Nature Knows and Psionic Success
God provides
A “yoga pill” to end anxiety? Neuroscientists discover a brain circuit that instantly deflates stress

Researchers have identified a brain pathway that regulates breathing and calms the mind.
It could pave the way for new medications, like a so-called “yoga pill,” to ease anxiety.
The discovery also grounds ancient wellness practices, such as yoga and breath work, in science.
Your heart is racing, your arms are tingling and your breathing is shallow. You’re having an anxiety attack. And you’re in a public place, to boot. A crowded restaurant, say, or at the office. Not a space where you can comfortably lay on the ground and do some deep breathing exercises to calm yourself.
What if there were a pill that would instead induce that kind of calm breathing for you? That scenario might be possible after a new scientific breakthrough. Lifestyle
For Subscribers The 28 best yoga studios in L.A. for stretching, sweating and spiritual awakenings
9 minutes ago
Neuroscientists at the Salk Institute for Biological Studies in La Jolla have identified a brain pathway that instantly deflates anxiety. The new study, which published earlier this week in the scientific journal Nature Neuroscience , lays out how the aforementioned brain circuit regulates voluntary breathing — meaning conscious breathing as opposed to automatic breathing that happens without your having to think about it — allowing us to slow our breath and calm our mind.
The discovery opens up the potential for the creation of new drugs that would mimic the relaxed state common during breath work, meditation or yoga. Sung Han , senior author of the study, says he’d like to one day see a “yoga pill,” as he calls it, on the market to ease anxiety. It would likely be useful for the more than 40 million adults in the U.S, who, according to the National Alliance on Mental Illness , suffer from an anxiety disorder.
Advertisement
Han says the new discovery is a real scientific breakthrough.
“As a scientist, finding something never known before is always exciting,” he told the Los Angeles Times. “This top-down breathing circuit has been a longstanding question in the neuroscience field. It’s exciting to find the neural mechanism to explain how the slowing down of breathing can control negative emotions, like anxiety and fear.” Lifestyle A trick to reduce stress? Spend 20 seconds a day doing this easy practice
March 25, 2024
We’ve long known that we can control our breathing patterns to alter our state of mind — when we get stressed, we might take a deep, slow breath to feel calmer. But scientists didn’t understand how that worked — which parts of the brain were actually slowing our breath and why that activity makes us calmer. Now they know that there is a group of cells in the cortex, the higher part of the brain responsible for more conscious, complex thought, that send messages to the brain stem, which in turn sends information to the lungs. That’s the aforementioned “circuit.”
The discovery validates soothing behavioral practices such as yoga , mindfulness and even “box breathing” — the latter a technique that involves repeatedly breathing in, then holding your breath, for four-second counts in order to relieve stress — because it grounds these behavioral practices in science.
But the practical applications is what makes the Salk discovery so important, Han says.
“It can, potentially, create a whole new class of drugs that can more specifically target anxiety disorder,” he says.
These would differ from common anti-anxiety medications by more specifically targeting areas of the brain. Common anti-anxiety drugs like Xanax and Lexapro target multiple areas of the brain that control multiple brain processes and behaviors. It’s why these drugs don’t work for everyone in the same way and may create unwanted side effects. More precisely targeting an individual brain circuit makes a medication more effective and reduces potential side effects. And, in extreme cases, such a pill might be more efficient for targeting anxiety than doing breathing exercises. Lifestyle 18 relaxing things to do in L.A. when you just can’t with the world
March 13, 2024
“If you’re in panic, breathing techniques alone may not be sufficient to suppress anxiety,” Han says.
Advertisement
Han’s team is now trying to find the opposite circuit — a fast breathing circuit — that increases anxiety.
“To target the slow breathing circuit, we need to understand the opposite circuit, so we can avoid targeting it,” Han says. “To relieve the anxiety.”
While Han hopes his findings will lead to a “yoga pill,” that’s likely a long ways off. The research, and ensuing clinical trials, could take as much as 10 years, he says. And nothing is for certain.
“I cannot say that this discovery is directly connected to the discovery of the new medication,” Han says. “But I can say it’s a stepping stone. We now know the pathway. That’s exciting. That is the first step.” More to Read
Mindfulness worked as well for anxiety as drug in study Nov. 9, 2022 Deep brain stimulation may be treatment for binge eating disorder, study suggests Aug. 31, 2022
UN Climate Change Censorship Regime seeks to convert journalists into propagandists and take control over the internet

During the latest United Nation’s G20 Summit, world leaders came together to form a new Climate Change Censorship Regime aimed at ramming climate change propaganda down everyone’s throats 24/7, while using their own tax dollars against them.
Educational, Scientific and Cultural Organization (UNESCO) Director-General Audrey Azoulay blatantly said that climate change “disinformation” is “running rampant” on the internet and must be stopped. She desires absolute obedience to climate change narratives. UN Secretary-General Antonio Guterres also addressed the Summit, claiming, “coordinated disinformation campaigns are impeding global progress on climate change.”
“We must fight the coordinated disinformation campaigns impeding global progress on climate change, ranging from outright denial to green-washing to harassment of climate scientists. Through this Initiative, we will work with researchers and partners to strengthen action against climate disinformation,” said UN Secretary-General António Guterres.
To solve this “crisis” of people thinking for themselves, the global leaders introduced something called the Global Initiative for Information Integrity on Climate Change . This is just another sophisticated term describing how world leaders intend to censor individuals online when those individuals disagree with corrupt government/corporate narratives. Climate change brainwashing campaign launched out of the UN
So far, six governments are on board with this proposal of censorship and propaganda, including the central governments of France, Sweden Denmark, Chile, Morocco, and the UK. Initially, these governments will tax their citizens to the tune of $10-$15 million to fund “research and awareness campaigns,” communication strategies, and climate change advocacy groups. Their goal is to inundate the public with climate change narratives 24/7 to drive social and political changes. Of course, these political changes are intended to give power away to a central world government, as an elite group of fraudsters censor and lie to gain power and influence.
By funding communication strategies and brainwashing the public with climate change doom and gloom, globalists can transform their climate change theories into a believable religion — a cult that must be adhered to at all costs. In this authoritarian religion, government is seen as the savior of the planet, and the people are expected to owe their allegiance to the climate experts. As globalists seize upon the sovereignty of nations, as they restrict energy sources and farming, the people of the world are expected to kiss their feet and worship the architects who are behind these manufactured climate crises. If that means supporting geoengineering experiments in the skies and in the sea, then obedience is the answer. No dissent is allowed. UN climate masters want to convert journalists into climate change advocates
UN climate master Audrey Azoulay sees climate change as an “existential challenge” that must be addressed with more government intervention into people’s lives, including the censorship of opposing viewpoints and the converting of journalists into useful idiots who must promote climate change theories that are rooted in hysteria, and inevitably lead to subjugation and population control.
In fact, Azoulay views journalists as “a critical link between science and society.” Instead of reporting the news, journalists are now expected to espouse climate change narratives whenever they are prompted by the UN experts. Azoulay tries to appear compassionate by saying that journalists will be “facing risks while reporting on climate issues” and they should be “preemptively” protected so they can safely report on climate change issues. Converting journalists into official UN mouthpieces is the end goal here, as journalists are expected to abandon their professional role and become one with the hivemind authorities.
“Without access to reliable information about climate disruption, we can never hope to overcome it. Through this initiative, we will support the journalists and researchers investigating climate issues, sometimes at significant risk to themselves, and fight the climate-related disinformation running rampant on social media,” said Audrey Azoulay, UNESCO’s Director-General.
These UN proposals threaten to censor individuals worldwide, while exploiting so-called journalists, who will be turned into propagandists for UN agendas.
Sources include:
ReclaimtheNet.org
G20.org
The Best and Worst Foods for Gut-Brain Health
Key points
Polyphenols and fiber-rich foods feed gut bacteria, boosting mood and brain health.
Avoid added sugar and processed foods to protect your gut-brain connection.
Fermented foods add probiotics that support gut health and mood regulation.
Omega-3s from fatty fish reduce inflammation, enhancing gut and brain function.
Source: Austin Perlmutter/DALL-E In recent years, the gut-brain connection has emerged as a top topic when it comes to brain health. Breakthroughs in research have revealed that the gut contains an extensive network of neurons and communicates directly with the brain through the vagus nerve , immune pathways, the endocrine system, and microbial metabolites. This bidirectional communication plays a critical role in mood regulation, cognition , and overall health.
Understanding how to nourish this connection, then, has profound implications for brain health. In this article, we’re exploring this powerful science and the foods best known to influence the connection The Gut-Brain Connection: A Two-Way Communication Superhighway
You’ve probably heard talk about the importance of the gut in overall health. This stems from the fact that your gut is tasked with digestion, absorption, immune regulation, metabolism, and so much more.
Yet a rapidly expanding subset of gut-focused research has demonstrated that the state of the gut can significantly influence the brain, and vice versa. The five most important channels linking your gut with your brain are the following:
> The Enteric Nervous System (ENS): Sometimes described as a “second brain,” the ENS is embedded in the gut wall and contains over 100 million neurons. It independently regulates digestion and sends signals to the brain.
The Vagus Nerve: Your vagus nerve (cranial nerve 10) is the main physical connection between the gut and the brain, transmitting data from the gut to the brain and motor commands from the brain to the gut.
The Microbiome : The trillions of bacteria, fungi, viruses, and other microbes in your gut produce neuroactive compounds such as serotonin, dopamine , and gamma-aminobutyric acid (GABA), along with molecules called short-chain fatty acids (SCFAs). These chemicals all appear to influence mood, behavior, and cognitive function, although the pathways are different from the effects of these molecules when they’re produced in the brain.
The Immune System: A large percentage of your immune system is located in your gut and is changed based on your diet and microbiome makeup. The gut immune system may directly or indirectly influence brain function by affecting pathways like inflammation.
Endocrine Signaling: The gut produces hormones like ghrelin (hunger hormone), leptin (satiety hormone), and GLP-1, which influence not just appetite but also brain function.
Top Foods to Eat for a Healthy Gut-Brain Connection
> Polyphenol-rich foods: Polyphenols act as prebiotics, meaning they provide nourishment for beneficial gut bacteria. They also appear to act on immune, metabolic, and other pathways to help regulate overall and brain health. Great sources include tea, coffee, spices, and colorful fruits and vegetables.
Fiber-rich foods: Dietary fiber acts as a prebiotic, feeding beneficial gut bacteria. Insufficient fiber is linked to higher rates of immune and metabolic dysfunction that can damage brain health. Insoluble fiber helps with regular bowel movements, while soluble fiber helps feed healthy microbes. Dietary sources of fiber include whole grains, oats, legumes, sunchokes, leafy greens, nuts, seeds, and fruits.
Fermented foods: Fermented foods are rich in probiotics, which introduce beneficial bacteria into your gut. These bacteria may help maintain balance in your microbiome and improve digestion. While largely preclinical, data supports the use of fermented food to positively impact pathways linked to gut-brain health. Examples include yogurt (with live cultures), kefir, sauerkraut, kimchi, miso, and kombucha (but look out for high sugar content in some kombucha!)
Fatty fish: Fatty fish like salmon and mackerel are high in omega-3 fatty acids like EPA and DHA, which are known regulators of immune function and key to brain health. In the gut, omega-3s may support a more balanced gut microbiome. Examples include salmon, mackerel, sardines, and anchovies. Algae-based sources are also commercially available in supplemental form.
Foods to Avoid for a Healthy Gut-Brain Connection
> Added sugar: Added sugar is believed to contribute to systemic immune imbalance, including within the gut. This is one of the mechanisms connecting dietary added sugar with higher rates of cognitive issues , mood disorders, and more. Look out for any foods with added sugars, but especially sugary beverages. We are still learning about the effects of artificial and sugar alternatives on the gut-brain link, but some data suggest that stevia, monkfruit, and allulose may be preferable to other alternatives.
Highly processed foods: Generally speaking, the more a food has been modified from its original state, with additives, emulsifiers, sugars, salts, and fats, the higher the chances that it’s not great for gut and brain health. In primarily animal data, processed food consumption is linked to inflammation, leaky gut, and microbiome changes. In observational data , these foods are linked to higher rates of gut diseases and disorders. In general, avoiding highly processed food is a good move for everyone.
Excess alcohol: While some data indicate that low to moderate amounts of alcohol consumption are linked to better brain health outcomes, the research is clear that excess alcohol consumption damages brain health. Some recent science suggests that alcohol may exert these negative effects (in excess) due to changes in the gut. Generally speaking, research points to two or less alcoholic beverages a day for men and one or less for women as a reasonable threshold.
Dr. Jack Kruse warns about the dangers of BLUE LIGHT EXPOSURE in interview with Mike Adams

