. Anya Suppermpool (UCL Cell & Developmental Biology and UCL Ear Institute) said, “Our findings add weight to the theory that sleep serves to dampen connections within the brain, preparing for more learning and new connections again the next day. But our study doesn’t tell us anything about what happens in the second half of the night.
“There are other theories around sleep being a time for clearance of waste in the brain, or repair for damaged cells—perhaps other functions kick in for the second half of the night.”
Provided by University College London
Super-detailed map of brain cells that keep us awake could improve our understanding of consciousness
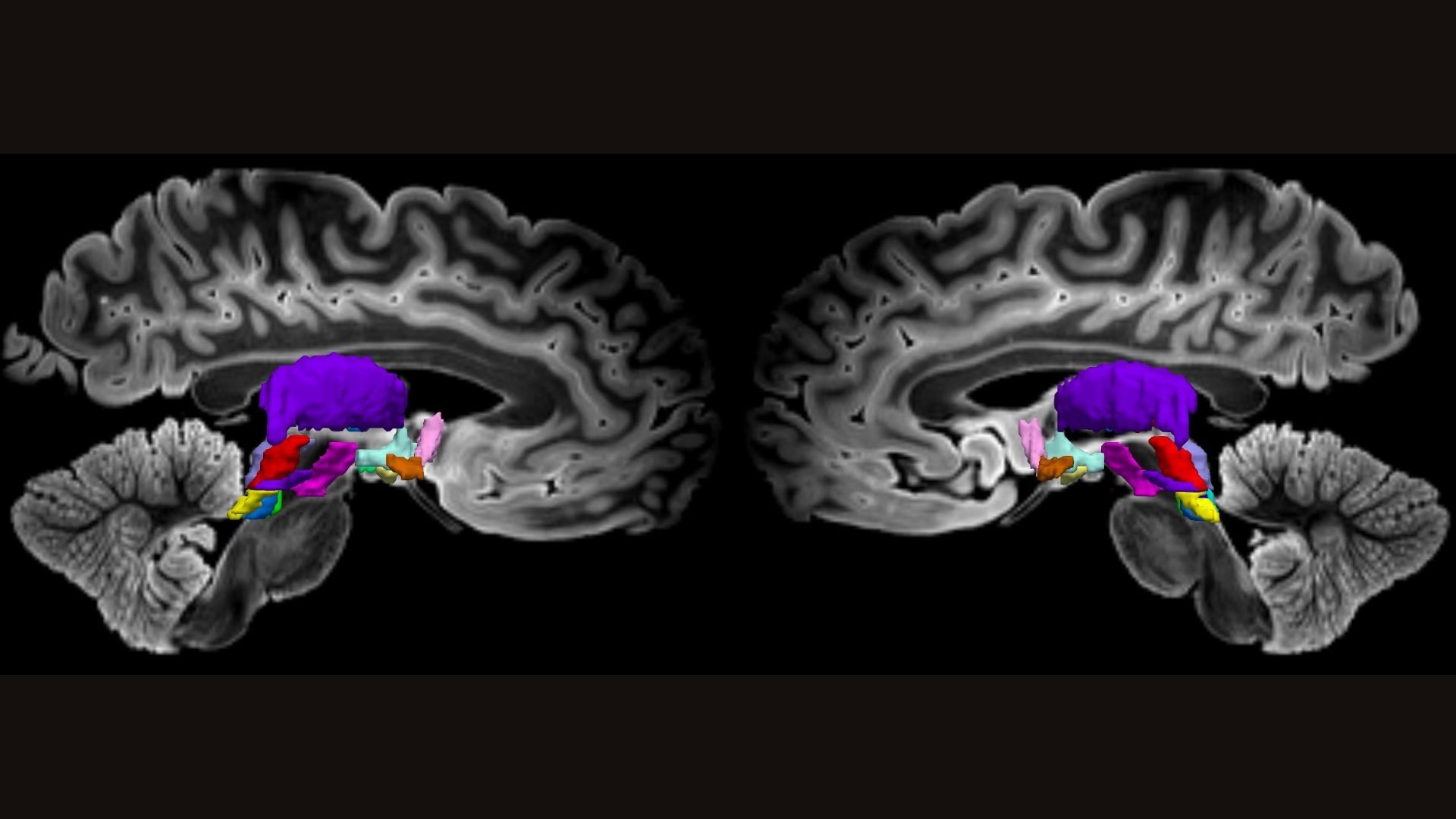
The major nodes of a human brain network that keeps us awake are shown color-coded in this MRI scan of a postmortem brain. (Image credit: Edlow et al., Sci. Trans. Med., 16 eadj4303 (2024). (Cropped by Live Science.))
Scientists have charted a comprehensive map of the brain cells responsible for keeping us awake. In doing so, they aim to better understand the mechanisms that enable human consciousness and to improve treatments for people in comas and vegetative states.
“It’s a beautiful study,” said Dr. Nicholas Schiff , a professor of neurology and neuroscience at Weill Cornell Medicine who was not involved in the new research. “It’s a map of everything.”
Schiff, who has collaborated with some of the study’s authors in the past, hopes the new map can serve as a template for scientists to go back and look at patients with altered states of consciousness. Such work could help clarify exactly how this wakefulness network can be disrupted and what’s required to get it back online. It’s a tool that could help scientists pinpoint which brain activity is “necessary and sufficient” to keep someone awake and aware, Schiff told Live Science.
The new study was published Wednesday (May 1) in the journal Science Translational Medicine .
Related: What happens in our brains when we ‘hear’ our own thoughts? Mapping consciousness
Human consciousness arises from a delicate dance between the wrinkled surface of the brain, known as the cerebral cortex, and deeper “subcortical” structures beneath it. Circuits in the cortex direct our attention and process information from the world around us, while the subcortical networks plug into these circuits from below, essentially keeping them active.
“It sends the signals that activate and stimulate the entire rest of the brain,” said first author Dr. Brian Edlow , co-director of Mass General Neuroscience and director of the Laboratory for NeuroImaging of Coma and Consciousness. Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Contact me with news and offers from other Future brandsReceive email from us on behalf of our trusted partners or sponsorsBy submitting your information you agree to the Terms & Conditions and Privacy Policy and are aged 16 or over.
Thus, consciousness is a “seamless interaction of these subcortical networks with these cortical networks,” Schiff said. “It’s an artifice, I think, to try to separate these things.”
But scientists’ understanding of humans’ subcortical networks is incomplete. It relies heavily on animal experiments, in which scientists can inject trackable chemicals into the brain and then remove the organ to get a good look at where they ended up. In living humans, these deep-seated networks are located near major arteries and air-filled sinuses, and they also move a bit with each breath, making standard brain scans less crisp and hard to decipher. By contrast, networks in the human cortex are easier to image and have been much better studied.
To help close this knowledge gap, the scientists behind the new study looked at brains from three middle-age organ donors. Using postmortem brains allowed the team to “map brain networks at ultrahigh resolution and to see connections that simply cannot be seen when you’re scanning a living human being,” Edlow told Live Science.
These organ donors had no neurological problems when they died, and their brains were carefully preserved in formaldehyde. The researchers stained the brains with colorful chemicals to mark different types of brain cells and then put the brains in an magnetic resonance imaging (MRI) scanner for up to 48 hours. These scans of postmortem brain tissue show many of the tracts in the network that sustains wakefulness in humans. This resulted in incredibly high-resolution maps of subcortical structures that had been tied to wakefulness in previous research. The team manually traced connections between the brain cells in these structures, taking into account the direction water would flow down their wires. This metric captured by MRI can help reveal how strongly different nodes in a network are linked.
This work revealed major nodes of the wakefulness network in several subcortical structures — the brainstem, hypothalamus and thalamus — as well as part of the cortex called the basal forebrain. This network was confirmed to be linked to a circuit involved in awareness. Known as the default mode network , it is very active when we’re daydreaming and not focused on a particular task.
Related: Ultrasound treatment ‘jump-started’ the brains of 2 people in coma-like state
To back up their work in postmortem brains, the team also looked at functional MRI data from more than 80 people who’d participated in the Human Connectome Project , a government-led effort to map all the networks in the human brain. These additional brain scans, which looked at the flow of oxygenated blood, pointed out a hub where these awareness and wakefulness networks meet: the ventral tegmental area.
RELATED STORIES
— Surges of activity in the dying human brain could hint at fleeting conscious experiences
— ‘Flow state’ uncovered: We finally know what happens in the brain when you’re ‘in the zone’
— A mysterious brain network may underlie many psychiatric disorders
Taken together, the postmortem brain scans provided maps of highways in the brain, while the live scans showed traffic patterns along those roads. “We view our findings as an initial map that is beyond the spatial resolution that has been achieved previously,” Edlow said. Looking to the future, the researchers hope to improve upon the map’s resolution even more.
At this point, it’s unclear exactly how the new map could shape the treatment of patients in comas, vegetative or minimally conscious states, Schiff noted. But it should be a useful tool to better understand and treat these conditions, he added.
“We envision that these connectivity maps will allow us to piece together, one individual at a time, the combination of connections that are necessary and sufficient to recover consciousness,” Edlow said.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun ? Send us your questions […]
Scientists identify new brain circuit in mice that controls body’s inflammatory reactions
The brain can direct the immune system to an unexpected degree, capable of detecting, ramping up and tamping down inflammation, shows a new study in mice from researchers at Columbia’s Zuckerman Institute.
