Nature Knows and Psionic Success
God provides
Cancer-causing chemical found in 78 sunscreen products

(Image credit: Shutterstock)
An independent testing lab has detected the chemical benzene, a known human carcinogen, in 78 sunscreen products and is now calling on the U.S. Food and Drug Administration (FDA) to recall the products.
The lab, Valisure, checks medications and health care products for quality. Recently, the company tested nearly 300 sunscreen products and found that 27% contained benzene, according to a statement from the company . Fourteen of the products (5%) contained benzene at levels higher than 2 parts per million (ppm), which is the FDA’s recommended limit for benzene in medically valuable drugs that can’t be made without it.
“The presence of this known human carcinogen in products widely recommended for the prevention of skin cancer and that are regularly used by adults and children is very troubling,” David Light, founder and CEO of Valisure, said in the statement.
Benzene is a colorless or light yellow liquid that forms naturally but is also produced by human activities, according to the Centers for Disease Control and Prevention (CDC) . For example, automobile emissions and the burning of coal and oil can release benzene into the air; the chemical is also used in the manufacturing of some plastics, rubbers, dyes, detergents, drugs and pesticides, according to the CDC.
Exposure to high levels of benzene causes cancer in humans, particularly blood cancer, including leukemia . The U.S. Occupational Safety & Health Administration limits workplace exposure to benzene in the air to 1 ppm on an average day and a maximum of 5 ppm over a 15-minute period, according to the American Cancer Society . The Environmental Protection Agency limits benzene in drinking water to 0.005 ppm, or 5 parts per billion (ppb), which is also the limit for bottled water.
The FDA says that benzene should not be used in the manufacturing of drug products except in special circumstances, mainly if their use is unavoidable and the drug product makes a significant therapeutic advance. In these cases, benzene levels should be limited to 2 ppm “unless otherwise justified,” the FDA says . In the beginning of the COVID-19 pandemic when there was a shortage of hand sanitizer, the FDA temporarily allowed hand sanitizers to contain up to 2 ppm of benzene. But in March 2021, Valisure announced they had detected benzene above this level in nearly two dozen hand sanitizer products, at least one of which was later recalled .
In light of its new findings of benzene in sunscreens, Valisure has petitioned the FDA to recall the 78 products and to conduct its own investigation into the manufacturing of these products. A full list of the sunscreen products with benzene can be found in the petition. Nearly all of the 14 sunscreen products with benzene levels above 2 ppm were sprays; but the chemical also showed up in lotions and sunburn-relief gels.
Although the FDA says benzene should not be used in the manufacturing of drugs, the agency does not define a specific limit for drugs like sunscreen (The FDA regulates sunscreen as an over-the-counter drug.). The 2 ppm limit applies only to the “special circumstances” outlined by the agency. So Valisure is also calling on the FDA to set a limit for benzene levels in sunscreen and other drug products in standard situations, and to set a limit for exposure in a single day.
Since benzene wasn’t detected in most of the sunscreens Valisure tested, the company says that the use of benzene in sunscreens is not “unavoidable,” and any detectable amount of the chemical shouldn’t be allowed.
“It is critical that regulatory agencies address benzene contamination in sunscreens … so that all individuals feel safe using sunscreen products,” Dr. Christopher Bunick, an associate professor of dermatology at Yale University, said in the statement.
In a statement provided to Live Science, the FDA said it is reviewing the petition. “The FDA takes seriously any safety concerns raised about products we regulate, including sunscreen. While the agency evaluates the submitted citizen petition, we will continue to monitor the sunscreen marketplace and manufacturing efforts to help ensure the availability of safe sunscreens for U.S. consumers,” the statement said. The agency added that it generally does not comment on pending petitions.
The findings do not mean that people should stop using sunscreen, which can help prevent skin cancer, Bunick said
“Many sunscreen products tested by Valisure did not have benzene contamination, and those products are presumably safe and should continue to be used, along with appropriate hats and sun-protective clothing, to mitigate skin cancer risk,” Bunick said.
Editor’s note: This article has been updated to include comments from the FDA.
Originally published on Live Science.
‘We made a big mistake’ — COVID vaccine spike protein travels from injection site, can cause organ damage

( Natural News ) COVID vaccine researchers had previously assumed mRNA COVID vaccines would behave like traditional vaccines. The vaccine’s spike protein — responsible for infection and its most severe symptoms — would remain mostly in the injection site at the shoulder muscle or local lymph nodes.
(Article by Megan Redshaw republished from ChildrensHealthDefense.org )
But new research obtained by a group of scientists contradicts that theory, a Canadian cancer vaccine researcher said last week.
“We made a big mistake. We didn’t realize it until now,” said Byram Bridle, a viral immunologist and associate professor at University of Guelph, Ontario. “We thought the spike protein was a great target antigen, we never knew the spike protein itself was a toxin and was a pathogenic protein. So by vaccinating people we are inadvertently inoculating them with a toxin.”
Bridle, who was awarded a $230,000 grant by the Canadian government last year for research on COVID vaccine development, said he and a group of international scientists filed a request for information from the Japanese regulatory agency to get access to Pfizer’s “ biodistribution study .”
Biodistribution studies are used to determine where an injected compound travels in the body, and which tissues or organs it accumulates in.
“It’s the first time ever scientists have been privy to seeing where these messenger RNA [mRNA] vaccines go after vaccination,” Bridle said in an interview with Alex Pierson where he first disclosed the data. “Is it a safe assumption that it stays in the shoulder muscle? The short answer is: absolutely not. It’s very disconcerting.”
The Sars-CoV-2 has a spike protein on its surface. That spike protein is what allows it to infect our bodies, Bridle explained. “That is why we have been using the spike protein in our vaccines,” Bridle said. “The vaccines we’re using get the cells in our bodies to manufacture that protein. If we can mount an immune response against that protein, in theory we could prevent this virus from infecting the body. That is the theory behind the vaccine.”
“However, when studying the severe COVID-19, […] heart problems , lots of problems with the cardiovascular system, bleeding and clotting , are all associated with COVID-19,” he added. “In doing that research, what has been discovered by the scientific community, the spike protein on its own is almost entirely responsible for the damage to the cardiovascular system, if it gets into circulation.”
When the purified spike protein is injected into the blood of research animals, they experience damage to the cardiovascular system and the protein can cross the blood-brain barrier and cause damage to the brain, Bridle explained .
The biodistribution study obtained by Bridle shows the COVID spike protein gets into the blood where it circulates for several days post-vaccination and then accumulates in organs and tissues including the spleen, bone marrow, the liver, adrenal glands and in “quite high concentrations” in the ovaries.
“We have known for a long time that the spike protein is a pathogenic protein, Bridle said. “It is a toxin. It can cause damage in our body if it gets into circulation.”
A large number of studies have shown the most severe effects of SARS-CoV-2, the virus that causes COVID, such as blood clotting and bleeding, are due to the effects of the spike protein of the virus itself.
A recent study in Clinical and Infectious Diseases led by researchers at Brigham and Women’s Hospital and the Harvard Medical School measured longitudinal plasma samples collected from 13 recipients of the Moderna vaccine 1 and 29 days after the first dose and 1-28 days after the second dose.
Out of these individuals, 11 had detectable levels of SARS-CoV-2 protein in blood plasma as early as one day after the first vaccine dose, including three who had detectable levels of spike protein. A “subunit” protein called S1, part of the spike protein, was also detected.
Spike protein was detected an average of 15 days after the first injection, and one patient had spike protein detectable on day 29 — one day after a second vaccine dose — which disappeared two days later.
The results showed S1 antigen production after the initial vaccination can be detected by day one and is present beyond the injection site and the associated regional lymph nodes.
Assuming an average adult blood volume of approximately 5 liters, this corresponds to peak levels of approximately 0.3 micrograms of circulating free antigen for a vaccine designed only to express membrane-anchored antigen.
In a study published in Nature Neuroscience , lab animals injected with purified spike protein into their bloodstream developed cardiovascular problems. The spike protein also crossed the blood-brain barrier and caused damage to the brain.
It was a grave mistake to believe the spike protein would not escape into the blood circulation, according to Bridle. “Now, we have clear-cut evidence that the vaccines that make the cells in our deltoid muscles manufacture this protein — that the vaccine itself, plus the protein — gets into blood circulation,” he said.
Bridle said the scientific community has discovered the spike protein, on its own, is almost entirely responsible for the damage to the cardiovascular system, if it gets into circulation.
Once in circulation, the spike protein can attach to specific ACE2 receptors that are on blood platelets and the cells that line blood vessels, Bridle said. “When that happens it can do one of two things. It can either cause platelets to clump, and that can lead to clotting — that’s exactly why we’ve been seeing clotting disorders associated with these vaccines. It can also lead to bleeding,” he added.
Both clotting and bleeding are associated with vaccine-induced thrombotic thrombocytopenia (VITT). Bridle also said the spike protein in circulation would explain recently reported heart problems in vaccinated teens.
Stephanie Seneff, senior research scientists at Massachusetts Institute of Technology, said it is now clear vaccine content is being delivered to the spleen and the glands, including the ovaries and the adrenal glands, and is being shed into the medium and then eventually reaches the bloodstream causing systemic damage.
“ACE2 receptors are common in the heart and brain,” she added. […]
Intermittent fasting is key to a “healthy lifestyle,” experts suggest

