Nature Knows and Psionic Success
God provides
Minimizing the impact of touch starvation in long-term care residents

Jennifer Birdsall, Ph.D. What is touch starvation?
Also known as “touch deprivation,” “skin hunger” or “hug deprivation,” touch starvation is what occurs when a person’s exposure to physical contact has been significantly reduced or eliminated, such as during the COVID-19 pandemic and associated social distancing.
I began researching this phenomenon and discovered there was a name for it after a number of psychologists in my organization sought consultation on ways to reduce the added psychological impacts they were seeing in their skilled nursing home patients from the lack of positive human touch. Further, the psychologists were expressing how difficult it was for themselves not being able to offer a needed hug or brief hand holding during their psychotherapy sessions with patients struggling with significant grief, depression and fears.
While most residents in long-term care communities understand the reasons we cannot hug or hold a hand with those we care about, the effects of long-standing touch starvation are nonetheless significant.
Why is physical contact so important?
Positive human touch is an integral part of human interaction and a legitimate physical and emotional need. It is hardwired and begins at birth, starting with the physical contact between a mother and newborn that facilitates bonding.
Positive physical touch in turn leads to a positive physiological experience at the neurochemical level. This not only occur through physical contact between parents and children or between romantic partners, but includes all positive physical touch — even platonic contact among friends and colleagues, and between patients and their formal caregivers. Examples are a hug or warm embrace, one arm linked through another, holding hands, a reassuring hand on a shoulder, high fives, handshakes, a pat on the back, etc. Unfortunately, apart from the immediate family one lives with, most of these experiences are off limits due to COVID-19 infection control protocols and social distancing guidelines.
Losing this part of the human experience and not knowing when it will safely return is yet another devastating consequence of the pandemic. Over time, the mental health consequences of touch starvation can include increases in stress, depression, anxiety, sleep disturbance and trauma-related symptoms.
How does human touch impact our emotional well-being?
When we feel a friendly touch on our skin, for example a pat on the back, our brains release oxytocin, a neuropeptide involved in increasing positive, feel-good emotions. It does this by promoting a sense of positive social connection, trust, empathy, and bonding in relationships. At the same time, it works to decrease fear and anxiety responses in the brain. Hence why oxytocin is affectionately known as the “cuddle hormone” or “love hormone.” Without physical contact, a person loses the positive emotional boost from this mood lifting hormone.
What can we do to reduce the negative impacts of touch starvation?
Oxytocin is not the only “feel good” hormone. Therefore, during a time of social distancing, it is important to focus on ways to increase the natural release of our other mood lifting neurochemicals including dopamine, serotonin, and endorphins.
Dopamine is a neurotransmitter that is important in the brain’s reward system. We get a boost of dopamine when we experience something pleasurable, including praise or when we complete a task.
Serotonin is a neurotransmitter that helps regulate mood. This is why certain antidepressants called selective serotonin reuptake inhibitors (SSRIs), target serotonin by increasing the availability of serotonin in the brain. Activities that increase serotonin can improve our mood.
Endorphins are your body’s natural pain reliever, which your body produces in response to discomfort or stress. Endorphin levels also increase when you engage in reward-producing activities, such as eating and exercising.
What are activities we can provide our residents to support the release of these three feel good neurochemicals? (Tip: these strategies will work for you too!)
1. Connecting with others virtually . Help residents have virtual meetings with their family and friends. Engaging in pleasant events in general helps release serotonin and dopamine. Plus, while not the same impact as in-person encounters and physical contact, having shared positive encounters with people you care about, even remotely, can release oxytocin through the bonding experience.
2. Moving and exercising . Encourage residents to move safely (e.g., stretching and chair exercises). Exercise can release endorphins. Regular exercise routines increase dopamine and serotonin production.
3. Getting outside . Enable safe, social-distanced opportunities for residents to spend time in outdoor areas. Sunlight increases the production of serotonin and endorphins. Plus, change of scenery can improve mood.
4. Giving praise and compliments. Find opportunities to give genuine praise and compliments to your residents. Compliments and praise are a form or reward and lift a person’s mood by releasing dopamine.
5. Smiling and Laughing . Find ways to make your residents laugh. All three “feel good” neurochemicals — dopamine, serotonin and endorphins — get released when we smile and laugh. Play funny movies, television shows or YouTube videos. Prepare a joke of the day that CNAs can share with their residents during care activities. Encourage CNAs and nursing staff to ask residents to share a funny memory from their past that will get everyone laughing. And finally, make sure staff are still smiling, as smiles are contagious — even from behind a mask, which can still be “seen” in the eyes.
Jennifer Birdsall, Ph.D., a licensed clinical psychologist, is clinical director of CHE Behavioral Health Services in Los Angeles.
Essential oils to relax, heal & rejuvenate you for summer

Essential oils help people heal and relax, diminish feelings of fatigue and anxiety. Many of them work stimulate certain areas of the body and alleviate symptoms of distress. They can affect parts of the brain that control emotions, behaviour, motivation, long-term memory, and assist in lowering depression, anxiety, and self-doubt. Which oils?
Basil
The reason basil is effective is because it helps to remove stress and calm the nervous system. It stimulates the adrenal glands giving you more motivation and more energy. Having more energy helps you become more productive and this increases your mood and level of satisfaction. Basil oil lowering your stress makes you feel stronger and more resilient. It is also rich in antioxidants and vitamin C. This oil however, should not be used when pregnant as it may cause early contractions. Lemon
Lemon helps to boost your dopamine and serotonin levels. These two hormones directly affect your overall wellbeing. An increase of dopamine makes you feel more mentally alert. It helps to improve your concentration and general mood. This makes it easier to perform your work, as well as to interact better with others. Serotonin increase balances your mood and prevents depression. Lavender
Although it is popularly used for relaxation, lavender oil also has a clear uplifting effect that lifts your mood. It reduces anxiety so you are calmer. It also helps you sleep better which will help you feel better the next day. Lavender is good for your immune system so it can help you kick that cold, or prevent you from actually getting one. Lavender oil can be used in your bath, a diffuser or even a quick whiff out of the bottle will help. Bergamot
Bergamot oil has been shown to decrease work-related stress. Bergamot reduces the amount of cortisol in the body helping to reduce the feelings of anxiety. Using Bergamot helps lower your blood pressure and heart rate putting you in a more relaxed state. Bergamot also helps reduce the feeling of mental and physical fatigue. Jasmine
Jasmine produces a calming and romantic effect so it can help with anxiety, stress and aggression which promotes a feeling of well-being. It can also make you feel more energetic. This essential oil is another one to avoid when pregnant as it may cause early labour. Rose
Rose oil is great for alleviating depression as well as anxiety. The scent of roses boosts your self-esteem, makes you more confident and appealing and helps boost libido. Often people have fond memories associated with roses which in itself helps to lift your mood.
If you feel your mood, energy or wellbeing could do with a lift then look at some aromatherapy blends and energy elixirs. These can be specifically designed for your needs. Always use completely natural oils and mix them in a carrier oil if you are going to wear them on your skin. Best to consult a therapist to do it for you so you know the right quantities have been mixed together. Now that spring is coming it’s a great way to rejuvenate, relax and prepare to enjoy the summer sunshine.
For more information on how to look after your hair in the summer sun check out my article at https://www.wellbeing.com.au/body/beauty/hair-care-nurturing-and-revitalising-your-hair.html
Why should drink ginger tea regularly?
Ginger has been used for centuries as a natural remedy for many ailments. It’s also a familiar, easy-to-find condiment and can be a great substitute for coffee or other harmful drinks!
Ginger has long been not only a spice to taste better, but also a medicinal herb. The benefits of ginger tea not only improve health and prevent diseases, but also help you maintain your figure in a completely natural way.
Ginger tea has been used for centuries as a natural remedy for many ailments. However, their use as a morning drink is not common. This can be an energetic way to start your day. Benefits of ginger tea for health
Ginger tea is good for pregnant women
In fact, two-thirds of pregnant people suffer from irritability, nausea, or morning sickness. Ginger has been used to treat nausea caused by motion sickness and motion sickness. It is also used to reduce nausea in chemotherapy patients.
According to nutritionist Katie Boyd, if you are not pregnant but have discomfort during your period, ginger tea can help. “It helps to alleviate flatulence, especially around the” red light “period in women, she revealed. Ginger tea enhances immunity
Nutritionist Hayley Cimring advises: If you’re looking for a natural way to boost your immune system, you might consider using ginger tea. Ginger has antiviral, antimicrobial and anti-fungal properties, not to mention a rich source of vitamin C. “This is a great natural remedy that helps support a healthy immune system. Ginger root contains compounds called gingerols, shogaol and paradols. These compounds have the ability to aid the body in fighting inflammation and free radicals. Although drinking ginger tea is not a cure, “prevention is better than cure”. Ginger tea improves oral health
“Its anti-inflammatory and anti-microbial properties kill harmful bacteria and thus prevent tooth decay,” said Henry Hackney, a dentist. Furthermore, daily consumption of ginger aids in plaque reduction and strengthens your gums.
Raffinose, the main active ingredient in ginger, helps soothe various toothache. However this is only a temporary solution, you need to see your dentist when the problem worsens.
Watch next: 7 Health Benefits of Green Tea & How to Drink it Ginger tea reduces indigestion
Most people know how uncomfortable it feels to eat a large meal. But if you find yourself having heartburn more than twice a week, you may have gastroesophageal reflux disease (GERD). If that is the case, you can drink ginger tea every day to help fight reflux disease. One of the benefits of ginger tea is that it will help speed digestion, help empty the stomach and alleviate indigestion and heartburn. Ginger tea restricts chronic inflammation
With a cut on your hand or ankle sprain, you may find that your body responds by getting inflamed to facilitate the healing process. And that is a normal response, but not all inflammation is beneficial for the body. Specifically, chronic inflammation can lead to an increased risk of diseases like diabetes and depression.
Nutritionist Katie Boyd recommends sipping ginger tea every day. “The biggest effect I get from drinking ginger tea is that it supports the natural inflammatory response.” Ginger tea reduces the risk of cancer
Drinking ginger tea every day can help prevent cancer. Ginger contains many antioxidants (such as vitamin C) and nutrients (such as potassium) to fight inflammation and overall disease, typically cancer. There is a lot of additional science on this topic. As PLOS One revealed in 2015, researchers conclude that ginger may help prevent pancreatic cancer. Plus, a study in the journal Nutrients shows that ginger can suppress colorectal cancer cells. Ginger tea supports weight loss
According to Time magazine, 49% of all Americans are trying to lose weight – in fact, one in two people has an overweight problem.
