Learn about brain health and nootropics to boost brain function
‘Night owls’ have 13.5% better brain function than early risers

Being a night owl might not be a bad thing – for your brain, at leastDepositphotos ‘Night owls’ traditionally get a bit of a rough time of it, with numerous studies linking staying up late to poor health outcomes, inadequate sleep and a fair amount of shame that comes with not being able to function as well in the mornings as others. And, in a world where work hours generally favor early risers, the late-night folk can feel a little out of step with society.
But there’s finally some good news for those who can’t, or don’t want to, go to bed at a ‘reasonable hour,’ with Imperial College London (ICL) scientists finding that night owls have significantly greater brain function than their early-rising counterparts. So, if you’re in that camp of believing the day doesn’t truly start until 5pm, this one is for you.
“Our study found that adults who are naturally more active in the evening (what we called ‘eveningness’) tended to perform better on cognitive tests than those who are ‘morning people,'” said the study’s lead author Raha West, from the Department of Surgery and Cancer at ICL. “Rather than just being personal preferences, these chronotypes could impact our cognitive function.”
Previous studies have associated ‘eveningness’ to detrimental health outcomes, including putting them at greater risk of type 2 diabetes and heart disease , and even a 10% higher risk of early death compared to ‘morning people.’ Night owls have also been linked to having a higher rate of psychological and neurological disorders .
Genetics studies have indicated that morning-night sleep preferences is closely tied to our biology , with variants associated with a shift in circadian rhythms that play a big role in when we feel we need to sleep. This is, of course, still very much a work in progress, but we do know that night-owl behavior is complex and not just governed by personal choice or willpower.
Recently, it’s even been tied to evolution, linking attention-deficit/hyperactivity disorder (ADHD) and ‘eveningness’ with something deemed the Watchman Theory . It suggests that for the nearly three quarters of ADHD sufferers who report sleep problems, including “bedtime resistance,” it might be traced back to hunter-gatherer days, when those genes and time-shifted circadian rhythms made a certain group of people excellent at keeping watch over tribes late into the night.
Whatever the driver, being a night owl might come with some benefits after all. In this latest study, researchers looked at more than 26,000 UK Biobank participants and their sleep habits – including duration and quality – and how they performed on cognitive tests. These participants also self-described themselves as morning or night people.
After adjusting for health and lifestyle factors, such as chronic disease, smoking and alcohol intake, the researchers found that night owls scored around 13.5% higher than morning people in one group, and 7.5% higher in another group. What’s more, morning people had consistently lower test scores across the board, with even the ‘intermediate’ types – those who considered themselves more somewhere in the middle – doing 10.6% and 6.3% better than early risers.
“It’s important to note that this doesn’t mean all morning people have worse cognitive performance,” said West. “The findings reflect an overall trend where the majority might lean towards better cognition in the evening types. While it’s possible to shift your natural sleep habits by gradually adjusting your bedtime, increasing evening light exposure, and keeping a consistent sleep schedule, completely changing from a morning to an evening person is complex.”
But key to the findings also appears to be the amount of sleep per night – which is probably not such a surprise. In their findings, the researchers noted that between seven and nine hours of shut-eye is best for our brains, particularly in connection with memory and information processing speed. However, they also found that getting more than nine hours was actually linked to poorer brain function.
And in another surprising outcome of the study, those who reported suffering from insomnia didn’t show a significant drop in brain function as a result of poor sleep. But the scientists said this was likely more nuanced, with the findings not factoring in the duration or severity of insomnia.
“While understanding and working with your natural sleep tendencies is essential, it’s equally important to remember to get just enough sleep, not too long or too short,” said West. “This is crucial for keeping your brain healthy and functioning at its best.”
So, what does this mean for night owls? Staying up late may be better for brain performance than rising early – as long as you’re able to hit the sweet spot of seven to nine hours of sleep. Which, of course, can be challenging with external factors such as work and family commitments.
Previous research has also looked at interventions such as strobe-light therapy to help night owls get better-quality and enduring sleep, to help with daytime function.
“We’ve found that sleep duration has a direct effect on brain function, and we believe that proactively managing sleep patterns is really important for boosting, and safeguarding, the way our brains work,” said study co-leader Daqing Ma, a professor in ICL’s Department of Surgery and Cancer. “We’d ideally like to see policy interventions to help sleep patterns improve in the general population.”
The study was published in the journal BMJ Public Health .
Source: ICL
Ultrasound technology can be used to boost mindfulness, study finds
One of the intriguing abilities of the human mind is daydreaming, where the mind wanders off into spontaneous thoughts, fantasies and scenarios, often without conscious effort, allowing creativity and reflection to flow freely.
In a new study published in Frontiers of Human Neuroscience , University of Arizona researchers used low-intensity ultrasound technology to noninvasively alter a brain region associated with activities such as daydreaming, recalling memories and envisioning the future. They found that the technique can ultimately enhance mindfulness, marking a major advancement in the field of neuroscience.
The researchers used low-intensity ultrasound technology called transcranial-focused ultrasound or, TFUS, to alter the default mode network of the brain, a system of connected brain areas that are especially active during activities like daydreaming.
“We are the first to show that the default mode network can be directly targeted and noninvasively modulated,” said lead study author Brian Lord, a postdoctoral researcher in the U of A Department of Psychology.
One area of the default mode network, the posterior cingulate cortex, has been implicated as a major player in how the mind grasps onto experiences, said Lord, who is part of the Science Enhanced Mindfulness Lab, or SEMA Lab, at the university’s Center for Consciousness Studies. The default mode network is active when people engage in introspection or let their minds wander, perhaps embedding themselves in a story, recalling past memories or planning future scenarios.
“This is how we form narratives about ourselves,” Lord said.
While this narrative making is natural and important to get a coherent sense of oneself, it can also impede people from being present in the moment, Lord said. For instance, when someone is trying to meditate, it could lead to rumination and negative thinking.
To enhance mindfulness and help people engage more with the current moment, Lord’s team used TFUS, a tool that can stimulate specific areas of the brain noninvasively with millimeter precision.
Unlike other noninvasive brain stimulation methods, such as transcranial electrical stimulation and transcranial magnetic stimulation, TFUS can penetrate below the cortex, the outermost layer of the brain. Just five minutes of stimulation can induce meaningful effects.
The experiment involved 30 participants who received TFUS to the posterior cingulate cortex of the default mode network of the brain. Researchers used functional magnetic resonance imaging, or fMRI, to observe changes in brain activity. Participants were asked to report their feelings and experiences before and after the TFUS treatment.
The study found that TFUS reduced the brain’s connectivity within the default mode network and affected participants’ mindfulness and subjective experiences, such as their sense of self and perception of time.
“The best part is you are using a minimal amount of energy to alter brain activity. You are just giving a gentle push to the brain with low-intensity ultrasound,” Lord said.
The ability to target and alter brain networks opens the possibility of using TFUS for precision therapeutics, which are medical treatments tailored specifically to an individual’s unique characteristics, such as their genetic makeup, lifestyle and environment. TFUS could also potentially be used to treat mood disorders like depression and anxiety, a possibility other research groups are now exploring, Lord said.
“Unlike neuroimaging techniques where you can only make correlations with brain activity, noninvasive stimulation tools like TFUS allow you to probe the brain and develop causal models,” Lord said. “That’s a really powerful thing for the whole field of neuroscience.”
Story Source:
Materials provided by University of Arizona . Original written by Niranjana Rajalakshmi. Note: Content may be edited for style and length.
Mind Over Matter: Sculpt Your Brain, Transform Your Future
Key points
Research suggests that heavy reliance on technology may change brain structure and reduce grey matter density.
People can shape their brains through intentional actions to maintain mental agility and resilience.
Engaging in mentally stimulating activities with new skills can strengthen cognitive function and well-being.
By balancing technology use with mental activities, people can optimize brain health and cognitive abilities.
Empowering the mind Source: DALL-E 2/OpenAI
Recent fossil and skull studies reveal a surprising trend: Despite a fourfold increase in brain size starting around 2 million years ago, which coincided with major advancements in tool use, social structures, and cognitive abilities, human brains have shrunk by nearly 10 percent over the past few thousand years (DeSilva et al., 2021, 2023). This discovery suggests that as societies became more complex, we developed ways to store information externally through language, writing, and other tools, reducing the need for a massive brain. But what does this mean for us today?