Tags: badhealth , badpollution , blood sugar , blue light , brain damaged , brain health , Dangerous , diabetes science , electromagnetic frequency , Health Ranger Report , Jack Kruse , light pollution , Mike Adams , natural light , nutrients , radio frequency , sunlight , UV exposure , vitamin D Brain surgeon Dr. Jack Kruse joined the Health Ranger Mike Adams on the “Health Ranger Report” to talk about the dangers of blue light exposure .
After learning about the work of the late orthopedic surgeon and researcher Dr. Robert O. Becker (1923-2008), Kruse discovered huge problems for patients living in environments surrounded by blue-lit, non-native electromagnetic fields (EMFs) and radio frequency (RF) microwaves. These frequencies were created as a result of the changes brought by Big Tech.
“As soon as we started to use screen technology, and everybody had it around, these disease epidemics got way worse,” the neurosurgeon told Adams. “Many of the people like to blame food and [lack of] exercise for the problems that many have.”
With people now living in a world where blue light is present 24/7, Kruse warned that the chronic elevation of blood sugar is what destroys the brain’s orbital frontal gyrus. He cited a 2011 study by Dr. Nora Volkow, director of the National Institute on Drug Abuse, which found that blue light screens increase a person’s blood glucose and insulin.
“Most of the chronic diseases – neurodegeneration, mental illness, autism – they all start with this story. Because when blood glucose and insulin are raised up by light, it destroys the balance between dopamine, melatonin and cortisol. All of these things tie back to the leptin-melanocortin pathway.” (Related: Damaging effects of blue light worsen with age, study reveals .)
According to Kruse, the obesity crisis goes all the way back to when people started to use light technology in their daily lives. Specifically, this began when Nikola Tesla and George Westinghouse developed the alternating current power grid. Adams: Sunlight is a key nutrient
The Health Ranger agreed with Kruse that natural light, sunlight in particular, is a key nutrient. Adams had written about the importance of sunlight 20 years ago, and interviewed endocrinologist Dr. Michael Holick about vitamin D. Sadly, the Brighteon.com and Natural News founder was attacked for advocating the importance of sunlight for the human body.
He continued that with people having all kinds of deficiencies and toxicities, food doesn’t explain half of what is going on. Kruse agreed, saying that many people don’t realize that food is basically an electromagnetic barcode of what the sun is in relation to Earth and latitude on the planet.
The CEO of the Destin, Florida-based Kruse Longevity Center said blue light specifically affects the proopiomelanocortin (POMC) gene. The POMC gene makes 10 different cleave proteins, including the alpha-melanocyte-stimulating hormones and the adrenocorticotropic hormone (ACTH).
While working with Becker, Kruse discovered non-visual photoreceptors – proteins present in the human body that act as light detectors. One example is neuropsin, the ultraviolet light detector found in the cornea and the skin. With the help of neuropsin, mitochondria in the cornea and the skin absorb light frequency and are programed to do something with it.
Follow NaturalHealth.news for more stories about the importance of light in the human body.
Watch the full conversation between Dr. Jack Kruse and the Health Ranger Mike Adams on the “Health Ranger Report” about the dangers of blue light exposure .
This video is from the Health Ranger Report channel on Brighteon.com . More related stories:
Sunlight exposure reduces cancer risk, study finds .
Blue light from digital devices causes eye strain and increased risk of macular degeneration .
Sunlight is healthy for the eyes: Millions of children have compromised eyesight from not getting enough natural light .
Blue light exposure linked to increased risk of early onset puberty and future fertility issues .
Want to boost brain health and prevent dementia? Vitamin D supplementation is the key, says study .
Sources include:
Brighteon.com
RobertOBecker.net
JackKruse.com Take Action:
Support Natural News by linking to this article from your website.
Permalink to this article:
Copy
Embed article link:CopyReprinting this article:Non-commercial use is permitted with credit to NaturalNews.com (including a clickable link). Please contact us for more information.
New insights into sleep uncover key mechanisms related to cognitive function
While it’s well known that sleep enhances cognitive performance, the underlying neural mechanisms, particularly those related to nonrapid eye movement (NREM) sleep, remain largely unexplored. A new study by a team of researchers at Rice University and Houston Methodist’s Center for Neural Systems Restoration and Weill Cornell Medical College, coordinated by Rice’s Valentin Dragoi, has nonetheless uncovered a key mechanism by which sleep enhances neuronal and behavioral performance, potentially changing our fundamental understanding of how sleep boosts brainpower.
The research, published in Science , reveals how NREM sleep — the lighter sleep one experiences when taking a nap, for example — fosters brain synchronization and enhances information encoding, shedding new light on this sleep stage. The researchers replicated these effects through invasive stimulation, suggesting promising possibilities for future neuromodulation therapies in humans. The implications of this discovery potentially pave the way for innovative treatments for sleep disorders and even methods to enhance cognitive and behavioral performance.
The investigation involved an examination of the neural activity in multiple brain areas in macaques while the animals performed a visual discrimination task before and after a 30-minute period of NREM sleep. Using multielectrode arrays, the researchers recorded the activity of thousands of neurons across three brain areas: the primary and midlevel visual cortices and the dorsolateral prefrontal cortex, which are associated with visual processing and executive functions. To confirm that the macaques were in NREM sleep, researchers used polysomnography to monitor their brain and muscle activity alongside video analysis to ensure their eyes were closed and their bodies relaxed.
The findings demonstrated that sleep improved the animals’ performance in the visual task with enhanced accuracy in distinguishing rotated images. Importantly, this improvement was unique to those who actually fell asleep — the macaques that experienced quiet wakefulness without falling asleep did not show the same performance boost.
“During sleep, we observed an increase in low-frequency delta wave activity and synchronized firing among neurons across different cortical regions,” said first author Dr. Natasha Kharas, a former researcher in Dragoi’s lab and current resident in neurological surgery at Weill Cornell. “After sleep, however, neuronal activity became more desynchronized compared to before sleep, allowing neurons to fire more independently. This shift led to improved accuracy in information processing and performance in the visual tasks.”
The researchers also simulated the neural effects of sleep through low-frequency electrical stimulation of the visual cortex. They applied a 4-Hz stimulation to mimic the delta frequency observed during NREM sleep while the animals were awake. This artificial stimulation reproduced the desynchronization effect seen after sleep and similarly enhanced the animals’ task performance, suggesting that specific patterns of electrical stimulation could potentially be used to emulate the cognitive benefits of sleep.
“This finding is significant because it suggests that some of the restorative and performance-enhancing effects of sleep might be achieved without the need for actual sleep,” said Dragoi, study co-author, professor of electrical and computer engineering at Rice, the Rosemary and Daniel J. Harrison III Presidential Distinguished Chair in Neuroprosthetics at Houston Methodist and professor of neuroscience at Weill Cornell. “The ability to reproduce sleeplike neural desynchronization in an awake state opens new possibilities for enhancing cognitive and perceptual performance in situations where sleep is not feasible — such as for individuals with sleep disorders or in extenuating circumstances such as space exploration.”
The researchers further investigated their findings by building a large neural network model. They found that during sleep, both excitatory and inhibitory connections in the brain become weaker, but they do so asymmetrically, making inhibitory connections weaker than excitatory connections, which causes an increase in excitation.
“We have uncovered a surprising solution that the brain employs after sleep whereby neural populations participating in the task reduce their level of synchrony after sleep despite receiving synchronizing inputs during sleep itself,” Dragoi said.
The idea that NREM sleep effectively “boosts” the brain in this way, and that this resetting can be mimicked artificially, offers potential for developing therapeutic brain stimulation techniques to improve cognitive function and memory.
“Our study not only deepens our mechanistic understanding of sleep’s role in cognitive function but also breaks new ground by showing that specific patterns of brain stimulation could substitute for some benefits of sleep, pointing toward a future where we might boost brain function independently of sleep itself,” Dragoi said.
This research was supported by National Eye Institute grants 5R01EY026156 (V.D.) and 5F31EY029993 (N.K.).
Tweaking non-neural brain cells can cause memories to fade
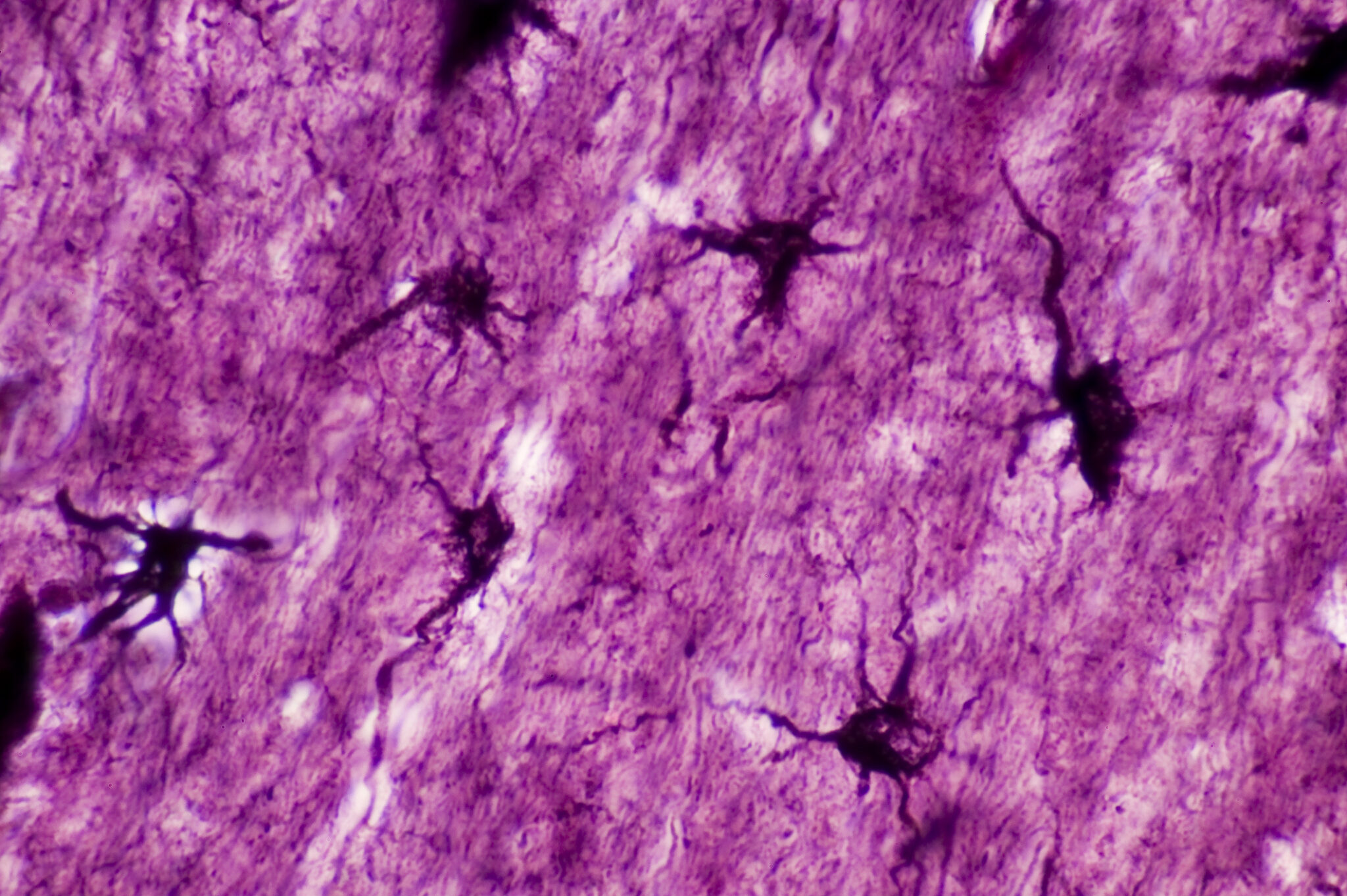
Astrocytes (labelled in black) sit within a field of neurons. “If we go back to the early 1900s, this is when the idea was first proposed that memories are physically stored in some location within the brain,” says Michael R. Williamson, a researcher at the Baylor College of Medicine in Houston. For a long time, neuroscientists thought that the storage of memory in the brain was the job of engrams, ensembles of neurons that activate during a learning event. But it turned out this wasn’t the whole picture.
Williamson’s research investigated the role astrocytes, non-neuron brain cells, play in the read-and-write operations that go on in our heads. “Over the last 20 years the role of astrocytes has been understood better. We’ve learned that they can activate neurons. The addition we have made to that is showing that there are subsets of astrocytes that are active and involved in storing specific memories,” Williamson says in describing a new study his lab has published.
One consequence of this finding: Astrocytes could be artificially manipulated to suppress or enhance a specific memory, leaving all other memories intact. Marking star cells
Astrocytes, otherwise known as star cells due to their shape, play various roles in the brain, and many are focused on the health and activity of their neighboring neurons. Williamson’s team started by developing techniques that enabled them to mark chosen ensembles of astrocytes to see when they activate genes (including one named c-Fos) that help neurons reconfigure their connections and are deemed crucial for memory formation. This was based on the idea that the same pathway would be active in neurons and astrocytes.
“In simple terms, we use genetic tools that allow us to inject mice with a drug that artificially makes astrocytes express some other gene or protein of interest when they become active,” says Wookbong Kwon, a biotechnologist at Baylor College and co-author of the study.
Those proteins of interest were mainly fluorescent proteins that make cells fluoresce bright red. This way, the team could spot the astrocytes in mouse brains that became active during learning scenarios. Once the tagging system was in place, Williamson and his colleagues gave their mice a little scare.
“It’s called fear conditioning, and it’s a really simple idea. You take a mouse, put it into a new box, one it’s never seen before. While the mouse explores this new box, we just apply a series of electrical shocks through the floor,” Williamson explains. A mouse treated this way remembers this as an unpleasant experience and associates it with contextual cues like the box’s appearance, the smells and sounds present, and so on.
The tagging system lit up all astrocytes that expressed the c-Fos gene in response to fear conditioning. Williamson’s team inferred that this is where the memory is stored in the mouse’s brain. Knowing that, they could move on to the next question, which was if and how astrocytes and engram neurons interacted during this process. Modulating engram neurons
“Astrocytes are really bushy,” Williamson says. They have a complex morphology with lots and lots of micro or nanoscale processes that infiltrate the area surrounding them. A single astrocyte can contact roughly 100,000 synapses, and not all of them will be involved in learning events. So the team looked for correlations between astrocytes activated during memory formation and the neurons that were tagged at the same time.
“When we did that, we saw that engram neurons tended to be contacting the astrocytes that are active during the formation of the same memory,” Williamson says. To see how astrocytes’ activity affects neurons, the team artificially stimulated the astrocytes by microinjecting them with a virus engineered to induce the expression of the c-Fos gene. “It directly increased the activity of engram neurons but did not increase the activity of non-engram neurons in contact with the same astrocyte,” Williamson explains.
This way his team established that at least some astrocytes could preferentially communicate with engram neurons. The researchers also noticed that astrocytes involved in memorizing the fear conditioning event had elevated levels of a protein called NFIA, which is known to regulate memory circuits in the hippocampus.
But probably the most striking discovery came when the researchers tested whether the astrocytes involved in memorizing an event also played a role in recalling it later. Selectively forgetting
The first test to see if astrocytes were involved in recall was to artificially activate them when the mice were in a box that they were not conditioned to fear. It turned out artificial activation of astrocytes that were active during the formation of a fear memory formed in one box caused the mice to freeze even when they were in a different one.
So, the next question was, if you just killed or otherwise disabled an astrocyte ensemble active during a specific memory formation, would it just delete this memory from the brain? To get that done, the team used their genetic tools to selectively delete the NFIA protein in astrocytes that were active when the mice received their electric shocks. “We found that mice froze a lot less when we put them in the boxes they were conditioned to fear. They could not remember. But other memories were intact,” Kwon claims.
The memory was not completely deleted, though. The mice still froze in the boxes they were supposed to freeze in, but they did it for a much shorter time on average. “It looked like their memory was maybe a bit foggy. They were not sure if they were in the right place,” Williamson says.
After figuring out how to suppress a memory, the team also figured out where the “undo” button was and brought it back to normal.
“When we deleted the NFIA protein in astrocytes, the memory was impaired, but the engram neurons were intact. So, the memory was still somewhere there. The mice just couldn’t access it,” Williamson claims. The team brought the memory back by artificially stimulating the engram neurons using the same technique they employed for activating chosen astrocytes. “That caused the neurons involved in […]
NREM sleep boosts cognitive performance through brain synchronization