Ginger root contains properties called gingerols and shogaols that help support the biological activities of the body. In other words, they increase your metabolism and lower your cholesterol levels. “Although drinking ginger tea alone won’t help you lose weight, it can help if you combine it with another healthy lifestyle,” Hickey said. Ginger tea helps with mental focus
Drinking ginger tea has been linked to supporting brain health. Studies using ginger extract have shown that it can improve cognitive function and enhance working memory. Of course, ginger tea is not a cure-all, but it’s incredibly helpful!
Drinking ginger tea every day is good for the heart
According to a 2017 study in the Journal of Nutrition, which surveyed 4,628 people – 2,805 women and 1,823 men between the ages of 18 and 77, consuming ginger was shown to reduce the risk of high blood pressure. In addition, the researchers concluded that ginger consumption reduced the risk of heart attack and blood clot formation as well as decreased cholesterol levels and improved blood circulation.
Watch next: What Happens To Your Body If You Drink Green Tea Daily For 30 Days ginger tea
First ‘plug and play’ brain prosthesis demoed in paralyzed person
Credit: CC0 Public Domain In a significant advance, UC San Francisco Weill Institute for Neurosciences researchers working towards a brain-controlled prosthetic limb have shown that machine learning techniques helped an individual with paralysis learn to control a computer cursor using their brain activity without requiring extensive daily retraining, which has been a requirement of all past brain-computer interface (BCI) efforts.
“The BCI field has made great progress in recent years, but because existing systems have had to be reset and recalibrated each day, they haven’t been able to tap into the brain ‘s natural learning processes. It’s like asking someone to learn to ride a bike over and over again from scratch,” said study senior author Karunesh Ganguly, MD, Ph.D., an associate professor in the UCSF Department of Neurology. “Adapting an artificial learning system to work smoothly with the brain’s sophisticated long-term learning schemas is something that’s never been shown before in a person with paralysis.”
The achievement of “plug and play” performance demonstrates the value of so-called ECoG electrode arrays for BCI applicartions. An ECoG array comprises a pad of electrodes about the size of a post-it note that is surgically placed on the surface of the brain. They allow long-term, stable recordings of neural activity and have been approved for seizure monitoring in epilepsy patients. In contrast, past BCI efforts have used “pin-cushion” style arrays of sharp electrodes that penetrate the brain tissue for more sensitive recordings but tend to shift or lose signal over time. In this case, the authors obtained investigational device approval for long-term chronic implantation of ECoG arrays in paralyzed subjects to test their safety and efficacy as long-term, stable BCI implants.
In their new paper, published September 7, 2020 in Nature Biotechnology , Ganguly’s team documents the use of an ECoG electrode array in an individual with paralysis of all four limbs (tetraplegia). The participant is also enrolled in a clinical trial designed to test the use of ECoG arrays to allow paralyzed patients to control a prosthetic arm and hand, but in the new paper, the participant used the implant to control a computer cursor on a screen.
The researchers developed a BCI algorithm that uses machine learning to match brain activity recorded by the ECoG electrodes to the user’s desired cursor movements. Initially, the researchers followed the standard practice of resetting the algorithm each day. The participant would begin by imagining specific neck and wrist movements while watching the cursor move across the screen. Gradually the computer algorithm would update itself to match the cursor’s movements to the brain activity this generated, effective passing control of the cursor over to the user. However, starting this process over every day put a severe limit on the level of control that could be achieved. It could take hours to master control of the device, and some days the participant had to give up altogether.
The researchers then switched to allow the algorithm to continue updating to match the participant’s brain activity without resetting it each day. They found that the continued interplay between brain signals and the machine learning-enhanced algorithm resulted in continuous improvements in performance over many days. Initially there was a little lost ground to make up each day, but soon the participant was able to immediately achieve top level performance.
“We found that we could further improve learning by making sure that the algorithm wasn’t updating faster than the brain could follow—a rate of about once every 10 seconds,” said Ganguly, a practicing neurologist with UCSF Health and the San Francisco Veterans Administration Medical Center’s Neurology & Rehabilitation Service. “We see this as trying to build a partnership between two learning systems—brain and computer—that ultimately lets the artificial interface become an extension of the user, like their own hand or arm.”
Over time, the participant’s brain was able to amplify patterns of neural activity it could use to most effectively drive the artificial interface via the ECoG array, while eliminating less effective signals—a pruning process much like how the brain is thought to learn any complex task, the researcher say. They observed that the participant’s brain activity seemed to develop an ingrained and consistent mental “model” for controlling the BCI interface, something that had never occurred with daily resetting and recalibration. When the interface was reset after several weeks of continuous learning, the participant rapidly re-established the same patterns of neural activity for controlling the device—effectively retraining the algorithm to its former state.
“Once the user has established an enduring memory of the solution for controlling the interface, there’s no need for resetting,” Ganguly said. “The brain just rapidly convergences back to the same solution.”
Eventually, once expertise was established, the researchers showed they could turn off the algorithm’s need to update itself altogether, and the participant could simply begin using the interface each day without any need for retraining or recalibration. Performance did not decline over 44 days in the absence of retraining, and the participant could even go days without practicing and see little decline in performance. The establishment of stable expertise in one form of BCI control (moving the cursor) also allowed researchers to begin “stacking” additional learned skills—such as “clicking” a virtual button—without loss of performance.
Such immediate “plug and play” BCI performance has long been a goal in the field, but has been out of reach because the “pincushion-style” electrodes used by most researchers tend to move over time, changing the signals seen by each electrode. Also, because these electrodes penetrate brain tissue, the immune system tends to reject them, gradually impairing their signal. ECoG arrays are less sensitive than these traditional implants, but their long-term stability appears to compensate for this shortcoming. The stability of ECoG recordings may be even more important for long-term control of more complex robotic systems such as artificial limbs, a key goal of the next phase of Ganguly’s research.
“We’ve always been mindful of the need to design technology that doesn’t end up in a drawer, so to speak, but which will actually improve the day-to-day lives of paralyzed […]
How to live longer: A plant which improves memory, helps with ageing and boosts longevity

Blue butterfly pea powder has been described as the latest and greatest new ingredient to hit the custom drink world, replacing chemical-filled drinks and other toxic food colouring agents to produce an eye-catching drink hailed as the liquid for longevity. The mesmerising colours of the flower when added with hot water are not just a feast for the eyes though. The plant is said to hold numerous health benefits from improving the ageing process, memory, digestive health to even increasing hair growth.
Hair loss treatment: A herb which increases hair growth
High blood pressure: Simple task to lower your reading
Blue Butterfly Pea Powder is packed full of antioxidants which help to support the skin’s collagen and elasticity.
The powerful plant also contains anthocyanin to support hair and eye health, both of which promote the overall healthy life cycle of your cells.
Blue butterfly pea powder is also a notable nerve tonic and provides support to the digestive, circulatory, and central nervous systems.
DON’T MISS
Vitamin D deficiency symptoms: Three warning signs in your muscles
Herbalist and holistic health practitioner, Rachelle Robinett said: “Butterfly pea flower is a natural nootropic, which means that it can potentially help improve cognitive function.
“A review found that butterfly pea flower had potential benefits particularly with boosting learning and memory, although more clinical human trials are needed to make this conclusive.
“Butterfly pea powder is a beautiful plant with a wide range of uses — from agricultural to medicinal, nutritional and otherwise.
“We are only beginning to understand and test or study the active compounds in them.” How to live longer: Butterfly pea powder contains ingredients known to improve memory and longevity The plant is also known as a brainpower plant as it not only enhances memory and brainpower, it also provides one with a calm, relaxed focus.
Butterfly pea flower is rich in antioxidants which means it can help the body fight back against the damage caused by free radicals, like inflammation and signs of ageing in the skin.
It’s particularly rich in anthocyanin, a type of antioxidant also found in blueberries and red wine that is well-known for fighting inflammation and boosting heart health.
The powerful plant also supports hair and eye health, both of which promote the overall healthy life cycle of one’s cells.
Butterfly pea powder provides support to the digestive, circulatory, and central nervous systems.
It can be made as a tea or it is edible and tastes and looks great in a green salad.
First ‘plug and play’ brain prosthesis demonstrated in a person with paralysis
In a significant advance, UC San Francisco Weill Institute for Neurosciences researchers working towards a brain-controlled prosthetic limb have shown that machine learning techniques helped an individual with paralysis learn to control a computer cursor using their brain activity without requiring extensive daily retraining, which has been a requirement of all past brain-computer interface (BCI) efforts. The BCI field has made great progress in recent years, but because existing systems have had to be reset and recalibrated each day, they haven’t been able to tap into the brain’s natural learning processes. It’s like asking someone to learn to ride a bike over and over again from scratch. Adapting an artificial learning system to work smoothly with the brain’s sophisticated long-term learning schemas is something that’s never been shown before in a person with paralysis.” Karunesh Ganguly, MD, PhD, Study Senior Author, Associate Professor, UCSF Department of Neurology The achievement of “plug and play” performance demonstrates the value of so-called ECoG electrode arrays for BCI applicartions. An ECoG array comprises a pad of electrodes about the size of a post-it note that is surgically placed on the surface of the brain. They allow long-term, stable recordings of neural activity and have been approved for seizure monitoring in epilepsy patients. In contrast, past BCI efforts have used “pin-cushion” style arrays of sharp electrodes that penetrate the brain tissue for more sensitive recordings but tend to shift or lose signal over time. In this case, the authors obtained investigational device approval for long-term chronic implantation of ECoG arrays in paralyzed subjects to test their safety and efficacy as long-term, stable BCI implants.
In their new paper, published September 7, 2020 in Nature Biotechnology , Ganguly’s team documents the use of an ECoG electrode array in an individual with paralysis of all four limbs (tetraplegia). The participant is also enrolled in a clinical trial designed to test the use of ECoG arrays to allow paralyzed patients to control a prosthetic arm and hand, but in the new paper, the participant used the implant to control a computer cursor on a screen.