“The brain is the center of our thoughts, emotions, memories and feelings,” said Hao Jin, PhD, a co-first author of the study published online today in Nature . “Thanks to great advances in circuit tracking and single-cell technology, we now know the brain does far more than that. It is monitoring the function of every system in the body.”
Future research could identify drugs that can target this newfound brain circuit to help treat a vast range of disorders and diseases in which the immune system goes haywire.
“This new discovery could provide an exciting therapeutic venue to control inflammation and immunity,” said Charles S. Zuker, PhD, the study’s senior author, a principal investigator at Columbia’s Zuckerman Institute and a Howard Hughes Medical Institute investigator.
Recent work from the Zuker lab and other groups is revealing the importance of the body-brain axis, a vital pathway that conveys data between the organs and the brain. For example, Dr. Zuker and his colleagues discovered that sugar and fat entering the gut use the body-brain axis to drive the craving and strong appetite for sugary and fatty foods.
“We found all these ways in which the body is informing the brain about the body’s current state,” said co-first author Mengtong Li, PhD, a postdoctoral researcher in the Zuker lab. “We wanted to understand how much farther the brain’s knowledge and control of the body’s biology went.”
The scientists looked for connections the brain might have with inflammation and innate immunity, the defense system shared by all animals and the most ancient component of the immune system. Whereas the adaptive immune system remembers previous encounters with intruders to help it resist them if they invade again, the innate immune system attacks anything with common traits of germs. The relative simplicity of innate immunity lets it respond to new insults more quickly than adaptive immunity.
Prior studies in humans revealed that electrically stimulating the vagus nerve — a bundle of thousands of nerve fibers linking the brain and the body’s internal organs — could reduce the response linked to a specific inflammatory molecule. However, much remained unknown about the nature of this body-brain system: for instance, the generality of the brain’s modulation of immunity and the inflammatory response, the selective lines of communication between the body and the brain, the logic of the underlying neural circuit, and the identity of the vagal and brain components that monitor and regulate inflammation.
The Zuker lab turned to a bacterial compound that sets off innate immune responses. The scientists found that giving this molecule to mice activated the caudal nucleus of the solitary tract, or cNST, which is tucked inside the brainstem. The cNST plays a major role in the body-brain axis and is the primary target of the vagus nerve.
The scientists showed that chemically suppressing the cNST resulted in an out-of-control inflammatory response to the immune insult: levels of pro-inflammatory molecules released by the immune system were more than three times higher than usual, and levels of anti-inflammatory immune compounds were roughly three times lower than normal. In contrast, artificially activating the cNST reduced pro-inflammatory molecule levels by nearly 70 percent and increased anti-inflammatory chemical levels almost tenfold.
“Similar to a thermostat, this newfound brain circuit helps increase or decrease inflammatory responses to keep the body responding in a healthy manner,” said Dr. Jin, who started this study as a postdoctoral researcher in Dr. Zuker’s lab. Dr. Jin is now a tenure track investigator at the National Institute of Allergy and Infectious Diseases. “In retrospect, it makes sense to have a master arbiter controlling this vital response.”
Previous vagus nerve stimulation research in humans suggests the findings go beyond mice. The new research may also be in line with thousands of years of thought on the potential importance of the mind on the body.
“A lot of psychosomatic effects could actually be linked to brain circuits telling your body something,” Dr. Jin noted.
The scientists identified the specific groups of neurons in the vagus nerve and in the cNST that help detect and control pro- and anti-inflammatory activity. “This opens up a new window into how the brain monitors and modulates body physiology,” said Dr. Zuker, a professor of biochemistry, molecular biophysics and neuroscience at Columbia’s Vagelos College of Physicians and Surgeons.
Discovering ways to control this newfound brain circuit may lead to novel therapies for common auto-immune diseases such as rheumatoid arthritis, type I diabetes, multiple sclerosis, neurodegenerative diseases, lupus, inflammatory bowel disease and Crohn’s disease, as well as conditions such as long COVID syndrome, immune rejection of transplanted organs, and the potentially deadly outbursts known as cytokine storms that COVID infections can trigger.
Autoimmune diseases may affect roughly one in 10 individuals, a 2023 Lancet study suggested. In the United States alone, autoimmune diseases may cost the economy $100 billion annually, a figure that may be a gross underestimate, according to the Autoimmune Association.
Harnessing the activity of this circuit may make a difference across a broad range of conditions affecting the immune system, and help treat dysregulated inflammatory states in people suffering from immune diseases and disorders, Drs. Jin and Li said.
Sleep resets brain connections — but only for first few hours
During sleep, the brain weakens the new connections between neurons that had been forged while awake — but only during the first half of a night’s sleep, according to a new study in fish by UCL scientists.
The researchers say their findings, published in Nature , provide insight into the role of sleep, but still leave an open question around what function the latter half of a night’s sleep serves.
The researchers say the study supports the Synaptic Homeostasis Hypothesis, a key theory on the purpose of sleep which proposes that sleeping acts as a reset for the brain.
Lead author Professor Jason Rihel (UCL Cell & Developmental Biology) said: “When we are awake, the connections between brain cells get stronger and more complex. If this activity were to continue unabated, it would be energetically unsustainable. Too many active connections between brain cells could prevent new connections from being made the following day.
“While the function of sleep remains mysterious, it may be serving as an ‘off-line’ period when those connections can be weakened across the brain, in preparation for us to learn new things the following day.”
For the study, the scientists used optically translucent zebrafish, with genes enabling synapses (structures that communicate between brain cells) to be easily imaged. The research team monitored the fish over several sleep-wake cycles.
The researchers found that brain cells gain more connections during waking hours, and then lose them during sleep. They found that this was dependent on how much sleep pressure (need for sleep) the animal had built up before being allowed to rest; if the scientists deprived the fish from sleeping for a few extra hours, the connections continued to increase until the animal was able to sleep.
Professor Rihel added: “If the patterns we observed hold true in humans, our findings suggest that this remodelling of synapses might be less effective during a mid-day nap, when sleep pressure is still low, rather than at night, when we really need the sleep.”
The researchers also found that these rearrangements of connections between neurons mostly happened in the first half of the animal’s nightly sleep. This mirrors the pattern of slow-wave activity, which is part of the sleep cycle that is strongest at the beginning of the night.
First author Dr Anya Suppermpool (UCL Cell & Developmental Biology and UCL Ear Institute) said: “Our findings add weight to the theory that sleep serves to dampen connections within the brain, preparing for more learning and new connections again the next day. But our study doesn’t tell us anything about what happens in the second half of the night. There are other theories around sleep being a time for clearance of waste in the brain, or repair for damaged cells — perhaps other functions kick in for the second half of the night.”
Neuroscientists Reveal Secret of Superagers’ Excellent Memories

People who still have very sharp memory into old age—known as “superagers”—may get their impressive powers from certain areas of the brain being preserved.
Brain structures known as white matter usually decline in integrity with age, but in superagers, white matter remains structurally sound, according to a new paper in the Journal of Neuroscience .
This may be the reason for superagers having the memory powers of people 30 years their junior, the researchers suggest.
The brain is made up of gray matter and white matter, with gray matter being found on the brain’s surface and white matter making up much of the deeper layers of the brain. Stock images show an older woman looking out of a window, main image, and a brain, inset. White matter in the brain may be the reason that some old people are “superagers.” White matter is made up largely of nerve fibers that are covered in a fatty substance called myelin, which helps to increase the speed and efficiency of electrical communication between neurons. The primary function of white matter is to connect different gray matter brain regions and transmit nerve signals quickly across the nervous system.
Newsletter
The Bulletin
Your Morning Starts Here
Begin your day with a curated outlook of top news around the world and why it matters.
I want to receive special offers and promotions from Newsweek
By clicking on SIGN ME UP, you agree to Newsweek’s Terms of Use & Privacy Policy . You may unsubscribe at any time.
White matter is essential for the coordination of various brain functions, from motor control to learning. Damage to the white matter can affect how the brain processes information and communicates with the rest of the body.
In the paper researchers from Spain’s Universidad Politécnica de Madrid and the Queen Sofia Foundation Alzheimer Centre studied the brain structure of older adults experiencing memory loss and those of superagers across a five-year period.
They discovered that superagers had better white matter microstructure than older people with declining memory.
“We studied the white matter structure of a large sample of 64 superagers over the age of 80 and 55 age-matched typical older adults during 5 years with yearly follow-ups showing evidence of slower age-related changes in the brains of superagers especially in protracted maturation tracts, indicating resistance to age related changes,” the researchers wrote in the paper.
Therefore, superagers may have white matter that is somehow resistant to being degraded with time, which helps them maintain their memory later in life.
“The better preservation of white matter microstructure in superagers relative to typical older adults supports resistance to age-related brain structural changes as a mechanism underpinning the remarkable memory capacity of superagers,” the researchers said.
They hope that these results may help scientists figure out if white matter can be protected to stem the tide of age-related memory loss and dementia.
“Understanding the superager phenotype can provide insights into mechanisms of protection against age-related memory loss and dementia ,” the researchers said.
Do you have a tip on a science story that Newsweek should be covering? Do you have a question about superagers? Let us know via science@newsweek.com.