While it’s well known that sleep enhances cognitive performance, the underlying neural mechanisms, particularly those related to nonrapid eye movement (NREM) sleep, remain largely unexplored. A new study by a team of researchers at Rice University and Houston Methodist’s Center for Neural Systems Restoration and Weill Cornell Medical College, coordinated by Rice’s Valentin Dragoi, has nonetheless uncovered a key mechanism by which sleep enhances neuronal and behavioral performance, potentially changing our fundamental understanding of how sleep boosts brainpower.
The research, published in Science , reveals how NREM sleep -; the lighter sleep one experiences when taking a nap, for example -; fosters brain synchronization and enhances information encoding, shedding new light on this sleep stage. The researchers replicated these effects through invasive stimulation, suggesting promising possibilities for future neuromodulation therapies in humans. The implications of this discovery potentially pave the way for innovative treatments for sleep disorders and even methods to enhance cognitive and behavioral performance.
The investigation involved an examination of the neural activity in multiple brain areas in macaques while the animals performed a visual discrimination task before and after a 30-minute period of NREM sleep. Using multielectrode arrays, the researchers recorded the activity of thousands of neurons across three brain areas: the primary and midlevel visual cortices and the dorsolateral prefrontal cortex, which are associated with visual processing and executive functions. To confirm that the macaques were in NREM sleep, researchers used polysomnography to monitor their brain and muscle activity alongside video analysis to ensure their eyes were closed and their bodies relaxed.
The findings demonstrated that sleep improved the animals’ performance in the visual task with enhanced accuracy in distinguishing rotated images. Importantly, this improvement was unique to those who actually fell asleep -; the macaques that experienced quiet wakefulness without falling asleep did not show the same performance boost.
“During sleep, we observed an increase in low-frequency delta wave activity and synchronized firing among neurons across different cortical regions,” said first author Dr. Natasha Kharas, a former researcher in Dragoi’s lab and current resident in neurological surgery at Weill Cornell. “After sleep, however, neuronal activity became more desynchronized compared to before sleep, allowing neurons to fire more independently. This shift led to improved accuracy in information processing and performance in the visual tasks.”
The researchers also simulated the neural effects of sleep through low-frequency electrical stimulation of the visual cortex. They applied a 4-Hz stimulation to mimic the delta frequency observed during NREM sleep while the animals were awake. This artificial stimulation reproduced the desynchronization effect seen after sleep and similarly enhanced the animals’ task performance, suggesting that specific patterns of electrical stimulation could potentially be used to emulate the cognitive benefits of sleep.
“This finding is significant because it suggests that some of the restorative and performance-enhancing effects of sleep might be achieved without the need for actual sleep,” said Dragoi, study co-author, professor of electrical and computer engineering at Rice, the Rosemary and Daniel J. Harrison III Presidential Distinguished Chair in Neuroprosthetics at Houston Methodist and professor of neuroscience at Weill Cornell. “The ability to reproduce sleeplike neural desynchronization in an awake state opens new possibilities for enhancing cognitive and perceptual performance in situations where sleep is not feasible -; such as for individuals with sleep disorders or in extenuating circumstances such as space exploration.”
The researchers further investigated their findings by building a large neural network model. They found that during sleep, both excitatory and inhibitory connections in the brain become weaker, but they do so asymmetrically, making inhibitory connections weaker than excitatory connections, which causes an increase in excitation.
“We have uncovered a surprising solution that the brain employs after sleep whereby neural populations participating in the task reduce their level of synchrony after sleep despite receiving synchronizing inputs during sleep itself,” Dragoi said.
The idea that NREM sleep effectively “boosts” the brain in this way, and that this resetting can be mimicked artificially, offers potential for developing therapeutic brain stimulation techniques to improve cognitive function and memory. Our study not only deepens our mechanistic understanding of sleep’s role in cognitive function but also breaks new ground by showing that specific patterns of brain stimulation could substitute for some benefits of sleep, pointing toward a future where we might boost brain function independently of sleep itself.” Valentin Dragoi, Rice University This research was supported by National Eye Institute grants 5R01EY026156 (V.D.) and 5F31EY029993 (N.K.).
Source:
Rice University
Journal reference:
Kharas, N., et al . (2024). NREM sleep improves behavioral performance by desynchronizing cortical circuits. Science . doi.org/10.1126/science.adr3339 .
Be the first to rate this article
Posted in: Medical Science News | Medical Research News
One serving of greens daily slows brain aging by over a decade