The researchers developed a BCI algorithm that uses machine learning to match brain activity recorded by the ECoG electrodes to the user’s desired cursor movements. Initially, the researchers followed the standard practice of resetting the algorithm each day. The participant would begin by imagining specific neck and wrist movements while watching the cursor move across the screen. Gradually the computer algorithm would update itself to match the cursor’s movements to the brain activity this generated, effective passing control of the cursor over to the user. However, starting this process over every day put a severe limit on the level of control that could be achieved. It could take hours to master control of the device, and some days the participant had to give up altogether.
The researchers then switched to allow the algorithm to continue updating to match the participant’s brain activity without resetting it each day. They found that the continued interplay between brain signals and the machine learning-enhanced algorithm resulted in continuous improvements in performance over many days. Initially there was a little lost ground to make up each day, but soon the participant was able to immediately achieve top level performance.
“We found that we could further improve learning by making sure that the algorithm wasn’t updating faster than the brain could follow — a rate of about once every 10 seconds,” said Ganguly, a practicing neurologist with UCSF Health and the San Francisco Veterans Administration Medical Center’s Neurology & Rehabilitation Service. “We see this as trying to build a partnership between two learning systems — brain and computer — that ultimately lets the artificial interface become an extension of the user, like their own hand or arm.”
Over time, the participant’s brain was able to amplify patterns of neural activity it could use to most effectively drive the artificial interface via the ECoG array, while eliminating less effective signals — a pruning process much like how the brain is thought to learn any complex task, the researcher say. They observed that the participant’s brain activity seemed to develop an ingrained and consistent mental “model” for controlling the BCI interface, something that had never occurred with daily resetting and recalibration. When the interface was reset after several weeks of continuous learning, the participant rapidly re-established the same patterns of neural activity for controlling the device — effectively retraining the algorithm to its former state.
“Once the user has established an enduring memory of the solution for controlling the interface, there’s no need for resetting,” Ganguly said. “The brain just rapidly convergences back to the same solution.”
Eventually, once expertise was established, the researchers showed they could turn off the algorithm’s need to update itself altogether, and the participant could simply begin using the interface each day without any need for retraining or recalibration. Performance did not decline over 44 days in the absence of retraining, and the participant could even go days without practicing and see little decline in performance. The establishment of stable expertise in one form of BCI control (moving the cursor) also allowed researchers to begin “stacking” additional learned skills — such as “clicking” a virtual button — without loss of performance.
Such immediate “plug and play” BCI performance has long been a goal in the field, but has been out of reach because the “pincushion-style” electrodes used by most researchers tend to move over time, changing the signals seen by each electrode. Also, because these electrodes penetrate brain tissue, the immune system tends to reject them, gradually impairing their signal. ECoG arrays are less sensitive than these traditional implants, but their long-term stability appears to compensate for this shortcoming. The stability of ECoG recordings may be even more important for long-term control of more complex robotic systems such as artificial limbs, a key goal of the next phase of Ganguly’s research.
“We’ve always been mindful of the need to design technology that doesn’t end up in a drawer, so to speak, but which will […]
Plug-and-play brain-decoding device picks up where it left off

Scientists are getting better at using machines to decode electrical signals coming from the brain, but a new “plug-and-play” device represents a significant step forward Machines that attach to the brain and decode its activity promise to open up all kinds of medical possibilities, potentially allowing for improved screening of Alzheimer’s or the monitoring of internal organs . One of their more promising applications involves allowing sufferers of paralysis to regain control of prosthetic devices and limbs via their brain signals, something a team from the University of California, San Francisco (UCSF) has now demonstrated with a first-of-a-kind plug-and-play device.
These types of machines are known as brain-computer interfaces (BCIs), and there are quite a few under development that have shown some promising capabilities over the past few years. In their various forms, these devices can be implanted in the brain and, powered by advanced algorithms, turn its electrical signals into control inputs for all kinds of devices, from prosthetic limbs , to complete exoskeletons and even drones .
The new technology developed at UCSF could mark a significant step forward in this field of research, with the team focusing on the software that translates brain activity into action. This machine learning algorithm was trained to track a paralyzed user’s imagined movements of the neck or wrist, as they watched a computer cursor make its way across a screen.
To begin with, this algorithm had to be reset each day, with the software gradually learning to match the user’s desired motions with the actual movement of the cursor on screen, eventually enabling them to control it. But this could take hours of experimentation each day, so the scientists began to explore other options.
Some tweaks to the algorithm enabled it to continue learning about the user’s brain activity and desired movements, without resetting and starting from scratch each day. The team found that this approach enabled the algorithm to better itself each day on an ongoing basis, and eventually meant that the user was able to plug in and begin using it to great effect right away. Steve Babuljak Senior author Karunesh Ganguly in the lab during previous research “We found that we could further improve learning by making sure that the algorithm wasn’t updating faster than the brain could follow – a rate of about once every 10 seconds,” says Karunesh Ganguly, a practicing neurologist with UCSF Health. “We see this as trying to build a partnership between two learning systems – brain and computer – that ultimately lets the artificial interface become an extension of the user, like their own hand or arm.”
The BCI used in these experiments is known as an ECoG array, which is a pad of electrodes around the size of a Post-it note that is surgically implanted on the surface of the brain. The researchers obtained special approval to implant it in paralyzed patients on a long-term basis for the purpose of their experiments, and found that over time, the users’ brains were optimizing their activity to control the BCI, without the need for daily recalibration.
“Once the user has established an enduring memory of the solution for controlling the interface, there’s no need for resetting,” says study senior author Karunesh Ganguly. “The brain just rapidly convergences back to the same solution.”
With enough work, the researchers found they could actually switch off the algorithm’s auto-updating feature and the user could simply plug in and start using it each day. Even without any daily calibration, the performance did not decline over a 44-day period of use, with the user also able go several days without using it and only experience a small decline in performance.
“The BCI field has made great progress in recent years, but because existing systems have had to be reset and recalibrated each day, they haven’t been able to tap into the brain’s natural learning processes. It’s like asking someone to learn to ride a bike over and over again from scratch,” says Ganguly. “Adapting an artificial learning system to work smoothly with the brain’s sophisticated long-term learning schemas is something that’s never been shown before in a paralyzed person.”
The research was published in the journal Nature Biotechnology .
How to boost your immune system: Simple Ideas
Before we continue, I want to make it clear; we are not advocating or stating that you should take any of these supplements listed below. We are providing data for you to analyse as we always do; our stance will forever remain the same. We don’t tell people what to do, we provide data, and then you decide how you are going to use that data. If you disagree with some or all of the information listed below, that is your right, and we are not going to argue with you. Listen to calming music
If you have to practice social distancing, you can always pick up the phone or use skype or WhatsApp to talk to a loved one or friend. Don’t sit alone and panic; talking about an issue helps relieve stress.
Supplements that are helpful and that we are ourselves are taking
Vit A, Vit D, and Zinc: All three are good for boosting the immune system. A bit of Vit C can also be helpful.
Olive leaf extract: Natural antiviral agent
B complex: has many benefits, one of which is to help one cope with stress.
How to boost your immune system: Out of the box strategies
I am only discussing the stuff below because I was asked by several subscribers what I am doing in terms of the coronavirus. For those that are willing to experiment the information listed below might prove to be of interest. I am not advocating that you do this, but I have used these substances for years and continue to use them. I am willing to push the envelope provided there is data to back up a novel therapy. Hydrogen peroxide 3%:
I use it as a disinfectant as its more effective than alcohol. Also, when the first signs of the flu start to manifest, I put undiluted 3% solution in both ears for 5-15 minutes. I wait until the bubbling stops before moving to the other ear. I also gargle with it and have always experienced substantial relief from a sore throat. I usually dilute 3% with some water and then gargle with it for 5 to 15 minutes. I have either stopped flu dead in its tracks or improved the recovery time by 50%.
The concentration of H2O2 required to kill half the bacteria within 15 s was 1.8 M (6%) but fell to 0.3 M (1%) at 2 min, to 10 mM (0.03%) at 1 h, and to 0.2 mM (0.0007%) with a 24-h exposure. The results indicate that if high levels of H2O2 can be sustained for long periods of time, H2O2 is an effective bactericidal agent, and the presence of LP and SCN- protects streptococci against killing by H2O2. Nevertheless, the combination of LP, H2O2, and SCN- is much more effective than H2O2 alone as an inhibitor of bacterial metabolism and growth. https://bit.ly/33y8B3t
Scientists at Oregon Health & Science University working with colleagues at the spin-out firm Najit Technologies published in vivo data demonstrating the utility of hydrogen peroxide (H2O2)-based approach to generating inactivated viral vaccines. Studies in mice demonstrated that H2O2-inactivated viral vaccines against lymphocytic choriomeningitis virus (LCMV), smallpox, and even West Nile virus triggered high titres of virus-specific CD8+ T cells or neutralising antibodies and provided long-term protection against subsequent challenge with lethal doses of the respective pathogen.
The researchers first confirmed that the oxidising agent H2O2 effectively inactivates both DNA and RNA viruses. They then demonstrated that the peroxide inactivation didn’t impact greatly on immunogenicity. When yellow fever virus (YFV) inactivated using either formaldehyde, BPL, or H2O2 was probed with immune serum from infected mice, the H2O2-inactivated virus retained 87–98% of the maximum antibody binding response observed with live virus. In contrast, YFV inactivated using formaldehyde or BPL demonstrated markedly reduced immunogenicity. https://bit.ly/2Qzv36Z
`The effect of H2O2 on adenovirus types 3 and 6, adeno-associated virus type 4, rhinoviruses 1A, 1B, and type 7, myxoviruses, influenza A and B, respiratory syncytial virus, strain Long, and coronavirus strain 229E was studied in vitro, using different H2O2 concentration and times of exposure. H2O2 in a 3 percent concentration inactivated all the viruses under study within 1–30 min. Coronavirus and influenza viruses were found to be most sensitive. Reoviruses, adenoviruses and adeno-associated virus were relatively stable. H2O2 is a convenient means for virus inactivation. https://bit.ly/2WyAU00 Honey
In general, I consume abnormally large amounts of sugar via honey, fruits and chocolates that contain three or fewer ingredients. No soy lecithin or anything that resembles it. It should have sugar, cocoa, cocoa derivatives for the most are okay, milk, and nuts or fruits). However, I eat no bread or any wheat-based products. I stopped all wheat consumption in 2013, and since then, I more than doubled my average natural sugar intake. During this period, I visited the Dentist only twice; on both occasions because they kept pestering me to come in for a check-up. Another benefit of not consuming any wheat is that I naturally lost all excess weight and I now weigh the same as I did at 19.