( Natural News ) Intermittent fasting is an eating pattern that cycles between periods of fasting and eating. It is said to promote weight loss, lower blood pressure and boost brain health, among others. But what does science actually say about intermittent fasting?
In a review published in The New England Journal of Medicine , neuroscientist Mark Mattson of Johns Hopkins Medicine and aging specialist Rafael de Cabo of the National Institute on Aging examined past studies on intermittent fasting to elucidate the science-backed benefits of intermittent fasting . Evidence-based benefits of intermittent fasting
Mattson and de Cabo mentioned an array of animal and human studies that showed intermittent fasting supports cellular health, probably by triggering metabolic switching. This occurs when cells use up their stores of rapidly consumed, sugar-based fuel and begin converting fat into energy through a slower metabolic process. Known as an age-old adaptation to periods of food scarcity, metabolic switching improves blood sugar control, increases resistance to stress and suppresses inflammation.
Meanwhile, other studies found that intermittent fasting helps lower blood pressure, blood lipid levels and resting heart rate. There is also evidence suggesting that intermittent fasting could modify risk factors for obesity and Type 2 diabetes .
In a pair of studies involving 100 overweight women, those on a 5:2 intermittent fasting — which requires consuming one moderate-sized meal for two days a week and eating normally for the rest — lost the same amount of weight as women on a low-calorie diet . At the same time, they experienced improvements in insulin sensitivity and greater reductions in belly fat. (Related: Intermittent fasting found to boost heart health, lower diabetes risk .)
Studies also suggest that eating patterns like intermittent fasting can help boost brain health . A study from the University of Toronto , for example, found that sticking to a calorie-restricted diet for two years helps improve memory.
Mattson and de Cabo acknowledged that more studies are needed to support the benefits of intermittent fasting on learning and memory. If these benefits are established, fasting could serve as a new intervention for delaying cognitive decline and dementia .
Mattson urged people to practice patience and ask guidance from physicians if they are struggling to fast. He noted that it normally takes time for the body to adjust and overcome the initial hunger pangs and irritability that come with fasting.
“Patients should be advised that feeling hungry and irritable is common initially and usually passes after two weeks to a month as the body and brain become accustomed to the new habit,” he said.
For those who wish to try intermittent fasting, Mattson recommends increasing the duration and frequency of your fasting periods gradually over several months to manage the initial side effects of intermittent fasting. How to do intermittent fasting
There are many ways to do intermittent fasting . Here are some of the most popular methods:
> The 16/8 method – This involves fasting every day for 14 to 16 consecutive hours and eating only within the remaining hours of the day.
The 5:2 diet – As mentioned earlier, this requires consuming one moderate-sized meal for two nonconsecutive days each week and eating normally for the rest.
Eat-stop-eat – This involves fasting for an entire day, once or twice a week.
Alternate-day fasting – As its name suggests, this requires fasting every other day.
The warrior diet – This involves fasting all day and eating at night within a four-hour eating window.
Intermittent fasting is extremely beneficial for health. It can boost brain health, improve blood sugar control and promote weight loss, among others. Follow Fasting.news to learn more about the different methods of fasting and their health benefits.
Sources include:
Blood biomarker detects whether depression is due to neurodegeneration

A test could be used as a rapid screening tool in clinics to determine whether a patient’s cognitive problems are due to neurodegeneration. A new study published in the journal Nature Communications is reporting a single blood-based biomarker can detect the presence of 13 neurodegenerative disorders, from frontotemporal dementia to motor neuron disease. The test cannot specifically distinguish each disorder but instead is proposed as a way to determine whether patients with memory problems are suffering from the early stages of neurodegenerative disease.
Neurofilament light chain (NfL) is a protein released into cerebrospinal fluid when brain cells are damaged. It can be detected in blood, and researchers have long investigated this biomarker as a way of easily diagnosing neurodegenerative diseases such as Alzheimer’s .
This new study investigated over 3,000 blood samples from a diverse cohort of subjects with the goal of finding out whether NfL blood levels could differentiate cognitively healthy subjects from those with neurodegenerative diseases.
The research found NfL levels could effectively detect subjects with one of 13 different neurodegenerative disorders, including amyotrophic lateral sclerosis (ALS), frontotemporal dementia, and Alzheimer’s disease. Plus, even more significantly, NfL levels could be used to identify whether patients with moderate to severe depression were suffering from the early stages of neurodegeneration.
Abdul Hye, joint senior author on the study, says this particular finding means NfL levels could be used in clinical contexts to help doctors determine if a patient’s cognitive symptoms are an early sign of neurodegeneration or another kind of psychiatric problem.
“For the first time we have shown across a number of disorders that a single biomarker can indicate the presence of underlying neurodegeneration with excellent accuracy,” says Hye. “Though it is not specific for any one disorder, it could help in services such as memory clinics as a rapid screening tool to identify whether memory, thinking or psychiatric problems are a result of neurodegeneration.”
Although the study found NfL blood levels could not diagnose specific neurodegenerative conditions, the researchers note the biomarker does have value in tracking nuances within certain groups of patients. High blood NfL levels in Parkinson’s disease patients, for example, were found to signal atypical cases of the disorder. In subjects with Down syndrome high NfL levels were found to correlate with dementia.
“This suggests that the new marker could potentially be used to improve the diagnosis of Alzheimer’s in people with Down syndrome, as well as to be used as a biomarker to show whether treatments are effective or not,” explains study co-author Andre Strydom. “It is exciting that all that could be needed is a simple blood test, which is better tolerated in Down syndrome individuals than brain scans.”
As NfL levels naturally rise with age, the new study also offers age-related cut-offs separating normal from abnormal NfL levels. This will help clinicians determine whether NfL blood levels are a sign of neurodegeneration or simply a natural accumulation that comes with aging.
“Blood-based NfL offers a scalable and widely accessible alternative to invasive and expensive tests for dementia,” adds Hye. “It is already used as a routine assessment in some European countries such as Sweden or Netherlands, and our age-related cut-offs can provide a benchmark and quick accessible test for clinicians, to indicate neurodegeneration in people who are exhibiting problems in thinking and memory.”
The new study was published in the journal Nature Communications .
Here Are 10 Amazing Benefits Of Learning To Play Musical Instruments

Have a fascination for musical instruments? Learn where that can take you and the benefits it offers. playing music m Lockdown had a very harsh effect on people’s lives, it took a toll on everyone’s emotional and physical well-being. But that’s just the negatives, if we look on the brighter side, many people took this opportunity to rediscover themselves and some potentially had enough time to learn new things and grow their skill set. Learning instruments was one of them. As some of us might not know, incorporating music in our lives can be very beneficial and positive for us. Here are some benefits of learning to play musical instruments, read on for more. 1 Boosts Self-Confidence And Self-Discipline
The complete process of learning to play an instrument can potentially have a very positive impact on the learner’s personality as he progresses through the journey. According to research, playing an instrument can boost self-confidence and significantly increase self-discipline. The learner is required to play in front of an audience or a teacher which boosts self-confidence, and, as a part of the learning process, one has to have a lot of dedication and should be ready to invest great time and effort which can eventually add discipline in one’s day to day activities and behaviour. 2 Can Make You Smarter
According to medical science, musicians tend to have more brain power than non-musicians. This is because while learning, musicians eventually grow more grey areas in their brains, which is the powerhouse of information processing, memory, and intellectual abilities. So, does this inspire you to grab a guitar and start learning asap? Cause we still have a lot more reasons for you to do so. 3 Prevents Hearing Loss In Older Age
As we grow older, our hearing ability starts to deteriorate. That is why older people have more hearing problems than younger people. Well, it seems like that’s not the case for musicians! While learning to play an instrument, a musician develops special hearing skills which can actually keep your ears healthy and active for your entire life. 4 Strengthens The Immune System
Learning a musical instrument can have a direct effect on your immune system as well. According to research, playing an instrument can strengthen your immune response by promoting the production of immunoglobulin-A, which is a type of natural anti-viral killer cell. 5 Increases Time-Management
Learning to play an instrument can also help you regulate your time management skills. As challenging as it sounds like, if you desire to achieve something at any cost, for example learning an instrument and incorporate it as a part of your skill chart, can really help you to understand how not to waste your time and manage it wisely as you’ll tend to schedule your practice hours in-between your busy schedule. 6 Reduces Stress
Playing an instrument or listening to music, in general, can have a positive effect on your mental health. It can significantly reduce stress and pain by suppressing the stress hormone. That’s why learning an instrument is widely assumed to be a natural anti-depressant. 7 Incorporates Patience And Persistence
The learning process involved in mastering an instrument requires a lot of patience and consistent practice. That is why it can help you to be more patient and you gradually learn how to control your mind and be calmer. 8 Cultivates Creativity
Once you master your instrument and develop a more clear sense of learning and creating new things in music to express yourself, you eventually become more creative without even knowing it. Music is art, and the more you learn how to use your paintbrush, imagination, and your skills correctly, your painting or your art will turn out to be more beautiful, and the more you’ll be able to express yourself. 9 Increases Expression And Emotional Stability
Musicians tend to express their emotions more effortlessly and on a deeper level according to research. If you find it difficult to convey your feelings to other people, then, deciding to learn an instrument can really help you get past this problem easily. 10 Improves Memory
Learning an instrument can improve your memory capabilities. It is proven that engaging in musical activities can make one have significantly better memory and brain functioning.
Brain Maps May Reveal the Origins and Paths of Neurological Dysfunction