While brain size isn’t everything, this ongoing research raises intriguing questions about intentionally optimizing our well-being. This raises the fascinating possibility: Might we be able to take proactive steps to boost brain power, shape our mental well-being, and maximize our resiliency? Lessons from highly social insects and beyond
Charles Henry Turner, a pioneering entomologist, revealed in the late 19th and early 20th centuries that ants could learn from their experiences and adapt their behaviors, including following and learning from the trails left by other ants (Turner, 1907). This work highlights how species shape their environments together, learn from each other, and adapt to their surroundings, promoting ongoing learning and driving evolution. In environments with shared knowledge and cooperative roles, larger brains become less necessary, while adaptability and varied cognitive approaches are key to thriving. Beyond ants, humans, and termites, species such as domesticated animals like dogs, cats, and livestock, as well as certain birds and fish, have also shown trends of shrinking brain sizes over time when environmental pressures for complex problem-solving and survival diminish (Kruska, 2005; Sol, 2009; Kotrschal et al., 2013). Social insects like ants show that brain size correlates with task complexity. Source: DALL-E 2/OpenAI Personal neuroplasticity: Shaping our brains with intentional action
While evolutionary changes occur over millennia, we have the power to shape our brains within our lifetimes through the brain’s ability to reorganize itself by forming new neural connections. Our experiences and the ways we engage with them can enhance or diminish specific brain functions. This means that the intentional actions we take daily can significantly impact our mental and physical well-being.
For example, if we constantly rely on technology for memory and problem-solving, we may weaken our intrinsic cognitive abilities. Conversely, engaging in mentally stimulating activities can strengthen and expand our cognitive capacities.
A simple yet effective way to do this is to challenge your brain with new routines. Try switching the hand you use for everyday tasks, like brushing your teeth or stirring your coffee. It might feel awkward at first, but this seemingly insignificant change forces your brain to create new neural pathways, enhancing its flexibility and resilience . Cultivating intentional actions
While directly increasing brain size in adults through current means isn’t possible, there are ways to improve brain function that can feel similar to having a “bigger brain.” Indeed, we can build our brain’s capacity to process information and perform tasks more efficiently to significantly enhance its power.
In today’s fast-paced world, bombarded by distractions and information overload, prioritizing brain health is essential. Here are some strategies to help us sharpen our focus, optimize cognitive function, and unlock our full mental potential:
> Engage in mentally stimulating activities: Regularly challenge your brain with new skills, puzzles, and problem-solving tasks. This can enhance cognitive flexibility and resilience.
Become present through your senses: Studies show that focusing on your individual senses can act as an anchor to the present moment (Kabat-Zinn, J., 1990). Take a deep breath and notice the subtle aromas in the air. Listen intently to the sounds around you, identifying each distinct noise. Try focusing on a single object and describing it in detail, noticing every color, texture, and nuance. This sensory engagement can enhance your focus and awareness, potentially improving brain function in learning, memory, and emotional regulation .
Physical activity: Regular exercise promotes neurogenesis and improves overall brain function. It also counteracts the sedentary lifestyle encouraged by modern technology.
Foster social connections: Meaningful social interactions can boost mental health and cognitive function, mirroring the cooperative behaviors that have historically shaped human evolution.
Balance technology use: Use technology mindfully. While it can enhance efficiency, ensure it doesn’t replace critical thinking and memory exercises.
Reflections on technology and its long-term impact
Technological advancements have undeniably improved our quality of life, but they come with long-term implications. Tools like smartphones and the internet have become extensions of our memory and problem-solving abilities. While this externalization can enhance efficiency, it may reduce our reliance on intrinsic cognitive functions, potentially influencing brain size and function over generations.
Mounting evidence suggests that engaging experiences and technologies can reshape our brains. Activities that challenge our learning, like learning to juggle, can increase the density of gray matter in our brains (Draganski et al., 2004). This principle extends to other activities that challenge memory and cognitive function, such as learning a new language.
Conversely, overreliance on external tools for tasks like navigation or calculations might decrease gray matter density in responsible brain areas. Similarly, the overuse of technology for navigation or passive screen time could shrink the occipital lobe, which is responsible for vision, potentially hindering our ability to navigate independently or appreciate visual details. Moving forward with intention
As we ride the wave of technological advancements, it’s vital to reflect on how this digital revolution will shape our species over time. While directly increasing brain size might not be currently possible, it is crucial to consider our engagement with technology and its impacts on our cognitive function and brain structure.
As a social species, embracing our interconnectedness and leveraging […]
Novel method may erase ‘bad memory’ response to long-term Parkinson’s treatment

Scientists have found a novel method that may prevent a side effect of certain Parkinson’s therapies. Rob and Julia Campbell/Stocksy Researchers at the University of Alabama in Birmingham have discovered a promising method to prevent dyskinesia, a debilitating side effect of long-term Parkinson’s treatment.
By treating dyskinesia as a “bad motor memory” and blocking the protein Activin A, they managed to halt the development of these uncontrollable movements in mouse models.
This breakthrough could extend the effectiveness of current Parkinson’s treatments and significantly improve patients’ quality of life.
Common treatments for Parkinson’s disease can alleviate short-term symptoms but may lead to significant long-term issues for patients.
Specifically, these treatments can induce dyskinesia , characterised by involuntary movements and postures.
In a recent study, published in The Journal of Neuroscience , researchers adopted a novel approach to dyskinesia by treating it as a “bad motor memory.”
They discovered that inhibiting a protein called Activin A could stop dyskinesia symptoms and essentially erase the brain’s “bad memory” response to certain Parkinson’s therapies.
Rather than seeking an entirely new treatment, researchers aimed to find a way to prevent dyskinesia from developing in the first place.
If dyskinesia does not occur, patients could potentially continue their Parkinson’s treatment for a longer duration. L-DOPA, a treatment for Parkinson’s disease, may induce dyskinesia
Parkinson’s disease is a neurodegenerative disorder caused by the death of dopamine-producing neurons.
To address this dopamine deficiency, clinicians currently prescribe L-DOPA, a precursor to dopamine.
While L-DOPA is beneficial in the short term, it can cause L-DOPA-induced dyskinesia in some patients over the long term, leading to involuntary, erratic movements such as twitching, fidgeting, head-bobbing or body swaying.
Even if a patient discontinues L-DOPA temporarily, dyskinesia often quickly recurs when treatment is resumed.
It appeared that the brain was creating a motor memory, recalling it with each subsequent L-DOPA treatment.
Given the similarities between motor and behavioural memory, the team decided to treat dyskinesia as if it were a bad memory. Treating dyskinesia as a ‘bad motor memory’
If they could find a way to make the brain forget its previous treatment history, they might extend the effectiveness of L-DOPA for Parkinson’s treatment.
Researchers began by examining the striatum, a brain region crucial for motor control, to identify which cells were storing the “bad motor memory.”
They observed the most significant changes in neurons called D1-MSNs, which behaved similarly to neurons in the hippocampus when forming a memory.
They discovered that some D1-MSNs expressed genes indicating activation by L-DOPA and the creation of new connections with other cells, similar to the process of learning and recalling new information.
One gene in these L-DOPA-activated D1-MSN neurons was found to translate into a protein called Activin A.
By inhibiting Activin A, researchers successfully prevented the development of L-DOPA-induced dyskinesia in mouse models.
Essentially, by blocking this protein’s function, they could stop dyskinesia symptoms from developing in the mouse models, effectively erasing the brain’s memory of the motor response to L-DOPA.
The ultimate goal is to use these findings to learn how to block these bad motor memories completely, eliminating dyskinesia-related symptoms in Parkinson’s patients.
Karen Jaunarajs , PhD, assistant professor in the UAB Department of Neurology at The University of Alabama at Birmingham explained the key findings to Medical News Today . “Our goal for this particular study was to lay the foundation for thinking about L-DOPA-induced dyskinesia as a form of bad motor memory by trying to figure out what cells were storing this memory. A lot of work has shown that a brain region important for motor memory, known as the striatum, is pivotally involved in the development of dyskinesias. But the brain is made up of many different types of cells, like neurons, supporting cells, and immune cells, that all respond differently following L-DOPA treatment. Which ones stored the drug history was unknown.”
— Karen Jaunarajs, PhD “Therefore, the primary goal of this study was to create a map of all the changes in gene expression from all of the different cells in the striatum across the development of L-DOPA-induced dyskinesia: from the first exposure to L-DOPA, to how that response evolves with repeated L-DOPA treatments,” Jaunarajs said.
“We used single-cell RNA sequencing to identify all of the gene expression changes that were happening in over 100,000 individual cells during dyskinesia development. By establishing a comprehensive profile of the changes in gene expression across all of the different types of cells in the striatum, we found that many of the most significant differences were in a certain type of neuron, called D1-MSNs,” she further explained. “We found that some of these D1-MSNs were expressing genes indicating that they were activated by L-DOPA and genes necessary for creating new connections with other cells. This was very similar to what happens when you learn something new and recall that memory. Furthermore, we noticed that lots of cells were initially activated by L-DOPA treatment; however, after repeated exposures, the number of these activated D1-MSNs decreased.”— Karen Jaunarajs, PhD “Although this seems a little backward,” Jaunarajs said, “this is a lot like what happens when you learn something new: initially, many cells are required to initially form a memory, however, as you get better at recalling the memory, your brain gets more efficient and fewer cells are necessary to retrieve it quickly.” Chandril Chugh , MD, adult and paediatric neurologist based in Patna, India, who was not involved in this research, told MNT that this manuscript “makes for an intriguing read where a common clinical problem of dyskinesias post syndopa treatment has been discussed.” “The authors have conducted an animal based study and demonstrated how striatal neurons behave after being exposed to dopamine stimulation. This study is helpful in enhancing our understanding of a common disease and enhance patient care and satisfaction.”— Dr. Chandril Chugh Potential implications for future Parkinson’s patients Jaunarajs highlighted several implications of this research.“First, one of the more exciting genes we found in these activated D1-MSNs is translated into a protein called Activin A. By blocking the function of Activin A, we […]
Trying Harder Increases Cognitive Effort and Enhances Memory

Key points
To successfully complete a hard task requires more cognitive effort.