The exciting thing is that the antibacterial effect of honey is in part is attributed to due to its ability to produce hydrogen peroxide.
The healing property of honey is due to the fact that it offers antibacterial activity, maintains a moist wound condition, and its high viscosity helps to provide a protective barrier to prevent infection. Its immunomodulatory property is relevant to wound repair too. The antimicrobial activity in most honeys is due to the enzymatic production of hydrogen peroxide. However, another kind of honey, called non-peroxide honey (viz., manuka honey), displays significant antibacterial effects even when the hydrogen peroxide activity is blocked. Its mechanism may be related to the low pH level of honey and its high sugar content (high osmolarity) that is enough to hinder the growth of microbes. The medical-grade honeys have potent in vitro bactericidal activity against antibiotic-resistant bacteria causing several life-threatening infections to humans. https://bit.ly/2QxKblc
Honey is one […]
Chemicals in organophosphate pesticides cause brain damage: Study

( Natural News ) Prenatal exposure to organophosphate pesticides, a kind of pesticide considered toxic to humans, has been linked to impaired cognition and significant changes in the brain .
In a major breakthrough, scientists from the University of California, Berkeley (UCB) and Stanford University found that teenagers exposed in utero to organophosphate pesticides demonstrated altered brain activities during tasks that required executive control.
Sharon Sagiv, an assistant professor of disease and environmental health at UCB and the study’s lead author, said that their findings offer insight into the impact of organophosphate pesticides on the brain.
Sagiv and her colleagues are also the first to use advanced brain imaging techniques to demonstrate that exposure in utero to the said toxic chemicals can change brain activities.
Their findings appeared online in the journal Proceedings of the National Academy of Sciences of the United States of America (PNAS). Prenatal pesticide exposure changes the brain
Despite breakthroughs in brain science, the potential impact of pesticides on neurodevelopment is still unclear. To this end, Sagiv and her colleagues used functional near-infrared imaging (fNIRS) to monitor blood circulation in the brains of 95 teenagers born and raised in California’s Salinas Valley.
The use of organophosphate pesticides in Salinas Valley, one of California’s major valleys and most productive agricultural regions, is common practice. This renders the cohort a relevant group to examine for the potential effects of organophosphate pesticide exposure on the brain.
The participants had also been part of an earlier phase of the Center for the Health Assessment of Mothers and Children of Salinas (CHAMACOS) study. This is a longitudinal birth cohort study assessing the possible effects of pesticide exposure and other environmental factors on children’s health and neurodevelopment.
UCB scientists initiated the CHAMACOS study more than 20 years ago. The findings of their earlier research had linked prenatal organophosphate exposure to attention problems and a low intelligence quotient in children.
For this recent second phase, Sagiv and her colleagues used fNIRS to measure cerebral changes as the participants engaged in various tasks that required executive function, attention, social cognition and language comprehension.
They also utilized data from the California Pesticide Use Reporting program to estimate the proximity of the participants’ homes to pesticide-treated sites.
Upon assessing these data, they found that participants with higher prenatal organophosphate pesticide exposure in utero had less blood flow in their prefrontal cortex than their peers during tasks that required cognitive flexibility . This refers to the ability to switch between thinking about two different concepts or to think about multiple concepts at once.
However, the same participants demonstrated greater blood flow to their parietal and temporal lobes than their peers when engaged in tasks that tested memory retrieval, or the process of remembering information stored in long-term memory.
Brenda Eskenazi, a professor of public health at UCB and a member of the research team, said that fNIRS and neuroimaging afforded them insight into the potential impact of prenatal organophosphate pesticide exposure on the brain . Similar patterns in other brain conditions
However, their findings offered no clear explanation as to how organophosphate pesticide exposure led to reduced blood flow in some regions, but greater blood flow in others during different cognitive tasks.
That being said, the patterns are not unique to organophosphate pesticide exposure. Similar patterns are apparent in other conditions that affect the brain, including Type 1 diabetes , Parkinson’s disease and Alzheimer’s disease , according to Allan Reiss, the study’s co-author and a professor of behavioral sciences at Stanford University .
Reiss also speculated that the increase in blood flow could mean that the brain is utilizing more neural resources to address deficiencies in certain areas as a result of long-term or prenatal organophosphate pesticide exposure.
Therefore, further studies might help shed light on the mechanisms behind the effects of organophosphate pesticide exposure on neurodevelopment. (Related: DDT pesticide exposure during pregnancy now scientifically linked to autism .)
Sagiv and her colleagues plan to repeat the brain imaging experiments on a larger cohort to determine if the patterns hold.
Read more articles about the harmful effects of pesticide exposure at Pesticides.news .
Sources include:
NaturalHealth365.com
Cinnamon and turmeric’s brain-boosting clout keeps stacking up

I hate to break it to you, but your brain is shrinking.
Mine is too.
It’s something that happens to everyone with age, and it’s the reason that the term “senior moments” exists.
As your brain shrinks, so does your memory, concentration and overall brain power. And suddenly, you have more moments where you misplace your sunglasses (on your head) or forget the name of an acquaintance you run into at the grocery store.
Now, despite the fact that brain shrinking and the consequences that come with it are considered a normal part of aging, you’re not doomed to a future filled with embarrassing and forgetful moments. There are ways to slow (or even reverse) brain shrinkage and cognitive decline, so you don’t notice much (if any) difference in your cognitive skills as you get older.
Exercise has been shown to counteract age-related brain shrinkage. So has meditation . And what you eat has also been proven in countless studies to have an impact on how your brain ages. In fact, a new study shows that potent doses of two spices could keep your cognitive skills sharp as a cactus needle well into your senior years… A cinnamon and turmeric supplement makes older brains sharper
A recent study from researchers at Swansea University in the U.K. found that a supplement stacking cinnamon, turmeric/curcumin, chromium and alpha-lipoic acid improved cognitive abilities in healthy older adults.
The study included 30 adults between 51 and 79 years old. For three months, half of them consumed the supplement and half of them consumed a placebo. Researchers wanted to see how the supplement influenced blood sugar, cholesterol and cognitive abilities. It had a somewhat positive impact on blood sugar and cholesterol. But the most significant impact was on their cognition…
People who took the supplement had much better word recall and reaction times than people who took the placebo. Why? Well, most likely because of the strong doses of cinnamon and curcumin they received in the supplement.
Past research on cinnamon, for example, has shown that it has a remarkably positive impact on brain health. In fact, a 2015 study published in the journal Nutritional Neuroscience showed that cinnamon extract shielded rats from oxidative stress-related damage to their brains and cognitive impairment. Cinnamon has also been shown to reduce inflammation, enhance memory, strengthen attention span and improve cognitive processing in humans.
Curcumin, a potent anti-inflammatory compound in turmeric, has been shown to reduce inflammation in the brain. This is good news since brain inflammation is associated with Alzheimer’s disease. Curcumin supplements have also been shown in past studies to improve older adults’ scores on memory tests and lower the number of cognitive decline markers visible in brain scans.
Clearly, these two spices have some serious cognitive health clout and have gained a reputation as effective nootropics . Although, the two other ingredients in the supplements study participants took — chromium and alpha-lipoic acid — are also linked to cognitive health benefits. So, they may deserve some of the credit, too. How to harness the brain-boosting benefits of cinnamon and turmeric
Including more cinnamon and turmeric in your diet is a wonderful idea if you’re trying to maintain a healthy brain as you age. Here are a few ideas: Put a heaping dose of cinnamon in your oatmeal
Add extra cinnamon to your chai tea
Sprinkle cinnamon in your yogurt
Use cinnamon in savory dishes like stews and chilis
Add turmeric to your eggs
Try turmeric tea
Have curry dishes more often
In some cases, however, you may need a more potent dose of these spices than you can get through diet alone. That’s where supplements come in.
The supplement used in the study was a 1,400 mg blend of cinnamon (Cinnamomum cassia bark extract), curcumin/turmeric (Curcumin Longa L. root extract and powder), chromium and alpha-lipoic acid. You may want to look for something similar to support your brain health. Of course, you’ll want to talk to your doctor before starting new supplements, especially if you have any existing health conditions or are on any medications to make sure there are no negative interactions.
Sources:
> Effects of a Cinnamon, Curcumin/Turmeric Dietary Supplement on Glucose, Lipid, and Cognitive Measures — Current Developments in Nutrition.
Spice up your holidays with brain-healthy seasonings — Harvard Health Publishing.
4 Spices That Give Your Brain a Boost — University of Pittsburgh Medical Center.
5 Spices with Healthy Benefits — John Hopkins Medicine. Possible Role of Common Spices as a Preventive and Therapeutic Agent for Alzheimer’s Disease — International Journal of Preventive Medicine. Ageing and the brain — Postgraduate Medical Journal.
Opinion: My Mother, Dementia and Organic CBD Oil

Yesterday, my redoubtable eight-six year old mother announced that she thought she might do some baking and make some organic scones for Organic September. You could be forgiven for thinking that is charming, but quite unremarkable.
CBD Restores Cognitive Function
Let me enlighten you reader. Nine months ago my mother couldn’t cook or feed herself, following a spectacular cognitive meltdown and subsequent vascular dementia diagnosis. She relied on the unfamiliar world of revolving care at home just to get through the day. Now she can pretty much run her own life again, go the gym and live an independent life, thanks to the remarkable regenerative powers of an organic CBD Oil supplement and Holy Basil, a herb revered in Ayurvedic medicine for illuminating the mind in the centuries-old, integrated medicine system of India.
This is the story of how my mother regained a life worth living and her mind back, thanks to the powerful, regenerative benefits of plant medicine. It is also a story of hope and how my sister and I got to turn back the clock. What if the cruel, life changing, twilight world of dementia can be stopped or even reversed? I’m here to tell you that based on my own first hand experience of dealing with a parent with a diagnosis of hardening of the arteries, organic CBD Oil has worked for us, and reversed the catastrophic decline in my mother’s brain health, witnessed over the past three or four years.