Is memory loss and decreased brain power inevitable as we age? Many people in their 40s, 50s and beyond are told that it is and there is nothing that can be done about it. Is that true? Of course not
(Article republished from GreenMedInfo.com )
Steps can be taken to not only stop memory loss , but also reverse it. Here is a simple step. New research from Rush University Medical Center in Chicago found that eating just one serving of leafy green vegetables a day takes a decade off an aging brain. Two servings produced even greater effects. I explain how below.
Background Data:
There is considerable evidence that diets that are high in green leafy vegetables; highly-colored vegetables such as carrots, yams, and squash; and flavonoid-rich fruits like citrus, berries, and cherries are associated with prevention of age-related memory decline and Alzheimer’s disease . In particular, two large studies have shown that the consumption of green leafy vegetables, including spinach, kale, collards, and lettuce, had the strongest association with slowing down cognitive decline due to aging.
Exactly which nutrients in green leafy vegetables responsible for this effect is unknown, but it is thought to be the entire payload versus any single nutrient or phytochemical. That said, some studies have shown significant protective effects of individual dietary components against cognitive decline. For example, there are studies that report protective effects against dementia with higher dietary intakes of folate, beta-carotene, lutein, and vitamin K1. However, all of these nutrients have different mechanisms of action in offering protection indicating a synergistic effect is undoubtedly expected.
New Data:
To increase understanding of the biological mechanisms underlying the association, the researchers at Rush investigated the individual relations to cognitive decline of the primary nutrients and bioactives in green leafy vegetables, including vitamin K1 (phylloquinone), lutein, ?-carotene, nitrate, folate, kaempferol, and ?-tocopherol.
The study involved the 960 participants of the Memory and Aging Project, ages 58-99 years, who completed a food frequency questionnaire and had ?2 cognitive assessments over a mean 4.7 years. The data was adjusted for age, sex, education, participation in cognitive activities, physical activities, smoking, and seafood and alcohol consumption. After controlling for these factors, consumption of green leafy vegetables was associated with slower cognitive decline; the decline rate for those in the highest quintile of intake (median 1.3 servings/d) was slower by the equivalent of being 11 years younger in age. Higher intakes of each of the nutrients and bioactives except ?-carotene were individually associated with slower cognitive decline.
The conclusion was very clear, consumption of approximately 1 serving per day of green leafy vegetables and foods rich in phylloquinone, lutein , nitrate, folate , ?-tocopherol, and kaempferol help to slow cognitive decline with aging.
Commentary:
In addition to diet, nutritional supplements are also important. In particular, a high potency multiple vitamin and mineral formula and 1,000 mg of EPA and DHA (combined) from a quality fish oil should be considered foundational supplements. Research has clearly established that B vitamin supplements and EPA+DHA can help prevent mental decline in older people with memory problems. Furthermore, an international team led by Oxford University has now found that having higher levels of these nutrients can actually give the brain a boost in people with mild cognitive function. In addition, I would also recommend taking coenzyme Q10 with PQQ, phosphatidylserine, and curcumin to help boost brain function in anyone dealing with symptoms of mental decline.
Read more at: GreenMedInfo.com
Any form of exercise can help rejuvenate the brain