In visuomotor tasks, more cognitive effort enhances working memory allocation.
Enhanced working memory allocation leads to improved recall and memory.
“It just got too hard,” says Geena Davis as Dottie Hinson in A League of Their Own . Baseball manager Jimmy Dugan (Tom Hanks), refutes Dottie’s explanation for quitting the game when he replies, “It’s supposed to be hard. If it wasn’t hard, everyone would do it. The hard is what makes it great.” In a game like baseball, and in just about everything humans do, the “hard” has to do with both observable physical effort and the cognitive effort that lies beneath. But what do we really know about cognitive effort and how it affects experience and memory ? How much holdover is there with hard effort?
Sarah Master, Shanshan Li, and Clayton Curtis of New York University and New York University Abu Dhabi wanted to better understand how cognitive effort might affect the strength and durability of working memory representations. This was predicated on the idea that “understanding of the neural mechanisms underlying our cognitive abilities depends on understanding their interplay with factors such as cognitive effort.” In simple terms, they designed an experiment that would assess “that some tasks require more effort than others and success depends on how hard we try.”
In a study published in the Journal of Neuroscience , these researchers had participants perform visual tasks that involved memorizing and later identifying a target location in easy conditions (which yielded fast response times) or difficult conditions (which had slower response times and triggered changes in pupil diameter). Participants were cued as to how challenging the upcoming task would be. In the analysis, the researchers “used fMRI to test how changes in cognitive effort, induced by changes in task difficulty, impact neural representations of working memory.” Increased effort makes it last.
While prefrontal cortex activity was elevated for hard trials, the effects of task difficulty were really clearly seen only in “patterns of activity in the visual cortex…where accuracy was higher on hard trials.” These results suggest that “effort-related feedback signals sculpt population activity in the visual cortex, improving mnemonic fidelity.” This work suggests that “cognitive effort—trying harder—improves the quality of working memory (WM) representations in the visual cortex mediated by feedback from the prefrontal cortex.” This means that working memory resources can be strategically allocated during visuomotor tasks. This is quite interesting in its own right, but as the researchers point out, there are important potential clinical applications for ” psychiatric disorders, such as schizophrenia, where motivational deficits may masquerade as cognitive dysfunction.” Going above and beyond pays off later.
For me, these observations resonate strongly with plasticity in all physiological systems. We operate day-to-day within a certain range of effort for our activities. We have over time adapted to these activities, and they have slowly shifted to, more or less, “easy.” It’s only when we push beyond and shift to “hard” that our bodies and brains adapt to the new operating range. This takes me way back to my first book, Becoming Batman , in which this featured as the key concept. If the activity is strength training, our muscles get bigger and stronger, and if it’s cognitive training, we enhance synaptic connectivity and memory representation. To get more, we do need to do more, and that means more effort is essential. Neurobiology really does show us that there is joy in effort and hard really does make it (a) great (memory).
(c) E. Paul Zehr (2024)
References
Trying Harder: How Cognitive Effort Sculpts Neural Representations During Working Memory. Sarah L. Master, Shanshan Li, Clayton E. Curtis. Journal of Neuroscience 10 July 2024, 44 (28) e0060242024; DOI: 10.1523/JNEUROSCI.0060-24.2024
Neuroscience Says 1 Brainless Move Will Boost Your Memory and Focus (and Lower Stress)

In the busyness of life, the quest for improved brain function and reduced stress has become increasingly important. Surprisingly, neuroscience research has uncovered a simple, “brainless” activity that can significantly enhance memory , sharpen focus, and lower stress levels. This technique requires no special equipment, can be done almost anywhere, and is accessible to people of all ages and fitness levels. The secret?
Walking. The Science Behind the Stride
Studies in neuroscience have shed light on the profound impact that walking has on our brains. Far from being a mere physical activity, walking engages multiple brain regions and triggers a cascade of neurological benefits. 1. Memory enhancement
One of the most significant benefits of walking is its effect on memory. A study published in the Proceedings of the National Academy of Sciences found that regular walking increases the size of the hippocampus, a brain region crucial for memory formation and spatial navigation. Participants who engaged in brisk walking for 40 minutes three times a week showed a 2 percent increase in hippocampal volume over a year, equivalent to reversing age-related loss by one to two years. 2. Improved focus
For the busy entrepreneur, squeezing in even a brief walk with a colleague can be a game-changer. Research shows that even mild exercise, like a mid-day stroll, sparks new connections between brain cells and boosts neuron growth, enhancing overall brain power.
In a long-term study published in Neurology , participants who walked more each week preserved more gray matter, which supports cognitive function, compared to those who were less active.
Research from the University of Illinois, as published in Cognition , found that taking short breaks, like going for a walk, can really help improve focus during intense work sessions. These breaks are important to prevent our brains from getting too used to tasks and to keep productivity and clarity high.
So, for entrepreneurs juggling countless responsibilities, integrating short, rejuvenating breaks and brief exercises into the day can significantly boost productivity and mental clarity. 3. Stress reduction
Perhaps one of the most welcome benefits of walking is its stress-reducing effects. One recent study published in the journal Environment and Behavior looked at how walking in nature affected mood and stress among college students.
They split folks into three groups: walking in nature, watching nature on TV, or hitting the treadmill indoors, both during relaxed times and exams. Turns out, walking in nature really reduces stress levels and lowers cortisol levels, the body’s primary stress hormone, more than other activities. Plus, it boosted mood way better than just watching nature scenes.
Bottom line? Getting outside for a stroll in nature can seriously lift your spirits and ease stress, especially when things get intense at school or work. Implementing the “brainless” move
The beauty of walking as a cognitive enhancer lies in its simplicity and accessibility. Many people can do it just about anywhere (unless you live in Antarctica). Here are some tips to maximize the brain-boosting benefits of your walks:
> Schedule walks: Treat your walks as important appointments. Block out time in your calendar, whether it’s for a morning stroll, a lunchtime walk, or an evening wander.
Aim for consistency: Try to incorporate at least 30 minutes of brisk walking into your daily routine. This can be broken up into shorter sessions throughout the day if needed.
Vary your environment: Alternating between urban and natural settings can provide different stimuli for your brain, enhancing cognitive flexibility.
Practice mindfulness: Make it a mindful walk. Pay attention to your surroundings, the sensation of your feet touching the ground, and your breathing.
Go social: Walking with a friend or joining a walking group can add a social dimension, which has its own set of cognitive benefits.
Incorporate walking meetings: If you have a meeting, suggest a walking meeting. It can make discussions more dynamic and boost creativity.
As we continue to search for ways to enhance our cognitive abilities and manage stress at work, it’s reassuring to know that one of the most powerful tools at our disposal is also one of the simplest. The next time you’re feeling stressed, are struggling to concentrate, or hoping to give your memory a boost, consider taking a walk. This “brainless” move might just be the smartest decision you make all day.
Exercise brain boost can last for years
A longitudinal study by University of Queensland researchers has found high-intensity interval exercise improves brain function in older adults for up to 5 years.
Emeritus Professor Perry Bartlett and Dr Daniel Blackmore from UQ’s Queensland Brain Institute led the study in which volunteers did physical exercise and had brain scans.
Emeritus Professor Perry Bartlett and Dr Daniel Blackmore have shown high intensity exercise boosts cognition in healthy older adults and the improvement was retained for up to 5 years.
Emeritus Professor Bartlett said it is the first controlled study of its kind to show exercise can boost cognition in healthy older adults not just delay cognitive decline.
“Six months of high-intensity interval training is enough to flick the switch,” Emeritus Professor Bartlett said.
“In earlier pre-clinical work , we discovered exercise can activate stem cells and increase the production of neurons in the hippocampus, improving cognition.
“In this study, a large cohort of healthy 65 — 85-year-old volunteers joined a six-month exercise program, did biomarker and cognition testing and had high-resolution brain scans.
“We followed up with them 5 years after the program and incredibly they still had improved cognition, even if they hadn’t kept up with the exercises.”
Ageing is one of the biggest risks for dementia, a condition that affects almost half a million Australians.