Losing Our Minds
My mother lost her mind, literally in January. She had a spectacular meltdown; following months of complaining she couldn’t sleep and a broken gut which is the pathway for disease to take root. For most of last year, I observed the slow, fragmented decline of her short-term memory and her increasingly confused, chaotic behaviour. One of the most difficult aspects of dementia is the increasing hostility, suspicion and loss of boundaries and the terrible black episodes of depression. My mother frequently told me she would rather be dead. That was hard to bear.
I was heartbroken. My mother’s personality had vanished. In her place was a stranger, and I had no idea how to deal with her or help her. Up to that point the articles I had read about dementia talked about management of the disease, not a cure or reversal. Overnight, my mother became incapable of looking after herself, which was so cruel, as she has always been fiercely independent since my father passed away. On the worst days of the last two years, she would phone at anytime of the night or day, she would tell her carers exactly what she thought of them, and every minor ailment became unbearable to her.
My Mother Get Her Mind Back and Joins a Gym
Now, eight months later, her mind is working fully again, her memory is pin sharp and she can even add up figures in her head faster than I can. She has a better social life than people half her age, and two weeks ago she confounded us all, when she went back to the gym, thanks to the extraordinary health benefits of organic CBD Oil and Holy Basil. She is also back cooking her own organic meals from scratch. I also engaged Dr Ibrahim FRCP, a former NHS consultant and top functional physician to treat my mother’s multiple health problems through diet, nutrition and a functional medical approach. Interestingly, he praised me for my research into CBD Oil and said if journalism doesn’t work out I should consider medicine! In the weeks following my mother’s cognitive breakdown and subsequent dementia diagnosis, I refused to accept that my sister and I had lost our mother to this cruel disease.
Even in the immediate aftermath, when we had to negotiate the bewildering world of care at home, along with brain scans, a definitive diagnosis, and the shockingly inadequate response by my mother’s GP surgery and the local mental health team. The only help we were offered to deal with my mother’s dementia, fragile state and black moods was anti-depressants. How can that be treatment for a serious brain disease?
Kindness Not Prescription
My mother has inflammatory bowel disease and antidepressants cause almost instant and very severe diahorrea. In fact, when I spoke to a member of the mental health team, I will never forget her chilling attempt to get me to give my mother antidepressants without her consent. It was at this point I became very angry. My mother didn’t need antidepressants. Mostly, having lost all her closest friends, she simply longed for someone of her own generation to talk to, to reminisce with, and have a cup of tea and cake.
Why Are We Medicating People for Everything, Including Loneliness?
When a society tries to medicate people for simply being lonely, we have really lost all sense of civilization and humanity.
So, this galvanized me into action. There has to be a better and more gentle, holistic way to help my mother.
I am fascinated my plants and food as medicine. In another life, I would love to have been an integrated doctor. So, I emailed and phoned the brightest people I know in plant science. These are the trailblazers who are leading a renaissance in plant medicine and integrated health, with the focus on food as medicine. One of my contacts in natural health told me to read the World Health Organisation report on CBD Oil. By the time I had finished reading the report, I new we had to try CBD oil in legal supplement form. WHO Scholarly Report into CBD – https://www.who.int/medicines/access/controlled-substances/CannabidiolCriticalReview.pdf
My mum and I are the original organic girls. My dad was very proud of his compost heap and I grew up on organic food and produce from the garden, and my family has always turned to plants to heal everything from a cold to arthritis and to keep the heart healthy. When I rang mum and told her about CBD Oil, she said, ‘ What have […]
The Regenesis Project and Prodrome Sciences Launch Clinical Trial, Plasmalogen Supplement Demonstrates Potential to Support Memory Function

SANTA MONICA, Calif., Sept. 3, 2020 /PRNewswire/ — Problems with failing memory are common for many individuals as they grow older, and is particularly characteristic of patients with Alzheimer’s disease. Research shows that aging-related cognitive decline may be affected by Omega-3 levels and the health of cell membranes. Certain nutritional supplements developed to target Omega-3 and plasmalogen levels have shown promise in supporting brain health among older adults.
Plasmalogens are unique lipid molecules that are necessary for optimal neurological health and performance. Plasmalogen levels decrease with age as the body is no longer able to make enough to keep up with demand; this phenomenon appears to be amplified in degenerative diseases such as Alzheimer’s. While it is not possible to replenish plasmalogens through diet alone, supplementation involving Omega-3 and DHA may help boost plasmalogen levels.
ProdromeSciences has developed a 100% vegan and all-natural Omega-3 nutritional supplement oil, ProdromeNeuro. ProdromeNeuro is specifically designed to elevate Omega-3 plasmalogens, support cellular function, and help restore, maintain, and optimize neural membranes. The first human trial of this supplement successfully demonstrated increased Omega-3 plasmalogen levels in all six subjects at 24-hours post-consumption ( p <0.001). On average, these participants yielded 24-hour plasmalogen levels at 180% of baseline. No adverse reactions were observed.
The Regenesis Project, a clinical research program led by expert neurologist Dr. Sheldon Jordan, is investigating the ProdromeNeuro oil supplement among participants with age-related cognitive decline. It is hoped that the consumption of this product over the course of 4 months will yield improved plasmalogen levels and optimized memory function.
Study enrollment is already over 50% complete. To learn more about this study and how to enroll, visit www.neurologysantamonica.com .
How Turmeric Can Boost Your Memory, Ease Joint Pain, and Reduce Inflammation

Turmeric’s benefits have been known for thousands of years, but thanks to Instagram and Pinterest (we see you, golden milk), the spice is enjoying a massive surge in popularity. “Turmeric is getting a lot of attention lately,” says nutritionist and registered dietician Karen Ansel , R.D.N., C.D.N., author of Healing Superfoods for Anti-Aging . “But this root has been used in Chinese and Ayurvedic medicine for thousands of years to fight inflammation and improve digestive health.”
Grown throughout India and other parts of Asia, turmeric is a major ingredient in curry powder. It’s mainly found in spice- or supplement-form, and as a spice it’s commonly used to brighten up curries, stir fries, soups, and even smoothies. $8.40
“Any time you have brightly colored foods, you know there are plant compounds in there doing something great,” says Dawn Jackson Blatner, R.D.N., a dietitian and author of The Superfood Swap . “And turmeric is a bright golden—there’s nothing like it.”
Curcumin, one of turmeric’s primary ingredients, is thought to help fight inflammation, says Jackson Blatner. “All diseases basically start with inflammation, from gingivitis in your mouth to heart disease, so the idea of having a teaspoon a day of turmeric may be a good thing.” How much turmeric should you take each day?
When you’re looking for the correct dosage to take in supplement form, there’s no quick answer to this question, especially since more studies are needed; it also depends on what you’re trying to treat, and what your health practitioner recommends. Many of the studies cited below used a dosage of 500 mg , once or twice a day. What are the side effects of taking turmeric?
Turmeric doesn’t seem to cause serious side effects, though at higher doses it may cause mild stomach distress (nausea, diarrhea, stomach upset). It’s a good idea to check with a health practitioner who’s familiar with natural treatments, however, because turmeric can interfere with certain medications.
So, could taking turmeric or curcumin supplements help boost your health? There’s a lot of misinformation out there, so we looked at the science to bring you 10 ways that turmeric and curcumin could possibly improve your health. 1. Turmeric might help your memory.
Research done in Asian populations back in 2006 found that people who ate more curry scored higher on cognitive function tests (tests that measure memory, attention span, etc.) than those who didn’t eat as much of the spice. The scientists chalked up this benefit to turmeric, which is a major part of the Asian diet.
Recent findings have also pointed to brain-related benefits: For example, a 2018 study of people aged 51 to 84 found that those who took a 90 milligram curcumin supplement twice a day for 18 months saw a boost in memory compared to those who took a placebo. The study was small, but the researchers theorize that curcumin’s anti-inflammatory effects might protect the brain from memory-related diseases. More research will be needed to confirm these findings. 2. Turmeric may help ward off heart disease.
Curcumin’s antioxidants and anti-inflammatory compounds may help protect against certain heart conditions, including diabetic cardiomyopathy (heart muscle disease), arrhythmia (irregular heartbeat) and more, according to a 2017 review in the journal Pharmacological Research . 3. Turmeric might have an impact on certain cancers.
A 2015 review published in the journal Molecules concluded that curcumin might have the potential to fight off certain cancers. But it’s important to take these claims with a grain of salt: So far, most of this research has been conducted in in vitro studies. Still, the authors of the review also note that curcumin has been shown to prevent or slow down the activity of certain tumor cells, including those of skin cancers , digestive cancers, and more. Certainly, more studies would be needed to determine the impact of tumeric on cancer. 4. Turmeric may ease osteoarthritis pain.
Osteoarthritis is the most common cause of disability in the United States, affecting an estimated 30.8 million Americans, according to the Arthritis Foundation . A 2016 research review found that taking curcumin for 4 weeks could help relieve osteoarthritis pain among people who already have the condition—an effect that’s comparable to taking NSAIDs or glucosamine. 5. Turmeric may help with hay fever.
If you’re miserable in certain seasons with the sniffling, hacking, itchy, runny nose, and congestion of hay fever , curcumin could help because of its antioxidant and inflammatory powers. In a 2008 review of animal studies on the effectiveness of curcumin on allergy symptoms, it was found to inhibit the release of histimines, resulting in a marked reduction of symptoms. 6. Turmeric could help with depression symptoms.
In people with major depressive disorder who were already taking an antidepressant, curcumin was found to help ease symptoms. It was a small study , of short duration (only six weeks), and there have been reports online that overstated the findings. But in the study, there seemed to be no ill effects of taking curcumin in conjunction with Prozac, the antidepressant in the study, and perhaps some benefits. 7. Turmeric may have an impact on cholesterol.
This one is iffy, but there is some evidence that curcumin could help keep a certain type of bad cholesterol in line. A 2017 review of seven studies looked at the effects of turmeric and curcumin on blood lipid levels, and found that they may offer some improvement in people with cardiovascular disease risks. The review authors pointed out, however, that it’s premature to use the substances in a clinical setting because it’s hard to know what the correct dosage would be, and that more studies are needed. 8. Turmeric could be good for the liver.