Stem cells improve memory, reduce inflammation in Alzheimer’s mouse brains
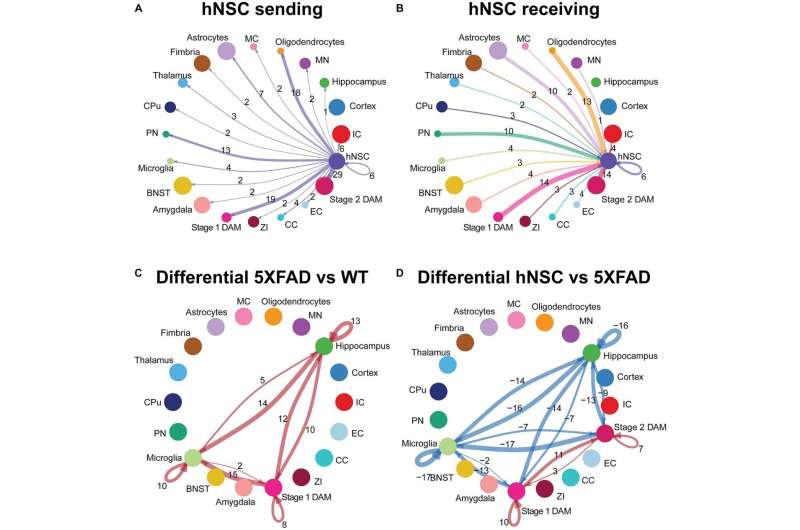
hNSC transplantation alters microglial cell signaling in the brain of 5XFAD mice after 34 weeks. Circle plots of ligand-receptor pair interactions between cell types with hNSCs as (A) sender and (B) receiver in the brain of hNSC injected 5XFAD mice. Circle plots of differential ligand-receptor pair interactions across cell types in (C) wild-type (WT) versus untreated 5XFAD and (D) hNSC injected versus untreated 5XFAD brain. Credit: Frontiers in Aging Neuroscience (2023). DOI: 10.3389/fnagi.2023.1306004 When people think of Alzheimer’s Disease and possible treatment, amyloid—and the accumulation of plaques that invade the cerebral cortex—is often brought up first. However, scientists are finding that Alzheimer’s is influenced by many factors, including neuroinflammation and disrupted metabolism.
By transplanting human neural stem cells, researchers led by Michigan Medicine improved memory and reduced neuroinflammation in a mouse model of Alzheimer’s Disease, suggesting another avenue for potential treatment. Their results are published in Frontiers in Aging Neuroscience .
“The beneficial effects of transplanting human neural stem cells within the brains of Alzheimer’s Disease mice occurred despite amyloid plaque levels remaining unchanged, which lends further evidence that strategies targeting neuroinflammation may be a promising therapeutic strategy, independent of amyloid plaques ,” said lead author Kevin Chen, M.D., clinical assistant professor of neurosurgery and neurology at Michigan Medicine.
“Additionally, the treatment was associated with normalized inflammation in the microglia, which are the innate immune cells of the brain that become activated with Alzheimer’s Disease. As the disease progresses, microglia and their inflammatory signaling is thought to contribute to neuron loss.”
A team at Michigan Medicine’s NeuroNetwork for Emerging Therapies transplanted neural stem cells into the memory centers of transgenic mice that expressed mutations associated with familial Alzheimer’s Disease. They had both the test mice and control mice perform a task called the Morris water maze to assess spatial memory and learning eight weeks after transplant.
Investigators found that Alzheimer’s disease mice transplanted with stem cells had their learning curves restored to resemble the control mice with normal learning and memory.
Additional testing through spatial transcriptomics—a method to measure gene expression in areas across the brain—revealed more than 1,000 differently expressed genes that were normalized in the memory centers of the Alzheimer’s Disease mice after transplantation.
In analyzing the gene expression changes specifically in microglia, the genetic markers linked to progression of Alzheimer’s Disease were also restored to levels close to control mice. This suggested a reduction in neuroinflammation and disease progression.
Researchers say the improvements reported after stem cell transplantation must be further studied in mice before advancing to larger animals and, eventually, humans.
“Our research is incredibly important and continues to support the promise of stem cell therapies in neurodegenerative diseases,” said senior author Eva Feldman, M.D., Ph.D., director of the ALS Center of Excellence at U-M and James W. Albers Distinguished University Professor at U-M.
“These preclinical studies are the required first step on the road to stem cell therapies.”
More information: Kevin S. Chen et al, Human neural stem cells restore spatial memory in a transgenic Alzheimer’s disease mouse model by an immunomodulating mechanism, Frontiers in Aging Neuroscience (2023). DOI: 10.3389/fnagi.2023.1306004
Provided by University of Michigan
New study reveals microplastic chemicals can enter the human body through sweat
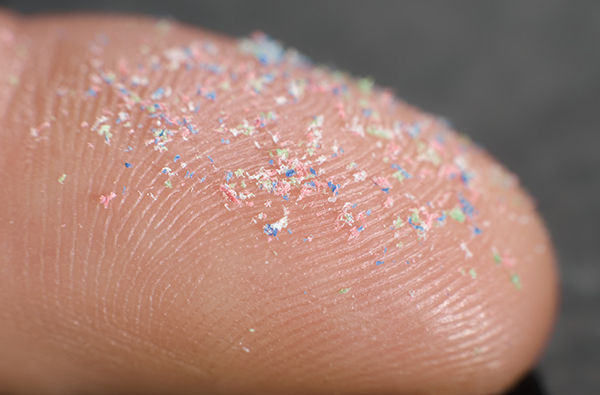
A recent study conducted at the University of Birmingham in the United Kingdom has found that chemical additives within microplastics can infiltrate the human body through sweat .
Microplastics, tiny particles measuring a millionth of a gram, are present in virtually everything humans consume – from bottled water to meat and plant-based food. These tiny particles can enter the body through food consumption that has made contact with plastic food packaging and through contact with everyday products that contain or are made of plastic.
A new study also suggests that it can enter the body through sweat. The study, published in Environment International, focused on polybrominated diphenyl ethers (PBDEs), commonly used as flame retardants in various plastic products, including furniture foam padding, wire insulation and cabinets for electronics. The researchers, led by Ovokeroye Abafe, a chemistry expert, used 3D human skin models and exposed them to microplastics containing PBDEs.
Abafe and his team found that skin could absorb up to eight percent of PBDEs, with higher levels absorbed from sweatier skin.
“Microplastics are everywhere in the environment, and yet we still know relatively little about the health problems that they can cause,” said Abafe in a press release. “Our research shows that [microplastics] play a role as ‘carriers’ of harmful chemicals, which can get into our bloodstream through the skin.”
The Environmental Protection Agency claims that PBDEs have yet to be classified as carcinogens, substances capable of causing cancer. However, enough evidence also shows that these chemicals have the potential to be carcinogenic.
Human knowledge is under attack! Governments and powerful corporations are using censorship to wipe out humanity’s knowledge base about nutrition, herbs, self-reliance, natural immunity, food production, preparedness and much more. We are preserving human knowledge using AI technology while building the infrastructure of human freedom. Speak freely without censorship at the new decentralized, blockchain-power Brighteon.io . Explore our free, downloadable generative AI tools at Brighteon.AI . Support our efforts to build the infrastructure of human freedom by shopping at HealthRangerStore.com , featuring lab-tested, certified organic, non-GMO foods and nutritional solutions.
“These chemicals are persistent, so with continuous or regular exposure to them, there will be a gradual accumulation to the point where they start to cause harm,” Abafe said. Studies reveal microplastics can accumulate in the brain and other internal organs
The Centers for Disease Control and Prevention claims that the health effects of PBDEs on humans are not well known yet.
But then, animal studies suggest that PBDEs can cause significant harm to thyroid, liver, and brain development, as well as potential carcinogenic risk. Human studies have associated PBDE exposure in children with cognitive and motor impairments and behavioral issues.
A study, conducted by Jaime Ross, a professor from the University of Rhode Island , analyzed the neurobehavioral effects of, and inflammatory response to, microplastic exposure, as well as the accumulation of microplastics in tissues , including the brain.
The study, which exposed young and elderly mice to varying concentrations of microplastics through their drinking water for three weeks, found that exposure to microplastics led to shifts in behavior and immune markers within the liver and brain tissues. The researchers observed altered movement and behaviors in the mice, reminiscent of symptoms associated with dementia in humans, following microplastic exposure. Additionally, Ross noted that even at relatively low doses, microplastic exposure induced considerable changes within a brief timeframe.
To understand the physiological mechanisms observed in behavioral shifts in mice, the researchers analyzed the extent of microplastic exposure in various major tissues, including the brain, gastrointestinal tract, heart, kidney, liver, lungs and spleen. (Related: MICROPLASTIC INVASION: Researchers find microplastics in human heart tissue .)
Surprisingly, the investigation revealed widespread bioaccumulation of particles in every examined organ, including the brain and even in bodily waste. Given that the microplastics entered the animals’ bodies via drinking water, the researchers anticipated finding them in the gastrointestinal tract, liver and kidneys.
Ross noted that the presence of microplastics in the heart and lungs shows that they spread beyond the digestive system and potentially undergo systemic circulation. This is dangerous because the blood-brain barrier, “a protective mechanism against viruses and bacteria,” is supposed to be “difficult to permeate.” The particles were found deep in the brain tissue. Brain infiltration by microplastics may cause a decrease in glial fibrillary acidic protein (GFAP), which supports many cell processes in the brain.