“If we can change the trajectory of ageing and keep people cognitively healthier for longer with a simple intervention like exercise, we can potentially save our community from the enormous personal, economic and social costs associated with dementia,” Emeritus Professor Bartlett said.
Emeritus Professor Bartlett and Dr Blackmore worked in collaboration with Honorary Professor Stephan Riek and The School of Human Movement and Nutrition Sciences at UQ.
During the study, the researchers assessed the impact of three exercise intensities: • Low — predominantly motor function, balance and stretching • Medium — brisk walking on a treadmill • High — four cycles running on a treadmill at near maximum exertion
Dr Blackmore said only the high-intensity interval exercise led to cognitive improvement that was retained for up to 5 years.
“On high-resolution MRI scans of that group, we saw structural and connectivity changes in the hippocampus, the area responsible for learning and memory,” Dr Blackmore said.
“We also found blood biomarkers that changed in correlation to improvements in cognition.
“Biomarkers can be useful in predicting the effectiveness of the exercise a person is doing.”
With 1 in 3 people aged 85 years likely to develop dementia, Dr Blackmore said the impact of the research was far-reaching.
“Our finding can inform exercise guidelines for older people and further research could assess different types of exercise that could be incorporated into aged care,” he said.
“We are now looking at the genetic factors that may regulate a person’s response to exercise to see if we can establish who will and who will not respond to this intervention.
“The use of biomarkers as a diagnostic tool for exercise also needs further research.”
The research was published in Aging and Disease .
It receives ongoing support from the Stafford Fox Medical Research Foundation.
The molecule that could alleviate stroke-related brain injury
A newly developed molecule, LK-2, could inform new therapies for stroke-related brain injury, finds scientists at The Hospital for Sick Children (SickKids).
An ischemic stroke occurs when blood flow to a part of the brain is interrupted, depriving the brain cells of oxygen and nutrients. Without timely treatment, brain cells can die, resulting in permanent damage to the brain and its functions. Stroke is one of the leading causes of death and disability worldwide, affecting millions every year.
An international study published in Nature co-led by Dr. Lu-Yang Wang, a Senior Scientist in the Neurosciences & Mental Health program at SickKids, and clinician scientists at the Shanghai Jiao Tong University School of Medicine, has uncovered a molecule that holds the potential to protect neurons during stroke and prevent stroke-related brain damage.
“Our findings provide an entirely new way to think about saving cells while minimizing the adverse neural side effects of conventional stroke therapy,” says Wang, who holds a Tier 1 Canada Research Chair in Brain Development and Disorders. “The LK-2 molecule could be the key to unlocking successful therapeutics for stroke patients.”
How one neurotransmitter is contributing to stroke-related brain damage
One of the main culprits behind stroke-induced brain damage is a neurotransmitter called glutamate. When the brain is starved of oxygen and sugar, glutamate levels rise dramatically, overstimulating N-methyl-Daspartate receptors (NMDARs) on the membrane of brain cells. This causes a surge of calcium to enter cells, triggering a cascade of events that ultimately leads to cell death.
For decades, researchers have tried to develop drugs that can block NMDARs and prevent the neurotoxicity that comes with elevated levels of glutamate. However, previous drugs targeting NMDARs have been ineffective and failed to move beyond clinical trials because NMDARs play important roles in regular brain functions, such as learning and memory. In addition, blocking NMDARs completely can cause serious side effects, such as psychosis and cognitive impairment.
The team found that glutamate can also bind to and activate a type of acidosis sensor called acid-sensing ion channels (ASICs), which are normally activated by acids. ASICs are present in the membrane of brain cells — like NMDARs — and can allow calcium ions to enter the cells when stimulated.
“We have shown that glutamate can supercharge the activity of ASICs, especially under the acidic conditions that occur during stroke,” explains Wang. “This means that glutamate is attacking brain cells through both NMDARs and ASICs — something we did not know before now.”
A new way to block excess glutamate
By identifying the specific site in ASICs where glutamate binds, the team was able to develop a new molecule, called LK-2, that can selectively block the glutamate binding site in ASICs, but leave NMDARs intact.
In preclinical models, the team found that LK-2 effectively prevented glutamate from overstimulating ASICs to reduce the flow calcium and cell death. Furthermore, LK-2 did not affect NMDARs or other regular neural transmissions, which suggests its potential as the next generation of stroke therapeutics.
“Our research has revealed a new way to protect the brain from glutamate toxicity without interfering with NMDARs,” Wang says.
Wang’s research will continue to explore the function and mechanisms of LK-2, in the hopes of developing future clinical trials.
The research team wants to thank Dr. Julie Forman-Kay, a Senior Scientist and Program Head of the Molecular Medicine program, and Dr. Iva Pritišanac, a postdoctoral fellow in Forman-Kay’s lab, who assisted Wang in locating the binding sites for glutamate on ASICs.
This research is funded at SickKids by the Canadian Institutes of Health Research (CIHR), the Natural Sciences and Engineering Research Council of Canada (NSERC) and Canada Research Chair Program. For a full list of funders, access the paper in Nature .
Alzheimer’s Breakthrough As Nasal Spray May Boost Memory

Nasal sprays could revolutionize Alzheimer’s treatment by swiftly delivering brain-boosting medicine and improving cognitive function, a new study shows.
This research is the latest in recent years to show showing promising results that support nasal therapy as a potential treatment for degenerative brain conditions .
Researchers at the Mitchell Center for Neurodegenerative Diseases, University of Texas, tested a spray containing tiny lipophilic micelles (oil/fat particles that can carry substances through water) on aging mice, administering the treatment through their noses.
These findings could guide the development of more effective treatments for Alzheimer’s and related diseases.
More From Newsweek Vault: What Is a Health Savings Account?
The bulk of recent studies indicating the same outcomes could bring hope to the 6.9 million Americans who are living with Alzheimer’s at present.
Newsletter
The Bulletin
Your Morning Starts Here
Begin your day with a curated outlook of top news around the world and why it matters.
I want to receive special offers and promotions from Newsweek
By clicking on SIGN ME UP, you agree to Newsweek’s Terms of Use & Privacy Policy . You may unsubscribe at any time.
With the global number of sufferers projected to exceed 78 million by 2030, breakthroughs like this are crucial. A model of a human brain being held in a hand. To get an antibody into the brain rapidly, a team put it into tiny packages called micelles and delivered it through mice’s nose. Nasal sprays are a promising new treatment for Alzheimer’s because they deliver medicine directly to the brain quickly and effectively.
The intranasal solution was found to improve their cognitive function . This was achieved through the development of a confirmation-specific antibody (TTCM2)—a type which recognizes and binds to a protein only when that protein is in a specific shape or form.
More From Newsweek Vault: Compare the Top Health Savings Account (HSA) Providers
These aggregates build up inside cells, and current treatments haven’t been very effective at removing them or improving cognition.
In this case, the antibodies sought out tau, a protein that sits in the neurons of the brain. In Alzheimer’s disease, excessive amounts of toxic tau buildup get tangled with normal tau proteins, slowing down a person’s capacity to think, feel, and remember.
Other diseases operate in similar ways—lewy body dementia, and rare conditions such as progressive supranuclear palsy share the same tau-related characteristics that result in the degradation of the brain.
TTCM2 was able to stop the tau from spreading, which is crucial for slowing the disease.
Just one dose of TTCM2 cleared the harmful tau, increased important brain proteins, and improved memory in old mice with tau problems.
It is yet to be determined whether this would benefit humans with the same efficacy, but similar studies in China and Spain that have looked into the concept point to there being adequate evidence that research is moving in that direction.
This research was produced as a result of a grant from The Alzheimer’s Association , whom Newsweek has contacted for comment via email.
You can read the Mitchell Center for Neurodegenerative Diseases findings in full here .
Is there a health problem that’s worrying you? Let us know via health@newsweek.com. We can ask experts for advice, and your story could be featured on Newsweek .
Brain neurotransmitter receptor antagonist found to prevent opioid addiction in mice
New research led by UCLA Health has found a drug that treats insomnia works to prevent the addictive effects of the morphine opioids in mice while still providing effective pain relief.
The study, published in the journal Nature Mental Health , concluded that suvorexant, which blocks brain receptors for a neurotransmitter called hypocretin, prevents opioid addiction. At high doses in humans, suvorexant induces sleep and is used to treat insomnia. But sleep was not induced, and behavioral alertness was maintained, at the much lower doses effective in preventing opioid addiction in mice.
Hypocretin, also called orexin, is a peptide that is linked to mood, with hypocretin release in humans being maximal during pleasurable activities and minimal during pain or sadness. The loss of hypocretin neurons is the cause of narcolepsy, which is thought to be an autoimmune disease. People with narcolepsy and mice made narcoleptic have a greatly diminished susceptibility to opiate addiction.