A study review showed that a higher-dose of curcumin supplements could have a positive effect on non-alcoholic fatty liver disease (NAFLD), a condition in which there’s a build-up of fat in the liver that’s not caused by drinking too much alcohol. It’s one of the most common causes of liver disease in the U.S., according to the […]
How does loneliness affect our brains?

Jenny Siegwart Long before the world had ever heard of covid-19, Kay Tye set out to answer a question that has taken on new resonance in the age of social distancing: When people feel lonely, do they crave social interactions in the same way a hungry person craves food? And could she and her colleagues detect and measure this “hunger” in the neural circuits of the brain?
“Loneliness is universal thing. If I were to ask people on the street, ‘Do you know what it means to be lonely?’ probably 99 or 100% of people would say yes,” explains Tye, a neuroscientist at the Salk Institute of Biological Sciences. “It seems reasonable to argue that it should be a concept in neuroscience. It’s just that nobody ever found a way to test it and localize it to specific cells. That’s what we are trying to do.”
In recent years, a vast scientific literature has emerged linking loneliness to depression, anxiety, alcoholism, and drug abuse. There is even a growing body of epidemiological work showing that loneliness makes you more likely to fall ill: it seems to prompt the chronic release of hormones that suppress healthy immune function. Biochemical changes from loneliness can accelerate the spread of cancer, hasten heart disease and Alzheimer’s, or simply drain the most vital among us of the will to go on. The ability to measure and detect it could help identify those at risk and pave the way for new kinds of interventions.
In the months ahead, many are warning, we’re likely to see the mental-health impacts of covid-19 play out on a global scale. Psychiatrists are already worried about rising rates of suicide and drug overdoses in the US, and social isolation, along with anxiety and chronic stress, is one likely cause. “The recognition of the impact of social isolation on the rest of mental health is going to hit everyone really soon,” Tye says. “I think the impact on mental health will be pretty intense and pretty immediate.”
Yet quantifying, or even defining, loneliness is a difficult challenge. So difficult, in fact, that neuroscientists have long avoided the topic.
Loneliness, Tye says, is inherently subjective. It’s possible to spend the day completely isolated, in quiet contemplation, and feel invigorated. Or to stew in alienated misery surrounded by a crowd, in the heart of a big city, or accompanied by close friends and family. Or, to take a more contemporary example, to participate in a Zoom call with loved ones in another city and feel deeply connected—or even more lonely than when the call began.
This fuzziness might explain the curious results that came back when Tye, before publishing her first scientific paper on the neuroscience of loneliness in 2016, ran a search for other papers on the topic. Though she found studies on loneliness in the psychological literature, the number of papers that also contained the words “cells,” “neurons,” or “brain” was precisely zero. Neuroscientists have long assumed that questions about how loneliness might work in the human brain would elude their data-driven labs. Though the nature of loneliness has preoccupied some of the greatest minds in philosophy, literature, and art for millennia, neuroscientists have long assumed that questions about how it might work in the human brain would elude their data-driven labs. How do you quantify the experience? And where would you even begin to look in the brain for the changes brought about by such a subjective feeling?
Tye hopes to change that by building an entirely new field: one aimed at analyzing and understanding how our sensory perceptions, previous experiences, genetic predispositions, and life situations combine with our environment to produce a concrete, measurable biological state called loneliness. And she wants to identify what that seemingly ineffable experience looks like when it is activated in the brain.
If Tye succeeds, it could lead to new tools for identifying and monitoring those at risk from illnesses worsened by loneliness. It could also yield better ways to handle what could be a looming public health crisis triggered by covid-19. Finding the loneliness neurons
Tye has homed in on specific populations of neurons in rodent brains that seem to be associated with a measurable need for social interaction—a hunger that can be manipulated by directly stimulating the neurons themselves. To pinpoint these neurons, Tye relied on a technique she developed while working as a postdoc in the Stanford University lab of Karl Deisseroth.
Deisseroth had pioneered optogenetics, a technique in which genetically engineered, light-sensitive proteins are implanted into brain cells; researchers can then turn individual neurons on or off simply by shining lights on them though fiber-optic cables. Though the technique is far too invasive to use in people—as well as an injection into the brain to deliver the proteins, it requires threading the fiber-optic cable through the skull and directly into the brain—it allows researchers to tweak neurons in live, freely moving rodents and then observe their behavior.
Tye began using optogenetics in rodents to trace the neural circuits involved in emotion, motivation, and social behaviors. She found that by activating a neuron and then identifying the other parts of the brain that responded to the signal the neuron gave out, she could trace the discrete circuits of cells that work together to perform specific functions. Tye meticulously traced the connections out of the amygdala, an almond-shaped set of neurons thought to be the seat of fear and anxiety both in rodents and in humans. JENNY SIEGWART Kay Tye, a neuroscientist at the Salk Institute of Biological Sciences, is trying to detect and measure loneliness in the brain’s neural circuits. Scientists had long known that stimulating the amygdala as a whole could cause an animal to cower in fear. But by following the maze of connections in and out of different parts of the amygdala, Tye was able to demonstrate that the brain’s “fear circuit” was capable of imbuing sensory stimuli with far more nuance than previously understood. It seemed, in fact, to modulate courage too.
By the time Tye set […]
14 healthy reasons to workout before 9am

The optimum time of day to exercise is ultimately one that suits your individual lifestyle, sleeping habits and preferences. After all, squeezing in a workout at 7pm because you couldn’t resist a lie-in is always going to be a better option than skipping it altogether.
With that said, there are a whole host of benefits associated with swerving the snooze button and getting your workout done first thing. With advice from personal trainer James Starks, co-founder of Starks Fitness , we present 14 compelling reasons to hit the gym before 9am: 16 reasons to workout in the morning
The first couple of hours in the morning sets the tone for the rest of your day. Here are 14 morning workout benefits that might just convince you to set your alarm extra-early tomorrow morning: 1. Fewer distractions
When you first wake up, you’re totally unplugged from the world and haven’t yet turned your attention to your daily to-do list. For an hour or two hours, freedom from work and social commitments means you can focus more intently on your workout. Plus, when you exercise in the morning, you’re less likely to be interrupted by phone calls, texts or emails. 2. Reduced appetite
It may sound counter-intuitive, but a morning workout helps to banish food cravings. A study by Brigham Young University found that 45 minutes of moderate-to-vigorous exercise in the morning actually reduces a person’s emotional response to pictures of food. Not only were participants less tempted by the food, but they didn’t eat more food to make up for the extra calories they burned while exercising. 3. Increased overall activity
Far from completely wearing you out, working out in the morning can inspire you to move more throughout the day. In the same study , participants showed an increase in total physical activity on the days they worked out in the morning. ‘Once you’ve passed the hurdle of getting to the gym, it will leave you in a better state of mind and more likely make you take the stairs rather than the lift,’ says Stark. 4. Increased fat-burning
Exercising on an empty stomach – sometimes referred to as ‘fasted cardio’ – isn’t for everyone, but if weight loss is your goal, it might just help you supercharge your fat-burning potential. In a study of 10 men, published in the British Journal of Nutrition , working out before breakfast was shown to burn up to 20 per cent more fat compared to working out in the afternoon or evening. 5. Improved decision making
Working out in the morning also gives your brain a boost. A morning bout of moderate-intensity exercise improves cognitive performance – like decision-making, attention and visual learning – across the day, according to a study published in the British Journal of Sports Medicine . When participants added brief walking breaks over the course of an eight-hour day, they also saw a boost in short-term memory – even as little as three minutes every half an hour. 6. Fire up the brain
A morning workout may be a better match for your circadian rhythm, which involves the timed release of hormones such as cortisol. While it’s commonly known as the ‘stress hormone’, since it’s part of your body’s natural response to threats of harm or danger, cortisol’s role is to make you feel awake and alert. Typically, levels of the hormone increase in the morning – naturally peaking at around 8am – and dip in the evening. 7. Energy boost
Regular exercise is known to boost energy and reduce feelings of fatigue. In a study published in the journal Psychotherapy and Psychosomatics , researchers found that inactive people with persistent fatigue increased their perceived energy levels by 20 per cent and decreased fatigue by as much as 65 per cent by participating in regular exercise. By getting your workout in early, you’ll benefit from more energy throughout the day. 8. Mood boost
When you exercise, your body releases an array mood-boosting brain chemicals – including dopamine, norepinephrine, serotonin and endorphins – which promotes a sense of wellbeing. Working out also balances your body’s level of stress hormones, such as adrenaline and cortisol. ‘Getting the body moving is a well-known way of boosting endorphins – the body’s feel-good hormones – ensuring that you are set up for a productive day,’ says Stark. ‘Coming out of the gym will leave you feeling in a more positive mood and ready to take on the day.’ 9. Better food choices
Regular exercise can even change your food preferences and give you an appetite for fruits and vegetables. Analysis by Indiana University found that people who exercised for at least 30 minutes, five times or more a week ate the most fruit and vegetables, while those who exercised the least also ate the least. ‘Having already made the decision to get to the gym, you’re more likely to make the correct choices when it comes to food,’ says Stark. 10. Build muscle faster
Testosterone plays an important role in building and maintaining muscle mass and helping your body recover after a workout. It increases neurotransmitters, which encourage tissue growth; interacts with nuclear receptors in DNA, stimulating protein synthesis; and increases levels of growth hormone, which is essential for repairing muscles. Your testosterone levels are highest upon waking, so a morning workout will help you reap the benefits. 11. Better sleep
Where an evening workout is likely to rev you up before bed, boosting your heart rate and core temperature, a morning workout can help you get a better night’s kip. A study by Appalachian State University, adults who exercised at 7am fell asleep faster and slept better than those who hit the gym in the afternoon or evening. Who could turn down the opportunity for deeper, longer, higher-quality sleep? 12. Reduced diabetes risk
Hitting the gym first thing may help ward off type 2 diabetes by helping to regulate blood sugar levels. In a study by KU Leuven University, participants who exercised […]
How Brain Flexibility Emerges in Infants
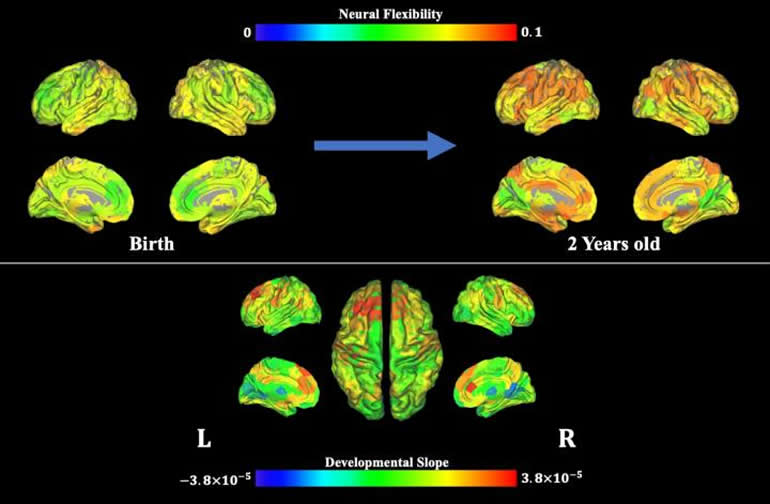
Summary: Neuroimaging study reveals how human brain complexity and cognitive flexibility develops during early infancy.