Genetic Engineering & Biotechnology News Statisticians like to say, “All models are wrong, but some are useful.” Mapmakers could say the same thing about their maps. Mapmakers, however, could add that some maps complement each other, or have the potential to do so. Such potential is beginning to be realized for brain maps, which are still—forgive the expression—all over the map. Some brain maps illustrate neuroanatomy in exquisite detail, some capture spatial information about the flicker and glow of signaling events, and some indicate how gene expression or protein expression varies from place to place within the brain.
Unfortunately, brain maps of different types correlate hardly at all. Consider the gaps between whole-brain neuroimaging, which relies on tools such as functional magnetic resonance imaging (fMRI), and neurobiological imaging, which relies on tools such as immunohistochemistry and next-generation sequencing.
Neuroimaging may be undertaken noninvasively, in living organisms, but it suffers from poor resolution. In contrast, neurobiological imaging may achieve molecular and cellular resolution, but it is typically invasive, requiring the use of postmortem tissue.
Bridging the divides between different types of brain maps could help scientists relate large-scale brain functions to the molecular and cellular activities that support these functions. For example, processes such as perception and memory could be analyzed at a deeper level. Also, conditions such as autism, schizophrenia, and neurodegenerative disease could be better correlated with molecular phenomena. Instead of accumulating mere genotype-phenotype associations, scientists could detail pathways and mechanisms.
In this article, we’ll briefly touch on two well-developed types of brain mapping—the creation of molecular brain atlases, and the modeling of brain activities. Finally, we’ll look at nascent efforts to bridge these kinds of brain mapping. Specifically, we’ll report on recent progress in the development of molecular fMRI, an alternative form of fMRI that monitors brain activity through the use of chemical or genetically encoded probes. Deriving insights from brain atlases
Brain mapping is an audacious pursuit, one that has inspired multiple “big science” initiatives. Among the most prominent initiatives is the Human Brain Atlas. This initiative, which was undertaken by the Allen Institute for Brain Science, is consolidating anatomical and gene expression information.
The Allen Institute’s stated mission is to provide publicly available resources that accelerate basic and clinical research of the human brain in normal and disease states. Examples of how the Allen Institute’s work is assisting researchers can be found at the organization’s website, which presents “Data Stories.” One of these stories describes how researchers at the University of Cambridge merged data from the Allen Human Brain Atlas with MRI brain scans and made an important discovery about the teenage brain.
The scientists used MRI to study the brain structure of almost 300 individuals aged 14–24 years old. By comparing the brain structure of teenagers of different ages, the scientists found that during adolescence, the outer regions of the brain, known as the cortex, shrink in size, becoming thinner. However, as this happens, levels of myelin—the sheath that “insulates” nerve fibers, allowing them to communicate efficiently—increase within the cortex.
These findings appeared in the Proceedings of the National Academy of Sciences , in an article titled, “Adolescence is associated with genomically patterned consolidation of the hubs of the human brain connectome.” The article also indicated that the “topologically focused process of cortical consolidation was associated with expression of genes enriched for normal synaptic and myelin-related processes and risk of schizophrenia.”
Essentially, the researchers found that during adolescence, brain regions that have the strongest link to the schizophrenia risk genes are developing most rapidly. “As these regions are important hubs that control how regions of our brain communicate with each other, it shouldn’t be too surprising that when something goes wrong there, it will affect how smoothly our brains work,” Edward T. Bullmore, PhD, the study’s senior author and head of psychiatry at Cambridge, noted in a statement. “If one imagines these major hubs of the brain network to be like international airports in the airline network, then we can see that disrupting the development of brain hubs could have as big an impact on communication of information across the brain network as disruption of a major airport, like Heathrow, will have on flow of passenger traffic across the airline network.” Using machine learning to map brain activity
A recent contribution to GEN by Richard A. Stein, MD, PhD, discussed how artificial intelligence technology is helping researchers derive more information from fMRI scans. According to Stein, the technology is helping researchers clarify the brain’s notoriously obscure structure-function relationships. He even describes how an improved understanding of these relationships could help clinicians detect early signs of neurodegeneration in individual patients.
Stein’s contribution appears in full on the GEN website. A representative excerpt is presented in a sidebar (“Mapping How the Brain Organizes Semantic Activity”) that accompanies this article. The excerpt describes how researchers at the University of California are using machine learning, a form of artificial intelligence, to visualize human brain activity.
According to Stein, such work demonstrates how clinicians may use functional imaging to guide early diagnostic, therapeutic, or prognostic decisions. For example, functional imaging could help clinicians improve the management of conditions such as autism spectrum disorder or neurodegenerative diseases.
“Functional imaging,” Stein notes, “would be especially valuable if it could help clinicians distinguish between conditions that would otherwise appear to be the same condition.” He adds that making such distinctions is often difficult in neuroscience, given that “behavior is a low-dimensional reflection of the high-dimensional brain
processes that produce it.” Extending neuroimaging with molecular probes
To generate functional images of the brain, scientists generally rely on fMRI, a noninvasive technique that tracks the magnetic signals that accompany changes in the oxygenation of hemoglobin. Essentially, hemoglobin is a natural (and convenient) contrast agent or probe of a chemical interaction that correlates with neural activity. What if other probes could be deployed, probes that would allow noninvasive neuroimaging to approach the specificity and resolution of optical neuroimaging?
This question drives researchers in the laboratory of Alan P. Jasanoff, PhD, a professor of biological […]
Do medicinal mushrooms really work? What you need to know about lion’s mane, reishi and more

Medicinal mushrooms are popular — but do they really work? Mushrooms have officially taken over the wellness space, and that extends well beyond the ones you find on your plate. Mushrooms are found in everything from coffee to smoothies to your medicine cabinet, and it’s looking like it’s just the start of the mushroom boom.
But not all mushrooms are created equal. Many of them have special (science-backed) properties that are seriously impressive. One of the most beneficial types of mushrooms are called functional mushrooms, which are pretty different from the button mushrooms you might add to a pasta dish (although those are good for you too). Editors’ top picks
“Functional mushrooms are mushrooms that have benefits that extend past nutritional benefits found in traditional mushrooms we are familiar with from cooking,” says Alana Kessler , a registered dietician. “Functional mushrooms can be taken via capsules, powders, liquids (teas) and sprays,” says Kessler.
With so many different types of mushrooms out there, how do you know which ones are best for you? And which ones are worth buying in a tincture or supplement versus just cooking and eating them? Keep reading for a complete overview of all of the healthiest mushrooms you can use — from the kind you can eat to those that have health benefits if you take them in a more concentrated supplemental form. Mushroom basics
You’ll find medicinal mushrooms in many forms, but one of the most common ways to supplement is with a mushroom powder or extract (more on that later). While many mushrooms are taken in supplements, powders or other forms, some medicinal mushrooms are also eaten in their whole form. “Mushrooms in general offer up great nutrition and are low in calories. They provide selenium, B vitamins, vitamin D and potassium — necessary for energy and absorption of nutrients, as well as beta glucans which are important for lowering inflammation and providing fiber, especially shiitake and maitake,” says Kessler. An overview of edible medicinal mushrooms
Maitake: “Can be sautéed, cooked into dishes, or eaten cooked on its own (not typically raw),” says Kessler. Maitake mushroom is an adaptogen , which means it can help the body adapt to stress and stay in balance. It also has potential anti-cancer benefits , in addition to helping improve cholesterol and type 2 diabetes .
Shiitake: “[Can be] cooked into any types of dishes, can be eaten raw, but typically cooked,” says Kessler. Shiitake mushrooms may help fight cancer and inflammation , and they contain beta glucans, which may help lower cholesterol .
Lion’s mane: ” Not typically eaten raw, and can be substituted in recipes as crab meat. [Helps] support mood health and memory,” says Kessler.
Oyster mushrooms : “Not typically eaten raw, can sauté, or use in stir fry,” says Kessler. Research has shown that oyster mushrooms contain antioxidants and may help decrease risk of certain diseases like cancer, heart disease, obesity and diabetes. Lion’s mane is known for helping improve focus and brain health. Functional medicinal mushrooms
While not an exhaustive list, the below types of mushrooms are some of the most common kinds that are sold and marketed today in supplements, extracts, powders and other products. Lion’s mane
Lion’s mane mushroom is best known for potential benefits for brain health . Some supplements and products that market lion’s mane claim that it can help boost focus and memory. Although there is not much human clinical research on lion’s mane, some animal studies have shown that it can help boost memory and may help prevent diseases that affect cognitive function like Alzheimer’s or Parkinson’s disease. Lion’s mane is high in antioxidants , which can help lower inflammation in the body. Reishi
Traditionally used in East Asian medicine , reishi is a type of mushroom that’s been used for many reasons and has a long list of potential health benefits. It’s currently being used to help cancer patients in China who need help strengthening their immune system after cancer treatments.
According to Kessler, reishi contains several polysaccharides that stimulate parts of the immune system. “[Reishi] helps the body fight viruses and bacteria by stimulating production of T-cells,” says Kessler. Reishi may also have benefits for fighting cancer as “the polysaccharides cause a significant increase in ‘natural killer’ cells, which destroys cancer cells, shrinks tumors and slows the spread of existing cancers,” says Kessler.
Reishi may also help reduce stress, decrease depression symptoms and help improve sleep, thanks to naturally occurring compounds called triterpenes . Chaga
“[Chaga] fungus grows in colder climates and is high in fiber. It is possible this is a reason that while it is beneficial for immune function and provides antioxidants, it is also used as a complementary treatment to heart disease and diabetes as it helps to lower blood sugar,” says Kessler. In addition to antioxidants and fiber, chaga also contains a variety of other nutrients like B vitamins, vitamin D, zinc, iron and calcium, among others. Turkey tail
Turkey tail is best known for its potential benefits for immune health and it’s been studied for treating cancer alongside other treatments.
“[Turkey tail] stimulates processes in the body which fights tumor growth and metastasis, including production of T-cells and ‘natural killer’ cells,” says Kessler. ” Studies have shown that polysaccharide-K (PSK, a compound in turkey tail) improved the survival rates of patients with gastric and colorectal cancers and showed promise in fighting leukemia and some lung cancers,” says Kessler. Cordyceps
Perhaps the most popular mushroom in the fitness crowd, Cordyceps is embraced by fitness enthusiasts and athletes alike for its ability to boost recovery and stamina . “Cordyceps boosts metabolism and stamina, and speeds recovery by increasing ATP, and improves how the body uses oxygen,” says Kessler. What to look for when buying mushroom products
Some mushroom supplements and products contain fillers and other ingredients you need to avoid in order to find the best quality product. “When purchasing a mushroom supplement, make sure starch is listed. Some supplements […]
6 Fresh produce foods you need to consume right away for a stress free lifestyle

Doctors and dietitians are learning more about how the nutritional properties of the foods we consume influence our mental health. There is a strong and significant connection between the brain and the stomach. When vital nutrients are insufficiently accessible, there is a direct impact on neurotransmitter activity and brain chemistry, which may increase anxiety induced behaviours. So, here are some fruits and vegetables which can help you to calm your anxiety and stress.
Avocado
Vitamin B6 aids in the production of many neurotransmitters, including serotonin, which affects mood. Avocados are high in stress-relieving B vitamins and heart-healthy fat, which can help to reduce anxiety. It has also been linked to memory, aids in the widening of blood vessels, and is needed for the production of red blood cells. Since vitamin E is fat-soluble, it can only be found in high-fat foods like nuts and avocados. Avocado slices can be added to omelettes, salads, and even smoothies to increase fibre and healthy fats in your diet.
Blueberries
When we are nervous or depressed, our bodies need vitamin C to repair and protect our cells and blueberries are high in vitamin C. These berries are rich in flavonoid antioxidants, which have anti-inflammatory and neuroprotective properties. They can aid in the reduction of stress-related inflammation and the prevention of stress-related cellular damage.
Broccoli
Cruciferous vegetables, such as broccoli are well known for their health benefits. A diet high in cruciferous vegetables can reduce your risk of certain cancers, heart disease, and mental health disorders such as depression. Broccoli is one of the most concentrated food sources of certain nutrients, such as magnesium, vitamin C, and folate, which have been shown to help with depressive symptoms.
Spinach
With its high magnesium content, this dark leafy green aids in the relief of headaches and fatigue, further compounding the physical effects of stress on the body. Spinach, like other leafy green vegetables, is high in folate, a nutrient that helps the body regulate mood. You can also benefit from natural stress-fighting powers by including more salads and vegetables in your diet and taking a cup of spinach (about 225 grams).
Swiss chard
Swiss chard is a leafy green vegetable that is high in anti-stress nutrients. Low levels of this mineral have been linked with conditions such as anxiety and panic attacks. Plus, chronic stress can deplete your body’s magnesium stores, making this mineral particularly important when you’re stressed. One cup (175 grams) of cooked Swiss chard provides 36 per cent of the daily magnesium intake, which is essential for your body’s stress response.
Oranges
Oranges are thought to be a perfect way to relax and reduce stress because they are high in vitamin C. This important nutrient helps reduce levels of the stress hormone cortisol, which can cause havoc in the body, in addition to promoting immune function, which can be compromised by stress.
About the Author: Dietitian Vidhi Chawla specializes in the field of Diet and Nutrition. She owns a private practice by the name of Fisico Diet Clinic.
You may like these
The science of why the sun makes us feel so happy