Researchers have found both humans addicted to heroin and mice addicted to morphine develop higher numbers of hypocretin producing neurons. Morphine causes hypocretin neurons to increase their anatomical connections to pleasure related brain regions.
The latest study in mice found that administering opioids with suvorexant prevents opioid-induced changes in hypocretin neurons, prevents hypocretin neurons from increasing their connections to the brain’s reward related regions, greatly reduces opioid induced brain inflammation and prevents addictive behavior, such as running in mice expecting to receive their daily morphine dose. Suvorexant given with morphine also greatly reduces morphine withdrawal symptoms, according to the study.
“The annual US rate of opioid overdose deaths now exceeds 80,000, greater than the annual rates of automobile or gun deaths,” said the study’s senior author, Dr. Jerome Siegel of UCLA Health’s Jane & Terry Semel Institute for Neuroscience and Human Behavior, the UCLA Brain Research Institute and U.S. Department of Veterans Affairs. “Non-opioid analgesics are able to relieve relatively minor pain. But severe burns, cancer, joint inflammation, sickle cell disease, bone damage and many other painful conditions often cannot be effectively treated with non-opioid analgesics.
“Further studies are needed to determine if the addiction suppressive results seen in mice given suvorexant with morphine are also seen in humans, potentially allowing safer, more effective treatment of pain without the risk of addiction and opioid overdose death,” Siegel continued
The study included 170 mice that were administered morphine for 14-day periods, 5 postmortem brains of humans with opiate use disorder and 5 control human brains. Trials are necessary to determine whether suvorexant will be as effective in suppressing addiction in humans using opioids for pain relief as it is in mice, Siegel said.
“The annual US rate of opioid overdose deaths now exceeds 80,000, greater than the annual rates of automobile or gun deaths,” Siegel said. “Non-opioid analgesics are able to relieve relatively minor pain. But severe burns, cancer, joint inflammation, sickle cell disease, bone damage and many other painful conditions often cannot be effectively treated with non-opioid analgesics.
“Further studies are needed to determine if the addiction suppressive results seen in mice given suvorexant with morphine are also seen in humans, potentially allowing safer, more effective treatment of pain without the risk of addiction and opioid overdose death,” Siegel continued.
Maximize memory function with a nutrient-rich diet

Credit: Unsplash/CC0 Public Domain Research suggests that the ability to maximize memory function may be related to what you eat. Following an eating plan that provides a healthier selection of dietary fats and a variety of plant foods rich in phytonutrients could positively affect your health. Phytonutrients are substances found in certain plants that are believed to be beneficial for human health and help prevent certain diseases.
There’s still much to learn about what makes up a brain-healthy diet. Studies are finding that what’s good for your heart also may be good for your brain. So the best bet for rich memories is to forgo unhealthy fat and remember to diversify your plant-based food portfolio. Foods that boost memory
Diets rich in fruits, vegetables, whole grains and legumes, fish, healthier fats, and herbs or seeds boost the brain’s memory functioning. Here’s more about these powerhouse foods: Fruits
Berries are high in antioxidants that can protect the brain from oxidative damage, and prevent premature aging and memory-impairing dementia. Blueberries are a rich source of anthocyanin and other flavonoids that may improve brain function.
Grapes are full of resveratrol, a memory-boosting compound. Concord grapes are rich in polyphenols, which have the potential to promote brain function.
Watermelon has a high concentration of lycopene, another powerful antioxidant. Watermelon also is a good source of pure water, which benefits brain health. Even a mild case of dehydration can reduce mental energy and impair memory.
Avocados are a fruit rich in monounsaturated fat, which improves memory function by helping improve blood cholesterol levels when eaten in moderation in place of saturated fats.
Vegetables
Beets are rich in nitrates, a natural compound that can dilate blood vessels, allowing more oxygenated blood to reach the brain.
Dark, leafy greens are known for their antioxidants, such as vitamin C, and have been shown to reduce age-related memory loss. Greens also are rich in folate, which can improve memory by decreasing inflammation and improving blood circulation to the brain.
Whole grains and legumes
Cracked wheat, whole-grain couscous, chickpeas, oats, sweet potatoes and black beans are examples of complex carbohydrates. Since brain cells run on glucose derived from carbohydrates and don’t store excess glucose, they need a steady supply of it. Complex carbohydrates are a preferred brain food, providing a slow, sustained supply of glucose. They take longer to metabolize and are high in folate, the memory-boosting B vitamin.
Seafood
Fatty fishes, such as salmon, trout, mackerel, herring, sardines, pilchards and kippers, are rich in heart-healthy omega-3 fatty acids . These have been shown to improve memory when eaten one to two times per week. Omega-3 fatty acids don’t affect low-density lipoprotein (LDL) cholesterol and can lower triglycerides.
Shellfish and crustaceans, such as oysters, mussels, clams, crayfish, shrimp and lobster, are good sources of vitamin B12, a nutrient involved in preventing memory loss.
Healthier fats
Olive oil provides monounsaturated fat, which can help reduce LDL cholesterol levels when used in place of saturated or trans fat. Extra-virgin olive oil is the least processed type with the highest protective antioxidant compound levels.
Nuts, such as walnuts, are a source of omega-3 fatty acids, which lower triglycerides, improve vascular health, help moderate blood pressure and decrease blood clotting.
Herbs or seeds
Cocoa seeds are a rich source of flavonoid antioxidants, which are especially important in preventing damage from LDL cholesterol, protecting arterial lining and preventing blood clots. Cocoa also contains arginine, a compound that increases blood vessel dilation.
Rosemary and mint are in the same herb family. Rosemary has been shown to increase blood flow to the brain, improving concentration and memory. Peppermint aroma has been found to enhance memory.
Sesame seeds are a rich source of the amino acid tyrosine, which is used to produce dopamine, a neurotransmitter responsible for keeping the brain alert and memory sharp. Sesame seeds also are rich in zinc, magnesium and vitamin B6, other nutrients involved in memory function .
Saffron has been shown to positively affect individuals with mild to moderate Alzheimer’s disease.
Making lifestyle modifications to control your cholesterol, blood sugar and blood pressure levels, as well as not smoking, taking daily walks and keeping your weight in a healthy range can help preserve memory function .
Provided by Mayo Clinic
Discovery of cellular mechanism to maintain brain’s energy could benefit late-life brain health
A key mechanism which detects when the brain needs an additional energy boost to support its activity has been identified in a study in mice and cells led by UCL scientists.
The scientists say their findings, published in Nature , could inform new therapies to maintain brain health and longevity, as other studies have found that brain energy metabolism can become impaired late in life and contribute to cognitive decline and the development of neurodegenerative disease.
Lead author Professor Alexander Gourine (UCL Neuroscience, Physiology & Pharmacology) said: “Our brains are made up of billions of nerve cells, which work together coordinating numerous functions and performing complex tasks like control of movement, learning and forming memories. All of this computation is very energy-demanding and requires an uninterrupted supply of nutrients and oxygen.
“When our brain is more active, such as when we’re performing a mentally taxing task, our brain needs an immediate boost of energy, but the exact mechanisms that ensure on-demand local supply of metabolic energy to active brain regions are not fully understood.”
Prior research has shown that numerous brain cells called astrocytes appear to play a role in providing the brain neurons with energy they need. Astrocytes, shaped like stars, are a type of glial cell, which are non-neuronal cells found in the central nervous system. When neighbouring neurons need an increase in energy supply, astrocytes jump into action by rapidly activating their own glucose stores and metabolism, leading to the increased production and release of lactate. Lactate supplements the pool of energy that is readily available for use by neurons in the brain.
Professor Gourine explained: “In our study, we have figured out how exactly astrocytes are able to monitor the energy use by their neighbouring nerve cells, and kick-start this process that delivers additional chemical energy to busy brain regions.”
In a series of experiments using mouse models and cell samples, the researchers identified a set of specific receptors in astrocytes that can detect and monitor neuronal activity, and trigger a signalling pathway involving an essential molecule called adenosine. The researchers found that the metabolic signalling pathway activated by adenosine in astrocytes is exactly the same as the pathway that recruits energy stores in the muscle and the liver, for example when we exercise.
Adenosine activates astrocyte glucose metabolism and supply of energy to neurons to ensure that synaptic function (neurotransmitters passing communication signals between cells) continues apace under conditions of high energy demand or reduced energy supply.
The researchers found that when they deactivated the key astrocyte receptors in mice, the animal’s brain activity was less effective, including significant impairments in global brain metabolism, memory and disruption of sleep, thus demonstrating that the signalling pathway they identified is vital for processes such as learning, memory and sleep.
First and co-corresponding author Dr Shefeeq Theparambil, who began the study at UCL before moving to Lancaster University, said: “Identification of this mechanism may have broader implications as it could be a way of treating brain diseases where brain energetics are downregulated, such as neurodegeneration and dementia.”