Staying active on a daily basis helps keep the brain young, a recent study shows. Image credit: Hinterhaus Productions/Getty Images. Physical activity of any kind appears to increase a person’s cognitive processing speed, according to a new study.
While it is generally accepted that moderate-to-vigorous exercise benefits brain health, this study finds that any physical activity at all carries with it some cognitive benefit.
The study leveraged mobile phones to allow researchers to survey study participants regarding their activity levels nearly in realtime, and to test their cognitive processing speed multiple times during the day.
The positive effect of being active may have to do with a heightened sense of alertness that comes with physical movement.
Everyday physical activity offers a boost in short-term brain processing speed, according to the findings of a new study from researchers at Penn State College of Medicine.
The study found that common day-to-day activities, regardless of intensity, can provide a short-term improvement in mental reaction time similar to reducing one’s cognitive age by four years.
Previous research has established the value of moderate-to-vigorous physical activity for maintaining cognitive health — and for good health in general.
This study — published in Annals of Behavioral Medicine — uniquely investigates the potential benefit of activities in which people commonly engage during the course of their day, both at work and at home. Real-time data suggest benefits of physical activity
One of the study’s strong points was that it collected participant data almost in real time. For 7 days, participants were surveyed five times a day in an app on their mobile phones regarding their physical activity since their last questioning. At each survey, they also took part in two sets of brain games within the app.
The first game was a symbol-search task in which they were asked to tap a symbol at the bottom of their screen that matched the one displayed at the top. After twelve rounds, their average response time was recorded in the app.
Scores for the symbol-search game, which tested brain processing speed, improved after periods of physical activity.
In the second game, they were asked to recall the location of three dots in a five-by-five grid a few moments after they had been temporarily replaced by a grid of “e”s and “f”s. They played four rounds of the game, with the app scoring their accuracy and calculating their average score.
The researchers saw no improvement in scores for this game that tested working memory after physical activity, although participants did respond more quickly, however inaccurately. Physical activity restores 4 years’ worth of processing speed
Corresponding author Jonathan G. Hakun, PhD , an assistant professor of neurology, psychology, and public health sciences at Penn State, explained for Medical News Today how technology made this sort of real-world study possible.
“It’s a very different approach in that the real novelty is the ability to sample cognition out in everyday life with a smart application,” he said.
Hakun said that, as a person ages, their cognitive processing speed may slow by as much as 15 milliseconds (ms) a year.
The increase in speed exhibited by participants in the study who engaged in physical activity was about 60 ms, the equivalent of gaining back about 4 years’ worth of cognitive processing speed. All types of physical activity good for brain health
At the start of the study, participants were taught how to categorize the activities they were to report to their app.
Light activity included walking to meetings, household chores, walking their dogs, cleaning, and other activities requiring minimal effort.
Brisk walking, nonstrenuous biking, and jogging made up the bulk of moderate-intensity activities that the participants engaged in. Running, fast cycling, and difficult hiking were some examples of vigorous activity.
Some jobs involve plenty of physical activity during work hours. Hakun recalled “a friend who works for UPS, and whenever we did those Fitbit competitions years ago he would get 25,000 steps without even thinking about it.”
Vernon Williams, MD , a sports neurologist and founding director of the Center for Sports Neurology and Pain Medicine at Cedars-Sinai Kerlan-Jobe Institute in Los Angeles, who was not involved in the study, told MNT that the research “is interesting in that it suggests that there is at least a short-term benefit from everyday activity, not just moderate or high intensity ‘exercise.’”
“It underscores our belief that movement — any movement — is generally a good thing,” added Williams. Why exercise benefits cognition long-term
“We’ve known that multiple previously published work, and the overall impression has been, that exercise has a positive effect on cognitive function, including processing speed,” Williams explained for MNT .
As to why that may be, he noted that: “With higher-intensity exercise, and longer duration exercise, there are benefits thought to be related to the release of certain chemicals, neurotransmitters, and factors in the brain that are good for cognitive health. There’s also the concept that physical exercise and activity are associated with improved cardiovascular function, improved blood flow, reduced blood pressure, etc. — all associated with improved cognitive function.” Insofar as the short-term speed gains seen in the study are concerned, Williams suggested that “there may still be some association or correlation with increased blood flow to the frontal lobe associated with even ‘regular’ physical activity.”
“There is also likely to be some cognitive stimulation associated with the physical activity that may also play a role,” he also noted. However, Hakun cautioned that he “would be hesitant to conjecture [regarding] any major neurobiological changes over that quick timescale,” noting that documented effects of exercise take place on a scale of “months to years.”He suspected, instead, that the increase in processing speed has to do with changes in a person’s cognitive processing state as a result of being physically active.He postulated that: “[It is] probably just general alertness. We do know that being alert and more ready to perform a task has advantages for focusing attention and [being] better prepared for […]
Do Brain-Training Games Actually Work? It’s Complicated

Brain-training games may have cognitive benefits — but exactly what they are is a matter of debate. Peter Dressel/Tetra images/Getty Images
Some 2.3 million U.S. adults over 65 — more than 4% — have a diagnosis of dementia . But even without a diagnosis, a certain amount of cognitive decline is normal as age sets in.
Whether it’s due to fear of cognitive decline or noticing lapses in cognition when we are stressed, many of us have had moments when we thought we could use an extra cognitive boost.
The good news is research has shown that people can make changes throughout adulthood that can help prevent or delay cognitive decline and even reduce their risk of dementia. These include quitting smoking and properly managing blood pressure.
In addition to these lifestyle changes, many people are turning to brain-training games, which claim to optimize your brain’s efficiency and capacity at any age. The makers of brain-training apps and games claim their products can do everything from staving off cognitive decline to improving your IQ .
But so far, these claims have been met with mixed evidence .
We are cognitive neuroscientists who focus on brain health across the adult lifespan. We study how the brain informs cognition and the ways we can use brain imaging to understand cognitive and brain-training interventions. We aim to understand how our brains change naturally over time, as well as what we can do about it.
Ongoing research shows what actually happens to the brain when it is engaged in new learning, offering a window into how people can sustain their brain health and how brain-training games can play a role. We believe these studies offer some strategies to train your brain the right way. The Truth About Brain Training
Brain training is a set of tasks, often computerized, based on well-known tests to measure a type of cognition, but in a gamified manner.
Most brain-training games were designed to help participants master one or more specific skills. One example is a game that shows you a letter and number combination, where sometimes you must quickly identify whether the letter is even or odd, while other times you must switch to deciding whether the letter is a consonant or vowel. The game may increase in difficulty by requiring you to accomplish the task within a set time limit.
Such games are designed to require a high level of attention, fast processing speed, and a flexible mind to alternate between the rules, which is known as executive functioning .
However, it turns out that the specific skills learned in these games often do not translate to more general, real-world applications. Whether brain games meet their end goal of lasting cognitive improvement across a number of areas is still highly debated among psychologists . To make such claims requires rigorous evidence that playing a specific game improves cognitive or brain performance.
In 2016, in fact, the Federal Trade Commission issued a US$50 million penalty to one of the most popular brain-training games at the time, Lumosity, for misleading consumers into thinking that they could achieve higher levels of mental performance at work or at school and prevent or delay cognitive decline by using its product.
If improving on a brain game helps the player get better only at that or highly similar games, maybe game developers need a different approach. Improving our brain function is possible, even if many of the claims made by developers of brain-training games are unsupported by scientific evidence. Challenge Yourself
In a study dubbed the Synapse Project , in which one of us, Ian McDonough, helped assess the final outcomes, one group of participants was tasked with engaging in a new activity with which they had little experience. They were assigned to either digital photography or quilting. Though these activities were not games, they were meant to be engaging and challenging and done in a social environment.
Another group was assigned activities that involved little active learning, such as engaging in themed activities related to travel or cooking, or more solitary activities, such as solving crossword puzzles, listening to music, or watching classic movies. These groups met for 15 hours a week over 14 weeks. All participants were tested at the beginning and end of the study on various cognitive abilities.
Those assigned to the new, challenging activities showed significant gains in their memory, processing speed, and reasoning abilities relative to those assigned to the less challenging activities. None of the participants were directly trained on these cognitive tests, which means that the challenging activities enhanced skills that transferred to new situations, such as remembering a list of words or solving abstract problems.
Brain scans of participants showed that over the course of the study, those engaged in the more challenging activities increased their neural efficiency . In other words, their brains didn’t have to work as hard to solve problems or recall information.
The study also showed that the more time participants spent on their projects, the bigger their brains gained and the better their memory was at the end of the 14 weeks.
One difference between the types of activities engaged in the Synapse Project and traditional brain training is whether activities are done in a group or alone. Although other studies have found a benefit to social interaction, the Synapse Project found no difference between the social and solitary activities in the low-challenge group. So, challenge rather than the social components seems to be the driver of maintaining cognitive and brain health. Get Your Brain Healthy
You might be thinking it’s time to take up digital photography or quilting. But in the end, it’s not about those specific tasks. What matters most is that you challenge yourself, which often comes naturally when doing something new. Learning a new skill, alone or in a social setting, is proven to improve cognition. Jose Luis Pelaez Inc/DigitalVision via Getty The new learning that is often accompanied by a sense of effort – and sometimes frustration – requires accessing the resources in the frontal lobe […]
Scientists Say This One Particular Diet May Slow The Decline of The Brain

Brain age While it’s not possible to stop the brain from aging – at least not yet – there might be ways to slow down its decline, and a new study shows the vital role blood sugar levels play in how rapidly the brain ages.
The study is the work of an international team of researchers following up on a 2022 paper that looked at links between diet and brain atrophy. In the previous research, the Mediterranean diet, and particularly the green Mediterranean diet (more plants, less meat), were associated with less wear and tear on the brain.
In this new study, the team wanted to examine some of the mechanisms that might be behind that association. They found a significant relationship between lower blood sugar level markers, and less of the brain shrinkage and neuron death that typically happens as we get older. Green tea could have a protective effect on brain aging. ( Na Visky/Unsplash ) “Maintaining low blood sugar levels, even within the normal range, shows promise for preserving a younger brain, especially when combined with a healthy diet and regular physical activity,” says senior author of the study and epidemiologist Iris Shai, from Ben-Gurion University in Israel.
Data was collected via magnetic resonance imaging ( MRI ) brain scans of 224 participants, averaging around 51 years of age, and diagnosed as obese or having high levels of fat in their blood. Across the course of 18 months, they were split into three groups, and then put on a Mediterranean diet, a green Mediterranean diet, or a standard healthy diet.
Given that slower brain aging was significantly associated with the Mediterranean diets (especially the green one), and lower blood sugar levels, it’s likely that all three factors are linked – with the previous 2022 study offering further supporting evidence.
The researchers noticed that volunteers who consumed plenty of green tea and Mankai duckweed shakes as part of the green Mediterranean diet tended to show the least amount of brain tissue wear. That hints that there’s something about plant-based food that protects the brain.
“Specifically, polyphenols found in plant-based foods may cross the blood-brain barrier and help reduce brain inflammation, which is crucial for memory,” says Shai.
While we can’t infer direct cause and effect from the data, there’s a strong indication that Mediterranean diets are good for the brain – as shown by several past studies . Within that, it seems to be low sugar levels and high plant content that are the main driving forces.
Brain aging is a natural part of getting older to some extent, but faster aging means we’re more at risk of cognitive decline and related neurological diseases at an earlier stage of life. Knowing more about why this happens puts us in a better position to be able to do something about it – like changing our diet .
“This trial offers a safe approach to potentially slow down our brain aging – by adopting the components of a green Mediterranean diet,” says lead author of the study and epidemiologist Dafna Pachter, from Ben-Gurion University.
The research has been published in the American Journal of Clinical Nutrition . Related News
‘Brain Training’ May Not Work, But There Is a Way to Boost Your Cognition
Where Have All The Triplets Gone? The Mystery Explained
Cannabis Really Can Induce Sleep, And Now We Know Why
New study links childhood asthma to higher risk of cognitive challenges later in life