Source: University of North Carolina Health Care
Cognitive flexibility refers to the ability to readily switch between mental processes in response to external stimuli and different task demands. For example, when our brains are processing one task, an external stimulus is present, requiring us to switch our mental processes to attend to this external stimulus. This ability of switching from one to another mental task is the cognitive flexibility. Such flexibility can predict reading ability, academic success, resilience to stress, creativity, and lower risk of various neurological and psychiatric disorders. To shed light on the development of this critical cognitive process during early infancy, researchers at the UNC Biomedical Research Imaging Center (BRIC) at the UNC School of Medicine conducted a brain imaging study in infants to examine the emergence of neural flexibility, which refers to the frequency with which a brain region changes its role (or allegiance to one functional network to another). Neural flexibility is thought to underlie cognitive flexibility.
Publishing their work in the Proceedings of the National Academy of Sciences (PNAS), the researchers show that brain regions with high neural flexibility appear consistent with the core brain regions that support cognitive flexibility processing in adults, whereas brain regions governing basic brain functions, such as motor skills, exhibit lower neural flexibility in adults, demonstrating the emergence of functionally flexible brains during early infancy.
For this study, the authors used magnetic resonance imaging to examine brain activity up to seven times in 52 typically developing infants under the age of two during natural sleep. The researchers, led by Weili Lin, PhD, director of BRIC, the Dixie Lee Boney Soo Distinguished Professor of Neurological Medicine, and Vice Chair of Basic Research in the UNC Department of Radiology, found that neural flexibility increased with age across the whole brain, and specifically in brain regions that control movement, potentially enabling infants to learn new motor skills. Neural flexibility also increased with age in brain regions involved in higher-level cognitive processes, such as attention, memory, and response inhibition, indicating continuing development of these functional networks as babies become toddlers.
The age-related increase in neural flexibility was highest in brain regions already implicated in cognitive flexibility in adults, suggesting that cognitive flexibility may start to develop during the first two years of life.
“Neural flexibility in these brain regions may reflect early developmental processes that support the later emergence of cognitive flexibility,” Lin said. “What we’ve imaged, in essence, is the brain’s flexibility setting the stage for later maturity of higher cognitive brain functions.”
Additional analysis of brain regions with especially high neural flexibility revealed the presence of relatively weak and unstable connections from these regions to other parts of the brain, potentially showing how these regions can rapidly switch their allegiances between different functional networks. By contrast, neural flexibility in brain regions involved in visual functions remained relatively low throughout the first two years of life, suggesting that these regions had already matured. This image is of MRI data, showing neural flexibility over time. Image is credited to Biomedical Research Imaging Center at UNC-Chapel Hill. Lower levels of neural flexibility (i.e., greater established brain maturity) of visual brain regions at three and 18 months of age were associated with better performance on cognitive and behavioral assessments at the age of five or six years.
These findings provide insights into the development of higher-level brain functions, and could be used to predict cognitive outcomes later in life. The developed approach of assessing neural flexibility non-invasively could also provide a new means to assess subjects with neurodevelopmental disorders.
First author of this study is BRIC postdoctoral researcher Weiyan Yin, PhD. Other authors aside from Yin and Lin include Sheng-Che Hung, MD, clinical instructor of radiology; Han Zhang, PhD, assistant professor of radiology; Li Wang, PhD, research assistant professor of radiology; Dinggang Shen, PhD, Director of the UNC BRIC Image Analysis Core and professor of radiology, Hongtu Zhu, PhD, Peter Mucha, PhD, professor of mathematics and applied physical sciences; and Jessica Cohen, PhD, assistant professor of psychology and neuroscience, all at UNC-Chapel Hill. All but Mucha are members of BRIC.
Funding: The National Institutes of Health funded this work.
About this neurodevelopment research article
Source:
University of North Carolina Health Care
Contacts:
Mark Derewicz – University of North Carolina Health Care
Image Source:
The image is credited to Biomedical Research Imaging Center at UNC-Chapel Hill.
Original Research: Open access
“The emergence of a functionally flexible brain during early infancy” by Weili Lin et al. PNAS .
Abstract
The emergence of a functionally flexible brain during early infancy
Adult brains are functionally flexible, a unique characteristic that is thought to contribute to cognitive flexibility. While tools to assess cognitive flexibility during early infancy are lacking, we aimed to assess the spatiotemporal developmental features of “neural flexibility” during the first 2 y of life. Fifty-two typically developing children 0 to 2 y old were longitudinally imaged up to seven times during natural sleep using resting-state functional MRI. Using a sliding window approach, MR-derived neural flexibility, a quantitative measure of the frequency at which brain regions change their allegiance from one functional module to another during a given time period, was used to evaluate the temporal emergence of neural flexibility during early infancy. Results showed that neural flexibility of whole brain, motor, and high-order brain functional networks/regions increased significantly with age, while visual regions exhibited a temporally stable pattern, suggesting spatially and temporally nonuniform developmental features of neural flexibility. Additionally, the neural flexibility of the primary visual network at 3 mo of age was significantly and negatively associated with cognitive ability evaluated at 5/6 y of age. The “flexible club,” comprising brain regions with neural flexibility significantly higher than whole-brain neural flexibility, were consistent with brain regions known to govern cognitive flexibility in adults and exhibited unique characteristics when compared to the functional hub and diverse club regions. Thus, MR-derived […]
Scientists show how brain flexibility emerges in infants
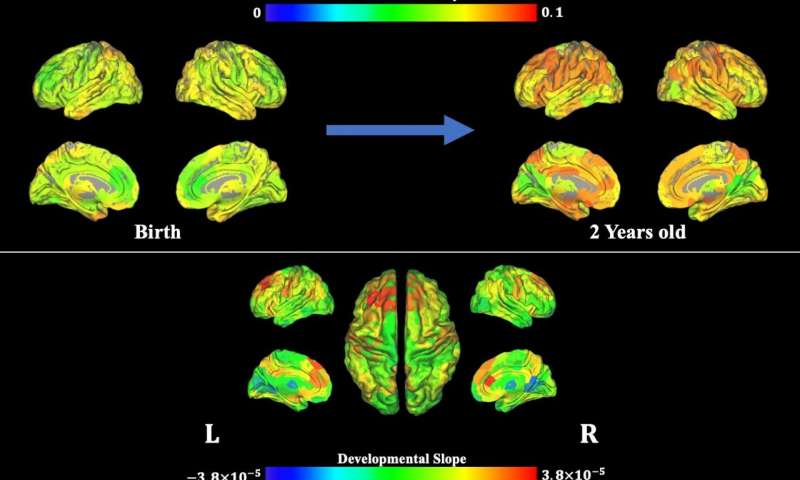
This image is of MRI data, showing neural flexibility over time. Credit: Biomedical Research Imaging Center at UNC-Chapel Hill. Cognitive flexibility refers to the ability to readily switch between mental processes in response to external stimuli and different task demands. For example, when our brains are processing one task, an external stimulus is present, requiring us to switch our mental processes to attend to this external stimulus. This ability of switching from one to another mental task is the cognitive flexibility. Such flexibility can predict reading ability, academic success, resilience to stress, creativity, and lower risk of various neurological and psychiatric disorders. To shed light on the development of this critical cognitive process during early infancy, researchers at the UNC Biomedical Research Imaging Center (BRIC) at the UNC School of Medicine conducted a brain imaging study in infants to examine the emergence of neural flexibility, which refers to the frequency with which a brain region changes its role (or allegiance to one functional network to another). Neural flexibility is thought to underlie cognitive flexibility.
Publishing their work in the Proceedings of the National Academy of Sciences (PNAS) , the researchers show that brain regions with high neural flexibility appear consistent with the core brain regions that support cognitive flexibility processing in adults, whereas brain regions governing basic brain functions, such as motor skills, exhibit lower neural flexibility in adults, demonstrating the emergence of functionally flexible brains during early infancy.
For this study, the authors used magnetic resonance imaging to examine brain activity up to seven times in 52 typically developing infants under the age of two during natural sleep. The researchers, led by Weili Lin, Ph.D., director of BRIC, the Dixie Lee Boney Soo Distinguished Professor of Neurological Medicine, and Vice Chair of Basic Research in the UNC Department of Radiology, found that neural flexibility increased with age across the whole brain, and specifically in brain regions that control movement, potentially enabling infants to learn new motor skills. Neural flexibility also increased with age in brain regions involved in higher-level cognitive processes, such as attention, memory, and response inhibition, indicating continuing development of these functional networks as babies become toddlers.
The age-related increase in neural flexibility was highest in brain regions already implicated in cognitive flexibility in adults, suggesting that cognitive flexibility may start to develop during the first two years of life.
“Neural flexibility in these brain regions may reflect early developmental processes that support the later emergence of cognitive flexibility,” Lin said. “What we’ve imaged, in essence, is the brain’s flexibility setting the stage for later maturity of higher cognitive brain functions.”
Additional analysis of brain regions with especially high neural flexibility revealed the presence of relatively weak and unstable connections from these regions to other parts of the brain, potentially showing how these regions can rapidly switch their allegiances between different functional networks. By contrast, neural flexibility in brain regions involved in visual functions remained relatively low throughout the first two years of life, suggesting that these regions had already matured.
