Learn about brain health and nootropics to boost brain function
Brain Wave Study Reveals Secrets of Unconsciousness
Spelunking the depths of unconsciousness may have gotten a notch easier, as researchers from MIT unveil a pioneering study on how general anesthetics affect our brain waves. New markers of brain wave activity could allow anesthetists to stop patients from entering a deeper state of unconsciousness, called burst suppression, which is linked to impaired cognition post-anesthesia.
The new research, produced by a team at MIT, was published in the Proceedings of the National Academy of Sciences . What goes on when we go under?
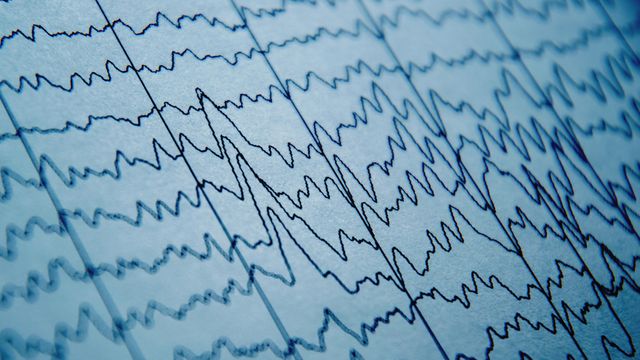
The researchers used a technique called electroencephalography (EEG) to analyze the brain waves of 10 healthy volunteers and 30 people who were to be put under general anesthesia for surgery. Most patients were dosed with the anesthetic propofol, which is administered intravenously. Others were given sevoflurane, an anesthetic gas.
The team wanted to understand how these anesthetics alter brain waves. These are synchronized patterns of activity that are produced by groups of neurons. Depending on what the brain is doing, different brain wave oscillations emerge. When we are engaged in challenging cognitive tasks, our brains emit high-frequency beta (15–30 hertz) and gamma (above 30 hertz) wave patterns.
But when we are put under anesthetics, these patterns are drastically altered. These anesthetics increase the output of inhibitory receptors in the brain that respond to the neurotransmitter GABA. This sends the brain into an unconscious state called slow-delta-alpha (SDA). In this state, much slower brain waves predominate; delta brain waves have a frequency of 1–4 hertz, while alpha waves oscillate at 8–14 hertz. Want more breaking news?
Subscribe to Technology Networks ’ daily newsletter, delivering breaking science news straight to your inbox every day.
Subscribe for FREE
Neuroscientists have previously studied both burst suppression and SDA, identifying distinct patterns of brain activity using EEG for both states. However, what occurs in the transition from one state to another has, so far, remained unclear.
But Brown and his team have now produced some insight. Slow waves
The team noted that as patients became unconscious, their alpha waves started to vary in amplitude in a distinctive pattern. Emery Brown, the Edward Hood Taplin Professor of Medical Engineering and Computational Neuroscience and a member of MIT’s Picower Institute for Learning and Memory and the Institute for Medical Engineering and Science, said, “If you track this modulation as it gets deeper or shallower, you have a very principled way to track level of unconsciousness under anesthesia.” When patients entered burst suppression, this pattern started to change. Alpha wave activity started to gradually decrease in amplitude. “You can see a very strong modulation, which is always there. As the modulation gets to be more profound, it eventually flattens out, and that’s when the brain reaches the deeper state,” Brown added. When propofol levels were decreased, the alpha waves’ amplitude began to increase once again.
Similar marker patterns were seen in delta waves. The team noted from patients’ EEG recordings that these brain waves, already the slowest brain wave category, lowered their frequency even further, indicating a decrease in brain activity.
Post-operation, patients who have entered burst suppression are more likely to experience adverse side effects, like memory loss and confusion. In rare cases, these side effects can last for months and are more likely to affect elderly patients, making a reliable indicator of burst suppression entry a useful tool. No energy, no activity
The researchers have begun to speculate how these drugs might exert such effects. Brown suggests that neuron metabolism is key. Propofol is thought to disrupt the production of a molecule called ATP, which cells use as an energy store. With fewer energy reserves available, neurons lose the ability to fire, decreasing activity. “This is consistent with the observation that burst suppression is very frequent in older patients, because their metabolic state may be less well-regulated than that of younger patients,” said Brown.
The team now wants to explore the mechanisms involved further and feed this data into an algorithm that could sound off automatic warnings to anesthetists as their patients enter burst suppression, allowing them to fine-tune anesthetic levels. Physicians could even be trained to spot the regimented burst suppression patterns themselves by looking at an EEG readout. “One of the reasons we’re excited about this is that it’s something you can actually see in the raw EEG,” Brown said. “Now that we have pointed out these patterns, they’re very easy to see.”
Reference : Adam E, Kwon O, Montejo KA, Brown EN. Modulatory dynamics mark the transition between anesthetic states of unconsciousness. Proceedings of the National Academy of Sciences. 2023;120(30):e2300058120. doi: 10.1073/pnas.2300058120
This article is a rework of a press release issued by MIT. Material has been edited for length and content.
Read more at www.technologynetworks.com