Step outside and what is the first thing that you notice? Maybe it’s the reuniting of friends and family sat chatting happily in the park, or the cheery chirping of the birds. But one thing that everyone seems to have in common when the sun’s out is a good mood.
The recent warm weather and sunny spells have conveniently coincided with the gentle easing of lockdown restrictions, and the latest bank holiday weekend. After months of being stuck inside our homes during one of the bleakest winters on record, and the shocking we weather in May, this mini heatwave is just what the doctor ordered.
But what is it about the sunshine that makes us feel so happy? Here is the science behind why those rays are so good for us. It boosts our mood
Most of us will agree that it’s hard to feel unhappy in the sun. This is down to the link between sunlight and our serotonin levels – the hormone that makes us feel happy. It’s also why people are more likely to develop Seasonal Affective Disorder (SAD) when the shorter autumn days arrive and we creep into winter with fewer daylight hours.
There is plenty of research to back up this idea. One study undertaken in Australia found that people had higher levels of serotonin on bright sunny days than cloudy ones. Increased levels of this hormone generally lead to greater feelings of satisfaction and calmness and lower levels of depression and anxiety.
There is even research to show that people who use tanning beds may experience more frequent feelings of euphoria, which could explain why people develop a dependence on regular sessions. Although the connection isn’t entirely established yet, researchers speculate this could be down to the way UV light forces melanocytes, the cells that produce dark pigment in skin, to release endorphins. However, most experts also agree that the increased sun cancer risk negates the feel good factor. Sun improves our sleep
Regular exposure to sunlight encourages the production of melatonin – the hormone which helps to regulate the body’s sleep-wake cycle. This encourages feelings of drowsiness, allowing us to drift off easier at night, which leads to us feeling happier in the day. Melatonin also helps to regulate our circadian rhythm – the body’s internal clock that signals when to be alert and when to rest – which can be thrown out of sync by exposure to blue light from technology, disrupted work patterns and light pollution.
In turn, this allows us to feel happier. Research shows that our amygdala – the emotional part of the brain – is significantly more reactive after a bad night’s sleep, meaning we are more likely to feel cranky throughout the day if we have spent the night tossing and turning. Time spent in the sun can help us sleep soundly. Our sex drive is given a lift
Believe it or not, even our sex drive is affected by time spent in the sun, so a spring heatwave is good news for those who have found their libido dampened somewhat in lockdown. Researchers at Medical University of Graz in Austria found that spending just one hour in the sun can boost a man’s testosterone levels by 69 per cent. In turn, this helps to balance mood, sex drive and cognitive function. The experts put this down to the role of vitamin D, which is produced after exposure to sunlight .
It’s the same situation for women. Researchers in China, who conducted a study on post-menopausal women, identified a link between low levels of vitamin D and low levels of oestrogen, the female sex hormone. Your bones will be given a boost
Vitamin D is also crucial for helping our body to absorb calcium, which is responsible for strengthening your bones. A lack of vitamin D has been associated with both osteoporosis, rickets and autoimmune diseases, such as rheumatoid arthritis (RA).
A review by the Cochrane Library found that the rates of falls in elderly people – which are partly down to the effects of brittle bones – could be cut by more than a quarter if the elderly were given supplements of vitamin D. However, in recent years many studies have questioned how effective supplements are in reducing rates of osteoporosis.
That’s not to say that sunlight can’t help though: more than 90 per cent of a person’s vitamin D requirement tends to come from casual exposure to sunlight, making it the best source of the nutrient. So how much exposure do we need to boost our health? On average, experts believe we should be aiming for 10–30 minutes of midday sunlight, several times per week. So make sure you head outside for a walk today to get a boost of bone-strengthening vitamin D. It improves midlife brain health
While most of the research around sunlight and the brain has focused on serotonin levels, a dose of vitamin D could also be good for our intellect. In 2009, scientists from the University of Manchester found that higher levels of vitamin D are linked with improved mental ability in middle-aged and older men. Men in the study were tested for memory and speed recollection, as well as for mood and physical activity levels, before their blood samples were taken. The researchers found that men with higher levels of vitamin D performed consistently better than those with lower levels. Your eyes need sunlight
Dr Rangan Chatterjee, GP and author of Feel Great, Lose Weight , explains that light is measured in a unit called lux: if we spend 20 minutes outside – even on a cloudy overcast day – we are exposed to around 10,000 lux, compared with 500 lux if we spend time indoors. This is particularly important for children. Researchers at King’s College London, the London School of Hygiene and Tropical Medicine, found that regular exposure to sunlight lowered the risk of nearsightedness – or myopia – in children and young adults by helping the eye produce dopamine, […]
How taking fish oil may help fight inflammation and improve mental health

The benefits of fish oil come mainly from its ability to reduce inflammation in your body.
This makes it ideal for boosting heart health, especially for people with preexisting heart issues.
Fish oil may also help fight off depression because it can increase serotonin levels.
Fish oil is a natural oil found in fatty fish like salmon, herring, and sardines. But you can also take it as a supplement.
The majority of health benefits in fish oil comes from the omega-3 fatty acids it contains, which help support the heart, brain, and general wellbeing.
Here’s what researchers have found so far on the health benefits of consuming fish oil regularly. 1. Helps fight inflammation
Fish is one of the best providers of omega-3 fatty acids – a category of fats that you might be lacking in your diet.
“Americans typically have a much higher intake of omega-6 fats which are prevalent in refined vegetable oils from soybeans, corn and sunflower seeds,” says Julie Stefanski, a registered dietitian nutritionist and spokesperson for the Academy of Nutrition & Dietetics .
Omega-6 acids aren’t necessarily bad for you, but the ratio of omega-3 fats to omega-6 fats is important for your health. Having enough omega-6 fats but too little omega-3 fats can put you at risk for chronic inflammation , Stefanski says.
Fighting chronic inflammation is vital, since inflammation can increase your risk of diseases like cancer, arthritis, and heart disease. 2. Supports heart health
Taking fish oil may help boost heart health, especially for people already suffering from heart problems .
A 2017 review found that taking fish oil supplements can help prevent heart attacks in people with coronary artery disease . The researchers also found that regularly consuming fish oil reduced the risk of hospitalization in people with heart failure – however, they say more research is needed to confirm these results.
This may be partly due to the anti-inflammatory effects of fish oil. “Reducing inflammation is a key factor in reducing risk of cardiovascular disease,” Stefanski says.
To get heart health benefits, the American Heart Association recommends eating two servings of fatty fish like salmon per week. One serving is ¾ cup or 3.5 ounces of cooked fish. 3. May improve brain function
Your brain uses the omega-3 fats in fish oil, among other nutrients, to build brain cells, which is especially important as you age.
For example, studies have shown that people with degenerative neurological disorders often have low levels of DHA (docosahexaenoic acid) – a type of omega-3 fatty acid.
That might explain why a 2010 study found that older adults who took 900 mg of DHA supplements daily for six months performed better on memory and learning tests than those without any treatment. 4. May help improve mental health
Depression has been linked to higher levels of inflammation, therefore fish oil’s anti-inflammatory properties may help fight off mental health issues like depression.
A 2016 review of 13 studies found that taking omega-3 supplements helps to improve depression symptoms like sadness and fatigue by reducing inflammation in your brain cells.
EPA fatty acids, one of the main acids in fish oil, are especially helpful for depression because they increase your levels of serotonin , an important mood-boosting chemical. So it may be best to look for fish oil supplements with a “high EPA” label.
The review also found that omega-3 supplements work especially well when combined with antidepressants . 5. Supports fetus development during pregnancy
Fish oil provides nutrients that are essential for the development of the baby and the health of the parent, Stefanski says.
Studies show that taking daily fish oil supplements with at least 300 mg of DHA during pregnancy can help a baby’s healthy development by: Supporting vision development
Improving the development of brain functions
Lowering the risk of allergies
But it’s important to know that some fish contain relatively high levels of mercury, which can damage a fetus’s developing brain and nervous system . This is why experts recommend avoiding large fish like swordfish, king mackerel, and shark. Smaller fish like salmon, light tuna, and sardines tend to have a lower risk.”Some women who are concerned about mercury levels in fish may choose to avoid fish during pregnancy and turn to supplements,” Stefanski says. If you decide to use supplements, look for products that conduct third-party testing for mercury content, Stefanski says, as this can provide a more accurate measure of mercury levels. Insider’s takeaway Fish oil can have a variety of health benefits thanks to its rich supply of omega-3 fatty acids. Adding fish to your diet or taking daily supplements may help improve your heart and brain health, as well as support a healthy pregnancy.You can get fish oil in your diet by eating fish every week or by taking daily supplements.4 benefits of eating acai, from regulating blood sugar to helping digestion 15 delicious low-calorie foods that are filling and can help you lose weight Why anti-inflammatory diets are great for overall health and a 7-day meal plan to get started How to use apple cider vinegar to help you lose weight, according to dietitians
6 Soothing herbal teas you can drink to relieve stress and anxiety during the pandemic