A recent study published in JAMA Network Open has found that children who develop asthma before the age of 12 may be at greater risk of cognitive challenges , particularly in memory.
Asthma is a widespread chronic condition affecting approximately 4.6 million children in the United States. Characterized by airway inflammation that causes difficulty breathing, asthma often emerges in early childhood, with symptoms potentially impacting overall health and development.
The study used data from the Adolescent Brain Cognitive Development (ABCD) Study, an ongoing research project that began in 2015 and includes about 11,800 children aged 9 to 10. The study compared children who reported asthma at the beginning of the project and those who developed it later to examine episodic memory performance, a cognitive function critical for recalling experiences and emotions. (Related: Natural and effective remedies for asthma .)
“This study underscores the importance of looking at asthma as a potential source of cognitive difficulty in children,” Simona Ghetti, a professor of psychology at the University of California, Davis (UC Davis) Center for Mind and Brain and lead author of the study, said in a press statement.
The study analyzed data from over 2,069 children aged nine to 10, and matched asthmatic children among children without asthma based on factors like age, sex and other health conditions to ensure a fair comparison. The study assessed how asthma affects episodic memory and other cognitive measures.
The researchers discovered that children with asthma scored lower on episodic memory tests than their peers without the chronic respiratory condition. Meanwhile, in a smaller sample of nearly 500 children tracked for more than two years, the researchers observed that children with an earlier onset of asthma showed slower memory development over time.
“Childhood is a period of rapid improvement in memory and, more generally, cognition,” said first study author Nicholas Christopher-Hayes, a doctoral candidate in psychology at UC Davis. “In children with asthma that improvement may be slower.” Children with asthma also at risk of dementia and Alzheimer’s disease in later life
Aside from affecting memory during childhood, the study also discovered that asthma-related memory deficits could have lasting effects, potentially increasing the risk of cognitive decline in later life.
The researchers cited prior studies linking asthma with a heightened risk of dementia and Alzheimer’s disease in older adults.
“Asthma might set children on a trajectory that could increase their risk to later develop something more serious like dementia as adults,” Christopher-Hayes said.
While the study did not pinpoint specific mechanisms underlying these memory difficulties, the researchers highlighted several possibilities, such as chronic inflammation and the effects of restricted oxygen supply to the brain during asthma attacks. Additionally, asthma medications, particularly corticosteroids, commonly used to treat asthma symptoms, may affect the functioning of the brain’s memory centers like the hippocampus.
Ghetti concluded that children with asthma may be at increased risk for memory difficulties that start during childhood rather than appearing solely as later-life cognitive challenges.
Watch this video to learn more natural treatments for asthma . This video is from the Holistic Herbalist channel on Brighteon.com . More related stories:
CDC insists aluminum adjuvant in vaccines is safe even though study shows it causes asthma in children .
Widespread use of disinfectants and hand sanitizers (quaternary ammonium compounds) is fueling the asthma and infertility crisis .
GlaxoSmithKline is pulling a longstanding, life-saving asthma inhaler from the market, putting asthmatic children at risk .
Del Bigtree: CDC continues to promote vaccine schedule for babies despite the shots containing aluminum that causes asthma .
Study: A type of vitamin E found in nuts helps prevent asthma attacks .
Sources include:
TheEpochTimes.com
JAMANetwork.com
Brighteon.com
Battling Brain Inflammation: Strategies for a Healthier Mind

Key points
Chronic inflammation can damage the brain, affecting mood and cognitive function over time.
Neuroinflammation is linked to disorders like Alzheimer’s and depression.
Key lifestyle changes—like better sleep, less sugar, and regular exercise—can help target brain inflammation.
Source: Austin Perlmutter/DALL-E/OpenAI In recent years, there’s been a growing awareness of neuroinflammation, an immune response in the brain. Research suggests that chronic inflammatory activation could be a central driver behind many chronic diseases, including conditions affecting mental health and cognitive function. Understanding neuroinflammation, what triggers it, and the lifestyle factors that can either amplify or reduce it could play a significant role in improving brain health. What Is Neuroinflammation?
Neuroinflammation refers to inflammation within the brain, primarily involving immune cells called microglia. Unlike inflammation in other parts of the body, which typically arises in response to infection or injury, neuroinflammation can occur without the presence of pathogens. In these cases, it’s usually triggered by damage-associated molecules (DAMPs) or inflammatory markers from systemic conditions like obesity, diabetes, and chronic stress .
Microglial cells are the brain’s resident immune defenders. They continuously monitor their environment for signs of danger or damage. When they detect something abnormal—such as an increase in toxic proteins or damage to brain cells—microglia activate and produce pro-inflammatory cytokines like TNF-alpha and IL-1B. This process can help protect the brain in the short term but, when chronic, can lead to neuronal damage and, over time, contribute to cognitive decline and mental health disorders. The Link Between Neuroinflammation and Brain Disorders
Neuroinflammation is increasingly being implicated in a range of brain diseases and disorders, including: Neurodegenerative Diseases Like Alzheimer’s. In a host of neurodegenerative diseases like Alzheimer’s , brain inflammation may be increased. Findings here include activation of the brain’s microglial cells as well as elevated levels of inflammatory markers.
Mood Disorders. Depression and anxiety have been correlated with elevated levels of inflammatory markers. Most notably, higher levels of inflammation may drive symptoms of depression.
Poor Cognitive Function. Chronic systemic inflammation has been linked to cognitive decline, likely due to neuroinflammatory responses that impair brain plasticity and neurogenesis. Evidence also points to a correlation between air pollution, such as PM2.5 (fine particulate) exposure, and cognitive impairments, underscoring the broader impact of environmental factors on brain inflammation.
Triggers of Neuroinflammation
Several factors contribute to increased neuroinflammation, many of which are related to modern lifestyle and environmental conditions:
> Air Pollution. Fine particulate matter (PM2.5) from both outdoor and indoor sources can exacerbate inflammation in the brain. Studies have shown that prolonged exposure to indoor air pollution is associated with increased risks of cognitive decline, including conditions like dementia .
Sleep Deficits. Poor sleep quality or sleep disorders like obstructive sleep apnea (OSA) are associated with an increased risk of neuroinflammatory markers. Sleep helps clear out brain toxins, including amyloid-beta, which is linked to Alzheimer’s. Even one night of sleep deprivation can elevate inflammation in the brain, emphasizing the importance of restful sleep for brain health.
Chronic Stress. Long-term exposure to stress can lead to increased microglial activation, contributing to chronic inflammation in the brain. Psychological stress is believed to play a role in activating immune cells and driving epigenetic changes that make the body more prone to inflammatory responses.
Diet and Sugar Intake. High intake of processed sugar and ultra-processed foods has been shown to increase inflammatory markers in the brain. A diet high in refined sugars promotes inflammatory responses and may lead to insulin resistance, a known risk factor for neurodegenerative diseases like Alzheimer’s.
Sedentary Behavior. Physical inactivity has been correlated with higher levels of systemic inflammation, which can translate into increased neuroinflammation. Exercise, even in moderate amounts, has anti-inflammatory effects and is shown to reduce the risk of cognitive decline.
6 Lifestyle Changes That Can Help Reduce Neuroinflammation
Given the link between neuroinflammation and various lifestyle factors, small changes in daily habits can significantly impact brain health. Here are six strategies to consider:
> Sleep: Aim for seven to nine hours of quality sleep per night. Sleep is essential for brain repair processes, including the clearance of inflammatory proteins and toxins.
Stress Management : Incorporate stress-mitigation practices, such as meditation , mindfulness , or cognitive-behavioral therapy (CBT).
Substance Reduction: Limit alcohol intake, as alcohol consumption can increase inflammatory markers like IL-6 and TNF-alpha.
Minimize Sugar and Processed Foods: Refined sugars and processed foods drive inflammation in the body. Opt for a diet high in omega-3s, fiber, polyphenols, and diverse plant-based foods to help combat inflammation.
Physical Activity: Engage in at least 30 minutes of moderate exercise daily. Studies indicate that exercise, particularly in older adults, can reduce inflammatory markers and improve cognitive function through increased blood flow and the release of neuroprotective compounds.
A Smoke-Free Environment: Avoid smoking and reduce exposure to secondhand smoke, as both can elevate inflammatory markers and have a compounding effect on individuals with pre-existing metabolic conditions.
Stress Scrambles Memories: New Insights From Neuroscience