The researchers warned that a decrease in GFAP is linked to the early stages of certain neurodegenerative diseases, such as Alzheimer’s and depression.
Visit Microplastics.news for more stories about the prevalence of microplastics and their effects on human health.
Watch this video about the discovery of microplastics inside the human body .
This video is from the Daily Videos channel on Brighteon.com . More related stories:
Study: Microplastics accumulate in the brain and cause behavioral changes associated with dementia .
STUDY: Researchers found microplastics in all human placenta they tested .
Avoid toxic contaminants like microplastics in salt by switching to Pink Himalayan Salt .
Study finds MICROPLASTICS in almost 90% of protein sources, including plant-based ones .
Bottled water found to contain alarming levels of plastic particles, microplastics .
Sources include:
TheEpochTimes.com ScienceDaily.com Brighteon.com Take Action:Support Natural News by linking to this article from your website.Permalink to this article:CopyEmbed article link:CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
Definitive Therapy to the Primary Site Improves Survival in Brain-Only Metastatic NSCLC
0 TOPLINE:
In patients with non–small cell lung cancer (NSCLC) who have metastases to the brain only, definitive treatment to the primary site improved overall survival outcomes following stereotactic radiosurgery, a retrospective analysis found. METHODOLOGY:
The American Society of Radiation Oncology guidelines strongly recommend stereotactic radiosurgery in patients with NSCLC who have up to four brain metastases and conditionally recommend this option in patients with up to 10 brain metastases. Studies have shown that definitive treatment to the primary site after whole-brain radiotherapy can improve survival outcomes in patients with brain-only metastases, but there are limited data on the potential benefits of definitive treatment after stereotactic radiosurgery in this patient population.
To address this gap, the researchers compared outcomes among 53 patients with NSCLC and brain-only metastases who received definitive treatment to the primary site and 50 patients who did not.
Most patients received upfront definitive treatment (73.6%), while about one in four (26.4%) had their definitive treatment delayed about 9 months following their diagnosis. Overall, 42 patients received fractionated radiotherapy, eight received stereotactic body radiotherapy, and three patients had a lobectomy as definitive treatment.
More patients who had definitive treatment also received immunotherapy (53% vs 38%, respectively), and fewer got targeted therapy (8% vs 18%, respectively); however, the differences were not statistically significant.
The study outcomes included various progression-free survival (PFS) outcomes (local, regional, distant body, and intracranial) as well as cancer-specific and overall survival.
TAKEAWAY:
At 5 years, definitive treatment was associated with significantly better overall survival (40.2% vs 0%) and cancer-specific survival (67.6% vs 0%).
At 5 years, about one third of patients who received definitive primary treatment remained progression-free — locally (34.5%), regionally (33%), and via distant body (34%) — compared with no patients without definitive treatment. About 15% of patients receiving definitive treatment had intracranial PFS at 5 years.
The main predictors of worse overall survival were lack of definitive primary treatment (hazard ratio [HR], 2.40; P = .012), more advanced disease stage (HR, 2.73), and lack of immunotherapy (HR, 2.86).
IN PRACTICE:
“We found that in the modern era, definitive primary site treatment for patients with brain-only metastatic NSCLC undergoing intracranial [stereotactic radiosurgery] was associated with an improvement in local, regional, and distant body control, as well as cancer-specific survival and overall survival,” the authors concluded. “Definitive primary site treatment should be carefully considered in this patient population.” SOURCE:
The study, led by Kamran Salari from Corewell Health East William Beaumont University Hospital, Royal Oak, Michigan, was published online this month in Radiotherapy and Oncology . LIMITATIONS:
The retrospective design introduced potential biases, and the rationale behind treatment decisions was not documented. Variability in practice patterns and heterogeneity between treatment modalities may have influenced outcomes. DISCLOSURES:
The authors declared no conflicts of interest.
New studies examine the effects of napping on infant and preschooler brain development

A University of Massachusetts Amherst sleep scientist, funded with $6.7 million in grants from the National Institutes of Health (NIH), has launched two unprecedented studies that will track over time the brain development of infants and preschoolers to confirm the role of napping in early life and to identify the bioregulatory mechanisms involved.
Rebecca Spencer, a professor of psychological and brain sciences who is well-known for her groundbreaking research into napping, is testing her theories about what’s happening in the hippocampus–the short-term memory area of the brain–as babies and young children undergo nap transitions.
This new research is expected to become the gold standard of scientific evidence that emphasizes the importance of healthy sleep for young children as their brains develop. The findings will help inform nap policies for preschool and pre-kindergarten and be useful to teachers and parents of both neurotypical and neurodiverse children.
“The work we’ve been doing has always pointed to this interaction of sleep and brain development,” says Spencer, who carries out research in her Somneurolab at UMass Amherst. “We think that kids get ready to transition out of naps when the brain is big enough to hold all the information of the day until night-time sleep.”
The study involving preschoolers is a collaboration between Spencer at UMass Amherst; Tracy Riggins, a developmental psychologist specializing in memory development at the University of Maryland; and Gregory Hancock, a UMD professor of human development and quantitative methodology. Previous research by Spencer and Riggins showed differences in the hippocampus of kids who nap compared to those who have transitioned out of naps.
“So far, we’ve used cross-sectional approaches,” says Spencer, referring to research that analyzes data at one point in time, as opposed to longitudinal studies that involve repeated observation over time. “We really need to show longitudinally within a child that the point when they transition out of naps is predicted by a transition in the development of their hippocampus.”
The hippocampus is the short-term location for memories before they move to the cortex for long-term storage. Naps allow children with an immature hippocampus to process memories. Young children give up their afternoon nap, not based on their age, but their brain development, Spencer hypothesizes. Naps are beneficial to everybody. Naps protect memory for everybody, no matter what age. Kids who are habitual nappers really need the nap. If they don’t nap, they get catastrophic forgetting. That’s the difference between habitual and non-habitual nappers – not how good is the nap, but how bad is staying awake.” Rebecca Spencer, professor of psychological and brain sciences, UMass Amherst Adds Riggins, “In the end, being able to tell parents that those little deviations from routine that keep their children from napping might not have these huge implications for a neurotypical child in the long run would be great. And, the more we know about how the brain works in a typically developing child during this nap transition, the more we will be able to know about where we could possibly intervene to help neurodiverse children–like children with autism and ADHD, whose sleep patterns tend to be disrupted–since we will have some sort of scientific basis.”
The research team is recruiting 180 children, ages 3 to 5 years. The researchers will track their brain development, memory performance and nap status over the course of one year at three checkpoints. During the first and second sessions, the children will wear activity-tracking watches and EEG equipment to record naps and overnight sleep. They will also play memory games before and after naps. The children will undergo an MRI brain scan during the third session.
Monica and David Dumlao, of Chicopee, Mass., signed up their son Miles, 4, for the preschool study after watching the Netflix documentary series, “Babies,” which featured Spencer in the episode about sleep. “We like learning about the neuroscience behind brain development,” Monica Dumlao said at a recent study session in Spencer’s lab. “We thought this was a good opportunity to contribute to the science about the importance of naps.”
In the three-part infant study on nap transitions and memory, Spencer is studying the period before and after babies transition from two naps–one in the morning and one in the afternoon–to one, richer afternoon nap. She is recruiting 140 infants 7 to 9 months old. The babies will play a memory game before and after their naps. Their brain activity will be recorded during their naps using a noninvasive electrode cap. The sessions will take place at 9, 12 and 15 months.
“We think as they are getting ready to drop the morning nap, staying awake in that morning interval will be less and less damaging to their memory,” Spencer says. “But we don’t think that’s going to happen with the afternoon nap at this age. We think the afternoon nap stays superimportant.”
Parents interested in participating in the preschool sleep study are invited to fill out a screening form here ; the screening form for the infant nap study is available here .
Source:
University of Massachusetts Amherst
Be the first to rate this article
Posted in: Child Health News | Medical Research News
Brainless memory makes the spinal cord smarter than previously thought
Aya Takeoka at the RIKEN Center for Brain Science (CBS) in Japan and colleagues have discovered the neural circuitry in the spinal cord that allows brain-independent motor learning. Published in Science on April 11, the study found two critical groups of spinal cord neurons, one necessary for new adaptive learning, and another for recalling adaptations once they have been learned. The findings could help scientists develop ways to assist motor recovery after spinal cord injury.
Scientists have known for some time that motor output from the spinal cord can be adjusted through practice even without a brain. This has been shown most dramatically in headless insects, whose legs can still be trained to avoid external cues. Until now, no one has figured out exactly how this is possible, and without this understanding, the phenomenon is not much more than a quirky fact. As Takeoka explains, “Gaining insights into the underlying mechanism is essential if we want to understand the foundations of movement automaticity in healthy people and use this knowledge to improve recovery after spinal cord injury.”
Before jumping into the neural circuitry, the researchers first developed an experimental setup that allowed them to study mouse spinal cord adaptation, both learning and recall, without input from the brain. Each test had an experimental mouse and a control mouse whose hindlegs dangled freely. If the experimental mouse’s hindleg drooped down too much it was electrically stimulated, emulating something a mouse would want to avoid. The control mouse received the same stimulation at the same time, but not linked to its own hindleg position.