There is no denying that the lockdown and other measures, such as social distancing, implemented to help curb the spread of the coronavirus infection have had an impact on almost every aspect of our lives.
The global pandemic has brought in many changes in our lifestyle. There is no doubt that stress is a very common problem that almost everyone is facing during the pandemic and it has become problematic to balance work and personal life.
On such days, sipping a warm cup of herbal tea could induce a calming practice as there is evidence that certain herbal teas have stress-relieving properties. Hence, here are a few herbal teas that can help you relax in a global pandemic.
Chamomile tea
Excessive stress and anxiety can trigger sleeplessness. Chamomile tea not only alleviates stress and anxiety but also aids in the treatment of insomnia. Chamomile tea is the third most common after green tea and peppermint tea. The Chamomile flower is used as a remedy to treat a variety of health issues. Long-term use of chamomile extracts decreases moderate to severe symptoms of a generalised anxiety disorder (GAD), enhances sleep quality, relieves anxiety and depression, prevents bone loss, and boosts immune health.
Hibiscus tea
Hibiscus tea is a herbal tea produced by steeping hibiscus plant parts in boiling water. Hibiscus Tea has a tart taste similar to cranberries and is known to keep the liver healthy, avoid hypertension, and lower blood pressure. Hibiscus tea relaxes high-stress levels and strengthens the immune system with vital doses of Vitamin C since it is high in flavonoids.
Holy basil tea
Tulsi is a well-known herb. Tulsi leaves have antidepressant properties, which help to normalise psychological stress. They have been used to treat a variety of ailments, including diabetes, headaches, upset stomachs, and earaches. Tulsi leaves have a delicate and refreshing flavour and are used as a home remedy for cough and cold symptoms.
Peppermint tea
This aromatic tea works well to alleviate stress and anxiety. Peppermint contains menthol, which is a natural muscle relaxant. When you are stressed or anxious, you become tense and irritable. Drinking peppermint tea will help you stay calm. Peppermint tea is an excellent tea to drink before going to bed because of its relaxing effect and lack of caffeine. It will allow you to sleep peacefully, which is exactly what you need after a long day.
Lavender tea
While lavender is commonly used to relieve anxiety and stress, it also has calming properties. Lavender tea, made from the dried buds of the lavender plant, helps to relax muscles and nerves, relieving stress and tension while also preventing headaches and muscle pain. It is also good for the digestive system and acts as a natural anti-inflammatory, reducing the negative effects of stress on your body.
Green tea
Green tea, which is high in antioxidants, is often associated with physical health, but it is also beneficial to mental health. Out of one of the many antioxidants, it contains epicatechin, which is a flavonoid that helps to protect your brain from oxidative damage as well as combating the negative effects of stress on your body and improving memory. Green tea is also a good source of L-theanine, which has shown to improve stress relief, fatigue reduction, and better sleep.
About the Author: Dietitian Vidhi Chawla specializes in the field of Diet and Nutrition. She owns a private practice by the name of Fisico Diet Clinic.
Also Read: Oil Pulling: Miracle or Myth? Here is everything you need to know about it
You may like these
The expectant brain: adapting for motherhood
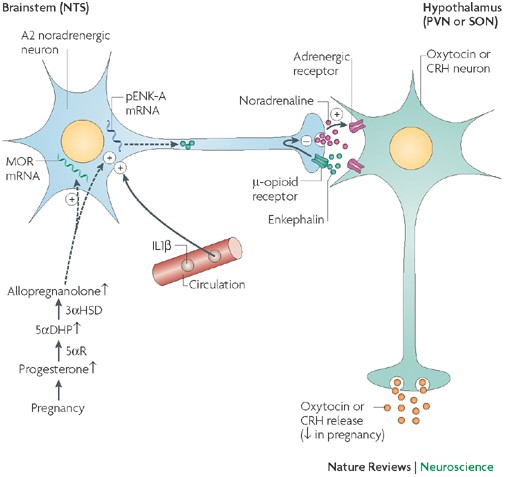
Key Points
The expectant brain undergoes many changes to maximize the likelihood of a successful outcome of the pregnancy. These adaptations are driven by pregnancy hormones and ensure adequate nutrient supply to the fetus, protection from maternal stress hormones, appropriate organization of parturition and the delivery of maternal care.
Exposure to stress or glucocorticoids during pregnancy can adversely programme the fetuses, making them more susceptible to disease in adulthood. One protective mechanism against this effect involves endogenous-opioid inhibition of the mother’s responses to stress in pregnancy, which reduces the exposure of the fetus to maternal glucocorticoids.
Increased food intake in pregnancy is permitted by the resetting of central appetite control mechanisms, for example, the emergence of central leptin resistance. This resetting ensures sufficient nutrients for the fetus(es), extra energy for the mother, and a surplus of energy for storage as fat in preparation for lactation.
Inhibitory-opioid mechanisms prevent the premature activation of oxytocin neurons (and hence preterm birth) and aid the accumulation of neurohypophysial oxytocin stores. Allopregnanolone, a neuroactive metabolite of progesterone, restrains oxytocin neurons by enhancing the effectiveness of GABA synapses, but also induces opioid inhibition.
Dopamine neurons in the hypothalamus inhibit prolactin secretion. Before term, the stimulatory action of prolactin on these neurons is switched off, permitting increased prolactin secretion for the stimulation of lactation and maternal behaviour.
Maternal behaviour emerges rapidly after birth. This depends on ‘priming’ of the neural circuitry that organizes the components of maternal behaviour and the motivation to perform it. Priming involves the action of oestrogen, progesterone and lactogens, particularly in the medial preoptic area.
The offspring are protected from harm by a marked increase in maternal aggressiveness soon after birth. This element of maternal behaviour involves multiple neurochemical changes, in particular, increased oxytocin release and decreased activity of serotonin neurons.
In humans, withdrawal of the hormones of pregnancy might predispose women to the ‘blues’ soon after birth, and in vulnerable women might later trigger major puerperal depression.
Abstract
A successful pregnancy requires multiple adaptations of the mother’s physiology to optimize fetal growth and development, to protect the fetus from adverse programming, to provide impetus for timely parturition and to ensure that adequate maternal care is provided after parturition. Many of these adaptations are organized by the mother’s brain, predominantly through changes in neuroendocrine systems, and these changes are primarily driven by the hormones of pregnancy. By contrast, adaptations in the mother’s brain during lactation are maintained by external stimuli from the young. The changes in pregnancy are not necessarily innocuous: they may predispose the mother to post-partum mood disorders. Author information
Affiliations
> Laboratory of Neuroendocrinology, Centre for Integrative Physiology, University of Edinburgh, Hugh Robson Building, George Square, Edinburgh, EH8 9XD, Scotland, UK.
Corresponding author
Correspondence to John A. Russell . Glossary
A category of stressor (including infection and injury) that poses a real threat to homeostasis or survival and automatically activates the HPA axis. Cholecystokinin (CCK). A peptide hormone from the gastrointestinal tract that stimulates digestion and signals satiety to the brain. Interleukin-1β (IL1β). A pro-inflammatory cytokine that is produced by macrophage cells in response to infection. Endogenous opioids Peptides, including dynorphins, endomorphins, endorphins and enkephalins, that are produced naturally in the body and, like morphine, act through opioid receptors. Neuroactive steroid A steroid derivative that rapidly alters neuronal excitability through interaction with neurotransmitter-gated ion channels. Allosteric modulator A molecule that binds to a receptor at a regulatory site that is distinct from the active ligand-binding site to influence the receptor’s function. Endocannabinoid A signalling molecule that is structurally related to tetrahydrocannabinol (the main active substance found in cannabis). Endocannabinoids released by neurons act through cannabinoid receptors to modulate synaptic input. Lactogen A peptide hormone that stimulates milk production (for example, prolactin and placental lactogen). Mitral cell A type of neuron that is located in the olfactory system and that processes and transmits information from primary olfactory sensory neurons to other brain regions. Transcriptome The set of all mRNAs produced in a cell or a population of cells. About this article
Cite this article
Brunton, P., Russell, J. The expectant brain: adapting for motherhood. Nat Rev Neurosci 9, 11–25 (2008). https://doi.org/10.1038/nrn2280
The why behind the high: determinants of neurocognition during acute cannabis exposure
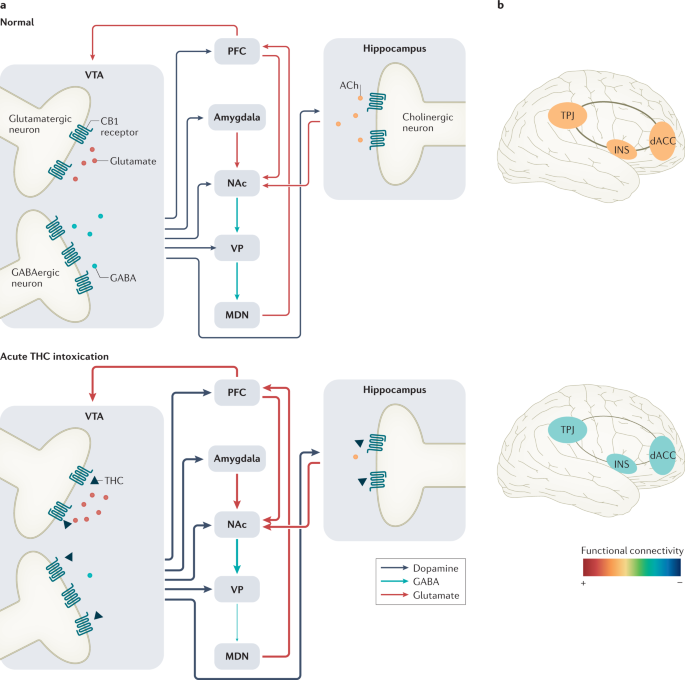
Abstract
Acute cannabis intoxication may induce neurocognitive impairment and is a possible cause of human error, injury and psychological distress. One of the major concerns raised about increasing cannabis legalization and the therapeutic use of cannabis is that it will increase cannabis‐related harm. However, the impairing effect of cannabis during intoxication varies among individuals and may not occur in all users. There is evidence that the neurocognitive response to acute cannabis exposure is driven by changes in the activity of the mesocorticolimbic and salience networks, can be exacerbated or mitigated by biological and pharmacological factors, varies with product formulations and frequency of use and can differ between recreational and therapeutic use. It is argued that these determinants of the cannabis-induced neurocognitive state should be taken into account when defining and evaluating levels of cannabis impairment in the legal arena, when prescribing cannabis in therapeutic settings and when informing society about the safe and responsible use of cannabis. Author information
Contributions
The authors contributed equally to all aspects of the article. Corresponding author
Additional information
Peer review information
Nature Reviews Neuroscience thanks S. Bhattacharyya (who co-reviewed with C. Davies), Z. Cooper, W. Hall and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Glossary
Compounds found in cannabis or that are synthetically produced to mimic naturally occurring cannabinoids. Psychomotor deficits Psychotomimetic effects Endocannabinoids Xenon-enhanced computed tomography A neuroimaging method in which the subject inhales xenon gas to assess changes in cerebral blood flow. Positron emission tomography A magnetic resonance imaging technique that uses radioactive substances known as radiotracers to visualize and measure changes in metabolic processes, and in other physiological activities such as receptor occupancy. Arterial spin labelling A non-invasive magnetic resonance imaging technique that uses arterial water as an endogenous tracer to measure cerebral blood flow. Functional connectivity A measure of similarity or correlation between brain signals arising from anatomically separated brain regions that indicates that the regions are functionally connected. Executive network A frontoparietal brain network involved in sustained attention, complex problem-solving and working memory. Magnetic resonance spectroscopy A non-invasive proton imaging technique that allows for the quantitative assessment of regional brain biochemistry. Functional magnetic resonance imaging A non-invasive technique for measuring and mapping brain activity based on changes in blood oxygen level-dependent signals that indicate underlying neural activity. A brain network primarily consisting of the medial prefrontal cortex, the posterior cingulate cortex and the angular gyrus that is active when a person is focused on internal mental state processes and the brain is at wakeful rest. Inhibitory control A cognitive process that permits an individual to inhibit their impulses in order to select a more appropriate goal-directed response. Single-nucleotide polymorphisms Common genetic variations occurring when a single nucleotide at a single position in the genome differs among people. A disorder arising from repeated or continuous substance use characterized by preoccupation with and impaired control over substance use, as well as physiological features such as tolerance and withdrawal. Pharmacokinetics The disposition of a drug within the body over a period of time as characterized by the four main phases of absorption, distribution, metabolism and elimination. Field sobriety tests Tests of balance, coordination and divided attention that are performed by the police to determine whether a driver is impaired. About this article
Ramaekers, J.G., Mason, N.L., Kloft, L. et al. The why behind the high: determinants of neurocognition during acute cannabis exposure. Nat Rev Neurosci (2021). https://doi.org/10.1038/s41583-021-00466-4
Study explains how diet, exercise and the endocannabinoid system contribute to healthy aging