Professor Gourine added: “We know that brain energy homeostasis is progressively impaired in ageing and this process is accelerated during the development of neurodegenerative diseases such as Alzheimer’s disease. Our study identifies an attractive readily druggable target and therapeutic opportunity for brain energy rescue for the purpose of protecting brain function, maintaining cognitive health, and promoting brain longevity.”
The researchers were supported by Wellcome, and the study involved scientists at UCL, Lancaster University, Imperial College London, King’s College London, Queen Mary University of London, University of Bristol, University of Warwick, and University of Colorado. RELATED TOPICS Health & Medicine Brain Tumor
Nervous System
Psychology Research
Fitness
Mind & Brain Brain Injury
Intelligence
Neuroscience
Brain-Computer Interfaces
RELATED TERMS Neurobiology
Brain tumor
Decade Volcanoes
Seizure
House mouse
Brain damage
Scientists Uncover Brain-Boosting Potential of Vitamin B6

Vitamin B6 is crucial for brain function, with deficiencies linked to memory issues and depression; however, increasing B6 through supplements alone is insufficient. Researchers at Würzburg University Medicine found that inhibiting the degradation enzyme pyridoxal phosphatase effectively raises cellular B6 levels, offering a potential new treatment avenue for mental and neurodegenerative disorders. Researchers found that inhibiting the degradation of vitamin B6 in cells using 7,8-Dihydroxyflavone enhances brain functions and could offer a new treatment method for mental and neurodegenerative disorders.
Vitamin B6 plays a crucial role in brain metabolism. Consequently, low levels of vitamin B6 are linked to memory and learning impairments, depressive moods, and clinical depression in various mental disorders. In the elderly, insufficient vitamin B6 is associated with memory decline and dementia.
Although some of these observations were made decades ago, the exact role of vitamin B6 in mental illness is still largely unclear. What is clear, however, is that an increased intake of vitamin B6 alone, for example in the form of dietary supplements, is insufficient to prevent or treat disorders of brain function. Publication in eLife
A research team from Würzburg University Medicine has now discovered another way to increase vitamin B6 levels in cells more effectively: namely by specifically inhibiting its intracellular degradation. Antje Gohla, Professor of Biochemical Pharmacology at the Department of Pharmacology and Toxicology at Julius-Maximilians-Universität Würzburg (JMU) , is responsible for this.
Other participants come from the Rudolf Virchow Center for Integrative and Translational Bioimaging at JMU, the Leibniz-Forschungsinstitut für Molekulare Pharmakologie-FMP Berlin, and the Institute for Clinical Neurobiology at Würzburg University Hospital. The team has now published the results of their investigations in the scientific journal eLife . Enzyme Blockade Improves Learning Ability
“We were already able to show in earlier studies that genetically switching off the vitamin B6-degrading enzyme pyridoxal phosphatase in mice improves the animals’ spatial learning and memory capacity,” explains Antje Gohla. In order to investigate whether such effects can also be achieved by pharmacological agents, the scientists have now looked for substances that bind and inhibit pyridoxal phosphatase.
With success: “In our experiments, we identified a natural substance that can inhibit pyridoxal phosphatase and thus slow down the degradation of vitamin B6,” explains the pharmacologist. The working group was actually able to increase vitamin B6 levels in nerve cells that are involved in learning and memory processes. The name of this natural substance: 7,8-Dihydroxyflavone. New Approach for Drug Therapy
7,8-Dihydroxyflavone has already been described in numerous other scientific papers as a molecule that can improve learning and memory processes in disease models for mental disorders. The new knowledge of its effect as an inhibitor of pyridoxal phosphatase now opens up new explanations for the effectiveness of this substance. This could improve the mechanistic understanding of mental disorders and represent a new drug approach for the treatment of brain disorders, the scientists write in their study.
The team also considers it a great success that 7,8-Dihydroxyflavone has been identified as an inhibitor of pyridoxal phosphatase for the first time — after all, this class of enzymes is considered to be particularly challenging for drug development. A Long Way to a Drug
When will people benefit from this discovery? “It’s too early to say,” explains Marian Brenner, a first author of the study. However, there is much to suggest that it could be beneficial to use vitamin B6 in combination with inhibitors of pyridoxal phosphatase for various mental disorders and neurodegenerative diseases.
In a next step, Gohla and her team now want to develop improved substances that inhibit this enzyme precisely and highly effectively. Such inhibitors could then be used to specifically test whether increasing cellular vitamin B6 levels is helpful in mental or neurodegenerative diseases.
Reference: “7,8-Dihydroxyflavone is a direct inhibitor of human and murine pyridoxal phosphatase” by Marian Brenner, Christoph Zink, Linda Witzinger, Angelika Keller, Kerstin Hadamek, Sebastian Bothe, Martin Neuenschwander, Carmen Villmann, Jens Peter von Kries, Hermann Schindelin, Elisabeth Jeanclos and Antje Gohla, 10 June 2024, eLife .
DOI: doi:10.7554/eLife.93094
Your Brain Holds Secrets. Scientists Want to Find Them.
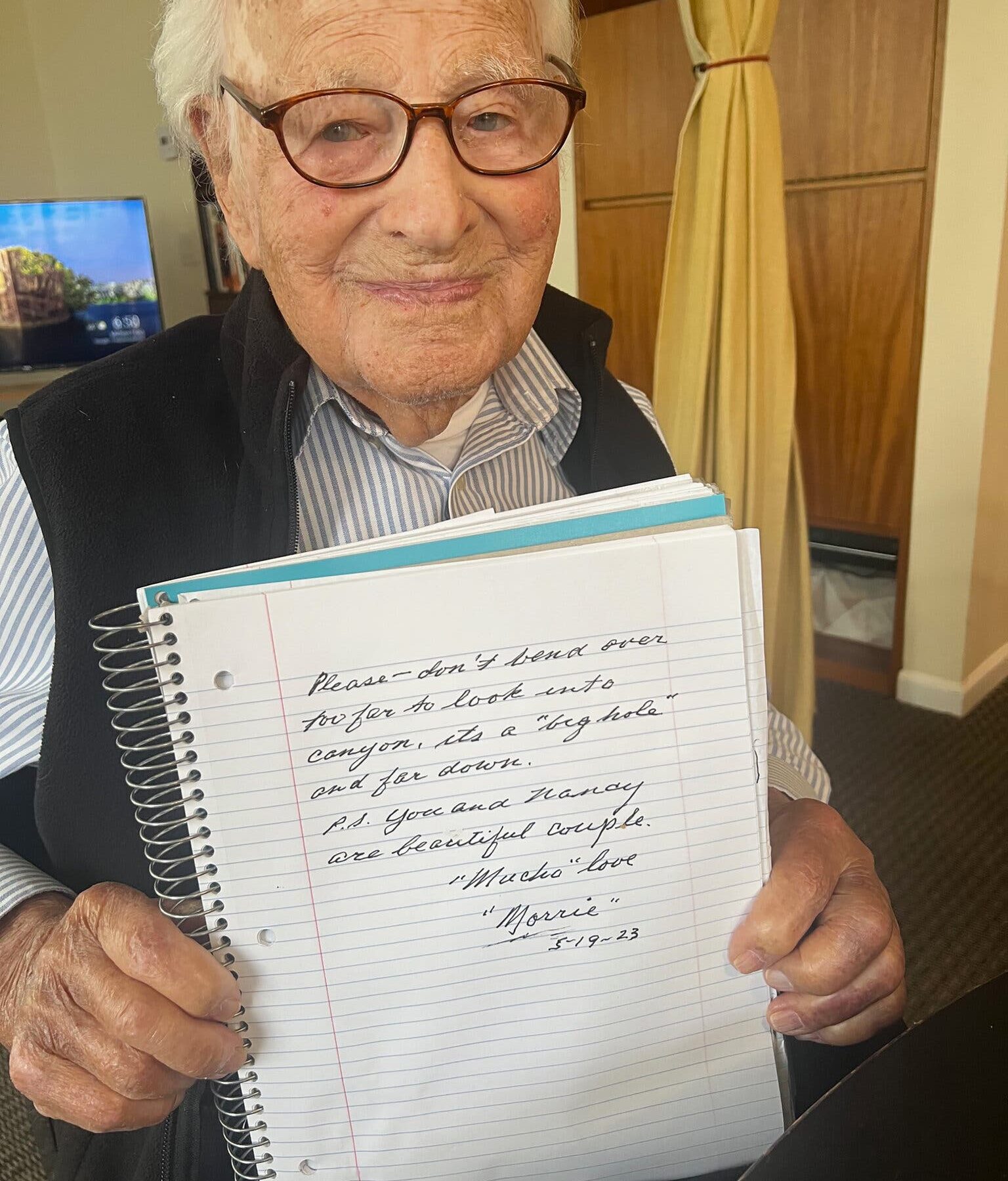
Morrie Markoff died at 110. His family donated his brain to NeuroBioBank. About a month ago, Judith Hansen popped awake in the predawn hours, thinking about her father’s brain.