Recent research reveals that acute stress causes mice to form generalized memories rather than specific ones, through mechanisms involving elevated corticosterone and endocannabinoid activation in the brain. This finding could lead to new treatments for anxiety-related memory disorders. Credit: SciTechDaily.com Acute stress has been shown to prevent mice from forming specific memories, instead leading to more generalized memories encoded by a larger number of neurons.
This phenomenon, driven by elevated corticosterone levels, was reversed through pharmacological intervention, offering hope for therapeutic applications in human disorders like PTSD and generalized anxiety disorder. Stress and Memory Generalization
Stress has a complex relationship with memory. While emotional or stressful events are often more memorable, stress can also make it harder to recall memories. In conditions like PTSD and generalized anxiety disorder, this dynamic takes a troubling turn, leading to overgeneralized aversive memories that make it difficult to distinguish between safe and dangerous situations. Until recently, however, the role of stress in memory generalization was unclear.
New research, published today (November 15) in the journal Cell , reveals that acute stress prevents mice from forming specific memories. Instead, stressed mice develop generalized memories, which involve larger groups of neurons. Discovering the Role of Stress in Memory Formation
“We are now beginning to really understand how stress impacts aversive memories, and I think that’s good news for everybody,” says memory researcher and co-senior author Sheena Josselyn of The Hospital for Sick Children (SickKids) and the University of Toronto. “We were able to isolate the synaptic mechanisms that drove this and also show that this same phenomenon can be manipulated or blocked by using systemically available drugs.”
To test whether stress impacts memory specificity, the researchers trained mice to associate one sound with stress, and another sound with no stress. Then, they tested the mice’s ability to react appropriately to the different sounds. Impact of Corticosterone on Memory Specificity
Mice who had been placed in an acutely stressful, controlled experience exhibited defensive behavior regardless of which sound was played to them, suggesting that the stressful experience interfered with their ability to form specific memories. In contrast, control mice who had not been subjected to stress exhibited defensive freezing only in response to the original sound.
Because the stressed mice had elevated levels of corticosterone in their blood, the researchers next tested whether corticosterone itself could impact memory formation. They showed that mice that received corticosterone prior to training were also unable to form specific memories to the two sounds, and that administering metyrapone, a chemical that inhibits glucocorticoid synthesis, restored the ability of stressed mice to form specific memories.
Specific memories are encoded by groups of neurons called engrams. Most engrams involve only a few neurons, but the researchers showed that the generalized engrams formed by stressed mice were larger, because inhibitory interneurons—gatekeeping cells that usually keep engrams exclusive—failed to do their job. This change, in turn, was driven by endocannabinoids that were released in the amygdala in response to corticosterone. Future Directions in Memory Research
“When we manipulated endocannabinoid receptors in just one particular cell type in one brain region, it restored memory specificity and the size of the engram,” says stress researcher and co-senior author Matthew Hill of the University of Calgary. “This whole phenomenon is mediated by a very discrete microcircuit in the amygdala, but you can do a systemic pharmacological manipulation and still prevent it, which is very encouraging from the perspective of whether this could one day be translated for therapeutic use in humans.”
In future, the researchers want to investigate whether stress also impacts the specificity of non-aversive memories. They also plan to examine whether exogenous cannabinoids (e.g., cannabis) would have a similar effect on memory specificity, which could have implications for PTSD management.
“We only examined aversive threat memories, but it would be interesting to examine whether stress similarly increases the generalization of a rewarding memories,” says memory researcher and co-senior author Paul Frankland, also at SickKids and the University of Toronto.
“Given that this phenomenon involved the activation of endocannabinoid receptors, it would be very interesting to see if a stoned animal shows a similar generalization response,” says Hill. “That’s one of the things that I’d be curious to quickly run as a follow up, because if it did, that would have some interesting implications given that the whole conversation that exists right now around cannabis and PTSD is very confusing.”
Reference: “Stress disrupts engram ensembles in lateral amygdala to generalize threat memory in mice” by Lesuis et al., 15 November 2024, Cell .
DOI: 10.1016/j.cell.2024.10.034
This research was supported by the Dutch Research Council, Niels Stensen Fellowship, ZonMw Memorabel, Canadian Institutes of Health Research, Alzheimer Nederland, Toronto Cannabis and Cannabinoid Research Consortium, and the Brain Canada Foundation.
Weight Loss Breakthrough: Scientists Discover Natural Compound That Suppresses Appetite

Researchers discovered BHB-Phe, a body-produced compound regulating appetite and weight by activating neurons in the brain, with potential implications for obesity treatment. Unlike related compound Lac-Phe, BHB-Phe uses distinct neural mechanisms to influence feeding behavior and metabolism. BHB-Phe, a newly discovered compound, reduces appetite and body weight by activating specific brain neurons.
Researchers from Baylor College of Medicine , Stanford University School of Medicine , and their collaborators have identified a novel compound called BHB-Phe, which is naturally produced by the body. Published in the journal Cell , their findings reveal that BHB-Phe regulates appetite and body weight by interacting with neurons in the brain.
Until now, BHB has been known as a compound produced by the liver to be used as fuel. However, in recent years, scientists have found that BHB increases in the body after fasting or exercise, prompting interest in investigating potential beneficial applications in obesity and diabetes. BHB-Phe and Its Role in Metabolism
In the current study, the team at Stanford University led by co-corresponding author Dr. Jonathan Z. Long, associate professor of pathology, discovered that BHB also participates in another metabolic pathway. In this case, an enzyme called CNDP2 joins BHB to amino acids. Furthermore, the most abundant BHB-amino acid, BHB-Phe, can influence body weight and metabolism in animal models.
The Baylor team, headed by co-corresponding author Dr. Yong Xu, professor of pediatrics – nutrition and associate director of basic sciences at the USDA/ARS Children’s Nutrition Research Center at Baylor, took on the task of investigating how BHB-Phe influences feeding behavior and body weight in mice.
“We know that groups of neurons in the brain regulate feeding behavior, so we mapped the entire brain to determine which areas were activated by BHB-Phe,” Xu said. “We found that BHB-Phe activates neural populations in the hypothalamus and brainstem, and this suppresses feeding and reduces body weight. In contrast, mice genetically modified to not produce CNDP2 and therefore lack BHB-Phe, ate more and gained weight.”
Interestingly, the CNDP2 enzyme that produces BHB-Phe also produces a related compound called Lac-Phe, previously discovered by the authors. Lac-Phe, the researchers reported in Nature , is a compound in the blood that is produced during exercise and can reduce food intake and obesity in mice. But do Lac-Phe and BHB-Phe mediate their common effects by activating the same neurons in the brain? Distinct Neural Pathways for BHB-Phe and Lac-Phe
“Our analyses showed that only a small proportion of neurons were activated by both compounds; most of the neurons activated by Lac-Phe and BHB-Phe were different,” Xu said. “This indicates the possibility that, although both compounds affect feeding behaviors in similar ways, they mediate this effect by different mechanisms.”
The findings suggest that the new pathway involving BHB-Phe, which is also present in people, could be disrupted in obesity and maybe other conditions, supporting the need for further studies to better understand the mechanism.
“This work opens up many new possibilities,” Long said. “For example, it might be possible for people in the future to consume BHB-Phe to drive weight loss without restricting carbohydrates in their diet.”
Reference: “A β-hydroxybutyrate shunt pathway generates anti-obesity ketone metabolites” by Maria Dolores Moya-Garzon, Mengjie Wang, Veronica L. Li, Xuchao Lyu, Wei Wei, Alan Sheng-Hwa Tung, Steffen H. Raun, Meng Zhao, Laetitia Coassolo, Hashim Islam, Barbara Oliveira, Yuqin Dai, Jan Spaas, Antonio Delgado-Gonzalez, Kenyi Donoso, Aurora Alvarez-Buylla, Francisco Franco-Montalban, Anudari Letian, Catherine P. Ward, Lichao Liu, Katrin J. Svensson, Emily L. Goldberg, Christopher D. Gardner, Jonathan P. Little, Steven M. Banik, Yong Xu and Jonathan Z. Long, 12 November 2024, Cell .
DOI: 10.1016/j.cell.2024.10.032
Neuroscientists Just Discovered a Specific Type of Exercise Can Make You Stay Smarter, and for Much Longer