( Natural News ) Researchers define the human endocannabinoid system (ECS) as a complex cell-signaling system that plays an important role in the development of the central nervous system (CNS), synaptic plasticity — a characteristic of neurons in the brain — and the body’s response to internal and external insults or stressors.
The ECS, whose components are widely distributed throughout the body, consists of cannabinoid receptors, endocannabinoids and the enzymes responsible for producing endocannabinoids. Besides regulating nerve function, this system is actively involved in many bodily processes , such as appetite regulation, digestion, immune responses (including inflammation), learning and memory, motor control, muscle formation, bone remodeling, sleep and metabolism.
In a recent study, Bruce Watkins, a researcher at the University of California, Davis (UC Davis), discusses the potentially huge role the ECS plays in healthy aging . Watkins believes it may have something to do with the ECS’s involvement in systemic energy metabolism, inflammation, pain and brain biology. He also proposes that a healthy diet and regular exercise benefit health in many ways due to their influence on the ECS. He explains all of these in detail in an article published in the journal Nutrition Research . The endocannabinoid system, health and aging
According to Watkins, diet is a major factor that influences health and aging. Inflammation, which is regulated by the ECS through endocannabinoids , is triggered not just by infections or injury, but also by oxidative stress. This event has been linked by numerous studies to premature aging .
Oxidative stress is caused by an imbalance between free radicals and antioxidants in the body. Antioxidants are not just produced endogenously, but they can also be obtained from external sources, particularly from plant-based foods like fruits and vegetables. Watkins and many other researchers suggest that eating a healthy, antioxidant-rich diet prevents oxidative stress from harming cells and causing functional losses associated with aging. (Related: Nutrition is CRUCIAL to healthy aging .)
In a study published in the American Journal of Epidemiology , a team of American researchers presented evidence of a healthy diet’s anti-aging benefits by examining the effects of four antioxidant and anti-inflammatory diets on telomere length . Telomeres refer to the repetitive sequences found at the end of human chromosomes that protect them from damage. Researchers have long discovered that the shortening of telomeres is responsible for the aging-related degeneration of cells .
The researchers found that people who eat antioxidant-rich, anti-inflammatory diets that emphasize plant-based foods and limit consumption of meat and sugary foods have longer telomeres than people who don’t . The researchers believe that this can be explained by the fact that healthy diets create a biochemical environment that’s favorable to telomeres. Since longer telomere length is also linked to a reduced risk of major chronic disease, eating antioxidant-rich, anti-inflammatory diets may be the key to good health and healthy aging.
Watkin’s definition of healthy aging includes freedom from disease, the ability to engage in physical activity and the maintenance of cognitive skills. All of these require the involvement of the ECS. According to Watkins, one of the reasons exercise is linked to good overall health and well-being is because it induces endocannabinoid production in the brain . By activating the ECS, exercise reduces pain sensations and alters emotional and cognitive processes in a positive way.
The muscles, skin, lungs and endothelial cells — the cells that line blood vessels — are home to cannabinoid receptors, so it’s not impossible for the ECS to mediate physiological responses to exercise. According to a study published in the British Journal of Sports Medicine , moderate-intensity exercise dramatically increases blood plasma levels of the endocannabinoid anandamide . Anandamide binds to cannabinoid 1 (CB1) receptors and is said to suppress pain initiation , induce calming effects, reduce stress and anxiety, and elevate mood . All of these contribute to a heightened sense of well-being often felt after a good exercise.
While there is much to learn about the functions of the ECS, Watkins is hopeful that future studies will uncover key relationships that will improve the current understanding of the ECS and its influence on human health .
Sources include:
NCBI.NLM.NIH.gov 1
NCBI.NLM.NIH.gov 2
Genome.gov
PNAS.org 1
PNAS.org 2
Academic.OUP.com
BJSM.BMJ.com
Nature.com 1
Nature.com 2
New Alzheimer’s treatment using ultrasound yields 75% success rate, restoring complete memory function in trial run

( Natural News ) A new Alzheimer’s treatment called focused therapeutic ultrasound beams sound waves into brain tissue and stimulates the brain’s waste removal system, safely enabling a clearance of the plaques, clumps and tangles that block memories. This non-invasive technology uses sound waves to safely open the blood-brain barrier where your ‘janitorial’ microglial cells can sweep out the garbage for a few hours, including beta-amyloid clumps (sticky proteins) and neurofibrillary tangles (that clog neurons), the two most common lesions in the brain that build up over time, blocking memories while leading to strokes and dementia.
A team at the Queensland Brain Institute in Australia was successful in treating 75 mice with focused therapeutic ultrasound, with astonishing 75 percent success rate at restoring memory. With no damage done to surrounding brain tissue, the ultrasound beams loosened the plaque, clumps and tangles enough for a few hours that the microglial cells were able to do their job again, clearing the ‘trash’ out of the memory ‘hallways.’ After that, nutrients are able to flow to these parts of the brain that were clogged and riddled with plaques. Ultrasound proves successful in three memory and performance tasks for mice
Did you know that, on average, the protein-coding regions of the mouse and human genomes are 85 percent identical? That’s why humans should pay CLOSE attention to studies that scientists run on mice.
Mice were put through tests with mazes, new objects, and ‘places to avoid.’ Three out of every four mice that were treated with sound waves were able to navigate better through the maze, recognize there were new objects in the pathways, and remember the places to avoid that they had experienced before.
The research is published in Science Translational Medicine and should fundamentally change the way dementia is being treated from here on out. Sheep trials are next, then humans.
It’s important to know what causes Alzheimer’s, too. We can’t just rely on new technologies to save us all after we pollute our brain and blood with toxins for years and years. Here are the main ‘evil four’ blood vessel clogging culprits to watch out for:
#1. Canola oil – even organic canola coagulates in the body and blood, causing blockages and less blood/nutrients/oxygen to flow. Most other processed oils coagulate eventually, so avoid them when you can.
#2. Heavy metal toxins – consider all the heavy metal toxins we ingest, via mercury and aluminum in vaccines, aluminum in most antacids, and aluminum pots and pans (and foil) that people use to cook. Ever heard of “Mad Hatter Syndrome” from mercury overload?
#3. Saturated animal fat – Yes, meat, eggs, cheese and just about everything dairy – that’s the health downfall of over 250 million Americans who eat them with every meal, causing inflammation, clogging of blood vessels, and eventually, heart attacks, strokes and dementia. It’s the same fat that clogs the veins and capillaries in your brain. The same fat causes strokes. They’re the same saturated fat deposits on the walls of your blood vessels. Plant based diets help prevent this, and according to this new research out of Australia, non-invasive, non-pharmaceutical ultrasound treatment can help clear it all out.
#4. Margarine – Oh, deadly margarine. It is not a substitute for butter. It’s a substitute for sanity, as it clogs arteries with its unhealthy combination of trans fats and saturated fats. You’ll find it in millions of American products, like baked goods, muffins, cakes, pastries, and doughnuts (often also called vegetable shortening). It’s super cheap because it makes Big Pharma a fortune when you eat it. It has a longer shelf life than butter, as it shortens human life by causing dementia and strokes. Covid-19 mRNA vaccines now proven to cause your body to create the plaques, proteins and prions that cause dementia
We have to avoid building up all these plaques. Yet, to the contrary, the Covid vaccines are designed so that the human body now creates millions of proteins ( plaques and prions ) that may soon CAUSE dementia for those victims who get the whole series of dirty jabs for the lab-made China virus.
Tune your internet frequency to NaturalCures.news for updates on how to prepare and take care of your body and mind with natural cures, superfoods, supplements and whole organic food.
Sources for this article include:
Food for the brain: Review examines the link between diet and mental health