Lower levels of neural flexibility (i.e., greater established brain maturity) of visual brain regions at three and 18 months of age were associated with better performance on cognitive and behavioral assessments at the age of five or six years.
These findings provide insights into the development of higher-level brain functions, and could be used to predict cognitive outcomes later in life. The developed approach of assessing neural flexibility non-invasively could also provide a new means to assess subjects with neurodevelopmental disorders.
Provided by University of North Carolina Health Care
Research shows how brain flexibility emerges in infants

North Carolina : To shed light on the development of cognitive flexibility during early infancy, researchers conducted a brain imaging study in infants to examine the emergence of neural flexibility, which refers to the frequency with which a brain region changes its role (or allegiance to one functional network to another).
Cognitive flexibility refers to the ability to readily switch between mental processes in response to external stimuli and different task demands. For example, when our brains are processing one task, an external stimulus is present, requiring us to switch our mental processes to attend to this external stimulus. This ability to switch from one to another mental task is cognitive flexibility. Such flexibility can predict reading ability, academic success, resilience to stress, creativity, and lower risk of various neurological and psychiatric disorders. Neural flexibility is thought to underlie cognitive flexibility.
Publishing their work in the Proceedings of the National Academy of Sciences (PNAS), the researchers show that brain regions with high neural flexibility appear consistent with the core brain regions that support cognitive flexibility processing in adults, whereas brain regions governing basic brain functions, such as motor skills, exhibit lower neural flexibility in adults, demonstrating the emergence of functionally flexible brains during early infancy.
For this study, the authors used magnetic resonance imaging to examine brain activity up to seven times in 52 typically developing infants under the age of two during natural sleep.
The research, led by Weili Lin, PhD, director of BRIC, the Dixie Lee Boney Soo Distinguished Professor of Neurological Medicine, and Vice-Chair of Basic Research in the UNC Department of Radiology, found that neural flexibility increased with age across the whole brain, and specifically in brain regions that control movement, potentially enabling infants to learn new motor skills.
Neural flexibility also increased with age in brain regions involved in higher-level cognitive processes, such as attention, memory, and response inhibition, indicating continuing development of these functional networks as babies become toddlers.
The age-related increase in neural flexibility was highest in brain regions already implicated in cognitive flexibility in adults, suggesting that cognitive flexibility may start to develop during the first two years of life.
“Neural flexibility in these brain regions may reflect early developmental processes that support the later emergence of cognitive flexibility,” Lin said. “What we`ve imaged, in essence, is the brain`s flexibility setting the stage for later maturity of higher cognitive brain functions.”
Additional analysis of brain regions with especially high neural flexibility revealed the presence of relatively weak and unstable connections from these regions to other parts of the brain, potentially showing how these regions can rapidly switch their allegiances between different functional networks. By contrast, neural flexibility in brain regions involved in visual functions remained relatively low throughout the first two years of life, suggesting that these regions had already matured.
Lower levels of neural flexibility (ie, greater established brain maturity) of visual brain regions at three and 18 months of age were associated with better performance on cognitive and behavioural assessments at the age of five or six years.
These findings provide insights into the development of higher-level brain functions and could be used to predict cognitive outcomes later in life. The developed approach of assessing neural flexibility non-invasively could also provide a new means to assess subjects with neurodevelopmental disorders.
Autumn blues? Try adding these 5 mood-boosting foods to your daily diet

Goodbye summer.
September is pretty much here. It is (pretty) cold, it is wet, it is still pretty dark when we wake up in the mornings, and honestly; who isn’t feeling just a little bit blah right about now? I mean, it doesn’t help that we are all over the place emotionally after the year we have all had either.
2020 has – and still is – the most unprecedented year any of us have ever lived through. And some days, things just feel pretty bleak, no?
The good news?
It is a lot easier to snap out of a funk if you are eating the right foods. It’s true. So before you pour yourself another coffee and tear the wrapping off a Snickers bar, know this: The food you eat when you are feeling sad, anxious, moody and stressed can end up doing two things: Either help pick you up – or keep on dragging you down.
So choose wisely.
These five foods are all known to have a positive effect on our mood and our feelings, and will do great things for your overall health too:
1. Green tea
Instead of your usual latte in the morning, try making yourself a cup of green tea. Sipping on something hot in general is soothing, and the perfect thing to be doing if you are feeling either stressed or anxious. And there are more benefits too. Studies, like this one published in American Journal of Clinical Nutrition , shows that green tea contains many mood-boosting nutrients including the amino acid L-theanine, which has been linked to reducing symptoms of depression and anxiety. 2. Greek, full-fat yoghurt
Eating a good and wholesome breakfast is always a good idea if you are looking to boost your mood and feel better. Greek yoghurt is an excellent choice as it has a healthy serving of protein to keep you full for longer (limiting any blood sugar crashes) and also, from a mood point of view, because it contains calcium. Calcium can have a major effect on mood regulation, as it plays a major role in releasing feel-good chemicals from your brain.
Eating calcium-rich foods is also advised if you suffer from PMS, as research has shown that calcium actually can help you cope with some of the symptoms related with the condition. A study of women taking 500 milligrams (mg) of calcium carbonate twice a day for 3 months found they had less fatigue, fewer changes in appetite, and less depression than women with PMS who did not take the supplement. 3. Wild salmon
Omega-3s are good for you in so many ways, also because these nutrients alter brain chemicals linked with mood —specifically dopamine and serotonin. To load up on these natural feel-good boosters, try eating a piece of wild salmon for dinner several times a week. Alternatively, flaxseeds are another great option to load up on plant-based Omega-3s. Try to add some to a smoothie, sprinkle on your cereal or just stir a handful into a soup or stew. 4. Blueberries
Berries, in general, are great, but none more so than blueberries when it comes to a type of antioxidant called flavonoids, which are known to help regulate mood, improve memory, and even help protect the brain from ageing.
According to research , blueberries help activate brain pathways associated with better cognition and cellular regulation, and researchers argue this anti-inflammatory superfood may also be helpful in treating PTSD and other serious mental health issues . 5. Spinach
Feeling down? You need to uptake your intake of magnesium now, experts agree . Not only because this mineral is essential for increasing your energy, relax the muscles and support brain function, but magnesium is also well-known for its mood-boosting properties.
Some of the best dietary sources of magnesium are dark leafy greens, such as spinach, kale and Swiss Chard. As well as these, try including more beans and lentils, pumpkin seeds and almonds into your diet too, and you’ll soon notice a difference.
The Big List of Nootropics

This is a comprehensive list of the most popular Nootropics in use today. Here you’ll learn what the nootropic is, what it does and suggested dosages.
If you are new to the world of Nootropics, you may be wondering the best way to use a particular compound. You’ll find that here.
If you are an experienced neurohacker this is a great quick reference guide.
You’ll find the full scope of benefits of each Nootropic. Its specific mechanism of action. How safe it is. And suggestions on pairing it with other Nootropics for your stack.
A word of caution – always start off with the lowest effective dose of any supplement. Each of our bodies is different so you need to find out the effects of each nootropic in your body. And how it will benefit you.
Acetyl L-Carnitine (ALCAR)
Acetyl L-Carnitine ((R)-3-Acetyloxy-4-trimethylammonio-butanoate) is an acetylated form of L-Carnitine. A derivative of the amino acid lysine which is naturally produced in your liver and kidneys. This synthesized form can easily cross the blood-brain barrier.
ALCAR is a nootropic because it targets your brain metabolism, boosts mitochondria energy, and acts as a neuroprotectant. Acetyl L-Carnitine protects neurotransmitters which makes it a powerful compliment to boost the effectiveness of other nootropics.
Acetyl-l-carnitine boosts memory, mental alertness, fluid thought, and is a strong antioxidant.
The usual suggested dosage for ALCAR is 500 – 1,500 mg per day.
Learn more about Acetyl-L-Carnitine
Alpha-GPC
Alpha GPC (alpha-glycerylphosphorylcholine) is found naturally in your brain. It is a precursor to acetylcholine – an essential neurotransmitter involved in memory, cognition, sleep and muscular control.
As a nootropic, Alpha GPC easily crosses the blood-brain barrier. It boosts acetylcholine levels in your brain contributing to improved memory, cognition, learning and focus. And protects against age-related memory loss.
You get Alpha GPC from raw beef liver, cod fish, spinach, milk, soy and eggs. As a supplement, Alpha GPC derived from soy or sunflower lecithin is a more efficient way of boosting acetylcholine in your brain.
Recommended daily dosage for Alpha GPC is 600 mg.
Alpha-Lipoic Acid (ALA)
Alpha-Lipoic Acid used as a nootropic is a synthetic version of lipoic acid. A compound naturally occurring in your body. This antioxidant is necessary for cellular energy production. And helps eliminate the free radicals created when nutrients convert to cellular energy.
ALA boosts energy levels, protects brain cells from free radical damage, and improves memory.
Recommended dosage for Alpha-Lipoic Acid is 200 – 400 mg per day.
Aniracetam
Aniracetam (1-(4-methoxybenzoyl)-2-pyrrolidinone) is an N-side chain derivative of piracetam. It is thought to be 5 to 8-times more potent than piracetam. Aniracetam is fat-soluble and has a shorter half-life compared to other racetams.
A potent nootropic, Aniracetam reduces anxiety and depression with no sedative effects. It seems to do this by activating the D2 and D3 Dopamine receptors in the brain. Aniracetam helps improve memory, learning, cognition, along with heightened reflexes and perception.
Dosing aniracetam is 750 – 1,500 mg per day. Do half your daily dose twice per day.
Ashwagandha
Ashwagandha has been used in Ayurvedic medicine for several thousand years. In Sanskrit it literally means “the smell of a horse” which implies this herb provides the vigor and strength of a stallion.As a nootropic, Ashwagandha helps relieve stress, fatigue, restore energy and boosts concentration. As an adaptogen, it helps your entire body by normalizing blood sugar, boosts insulin sensitivity, works as an antioxidant, promotes breast, lung and colon health, and protects against inflammation.The typical recommended dose of Ashwagandha is 250 – 500 mg per day.Artichoke Extract (Luteolin)Artichoke Extract is a PDE4 inhibitor. PDE4 is an enzyme that breaks down cAMP molecules (messenger systems that relay signals in the brain). Stopping PDE4 then prevents the breakdown of cAMP.