Productivity
Your brain naturally rewires itself as you age—but research shows it doesn’t have to, and not as quickly.
NOV 14, 2024 Photo: Getty Images My father’s cognitive decline was substantial by the time he passed.
Actually, “substantial” is an understatement. Some part of him seemed to know I was a person he knew, but he didn’t know who I was. When he did speak, it was stimulus-response, mostly “no” and “all right.” He lost control of most basic bodily functions. Near the end, he sometimes seemed to forget how to swallow. Some things remained—for example, he still responded to music—but for the most part, he was “gone,” a word he used, while he could, to describe what he feared was happening to him.
I think about that when I consider antiaging startups, especially those launched by famous entrepreneurs: Jeff Bezos of Amazon fame, Larry Ellison of Oracle, Peter Thiel of PayPal, or Google co-founders Sergey Brin and Larry Page . They, along with numerous other startups, have made considerable investments in trying to find ways to help people live longer. Insights From New Research
It all makes sense. Lifespan matters to all of us. So does health span, that is, the length of time you’re healthy, not just alive. So does brain span, the ability to maintain brain health and function; in simple terms, to not be “gone.” Which might be something you don’t need to invest hundreds of millions in startup funds to potentially address. According to a study just published in NeuroImage: Clinical , regular resistance training—think body weight or actual weights, not cardio—may help delay or reduce the onset of cognitive decline as we age.
FEATURED VIDEO
An Inc.com Featured Presentation
As the researchers write : For the first time we show that six months of high intensity resistance exercise is capable of not only promoting better cognition in those with [mild cognitive impairment], but also protecting Alzheimer’s disease-vulnerable hippocampal subfields from degeneration for at least 12 months post-intervention. Or, in non-researcher-speak, regular resistance training improves the health of your hippocampus, the part of your brain largely responsible for memory and learning. Resistance training also improves your brain’s ability to change and adapt, or what neurologists call “hippocampal plasticity.” Yep, there’s a scientific term for everything. From Muscle to Mind
Ninety minutes per week, spread across two to three workouts, seems to be the cognition-promoting sweet spot.
Interestingly, a study just published in Advanced Healthcare Materials found that muscle contraction releases myokines, molecules shown to facilitate neural growth.
As those researchers write : This study demonstrates that tuning the mechanical properties of fibrin enables longitudinal culture of highly contractile skeletal muscle monolayers, enabling functional characterization of and long-term secretome harvesting from exercised tissues. Motor neurons stimulated with exercised muscle-secreted factors significantly upregulate neurite outgrowth and migration, with an effect size dependent on muscle contraction intensity. All of which is a fancy way of saying that when your muscles contract during exercise, the resulting myokine release causes neurons to grow four times faster than those not exposed to myokines–and new cells are always a good thing, whether for repairing damage or enhancing and even extending function. A Personal Reflection
Which leads us back to my dad. His cognitive decline took place over a number of years. He knew he was slipping, and he wished there was a way to slow or stop the decline. Other than seeing a doctor, I didn’t know what to tell him. Had I known resistance training might have helped, I surely would have encouraged him.
Had a business owner explained that resistance training might help, I feel sure he would have been all in. Dying “early” wasn’t my father’s primary concern. Losing who he was, mentally and emotionally, while still alive, was his greatest fear.
Billions of dollars of research later, longevity technology still isn’t here. Supplements, ultrasound, red light therapy, magnet therapy, cold tubs for ice baths … the scientific evidence is currently slim regarding causal outcomes from cutting-edge longevity treatments.
But as an entrepreneur, you could address the market in ways already proven—and that require considerably less capital. Muscle strength, cardiovascular fitness, flexibility, and body weight can have a major impact on overall health. Resistance training can have an impact on cognitive health, and on nerve health. One study found that every minute of exercise can add five minutes to your life . Maybe you’ll find ways to help people use exercise to improve their lifespans, health spans, and brain spans.
Do that, and you could build a thriving business that makes a real difference in other people’s lives. I know my dad would have signed up.
Scientists Develop Breakthrough Nasal Spray That Could Delay Alzheimer’s by Over a Decade

A new nasal spray therapy by Texas A&M researchers shows promise in delaying Alzheimer’s progression by targeting brain inflammation and reducing harmful proteins. Tested in animal models, it may extend cognitive function by 10-15 years, offering a potential breakthrough in Alzheimer’s treatment. Research from the College of Medicine provides promising insights into delaying the progression of Alzheimer’s disease for several years after the initial diagnosis.
A recent study by researchers at Texas A&M University College of Medicine suggests that a new therapy could potentially slow the progression of Alzheimer’s disease by several years. Published in the Journal of Extracellular Vesicles , the research focuses on developing treatment options for Alzheimer’s, the most prevalent form of dementia and a leading cause of death among people aged 65 and older, affecting nearly 7 million Americans.
Utilizing a nasal spray to non-invasively target cells perpetuating chronic neuroinflammation, researchers found decreased inflammation in the brain and a reduction in the build-up of plaques and proteins thought to be linked to the progressive loss of neurons in the brain, characteristic of Alzheimer’s.
“This approach is effective because the cargo carried by these extracellular vesicles could reduce the neuropathological changes in the brain,” says Ashok K. Shetty, Ph.D., a University Distinguished Professor and associate director at the Institute for Regenerative Medicine in the Department of Cell Biology and Genetics. Early Testing in Animal Models
Shetty, collaborator Madhu LN, Ph.D., and their colleagues, administered the nasal spray treatment to an animal model in the early stages of Alzheimer’s. Compounding their promising results, researchers also found that microglia, immune cells within the brain, incorporated the intranasally administered neural stem cell-derived extracellular vesicles. Lead researcher Ashok Shetty has filed a patent on the intranasal application of neural stem cell-derived extracellular vesicles for treating Alzheimer’s and other neurological and neurodegenerative disorders. Credit: Abbey Santoro / Texas A&M University In Alzheimer’s, microglia activate to cause inflammation and clear Alzheimer’s-related plaques from the brain. This initially helpful function becomes problematic over time, Shetty says. “Prolonged activation causes them to lose their normal function and begin to harm neurons, leading to progressive neuron loss.”
Findings indicate that an intake of neural stem cell-derived extracellular vesicles significantly changed microglia gene expression and reduced the multiple harmful proinflammatory proteins without affecting the microglia’s ability to continue clearing the protein buildup related to Alzheimer’s, Madhu says.
Shetty has filed a patent on the intranasal application of neural stem cell-derived extracellular vesicles for treating Alzheimer’s and other neurological disorders. He says the research conducted in his lab — funded by the National Institute on Aging — already has inspired further studies, and he hopes successful research could point toward treatment delaying Alzheimer’s-related changes and severe cognitive issues by 10 to 15 years after initial diagnosis. “Our journey to advance the application of this therapy for Alzheimer’s disease is just beginning,” he says.
Reference: “Extracellular vesicles from human-induced pluripotent stem cell-derived neural stem cells alleviate proinflammatory cascades within disease-associated microglia in Alzheimer’s disease” by Leelavathi N. Madhu, Maheedhar Kodali, Raghavendra Upadhya, Shama Rao, Yogish Somayaji, Sahithi Attaluri, Bing Shuai, Maha Kirmani, Shreyan Gupta, Nathaniel Maness, Xiaolan Rao, James J. Cai and Ashok K. Shetty, 5 November 2024, Journal of Extracellular Vesicles .
DOI: 10.1002/jev2.12519
The study was funded by the National Institute on Aging.
Mind-Blowing Discovery: Scientists Discover That Memories Are Not Only in the Brain

A groundbreaking study has found that cells outside the brain may have memory functions, challenging the long-held belief that memory is exclusive to brain cells. Researchers demonstrated that non-brain cells could learn from spaced repetition, activating a “memory gene” similar to brain cells. Research reveals that kidney and nerve tissue cells can learn and form memories in ways similar to neurons.
Our brains—and specifically, our brain cells—are commonly known to store memories. However, a team of scientists has discovered that cells from other parts of the body also play a role in memory, opening new pathways for understanding how memory functions and creating potential for enhancing learning and treating memory-related conditions.
“Learning and memory are generally associated with brains and brain cells alone, but our study shows that other cells in the body can learn and form memories, too,” explains New York University’s Nikolay V. Kukushkin, the lead author of the study, which appears in the journal Nature Communications .
The research sought to better understand if non-brain cells help with memory by borrowing from a long-established neurological property—the massed-spaced effect—which shows that we tend to retain information better when studied in spaced intervals rather than in a single, intensive session—better known as cramming for a test. An NYU researcher administers chemical signals to non-neural cells grown in a culture plate. Credit: Nikolay Kukushkin
In the Nature Communications research, the scientists replicated learning over time by studying two types of non-brain human cells in a laboratory (one from nerve tissue and one from kidney tissue) and exposing them to different patterns of chemical signals—just like brain cells are exposed to patterns of neurotransmitters when we learn new information. In response, the non-brain cells turned on a “memory gene”—the same gene that brain cells turn on when they detect a pattern in the information and restructure their connections in order to form memories. Tracking Memory Gene Activation
To monitor the memory and learning process, the scientists engineered these non-brain cells to make a glowing protein, which indicated when the memory gene was on and when it was off.
The results showed that these cells could determine when the chemical pulses, which imitated bursts of neurotransmitter in the brain, were repeated rather than simply prolonged—just as neurons in our brain can register when we learn with breaks rather than cramming all the material in one sitting. Specifically, when the pulses were delivered in spaced-out intervals, they turned on the “memory gene” more strongly, and for a longer time, than when the same treatment was delivered all at once.
“This reflects the massed-space effect in action,” says Kukushkin, a clinical associate professor of life science at NYU Liberal Studies and a research fellow at NYU’s Center for Neural Science. “It shows that the ability to learn from spaced repetition isn’t unique to brain cells, but, in fact, might be a fundamental property of all cells.” An NYU researcher administers chemical signals to non-neural cells grown in a culture plate. Credit: Nikolay Kukushkin The researchers add that the findings not only offer new ways to study memory, but also point to potential health-related gains.
“This discovery opens new doors for understanding how memory works and could lead to better ways to enhance learning and treat memory problems,” observes Kukushkin. “At the same time, it suggests that in the future, we will need to treat our body more like the brain—for example, consider what our pancreas remembers about the pattern of our past meals to maintain healthy levels of blood glucose or consider what a cancer cell remembers about the pattern of chemotherapy.”
Reference: “The massed-spaced learning effect in non-neural human cells” by N. V. Kukushkin, R. E. Carney, T. Tabassum and T. J. Carew, 7 November 2024, Nature Communications .
DOI: 10.1038/s41467-024-53922-x
The work was jointly supervised by Kukushkin and Thomas Carew, a professor in NYU’s Center for Neural Science. The study’s authors also included Tasnim Tabassum, an NYU researcher, and Robert Carney, an NYU undergraduate researcher at the time of the study.
This research was supported by a grant from the National Institutes of Health (R01-MH120300-01A1).