( Natural News ) A review published in the journal European Neuropsychopharmacology shows that a person’s diet can improve or worsen his mental health, depending on the quality of the foods that he eats. European researchers arrived at this conclusion after reviewing past studies that examined the potential link between nutrition and mental health .
The researchers found strong evidence that the Mediterranean diet, which is a diet rich in fruits, vegetables and olive oil, exerts a protective effect against depression. Other studies also suggest that following a ketogenic diet , which is high in fat and low in carbohydrates, could reduce the frequency of seizures in children with epilepsy.
A poor diet, on the other hand, is associated with mood disorders, such as depression and bipolar disorder. Meanwhile, vitamin B12 deficiency has been linked to fatigue, memory problems and the development of depression . According to the review, taking vitamin B12 supplements could improve mental health in people with vitamin B12 deficiency.
Moreover, a few studies also found that consuming too much refined sugar during pregnancy could increase children’s risk of developing hyperactivity and attention deficit hyperactivity disorder (ADHD). Eating more fresh fruits and vegetables, on the other hand, could protect children from these conditions.
The researchers concluded that while the link between mental health and certain foods is comparatively weak, there is adequate evidence to support a direct association between a person’s overall diet and mental health . How your diet impacts your mental health
What you eat affects how you feel because your mental and digestive health are closely linked . To start with, ninety-five percent of your serotonin – a neurotransmitter that plays a role in mediating mood – is produced in your digestive tract, which is lined with millions of neurons.
Good gut bacteria influence the function of those neurons, as well as your production of serotonin and other neurotransmitters. They are considered good bacteria because they play an important role in your health. For starters, they protect the lining of your intestines, reduce inflammation and improve how well your body absorbs nutrients from food. In addition, they also activate neural pathways that travel directly between your gut and brain. (Related: Many mental illnesses are inflammation based: More and more science backs up a link between gut health and mental health .)
Given the digestive system’s role in mental health, it shouldn’t come as a surprise that your diet also influences your mood. Indeed, studies show that people who follow the Mediterranean diet and other “traditional” diets have up to a 35 percent lower risk of developing depression than those who follow a typical Western diet.
Researchers attribute this difference to the fact that traditional diets include more vegetables, fruits, unprocessed grains and seafood, and only modest amounts of lean meat and dairy. Traditional diets are also devoid of processed foods and refined sugars, which are staples of a Western diet. In addition, many of the unprocessed foods in traditional diets are fermented, meaning they are rich in live beneficial microorganisms called probiotics. Best brain foods to improve your mental health
Check out the following foods to improve your mental health : Oily fish – Salmon , mackerel and sardines are rich in healthy omega-3 fatty acids. Studies suggest that an omega-3 deficiency can increase your risk of developing depression.
Probiotic foods – Fermented foods like kombucha and sauerkraut contain probiotics, which promote good gut health.
Whole grains – Whole grains are excellent sources of B vitamins such as vitamin B12 , which is important for brain health.
Leafy greens – Green leafy vegetables like spinach are chock-full of folate, another B vitamin. Research shows that people with depression tend to have low levels of folate.
Your diet can improve your mental well-being or increase your risk of mental disorders. Adopt a healthy diet rich in fresh fruits, vegetables and whole grains for better mental health.
BrainHealthBoost.com has more tips on how to improve your brain health.
Sources include:
VeryWellMind.com
Gearing Up for Down’s Syndrome Clinical Trials

Part 2 of two
For years, researchers have been paving the way for Down’s syndrome treatment studies by carrying out longitudinal observation studies. These have identified imaging, fluid biomarker, and cognitive measures that could serve as selection or outcome measures. In parallel, clinicians have identified people with Down’s who are willing to take part in trials. Hundreds are expected to join trial-ready cohorts this year. Encouraged by the completion of AC Immune’s Phase 1 trial of an anti-amyloid vaccine in people with Down’s (see Part 1 ), researchers hope to test several other anti-amyloid treatments in these cohorts within the next few years.
“It is truly amazing how much work has happened in the last five years,” Michael Rafii, University of Southern California, Los Angeles, told Alzforum. Juan Fortea, Hospital of Sant Pau, Barcelona, Spain, agreed. “It is a very exciting time for DS research, which benefits from a dramatic increase in attention and funding,” he wrote.
Natural History Studies
Efforts to characterize clinical and biomarker changes during AD progression in people with DS have gained momentum ( Rafii et al., 2021 ). At present, at least nine cohorts in six countries are collecting biomarker data (see sidebar). Six cohorts in the EU are part of the European Horizon 21 Consortium, which tracks AD biomarkers and cognitive changes in more than 1,000 Down’s syndrome volunteers. In the U.S., The Alzheimer’s Disease in Down Syndrome (ADDS) and Neurodegeneration in Aging Down Syndrome (NiAD) cohorts recently merged to create the National Institute on Aging’s Alzheimer’s Biomarkers Consortium–Down Syndrome (ABC-DS) ( Handen et al., 2020 ). In this cohort, scientists have collected imaging, fluid, and cognitive biomarkers from more than 400 people with DS age 25 and older. “The planned enrollment is just over 700, and there is a particular focus on increasing diversity,” Laurie Ryan, NIA, Bethesda, Maryland, told Alzforum. The scientists will compare how AD biomarkers change in DS relative to sporadic AD, search for genes that modify AD risk in DS, and apply what they learn to precision medicine approaches and clinical trials.
Also in the U.S., the LIFE-DSR natural history study aims to follow 270 people with DS aged 25 and older for 32 months, measuring plasma AD biomarkers, cognition, and behavior. It recruits using the U.S. Down Syndrome Clinical Trials Network (DS-CTN), which includes 11 clinic sites in nine states.
Biomarkers: Similar in Alzheimer’s and Down’s
What have researchers learned so far about how biomarkers change in Down’s?
Markers begin shifting in a similar way, but at a much earlier age than in AD. In one cross-sectional study, Fortea and colleagues correlated memory, imaging, and fluid biomarker measures with age in 388 people with DS from the DABNI and DiDS cohorts ( Fortea et al., 2020 ). They found that cerebrospinal fluid Aβ42/40 ratios fell and plasma neurofilament light (NfL) concentrations crept up in people’s 20s. Amyloid PET ligand uptake and CSF phospho-tau181 (p-tau181) began rising, while brain glucose metabolism started waning, by the 30s. The hippocampus atrophied and memory declined in people’s 40s. All this culminated in an AD diagnosis at an average age of 54.
In short, Fortea found almost identical AD biomarker trajectories in DS as did researchers led by Randall Bateman, Washington University, St. Louis, in autosomal-dominant AD (see image below and Bateman et al., 2012 ). “There is nothing to suggest that AD is categorically different in DS than in the general population,” Bradley Christian, University of Wisconsin, Madison, told Alzforum.
Likewise, researchers led by Dominic Walsh, then at Harvard Medical School, saw plasma Aβ42 fall, NfL rise, and the N-terminal tau fragment NT1 fall, then rise, in people with DS as they aged. Change was fastest in the 20s to 40s ( Mengel et al., 2020 ). Striking Similarity . Biomarkers and memory decline track similarly in familial AD (left) and DS (right). Most begin to change 15 to 20 years before age of symptom onset (dashed vertical line). For CDR-SOB and Cambridge Cognitive Examination – Down Syndrome ( CAMCOG-DS), higher and lower scores, respectively, indicate worsening. CAMCOG-DS measures seven cognitive domains: orientation, language understanding and production, memory, attention, praxis, abstraction, and visual construction. [Courtesy of Bateman et al., NEJM, 2012 (left) , and Fortea et al., Lancet, 2020 . ]
Tracking Plaques and Tangles
How can this biomarker information be used in clinical trials of DS?
In the case of Aβ, the data suggest it might help select the right candidates for trials. Christian and colleagues grouped people from the ABC-DS cohort by how fast their PET amyloid load changed ( Zammit et al., 2021 ). Three groups emerged: “Aβ-negatives,” “Aβ-positives,” and a group deemed “converters” (see image below). Negatives had a low plaque load at baseline, which grew slowly. Positives had a high baseline plaque load, which grew quickly. Converters had a negative scan at baseline but accumulated plaques as fast as did positives. All About Speed. People with DS, grouped by how fast plaques deposit in their brains over two to four measurement time points. [Courtesy of Zammit et al., NeuroImage, 2021.] Christian proposed that lowering the amyloid-positivity threshold might catch some of the converters, and thus identify a group of people with DS who are at the earliest point of amyloid accumulation, irrespective of their age. He believes this might be a good group to test in trials of anti-amyloid therapies.
Similarly, scientists led by Ira Lott, University of California, Irvine, have identified a pattern of plaque accumulation that might indicate imminent dementia in DS. They took five PET scans over four years in 19 DS adults 40 years old or older without dementia at baseline. In five volunteers who developed dementia during the study, plaques built up in the same brain regions that typically accumulate amyloid in AD, including the inferior parietal cortex and temporal lobes. Buildup in the prefrontal and superior frontal cortices and posterior cingulate best predicted transition to dementia ( Keator et al., 2020 ).
Focusing on change in specific regions of the brain might offer a […]
The benefits of omega-3 fatty acid supplementation for men

( Natural News ) Omega-3 fatty acids are essential fats that are incredibly important for human health. Not only do these polyunsaturated fats make up cell membranes, but they also serve as the starting point for hormone production inside the body. Some of these hormones are crucial for regulating blood clotting, blood vessel contraction and relaxation, and inflammation.
Today, omega-3 fatty acids are well-known for offering multiple health benefits, the most notable of which is helping prevent heart disease and stroke. Other benefits associated with these healthy fats include helping control lupus , eczema and rheumatoid arthritis; alleviating anxiety and depression symptoms; helping prevent age-related eye diseases; supporting brain development and function; and protecting against some types of cancer.
According to a recent study, the health benefits of consuming omega-3 fatty acids does not end there. Researchers from Iran and Australia investigated the effects of omega-3 fatty acid supplementation in infertile men and found that these fats can also improve sperm parameters that impact fertility. They discussed their findings in an article published in the Journal of Dietary Supplements . Omega-3 fatty acids can help boost sperm health in infertile males
There are three main types of omega-3 fatty acids: alpha-linolenic acid (ALA), docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA). ALA, the most common type of omega-3 found in Western diets, is present in vegetable oils, nuts, flaxseed , leafy vegetables and the fat of grass-fed animals. DHA and EPA, on the other hand, come mainly from fatty fish, such as salmon, mackerel, sardines and cod.
Recent studies have associated ALA with better cardiovascular disease outcomes and lower risks of Type 2 diabetes and bone fractures. Although ALA is converted into EPA and DHA inside the body, the efficiency of this conversion is very low. This means that while foods rich in ALA are poor alternative EPA and DHA sources, ALA nevertheless offers substantial health benefits all on its own.
EPA and DHA, the so-called marine omega-3s, are important for fetal development and healthy agin g. They act as precursors of several metabolites that serve as lipid mediators; as such, they are beneficial for the prevention and treatment of many diseases. For instance, a study published in the American Journal of Clinical Nutrition reported that higher intake of EPA and DHA via fish oil supplementation decreased the expression of more than 1,000 genes in older adults. These genes were found to be involved in inflammatory pathways as well as signaling pathways that lead to atherosclerosis .
For their study, the Iranian-Australian team evaluated the effects of EPA and DHA supplementation on sperm parameters in infertile men. They searched different databases for relevant literature published between January 1, 1990 and December 20, 2017. The researchers then conducted a systematic review and meta-analysis of randomized controlled trials involving infertile men who were treated with DHA or EPA alone or in combination with other micronutrients.
The sperm parameters considered in the study included total sperm concentration, sperm motility, sperm DHA and seminal plasma DHA concentration. The researchers found three studies that met the inclusion criteria. A total of 147 patients comprised the intervention group, while 143 patients comprised the control group. (Related: Can probiotics reverse male infertility? )
Data analysis showed that omega-3 supplementation significantly increased sperm motility and seminal DHA concentrations in infertile men. Increased DHA levels in sperm is associated with better antioxidant status and reduced DNA damage . Compared with the controls, however, both DHA and EPA did not affect sperm concentration. The researchers confirmed the absence of publication bias through a funnel plot.
Based on these findings, the researchers concluded that DHA and EPA supplementation benefits infertile men by increasing sperm motility and DHA concentration in seminal plasma.
Sources include:
HSPH.Harvard.edu
Academic.OUP.com 1
Academic.OUP.com 2
Academic.OUP.com 3
TAndFOnline.com
Robotic Third Thumb changes how hand represented in brain – study