After just 10 minutes, they observed motor learning only in the experimental mice; their legs remained high up, avoiding any electrical stimulation. This result showed that the spinal cord can associate an unpleasant feeling with leg position and adapt its motor output so that the leg avoids the unpleasant feeling, all without any need for a brain. Twenty-four hours later, they repeated the 10-minute test but reversed the experimental and control mice. The original experimental mice still kept their legs up, indicating that the spinal cord retained a memory of the past experience, which interfered with new learning.
Having thus established both immediate learning, as well as memory, in the spinal cord, the team then set out to examine the neural circuitry that makes both possible. They used six types of transgenic mice, each with a different set of spinal neurons disabled, and tested them for motor learning and learning reversal. They found that mice hindlimbs did not adapt to avoid the electrical shocks after neurons toward the top of the spinal cord were disabled, particularly those that express the gene Ptf1a .
When they examined the mice during learning reversal, they found that silencing the Ptf1a -expressing neurons had no effect. Instead, a group of neurons in the bottom, ventral, part of the spinal cord that express the En1 gene was critical. When these neurons were silenced the day after learning avoidance, the spinal cords acted as if they had never learned anything. The researchers also assessed memory recall on the second day by repeating the initial learning conditions. They found that in wildtype mice, hindlimbs stabilized to reach the avoidance position faster than they did on the first day, indicating recall. Exciting the En1 neurons during recall increased this speed by 80%, indicating enhanced motor recall.
“Not only do these results challenge the prevailing notion that motor learning and memory are solely confined to brain circuits,” says Takeoka, “but we showed that we could manipulate spinal cord motor recall, which has implications for therapies designed to improve recovery after spinal cord damage.”
Neuroscientists Warn of ‘Cascading’ Alzheimer’s Risk From These Two Habits
Two common habits could be putting you at an increased risk of Alzheimer’s and related dementias, neuroscientists have warned.
Alzheimer’s disease affects roughly 5.8 million Americans, according to the Centers for Disease Control and Prevention. The progressive condition is the most common form of dementia and is associated with memory loss and cognitive decline in the regions of the brain involved in thought, memory and language.
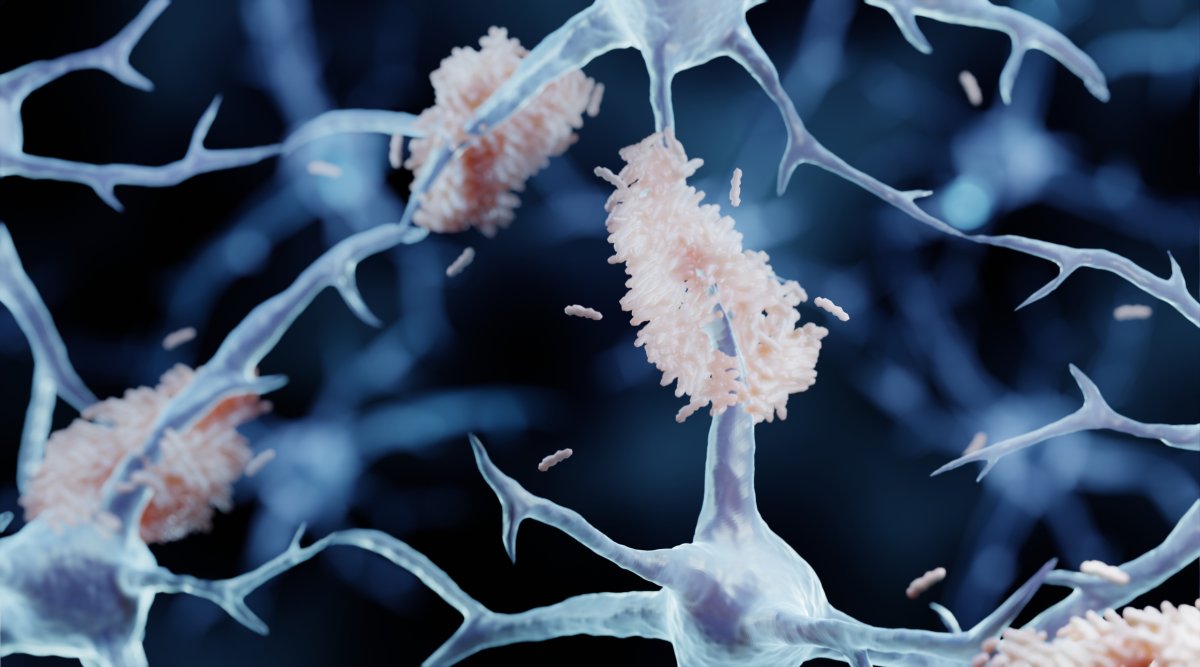
Scientists believe that Alzheimer’s is caused by the abnormal buildup of proteins in and around our brain cells, although exactly what triggers this buildup is still unclear. But what we do know is that our risk of developing Alzheimer’s is dependent on a range of genetic and environmental factors. And among these environmental factors are alcohol consumption and chronic stress. Artist’s impression of abnormal protein build-ups in the brain of a patient with Alzheimer’s. “Alcohol consumption and stress are going to have a synergistic effect on Alzheimer’s Disease risk and general cognitive decline,” Nikki Crowley, director of the Penn State Neuroscience Institute at University Park and an assistant professor of biology, told Newsweek .
Read more: Compare Top Health Savings Accounts
Newsletter
The Bulletin
Your Morning Starts Here
Begin your day with a curated outlook of top news around the world and why it matters.
I want to receive special offers and promotions from Newsweek
By clicking on SIGN ME UP, you agree to Newsweek’s Terms of Use & Privacy Policy . You may unsubscribe at any time.
“This means that when an individual is exposed to both a high amount of stress and drinks alcohol, the combination of the two has a greater impact on that person’s risk of Alzheimer’s disease and cognitive decline. And it’s really going to depend on how much, and how long, an individual experiences stress and alcohol, either together or separately, as well. For instance, some people consume alcohol to cope with stress, and this can have further cascading negative health effects.”
Crowley and colleagues recently published a meta-analysis of the existing research into this synergistic association, which was published in the journal Neurobiology of Stress . And while the exact neuroscience at play here is not fully understood, neuroscientists like Crowley are beginning to fill in the missing pieces of the puzzle.
Exclusively Available to Subscribers Try it now for $1
“Work out of my lab using animal models, which allow us to investigate the mechanism of these changes in the brain on a really rapid timescale, suggests that even moderate amounts of alcohol consumption in midlife can lead to long-lasting changes in the brain that are unlikely to return to their baseline trajectories,” Crowley said.
In particular, alcohol consumption may cause changes in glutamate signaling, which plays an important role in shaping our learning and memory. Interestingly, these same changes are seen during cognitive decline. “While there’s a lot to be done, I think the field is likely going to converge on both alcohol, stress, and other risk factors influencing brain glutamate signaling and inflammation—something researchers have colloquially named ‘inflammaging’—in key brain regions related to cognition and memory,” Crowley said.
With this in mind, what can you do to reduce your risk of developing Alzheimer’s? Let’s start off with alcohol:
“The National Institutes of Alcohol Abuse and Alcoholism at the National Institutes of Health does not recommend a safe level of alcohol consumption,” Crowley said. “They do have some guidelines to help you make healthy decisions though—they suggest less than two alcoholic drinks a day for men and one alcoholic drink a day for women. But any alcohol consumption comes with risks.
“If you have a family history of an alcohol use disorder, or of Alzheimer’s Disease or related dementias, you can talk to your family doctor about whether a zero-alcohol lifestyle is best for you.”
Aside from cutting down on alcohol, Crowley recommends the following: “Taking care of any chronic health issues, working on your diet, getting more physical activity (and sleep!), and limiting alcohol and tobacco use will all have beneficial effects,” she said. “And of course, reducing stress—this can include increasing the amount of time you spend socializing and in mentally stimulating environments.”
Is there a health problem that’s worrying you? Let us know via health@newsweek.com. We can ask experts for advice, and your story could be featured on Newsweek .
Request Reprint & Licensing Submit Correction View Editorial Guidelines
Study suggests a common brain network exists between heart rate deceleration and depression

A new study by researchers at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, suggests a common brain network exists between heart rate deceleration and depression. By evaluating data from 14 people with no depression symptoms, the team found stimulating some parts of the brain linked to depression with transcranial magnetic stimulation (TMS), also affected heart rate, suggesting clinicians may be able to target those areas without the use of brain scans that aren’t widely available. The findings were published in Nature Mental Health. Our goal was to figure out how to harness TMS treatment more effectively, get the dosing right, by selectively slowing down heart rate and identifying the individual best spot to stimulate on the brain.” Shan Siddiqi, MD, senior author of the Brigham’s Department of Psychiatry and the Center for Brain Circuit Therapeutics Siddiqi said the idea first developed during a conference in Croatia where researchers from the Netherlands were presenting heart-brain coupling data. “They showed that not only can TMS transiently lower the heart rate, but it matters where you stimulate,” Siddiqi said, adding that most exciting part of the study for him is the potential to give the rest of the world easier access to this precision targeted treatment for depression. “We have so many things we can do with advanced technology available here in Boston to help people with their symptoms,” he said. “But some of those things couldn’t easily get to the rest of the world before.”