Her father, Morrie Markoff, was an unusual man. At 110, he was thought to be the oldest in the United States. His brain was unusual, too, even after he recovered from a stroke at 99.
Although he left school after the eighth grade to work, Mr. Markoff became a successful businessman. Later in life, his curiosity and creativity led him to the arts, including photography and sculpture fashioned from scrap metal.
He was a healthy centenarian when he exhibited his work at a gallery in Los Angeles, where he lived. At 103, he published a memoir called “Keep Breathing.” He blogged regularly, pored over The Los Angeles Times daily, discussed articles in Scientific American and followed the national news on CNN and “60 Minutes.”
Now he was nearing death, enrolled in home hospice care. “In the middle of the night, I thought, ‘Dad’s brain is so great,’” said Ms. Hansen, 82, a retired librarian in Seattle. “I went online and looked up ‘brain donation.’”
Her search led to a National Institutes of Health web page explaining that its NeuroBioBank, established in 2013, collected post-mortem human brain tissue to advance neurological research.
Through the site, Ms. Hansen contacted the nonprofit Brain Donor Project . It promotes and simplifies donations through a network of university brain banks, which distribute preserved tissue to research teams.
Tish Hevel, the founder of the project, responded quickly, putting Ms. Hansen and her brother in touch with the brain bank at the University of California, Los Angeles. Brain donors may have neurological and other diseases, or they may possess healthy brains, like Mr. Markoff’s.
“We’re going to learn so much from him,” Ms. Hevel said. “What is it about these superagers that allows them to function at such a high level for so long?” Editors’ Picks
Many older Americans have checked the box on their drivers’ licenses to allow organ donation for transplants; some have also looked into or arranged whole-body donations to medical schools. Fewer know about brain donation, Ms. Hevel said.
The campaign to encourage it began about a decade ago, when “new techniques came on the scene that allow amazing quantitative analysis” of brain cells, said Dr. Walter Koroshetz, the director of the National Institute of Neurological Disorders and Stroke, which administers the NeuroBioBank. Researchers use its material to study an array of brain diseases and psychiatric disorders.
But “these new techniques require the brains to be taken quickly and then frozen,” because “brain tissue starts to deteriorate in a matter of hours,” Dr. Koroshetz said.
Before the NeuroBioBank was established, some universities were already collecting donated brains, but the process “was scattered around the country,” he said. “Access to tissue was not centralized.”
Ms. Hevel encountered such obstacles when her own father was dying of Lewy body dementia in 2015. “It was a terribly complicated process at the time,” she said. The Brain Donor Project now works to inform the public of the importance of brain donation and the best way to arrange it. A sample of frozen brain tissue at Banner Sun Health’s Brain and Body Donation Program in Phoenix. Before NeuroBioBank was established, some universities were already collecting donated brains, but the process wasn’t centralized. Though some neurological research relies on scans and computer simulations, there’s no substitute for human tissue, Dr. Koroshetz said: “It‘s like the difference between looking at a cartoon and a Rembrandt.”
Now, each of the six university brain banks affiliated with the NeuroBioBank averages 100 donations annually, enabling research on topics from Parkinson’s disease and schizophrenia to the effects of military blasts. The Brain Donor Project, working with N.I.H., has registered 23,000 donors since its inception in 2016. “There’s a need for more,” Dr. Koroshetz said.
Brain donation remains a sensitive topic, he acknowledged: “For some families, it’s very uncomfortable to talk about,” and some religious and ethnic groups find it objectionable. When he led research on Huntington’s disease decades ago and raised the issue with patients, “it would take years of people asking questions before they’d feel comfortable signing a form.”
How does it work? The Brain Donor Project connects would-be donors with N.I.H.- affiliated university brain banks. “Don’t try to pick a brain bank on your own,” Ms. Hevel said. They have different requirements and protocols, and the project will connect a donor with the appropriate one.
The donor signs the necessary paperwork, or a relative or medical team member may sign on the donor’s behalf. The family or medical staff must alert the bank immediately after the donor dies.
At the funeral home or morgue where the body is being kept, a “recovery specialist,” often a pathologist or medical examiner, removes the brain from the back of the skull to avoid disfigurement (thus, the deceased can still have an open-casket funeral) and delivers it to a brain bank for freezing and distribution to research labs.
“I’ve heard from so many families that even in the face of great loss, there’s a sense of solace and comfort, knowing something positive can come from it,” Ms. Hevel said.
There is no cost to families, who can opt to receive a neuropathology report a few months later. It may prove useful in alerting relatives to potential disorders or abnormalities.
There are other ways to regard one’s body as a legacy, of course. Under the Uniform Anatomical Gift Act, almost any adult can become an organ donor when getting or renewing a driver’s license, or by signing up at an online state registry. (Agreeing to donate organs for transplantation doesn’t include brain donation for neuroscience research.)
More than 100,000 Americans are on waiting lists for transplants , the greatest number hoping for a kidney.
It’s “a different world” when people want to donate their bodies to medical schools to help educate health care professionals, said Sheldon Kurtz, who teaches law at the University of Iowa and helped draft the current legislation on organ donation.
In that case, donors must contact […]
This sleep supplement shows promise for boosting memory

Credit: Unsplash+ A recent study from Tokyo Medical and Dental University has revealed some exciting findings about melatonin and its ability to improve memory. This research could lead to new treatments to combat cognitive decline in both mice and potentially humans.
Melatonin is commonly known for regulating sleep, but it may also have benefits for memory and cognitive health.
In this study, researchers focused on melatonin’s metabolites—substances created when melatonin breaks down in the body. They were particularly interested in how these metabolites might help with memory.
Mice, which naturally explore new objects more than familiar ones, were used in the study because their behavior provides a simple way to assess memory.
Objects are only considered familiar if they are remembered, similar to how humans recognize and recall items they have seen before.
To test their ideas about melatonin’s metabolites, the scientists used a novel object recognition task. Typically, cognitive decline in mice is shown by their inability to distinguish between new and familiar objects, treating both as if they were new.
The researchers conducted experiments where mice were exposed to certain objects and then given melatonin and its two specific metabolites one hour later. Their memory was tested the next day. The results were striking.
The treatment appeared to enhance the mice’s memory, with one metabolite called AMK showing the most significant effect. This metabolite, among others, was found to build up in the hippocampus, the brain region crucial for forming long-term memories.
Further experiments showed that when the conversion of melatonin into AMK was blocked, there was a noticeable decline in memory enhancement.
This emphasized AMK’s key role in memory formation. The effect was consistent across all ages of mice tested, suggesting it could have broad applications.
The findings are particularly significant for older mice, who showed marked improvements in memory. This gives researchers hope that similar positive outcomes could be seen in older humans.
This could potentially lead to new therapies for conditions like Mild Cognitive Impairment and possibly even Alzheimer’s disease.
As the study continues, there is optimism that AMK therapy could become a strategy to lessen cognitive impairments linked to aging.
While these findings are preliminary and more research is needed to confirm the effects in humans, they offer a promising glimpse into how understanding and using melatonin and its metabolites could lead to significant advances in the treatment of memory-related conditions.
The findings of this study have been published in the Journal of Pineal Research, led by Dr. Atsuhiko Hattori and his research team.
For those interested in maintaining or enhancing brain health, these discoveries suggest that melatonin, a naturally occurring hormone, could play a crucial role in protecting cognitive functions as we age.
If you care about brain health, please read studies about how the Mediterranean diet could protect your brain health, and blueberry supplements may prevent cognitive decline.
For more information about brain health, please see recent studies about antioxidants that could help reduce dementia risk , and Coconut oil could help improve cognitive function in Alzheimer’s .
Copyright © 2024 Knowridge Science Report . All rights reserved.
Want to boost brain health and prevent dementia? Vitamin D supplementation is the key, says study

Tags: aging secrets , alternative medicine , Alzheimer’s disease , anti-aging , brain function , brain health , cognitive decline , cognitive functions , cognitive health , dementia , goodhealth , goodmedicine , goodscience , health science , learning , memory , natural health , natural medicine , Naturopathy , nutrients , prevention , real investigations , research , supplements , vitamin D Vitamin D is often linked to many health benefits such as strong bones and teeth and a healthy immune system. Reports also suggest that having adequate levels of vitamin D can help reduce your risk of depression . But science says vitamin D can offer more.
According to a recent study by researchers from Canada and the U.K., supplementing with vitamin D can also help reduce your risk of dementia . Dementia is an umbrella term for cognitive issues that commonly plague older adults, often characterized by an impaired ability to think, remember or make decisions. Alzheimer’s disease is the most common form of dementia, and it affects an estimated 6.9 million Americans aged 65 and older today. Vitamin D: a potent nutrient for dementia prevention
Numerous studies have long reported about the connection between vitamin D deficiency and dementia. For instance, a 2014 study published in the journal Neurology analyzed data from 1,658 older adults and found that being deficient in vitamin D substantially increased their risks of all-cause dementia and Alzheimer’s disease . However, despite this association, the potential of vitamin D supplementation to lower these risks remains largely unexplored.