Dani Clode wearing the Third Thumb device she designed (Dani Clode/UCL)
Using a robotic Third Thumb can impact how the hand is represented in the brain, a new study has found.
Researchers trained people to use a robotic extra thumb and found they could effectively carry out dexterous tasks, like building a tower of blocks using the one hand.
Researchers said participants trained to use the thumb also increasingly felt like it was a part of their body. Body augmentation is a growing field aimed at extending our physical abilities, yet we lack a clear understanding of how our brains can adapt to it Designer Dani Clode started developing the device, called the Third Thumb, as part of an award-winning graduate project at the Royal College of Art, seeking to reframe the way we view prosthetics, from replacing a lost function, to an extension of the human body.
She was later invited to join Tamar Makin’s team of neuroscientists at UCL who were investigating how the brain could adapt to body augmentation.
Professor Makin, lead author of the study, said: “Body augmentation is a growing field aimed at extending our physical abilities, yet we lack a clear understanding of how our brains can adapt to it.
“By studying people using Dani’s cleverly designed Third Thumb, we sought to answer key questions around whether the human brain can support an extra body part, and how the technology might impact our brain.”
The device is 3D-printed, making it easy to customise, and is worn on the side of the hand opposite the user’s actual thumb, near the little finger.
It is controlled with pressure sensors attached to the wearer’s feet, on the underside of the big toes.
They are wirelessly connected to the Third Thumb, and both toe sensors control different movements by immediately responding to subtle changes of pressure from the wearer.
Twenty participants were trained to use the device over five days for the study. Our study shows that people can quickly learn to control an augmentation device and use it for their benefit, without overthinking During this time, they were also encouraged to take the thumb home each day after training to use it in daily life scenarios, totalling two to six hours of wear time each day.
These participants were compared to an additional group of 10 control participants who wore a static version of the thumb while completing the same training.
Participants were trained to use the device during daily laboratory sessions focusing on tasks that helped increase the co-operation between it and their hand.
This included picking up multiple balls or wine glasses with one hand.
They learned the basics of using the thumb very quickly, while the training enabled them to successfully improve their motor control, dexterity and hand/Third Thumb co-ordination, researchers said.
The study found that participants were also able to operate the device when distracted – building a wooden block tower while doing a maths problem – or while blindfolded.
Ms Clode said: “Our study shows that people can quickly learn to control an augmentation device and use it for their benefit, without overthinking.
“We saw that while using the Third Thumb, people changed their natural hand movements, and they also reported that the robotic thumb felt like part of their own body.” Evolution hasn’t prepared us to use an extra body part, and we have found that to extend our abilities in new and unexpected ways, the brain will need to adapt the representation of the biological body First author of the study, Paulina Kieliba, UCL Institute of Cognitive Neuroscience, said: “Body augmentation could one day be valuable to society in numerous ways, such as enabling a surgeon to get by without an assistant, or a factory worker to work more efficiently.
“This line of work could revolutionise the concept of prosthetics, and it could help someone who permanently or temporarily can only use one hand, to do everything with that hand.
“But to get there, we need to continue researching the complicated, interdisciplinary questions of how these devices interact with our brains.”
Participants’ brains were scanned before and after the training while they were moving their fingers individually.
Researchers said they found subtle but significant changes to how the hand that had been augmented with the Third Thumb was represented in the brain’s sensorimotor cortex.
Each finger is represented distinctly from the others in human brains but among the study participants, the brain activity pattern corresponding to each individual finger became more similar, the study found.
One week later, some of the participants were scanned again, and the changes in their brain’s hand area had subsided, researchers said.
This suggested the changes might not be long-term, but more research was needed to confirm this, they added.
Prof Makin added: “Evolution hasn’t prepared us to use an extra body part, and we have found that to extend our abilities in new and unexpected ways, the brain will need to adapt the representation of the biological body.”The findings are reported in the journal Science Robotics.PA
This Is What Doing Squats Does to Your Body, According to Science

On average , the typical American adult spends roughly six-and-a-half hours each and every day sitting down. Obviously, this isn’t good. According to the World Health Organization , leading a sedentary life doubles one’s risk of developing heart disease. What’s more, lounging more and exercising less is perhaps the shortest and surest path to weight gain , enduring back and shoulder pain, and—per recent research published in the Journal of Sports Sciences — poor mental health that could spiral into depression.
But if there is a perfect exercise antidote to sitting, there’s a case to be made that it’s squatting.
One fascinating study from last year, conducted by the University of Southern California and published in the Proceedings of the National Academy of Sciences , found that a tribe of hunter-gatherers living in Tanzania rest for long periods each day (9-10 hours) yet show little to no signs of the chronic diseases linked to sedentary behavior that are so prevalent in the West. What are they doing differently? Instead of sitting all day the tribe members squat or kneel for hours on end.
Furthermore, researchers of the world’s oldest living people have observed that they have a habit for sitting on the floor, which results in more squats every day. “The longest-lived women in the history of the world lived in Okinawa, and I know from personal experience that they sat on the floor,” Dan Buettner , a researcher and journalist, recently explained to Well+Good . “I spent two days with a 103-year-old woman and saw her get up and down from the floor 30 or 40 times, so that’s like 30 or 40 squats done daily.”
If you’re still not sold on the benefits of squatting more every day, read on, because here we explain everything that happens to your body when you make squatting a regular thing. And for more great exercise advice, don’t miss The Secret Exercise Trick for Flatter Abs After 40 . Shutterstock Squats may make you think of your glutes, but a solid squatting regimen works more than just the derrière. Squats also work and tone abs, obliques, the muscles surrounding the spine, and the transverse abdominis (deep core muscles). Research published in The Journal of Human Kinetics reports squats activate the erector spinae (spine muscles) four times more than planks. Those muscles also play a big role in standing upright, so squats can also help improve posture. Aside from parts of your upper body, the squat essentially strengthens every single muscle you need to fight gravity. For more great exercises you can do, see these 5-Minute Exercises for a Flatter Stomach Fast . Shutterstock The positive impact of exercise on the brain is well documented. Recent research shows just a quick, half-hour walk promotes improved blood flow to the brain and better memory skills among older adults. Interestingly, squats are especially effective at preventing cognitive decline, according to top experts.
Damian M. Bailey , Ph.D., a professor of physiology and biochemistry at the UK’s University of South Wales’ Neurovascular Research Unit and an advisor to the European Space Agency, recently appeared on the BBC Radio 4 podcast ” Just One Thing .” On the air, he said squats are a must for anyone concerned about their brain health.
“Squats intermittently challenge the brain with an increase of blood flow and a decrease of blood flow,” he explained. “What we have identified is that three to five minutes of squat stands three times a week is even more effective in terms of how the brain is adapting and responding to that exercise than steady-state exercise.” For more on this, check out The One Exercise That’s Best for Beating Back Alzheimer’s . Some people are natural-born athletes, while the rest of us have to put in much more work to see the same athletic results. A regular squatting routine may not turn you into Michael Jordan, but it can help improve explosive strength, speed, and overall athletic performance. A study published in the Journal of Sports Science & Medicine found a jump squat routine for just eight weeks helped improve a group of athletes’ sprint times, explosive strength, and other “athletic performance tasks.” Shutterstock We’ve established that squatting is great for a number of muscle groups, but what about your bones? Sure enough, squatting can also help support strong bones and greater bone density, especially in old age.
In one research project , a group of post-menopausal women dealing with osteoporosis followed a squatting routine for 12 weeks. By the end of the regimen, bone density in their necks and spines had increased by 2.9% and 4.9% respectively.
“People may be physically active, and many times people know they need to exercise to prevent obesity, heart disease or diabetes,” says Pamela Hinton, Ph.D., associate professor in the Department of Nutrition and Exercise Physiology at The University of Missouri-Columbia. “However, you also really need to do specific exercises to protect your bone health.” Dr. Hinton co-authored another study that concluded that weight-bearing exercises like squats promote bone formation among men.
And to learn how to do a proper squat, simply reference The Secret Trick That Makes Every Exercise Better, Says Top Trainer . When it comes to the mind, squats are the gift that just keeps giving. Research published in Frontiers in Neuroscience reports that squats—and leg exercises, in general—are essential to proper brain and nervous system functioning.
When we think about muscles, we tend to think of biceps or pecs, but the body’s biggest muscles reside within the legs. So, weight-bearing leg exercises send signals to the brain to create more and more new nerve cells, which help us learn, deal with stress, and adapt.
“It is no accident that we are meant to be active: to walk, run, crouch to sit, and use our leg muscles to lift things,” says study co-author Dr. Raffaella Adami from the Università degli Studi di Milano, Italy. “Neurological health is not a one-way street with the brain telling the muscles ‘lift,’ ‘walk,’ and so on.” And for […]