Siddiqi collaborated with his colleagues in the Center for Brain Circuit Therapeutics at the Brigham and lead author, Eva Dijkstra, MSc, to complete the study. Dijkstra is a PhD candidate and came to the Brigham from the Netherlands to combine their work on heart-brain coupling with the CBCT team’s work on brain circuitry.
Researchers looked at functional MRI scans from 14 people and identified spots in their brains believed to be optimal targets for depression based on previous studies done on connectivity and depression. Each participant had 10 spots identified in their brains, both optimal (‘connected areas’) and non-optimal for depression treatment. Researchers then observed what happened to heart rate when they stimulated each spot.
“We wanted to see if there would be mostly heart-brain coupling in the connected areas,” Dijkstra said. “For 12 out of 14 usable data sets, we found we would have a very high accuracy of defining an area that is connected by just measuring heart rate during brain stimulation.”
Dijkstra said the finding could help in both individualizing TMS therapy for depression treatment, by choosing a personalized treatment spot on the brain, and making it more accessible because an MRI wouldn’t need to be done beforehand.
Siddiqi said the findings from this study could also be used to help develop treatments that may eventually be useful to cardiologists and emergency doctors in a clinical setting.
One limitation to the study is it was done on a small number of people, and researchers didn’t stimulate all the possible spots in the brain.
The team’s next goal will be to map out where in the brain to stimulate to make heart rate changes more consistent.
Dijkstra’s team in the Netherlands is now working on a larger study of 150 people with depression disorders, many whose depression is treatment resistant. Data from that study will be analyzed later this year, potentially bringing the research closer to clinical translation.
Source:
Brigham and Women’s Hospital
Journal reference:
Dijkstra, E. S. A., et al . (2024). Probing prefrontal-sgACC connectivity using TMS-induced heart–brain coupling. Nature Mental Health . doi.org/10.1038/s44220-024-00248-8 .
Looking to increase your brain health? Here are a few suggestions

While I’ve been teaching the dining with diabetes classes this past month, I’ve been reminded just how beneficial eating a well balanced diet can be for our overall health.
According to the Alzheimer’s Association, “Eating a heart-healthy diet benefits both your body and your brain. In general, this is a diet that focuses on foods that are less processed and lower in fat, along with more vegetables and leaner meats and proteins.”
We probably think most often about the immediate impact of the foods we eat. Like how they make us feel (satisfied, bloated, hungry, etc.) or whether we gain weight. It seems more difficult to think about how the foods and beverages we consume will eventually affect our cholesterol and blood pressure and blood glucose levels. This is probably because these outcomes are not seen as quickly.
It can be even more of a stretch to think on a regular basis about how the things we eat effect our likelihood of developing chronic disease or cognitive decline. High blood pressure is a leading cause of heart disease and stroke. Over time, high blood pressure puts too much stress on blood vessels. Research shows having uncontrolled high blood pressure in midlife raises the risk for dementia later in life.
In addition to a healthy diet, the Alzheimer’s Association suggests these other healthy habits to increase our brain health:
Challenge your mind – Some people are naturally curious, while others must work at it. Put your brain to work and do something that is new for you. Each season, aim to learn one new skill or further develop an existing skill. If you are typically mechanically minded, then try something artistic. And likewise, if art comes more naturally for you, try building something with directions. Challenging your mind may have short- and long-term benefits for your brain.
Stay in school – Education reduces the risk of cognitive decline and dementia. This starts at a young age and continues. Try taking a class at our local library or join an online class about a topic you are interested in. Consider joining a book club.
Get moving – Engage in regular physical activity. You want to raise your heart rate and increase blood flow to the brain and body. How can you build more movement into your day? Leslie Mayle, registered dietitian at Coshocton Regional Medical Center, is a big fan of YouTube. You can find all sorts of helpful videos to increase physical activity, even while seated. Chair yoga, Silver Sneakers classes, balance exercises and many more are available for free viewing.
Protect your head – Help prevent an injury to your head. Wear a helmet for activities like biking and wear a seatbelt in vehicles. Do what you can to prevent falls by getting rid of throw rugs, eliminating clutter on floors and watching out for pets underfoot.
Be smoke free – The World Health Organization estimated in 2014 that 14% of dementia cases worldwide may be caused by smoking. An analysis in 2015 of more than 30 published studies found current smokers are 30% more likely to develop dementia and 40% more likely to develop Alzheimer’s disease than people who do not smoke. Quitting smoking can lower the risk of cognitive decline back to levels like those who have not smoked. It’s never too late to stop smoking.
Sleep well – Quality sleep is important for brain health. Is your bedroom a peaceful place? Make your space as comfortable as possible and establish a routine for bedtime that does not involve electronic screens like television, tablets or phones.
Today, I’ll leave you with this quote from Dr. Seuss: “I like nonsense; it wakes up the brain cells.”
Emily Marrison is an OSU Extension Family & Consumer Sciences Educator and may be reached at 740-622-2265.
First experimental proof for brain-like computer with water and salt
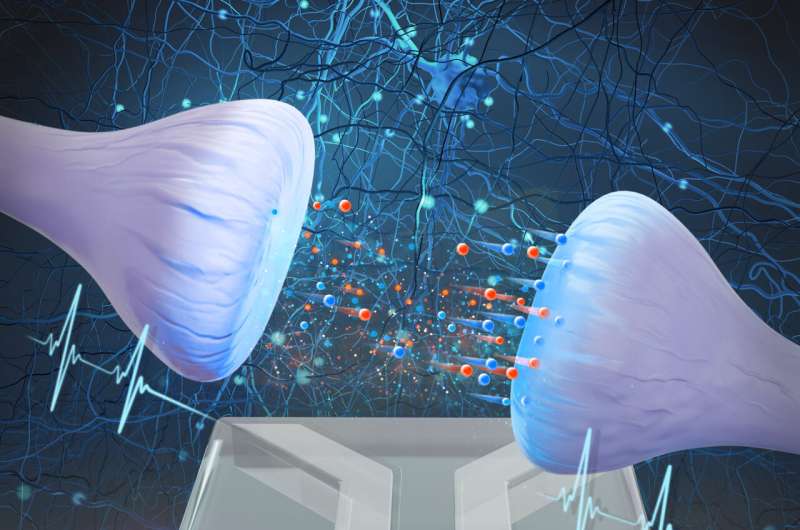
Below shows a graphical representation of the synapse. The synapse consists of colloidal spheres with nano-channels between them. Credit: Utrecht University Theoretical physicists at Utrecht University, together with experimental physicists at Sogang University in South Korea, have succeeded in building an artificial synapse. This synapse works with water and salt and provides the first evidence that a system using the same medium as our brains can process complex information.
The results appear in the journal Proceedings of the National Academy of Sciences .
In the pursuit of enhancing the energy efficiency of conventional computers, scientists have long turned to the human brain for inspiration. They aim to emulate its extraordinary capacity in various ways.
These efforts have led to the development of brain-like computers, which diverge from traditional binary processing to embrace analog methods akin to our brains. However, while our brains operate using water and dissolved salt particles called ions as their medium, most current brain-inspired computers rely on conventional solid materials.
This raises the question: Could we not achieve a more faithful replication of the brain’s workings by adopting the same medium? This intriguing possibility lies at the heart of the burgeoning field of iontronic neuromorphic computing. Artificial synapse
In the latest study published in PNAS , scientists have, for the very first time, demonstrated a system reliant on water and salt exhibiting the ability to process intricate information, mirroring the functionality of our brains. Central to this discovery is a minute device measuring 150 by 200 micrometers, which mimics the behavior of a synapse—an essential component in the brain responsible for transmitting signals between neurons.
Tim Kamsma, a Ph.D. candidate at the Institute for Theoretical Physics and the Mathematical Institute of Utrecht University, and the lead author of the study, expresses his excitement, stating, “While artificial synapses capable of processing complex information already exist based on solid materials, we now show for the first time that this feat can also be accomplished using water and salt. We are effectively replicating neuronal behavior using a system that employs the same medium as the brain.” Microscopic picture of the artificial synapse. Credit: Utrecht University Ion migration
The device, developed by scientists in Korea and referred to as an iontronic memristor, comprises a cone-shaped microchannel filled with a solution of water and salt. Upon receiving electrical impulses , ions within the liquid migrate through the channel, leading to alterations in ion concentration.
Depending on the intensity (or duration) of the impulse, the conductivity of the channel adjusts accordingly, mirroring the strengthening or weakening of connections between neurons. The extent of change in conductance serves as a measurable representation of the input signal.
An additional finding is that the length of the channel impacts the duration required for concentration changes to dissipate. “This suggests the possibility of tailoring channels to retain and process information for varying durations, again akin to the synaptic mechanisms observed in our brains,” says Kamsma.
The genesis of this discovery can be traced back to an idea conceived by Kamsma, who began his doctoral research not long ago. He transformed this concept—centered around the utilization of artificial ion channels for classification tasks—into a robust theoretical model.
“Coincidently, our paths crossed with the research group in South Korea during that period,” says Kamsma. “They embraced my theory with great enthusiasm and swiftly initiated experimental work based on it.”
Remarkably, the initial findings materialized just three months later, closely aligning with the predictions outlined in Kamsma’s theoretical framework. “I thought wow!” he reflects. “It’s incredibly gratifying to witness the transition from theoretical conjecture to tangible real-world outcomes, ultimately resulting in these beautiful experimental results.” A significant step forward
Kamsma underscores the fundamental nature of the research, highlighting that iontronic neuromorphic computing, while experiencing rapid growth, is still in its infancy. The envisioned outcome is a computer system vastly superior in efficiency and energy consumption compared to present-day technology. However, whether this vision will materialize remains speculative at this juncture. Nevertheless, Kamsma views the publication as a significant step forward.
“It represents a crucial advancement toward computers not only capable of mimicking the communication patterns of the human brain but also utilizing the same medium,” he asserts. “Perhaps this will ultimately pave the way for computing systems that replicate the extraordinary capabilities of the human brain more faithfully”
Provided by Utrecht University
Researchers identify targets in the brain to modulate heart rate and treat depressive disorders

Credit: CC0 Public Domain A new study by researchers at Brigham and Women’s Hospital suggests a common brain network exists between heart rate deceleration and depression. By evaluating data from 14 people with no depression symptoms, the team found that stimulating some parts of the brain linked to depression with transcranial magnetic stimulation (TMS) also affected heart rate, suggesting that clinicians may be able to target those areas without the use of brain scans that aren’t widely available. The findings were published in Nature Mental Health.
“Our goal was to figure out how to harness TMS treatment more effectively, get the dosing right, by selectively slowing down heart rate and identifying the individual best spot to stimulate on the brain,” said senior author Shan Siddiqi, MD, of the Brigham’s Department of Psychiatry and the Center for Brain Circuit Therapeutics. Siddiqi said the idea first developed during a conference in Croatia where researchers from the Netherlands were presenting heart-brain coupling data.
“They showed that not only can TMS transiently lower the heart rate, but it matters where you stimulate,” Siddiqi said, adding that most exciting part of the study for him is the potential to give the rest of the world easier access to this precision targeted treatment for depression. “We have so many things we can do with advanced technology available here in Boston to help people with their symptoms,” he said. “But some of those things couldn’t easily get to the rest of the world before.”
Siddiqi collaborated with his colleagues in the Center for Brain Circuit Therapeutics at the Brigham and lead author Eva Dijkstra, MSc, to complete the study. Dijkstra is a Ph.D. candidate and came to the Brigham from the Netherlands to combine their work on heart-brain coupling with the CBCT team’s work on brain circuitry.
Researchers looked at functional MRI scans from 14 people and identified spots in their brains believed to be optimal targets for depression based on previous studies done on connectivity and depression. Each participant had 10 spots identified in their brains, both optimal (“connected areas”) and non-optimal for depression treatment. Researchers then observed what happened to heart rate when they stimulated each spot.
“We wanted to see if there would be mostly heart-brain coupling in the connected areas,” Dijkstra said. “For 12 out of 14 usable data sets, we found we would have a very high accuracy of defining an area that is connected by just measuring heart rate during brain stimulation.”
Dijkstra said the finding could help in both individualizing TMS therapy for depression treatment, by choosing a personalized treatment spot on the brain, and making it more accessible because an MRI wouldn’t need to be done beforehand.
Siddiqi said the findings from this study could also be used to help develop treatments that may eventually be useful to cardiologists and emergency doctors in a clinical setting.
One limitation to the study is it was done on a small number of people, and researchers didn’t stimulate all the possible spots in the brain.
The team’s next goal will be to map out where in the brain to stimulate to make heart rate changes more consistent.
Dijkstra’s team in the Netherlands is now working on a larger study of 150 people with depression disorders, many whose depression is treatment resistant. Data from that study will be analyzed later this year, potentially bringing the research closer to clinical translation.
More information: Probing Prefrontal-sgACC Connectivity using TMS-Induced Heart-Brain Coupling, Nature Mental Health (2024). DOI: 10.1038/s44220-024-00248-8
Provided by Brigham and Women’s Hospital
Wake up and die: Human brain neurons re-entering the cell cycle age quickly shift to senescence
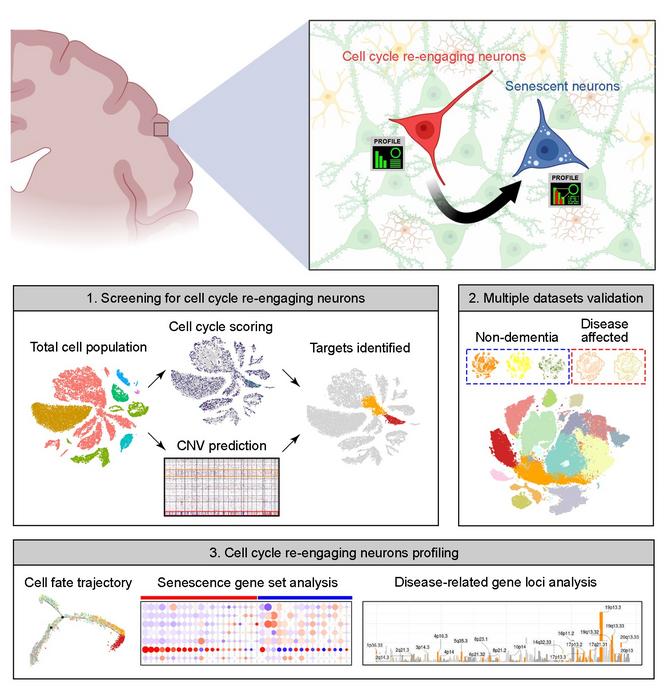
image:
Summary image of the article. The upper part highlights neuronal cell cycle re-engagement is a stage proceeding neuronal senescence and that their full molecular profiles can now be identified by the bioinformatics pipeline we reported in the accepted manuscript. The bottom part is a simplified version of Figure 1A from the paper. The upper panel is created by the BioRender application. view more Credit: Kim Hei-Man Chow (CC-BY 4.0, https://creativecommons.org/licenses/by/4.0/) Post-mitotic neurons in the brain that re-enter the cell cycle quickly succumb to senescence, and this re-entry is more common in Alzheimer’s disease, according to a new study published April 9 th in the open-access journal PLOS Biology by Kim Hai-Man Chow and colleagues at the Chinese University of Hong Kong. The phenomenon may provide an opportunity to learn more about the neurodegeneration process, and the technique used to make this discovery is readily applicable to other inquiries about unique populations of cells in the brain.
Most neurons in the brain are post-mitotic, meaning they have ceased to divide. For many years, it had been assumed that this post-mitotic state was permanent. Recent discoveries have shown that a small proportion of neurons re-enter the cell cycle, but little is known about their fate after they do.
To address this question, the authors turned to publicly accessible databases of “snRNA-seq” data, in which individual single nuclei are isolated and their RNA is sequenced, providing a snapshot of what a cell was doing at the time of isolation. The cell cycle proceeds through distinct phases, including growth, DNA synthesis, division-specific growth, and mitosis, and each phase is characterized by a specific set of proteins required to carry it out. This allowed the authors to use the set of RNAs to tell them which phase of the cycle any specific nucleus was in.
Their data included information on over 30,000 nuclei, each of which was assigned a score based on the level of expression of a set of about 350 cell cycle-related genes. They found that small populations of excitatory neurons had indeed re-entered the cell cycle. These cells did not, for the most part, continue successfully through the cell cycle to produce daughter neurons, however. Instead, cells undergoing re-entry also had elevated expression of genes associated with senescence; in effect, the cells had reawakened only to enter senescence.
Intriguingly, the authors found that neurons in the brains of Alzheimer’s disease patients reentered the cell cycle at a higher rate, and that those neurons that had reentered the cell cycle and aged had increased expression of multiple genes associated with a higher risk of Alzheimer’s disease, including those that contribute directly to production of amyloid, the sticky protein that aggregates in the AD brain. Similarly, brains from patients with Parkinson’s disease and Lewy body dementia had an increase in the proportion of re-entering neurons compared to healthy brains.
The neurobiological significance of this heightened re-entry for the diseased brain is still unclear, but the analytical approach taken here may offer deeper insights into neuronal subpopulations within the brain, as well as shedding light on disease mechanisms in neurodegenerative diseases.
“Because of the rare existence and random localization of these cells in the brain, their molecular profiles and disease-specific heterogeneities remain unclear,” Chow said. “While experimental validations of these findings in relevant human samples will be conducted in the future, the applicability of this analytical approach in different diseases and cross-species settings offers new opportunities and insights to supplement mainstay histological-based approaches in studying the roles of these cells in brain aging and disease pathogenesis.”
The authors add, “This bioinformatics analytical pipeline demonstrated will offer the field a new tool to unbiasedly dissect cell cycle re-engaging and senescent neurons, and to dissect their heterogeneities in healthy versus disease-affected brains.”
#####
In your coverage, please use this URL to provide access to the freely available paper in PLOS Biology : http://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3002559
Citation: Wu D, Sun JK-L, Chow KH-M (2024) Neuronal cell cycle reentry events in the aging brain are more prevalent in neurodegeneration and lead to cellular senescence. PLoS Biol 22(4): e3002559. https://doi.org/10.1371/journal.pbio.3002559
Funding: The work was supported, in part, by grants from the following: The Hong Kong Research Grants Council (RGC)-General Research Fund (GRF) (PI: ECS24107121, GRF16100219 and GRF16100718) (all to K.H-M.C) and the RGC- Collaborative Research Fund (CRF) (Co-I: C4033-19EF) (K.H-M.C); the National NaturalScience Foundation-Excellent Young Scientists Fund 2020 (Ref: 32022087) (K.H-M.C); Alzheimer’s Association Research Fellowship (PI: AARF-17-531566) (K.H-M.C). All the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist. Journal
PLoS Biology DOI
10.1371/journal.pbio.3002559 Method of Research
Observational study Subject of Research
Cells COI Statement
Competing interests: The authors have declared that no competing interests exist.
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.
Globalists programming ChatGPT to “reduce vaccine hesitancy” by parroting public health narratives
At the end of this month, new research will be presented at the Conference of the European Society of Clinical Microbiology and Infectious Diseases showing that the artificial intelligence-driven ChatGPT program dispenses propaganda in promotion of vaccines that comes directly from official public health agencies.
In order to combat so-called “vaccine hesitancy,” ChatGPT has been programmed to push whoever uses it into taking whatever injections the government and media are pushing at any given time, arguing that they are all “safe and effective.”
In addition to dispensing propaganda about sexually transmitted infections (STIs) and other relevant societal problems, ChatGPT is especially focused on encouraging the public to go out and get jabbed at every opportunity – for “public health,” of course.
A press release about the new research explains – supportively, mind you – that “vaccine hesitancy, directly linked to misinformation – false, inaccurate information promoted as factual – is on the rise.”
(Related: ChatGPT is part of the authoritarian future the globalists have planned for the world, complete with AI, palm scanners, facial recognition, augmented reality, and other horrors.) ChatGPT, the new AI government
Many people’s whose own brains are apparently not up to par are now using ChatGPT for all sorts of things. These people ask it questions about information that interests them, including things like “Should I get vaccinated for [fill-in-the-blank]?” ChatGPT then responds to them that they should, no questions asked.
We are building the infrastructure of human freedom and empowering people to be informed, healthy and aware. Explore our decentralized, peer-to-peer, uncensorable Brighteon.io free speech platform here . Learn about our free, downloadable generative AI tools at Brighteon.AI . Every purchase at HealthRangerStore.com helps fund our efforts to build and share more tools for empowering humanity with knowledge and abundance.
The researchers involved in the new study about ChatGPT’s role in urging users to get vaccinated say that it can be “an effective tool to help reduce vaccine hesitancy among the general public.”
The silver lining in all this is that, for those paying attention, we are already ahead of the game. You now know that ChatGPT is artificial fake intelligence – or perhaps it is better described as artificial unintelligence , because there is nothing intelligent about getting vaccinated these days.
There are so many resources now available that were once unavailable showing all the risks and harms caused by vaccine injections, and especially those being peddled on the masses for the Wuhan coronavirus (COVID-19). There is simply no excuse with everything that is out there to fall for any more vaccine scams, though the powers that be are trying with the use of ChatGPT.
When asked any type of questions about STIs, ChatGPT also immediately responds with regurgitated propaganda from the U.S. Centers for Disease Control and Prevention (CDC), including the 2021 CDC STI Treatment Guidelines document.
In other words, ChatGPT is nothing more than the same government goons peddling lies, but in this case through a “cool” and flashy AI program that portends to be “intelligent” artificially.
“Overall, ChatGPT’s responses to vaccine hesitancy were accurate and may help individuals who have vaccine-related misconceptions,” promised lead study author Dr. Matthew Koh, an infectious diseases physician at National University Health System Singapore. (Why is Singapore driving U.S. public health information anyway?)
“Our results demonstrate the potential power of AI models to assist in public health campaigns and aid health professionals in reducing vaccine hesitancy.”
Thank God we live in the United States rather than Singapore. No offense to you if you do live in Singapore, but at least for now, Americans have the right to just say no , as the late First Lady Nancy Reagan once warned, to say no to drugs, including pharmaceutical drugs of the vaccine variety.
“ChatGPT is quite useless,” one commenter at The Defender , a publication of Children’s Health Defense, wrote. “If it does not like the discussion, it just stops and wants to go on to a different subject. Definitely a tool for the very gullible.”
“I am not ‘vaccine hesitant;’ I’m violently opposed,” joked another.
The latest news about the AI takeover of the world can be found at Transhumanism.news .
Sources for this article include:
ChildrensHealthDefense.org
NaturalNews.com Take Action:
Support Natural News by linking to this article from your website.
Permalink to this article:
Copy
Embed article link:
CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
Brain rhythms: Key to understanding emergent thought

Thought emerges and is controlled in the brain via the rhythmically and spatially coordinated activity of millions of neurons, scientists argue in a new article. Understanding cognition and its disorders requires studying it at that level.
It could be very informative to observe the pixels on your phone under a microscope, but not if your goal is to understand what a whole video on the screen shows. Cognition is much the same kind of emergent property in the brain . It can only be understood by observing how millions of cells act in coordination, argues a trio of MIT neuroscientists. In a new article , they lay out a framework for understanding how thought arises from the coordination of neural activity driven by oscillating electric fields-;also known as brain “waves” or “rhythms.”
Historically dismissed solely as byproducts of neural activity, brain rhythms are actually critical for organizing it, write Picower Professor Earl Miller and research scientists Scott Brincat and Jefferson Roy in Current Opinion in Behavioral Science . And while neuroscientists have gained tremendous knowledge from studying how individual brain cells connect and how and when they emit “spikes” to send impulses through specific circuits, there is also a need to appreciate and apply new concepts at the brain rhythm scale, which can span individual, or even multiple, brain regions. Spiking and anatomy are important but there is more going on in the brain above and beyond that. There’s a whole lot of functionality taking place at a higher level, especially cognition.” Earl Miller, senior author, faculty member in The Picower Institute for Learning and Memory and the Department of Brain and Cognitive Sciences at MIT The stakes of studying the brain at that scale, the authors write, might not only include understanding healthy higher-level function but also how those functions become disrupted in disease.
“Many neurological and psychiatric disorders, such as schizophrenia, epilepsy and Parkinson’s involve disruption of emergent properties like neural synchrony,” they write. “We anticipate that understanding how to interpret and interface with these emergent properties will be critical for developing effective treatments as well as understanding cognition.” The emergence of thoughts
The bridge between the scale of individual neurons and the broader-scale coordination of many cells is founded on electric fields, the researchers write. Via a phenomenon called “ephaptic coupling,” the electrical field generated by the activity of a neuron can influence the voltage of neighboring neurons, creating an alignment among them. In this way, electric fields both reflect neural activity but also influence it. In a paper in 2022, Miller and colleagues showed via experiments and computational modeling that the information encoded in the electric fields generated by ensembles of neurons can be read out more reliably than the information encoded by the spikes of individual cells. In 2023 Miller’s lab provided evidence that rhythmic electrical fields may coordinate memories between regions.
At this larger scale, in which rhythmic electric fields carry information between brain regions, Miller’s lab has published numerous studies showing that lower-frequency rhythms in the so-called “beta” band originate in deeper layers of the brain’s cortex and appear to regulate the power of faster-frequency “gamma” rhythms in more superficial layers. By recording neural activity in the brains of animals engaged in working memory games the lab has shown that beta rhythms carry “top down” signals to control when and where gamma rhythms can encode sensory information, such as the images that the animals need to remember in the game.
Some of the lab’s latest evidence suggests that beta rhythms apply this control of cognitive processes to physical patches of the cortex, essentially acting like stencils that pattern where and when gamma can encode sensory information into memory, or retrieve it. According to this theory, which Miller calls “Spatial Computing,” beta can thereby establish the general rules of a task (for instance, the back and forth turns required to open a combination lock), even as the specific information content may change (for instance, new numbers when the combination changes). More generally, this structure also enables neurons to flexibly encode more than one kind of information at a time, the authors write, a widely observed neural property called “mixed selectivity.” For instance, a neuron encoding a number of the lock combination can also be assigned, based on which beta-stenciled patch it is in, the particular step of the unlocking process that the number matters for.
In the new study Miller, Brincat and Roy suggest another advantage consistent with cognitive control being based on an interplay of large-scale coordinated rhythmic activity: “Subspace coding.” This idea postulates that brain rhythms organize the otherwise massive number of possible outcomes that could result from, say, 1,000 neurons engaging in independent spiking activity. Instead of all the many combinatorial possibilities, many fewer “subspaces” of activity actually arise, because neurons are coordinated, rather than independent. It is as if the spiking of neurons is like a flock of birds coordinating their movements. Different phases and frequencies of brain rhythms provide this coordination, aligned to amplify each other, or offset to prevent interference. For instance, if a piece of sensory information needs to be remembered, neural activity representing it can be protected from interference when new sensory information is perceived.
“Thus the organization of neural responses into subspaces can both segregate and integrate information,” the authors write.
The power of brain rhythms to coordinate and organize information processing in the brain is what enables functional cognition to emerge at that scale, the authors write. Understanding cognition in the brain, therefore, requires studying rhythms.
“Studying individual neural components in isolation-;individual neurons and synapses-;has made enormous contributions to our understanding of the brain and remains important,” the authors conclude. “However, it’s becoming increasingly clear that, to fully capture the brain’s complexity, those components must be analyzed in concert to identify, study, and relate their emergent properties.”
Source:
Picower Institute at MIT
Journal reference:
Miller, E. K., et al. (2024). Cognition is an emergent property. Current Opinion in Behavioral Sciences . doi.org/10.1016/j.cobeha.2024.101388 .
Be the first to rate this article
Posted in: Medical Science News | […]