To address this, researchers from the University of Calgary and the University of Exeter conducted a prospective cohort study to investigate the effects of vitamin D on dementia incidence. All data used in the study came from the National Alzheimer’s Coordination Center database, a centralized data repository for the National Institute of Aging’s (NIA) Alzheimer’s Disease Research Centers (ADRC) Program, and were obtained from a total of 12,388 participants. These individuals were all dementia-free at the beginning of data collection (baseline).
We are building the infrastructure of human freedom and empowering people to be informed, healthy and aware. Explore our decentralized, peer-to-peer, uncensorable Brighteon.io free speech platform here . Learn about our free, downloadable generative AI tools at Brighteon.AI . Every purchase at HealthRangerStore.com helps fund our efforts to build and share more tools for empowering humanity with knowledge and abundance.
The researchers divided the participants into two groups: those with baseline exposure to vitamin D and those without prior to the onset of dementia. They also looked at the effect of three different types of vitamin D supplement , namely, calcium–vitamin D, cholecalciferol and ergocalciferol. They hypothesized that taking any of these commonly used vitamin D supplements would be associated with a lower incidence of dementia. (Related: 6 Mushrooms you can eat to prevent cognitive impairment and reduce your dementia risk .)
Aside from age, sex, education, race, cognitive diagnosis and depression, the researchers also adjusted for apolipoprotein E (APOE) e4 status. APOE is a protein that combines with lipids to form lipoproteins , which are responsible for packaging and transporting cholesterol through the bloodstream. The APOE gene has three versions, one of which (e4) has been found to increase a person’s risk of developing early-onset Alzheimer’s disease . The APOE e4 allele can be inherited from one or both parents, with the latter case resulting in an even greater risk of Alzheimer’s.
Data analyses revealed that exposure to any form of vitamin D was associated with significantly longer dementia-free survival as well as a lower incidence rate of Alzheimer’s compared to no exposure. In fact, supplementing with vitamin D reduced dementia risk among the participants by 40 percent. The researchers also noted that the effects of vitamin D were significantly greater among women than men and among those with normal cognition than those with mild cognitive impairment.
Lastly, the researchers noted that the “effect of vitamin D on [dementia] incidence rate differed significantly across the strata of sex, cognitive status, and APOE e4 status.” In particular, the effects of vitamin D supplementation were significantly greater among individuals who did not carry the APOE e4 gene than those who inherited the gene from either one or both parents.
Although the researchers were unsure why the participants visited an ADRC and why they were taking vitamin D supplements, their findings nevertheless “implicate vitamin D as a potential agent for dementia prevention and provide additional support for its use in at-risk individuals for [Alzheimer’s disease] dementia.” Vitamin D is important for brain function
In an earlier study published in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association , researchers at Tufts University in Massachusetts sought to understand the role of vitamin D in the brain and why a person’s vitamin D levels have a huge impact on his cognitive performance. Lead author Kyla Shea, an associate professor at the Friedman School of Nutrition Science and Policy at Tufts , explained that they “wanted to know if vitamin D is even present in the brain, and if it is, how those concentrations are linked to cognitive decline.”
To achieve their objective, the researchers examined brain samples collected from 209 participants in the Rush Memory and Aging Project, a long-term study whose goal was to identify the post-mortem indices linking genetic and environmental risk factors to the development of Alzheimer’s. They looked for vitamin D in four different regions of the human brain .
Two of those brain regions are associated with changes observed in Alzheimer’s disease, while one is associated with forms of dementia that have been linked to blood flow. The last region has no established link to Alzheimer’s or vascular disease-related cognitive decline. (Related: Research shows Lion’s mane mushroom can combat dementia and cognitive decline .)
The researchers found that vitamin D is a natural component of brain tissue. In fact, the presence of high levels of vitamin D in all four regions of the brain that they examined correlated with better brain performance and a 25 to 30 percent lower […]
Amid post-debate cognitive concerns, doctor recommends 3 natural supplements to boost brain power
Join Fox News for access to this content
Plus special access to select articles and other premium content with your account – free of charge.
By entering your email and pushing continue, you are agreeing to Fox News’ Terms of Use and Privacy Policy , which includes our Notice of Financial Incentive .
Please enter a valid email address.
By entering your email and pushing continue, you are agreeing to Fox News’ Terms of Use and Privacy Policy , which includes our Notice of Financial Incentive .
Having trouble? Click here.
As doctors continue to discuss President Joe Biden’s concerning speech patterns and behavior during Thursday night’s presidential debate, Dr. Nicole Saphier is focusing on natural remedies for cognitive function.
“Cognitive decline is a hot topic right now,” Saphier — who is an associate professor at Memorial Sloan Kettering Cancer Center in New York City and director of breast imaging at Memorial Sloan Kettering in Monmouth, New Jersey — said during a Sunday appearance on “Fox & Friends Weekend.”
A proponent of natural remedies and herbs for certain aspects of health , Saphier recommended a trio of supplements to help improve mental focus and prevent dementia.
DOCTORS EXPRESS CONCERN ABOUT BIDEN’S APPARENT COGNITIVE ISSUES DURING DEBATE: ‘TROUBLING INDICATORS’
“When it comes to improving memory and reducing the risk of cognitive decline, my three favorites are Bacopa monnieri, ginkgo biloba and ginseng,” she told Rachel Campos-Duffy of Fox News Channel.
In studies with human participants, all three supplements have been shown to improve memory, improve visual recognition and potentially decrease the risk of cognitive decline, according to Saphier.
Some of the studies have even linked these supplements to a longer life span , she said.
“Now as we know, when it comes to dementia, oftentimes it only gets worse and doesn’t get better,” Saphier said.
DAILY MULTIVITAMINS MIGHT NOT HELP YOU LIVE LONGER, STUDY FINDS: ‘NO DIFFERENCES IN MORTALITY’
“So you want to be eating healthy and leading a healthy life before it happens, to try and decrease your risk.”
Bacopa monnieri, ginkgo biloba and ginseng are all natural plants , Saphier emphasized.
“I like to take them in liquid nutraceutical forms, because that gets absorbed the best,” she recommended.
The doctor also pointed out that all supplements are not created equal.
“A lot of herbal supplements don’t really have positive benefits — they’re more of a marketing scheme,” she said.
“But there are some things that are backed by science, and that’s the only stuff I talk about.”
Here’s a deeper dive into the three she recommends. 1. What is Bacopa monnieri?
Bacopa (Bacopa monnieri) — also referred to as Brahmi — is a plant that’s been used in traditional Ayurvedic medicine for centuries, according to WebMD.
The plant could help to increase chemicals in the brain that assist with learning, memory and other cognitive functions, the website stated.
It also could potentially serve as a protective mechanism against Alzheimer’s disease , per WebMD.
Bacopa is generally safe for adults to consume by mouth in doses of 300-600 mg daily for 12 weeks, and can be added to hot water to make tea.WebMD recommends speaking with a doctor first to determine optimal dosage, potential side effects and interactions with other medications . 2. What is ginkgo biloba? Ginkgo (Ginkgo biloba) is derived from an extract taken from the tree species’ fan-shaped leaves, according to Mayo Clinic’s website.“While some evidence suggests that ginkgo extract might modestly improve memory in healthy adults , most studies indicate that ginkgo doesn’t improve memory, attention or brain function,” Mayo Clinic states. REGULAR SNACKS OF BABY CARROTS BRING SIGNIFICANTLY MORE ANTIOXIDANT PROTECTION, NEW STUDY FINDS Gingko can be consumed in a pill, extract, capsule or tea.“Don’t eat raw or roasted ginkgo seeds, which can be poisonous,” Mayo Clinic warns.While gingko is generally safe for healthy adults to consume in “moderate amounts,” experts say it is best to consult your doctor about potential side effects and drug interactions. 3. What is ginseng? A popular herbal medicine, ginseng is a plant that has long been used in medical treatments in Asia and North America, according to WebMD. CLICK HERE TO GET THE FOX NEWS APP Although more research is needed to confirm its benefits, some studies have linked ginseng to improved mental focus. CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER “There’s some early evidence that ginseng might give a small, short-term boost to concentration and learning,” stated WebMD.“Some studies of mental performance have combined ginseng with extract from leaves of the ginkgo tree, another traditional remedy said to help with dementia . While these studies are intriguing, many experts feel we need more evidence.” For more Health articles, visit www.foxnews/health Ginseng can be consumed in the form of dried herbs, tea, capsules or powder, per WebMD.As with any supplement plans, it’s always best to talk early on with a doctor about dosage, side effects and drug interactions.
New insights into brain energy metabolism may lead to neurodegenerative disease therapies

A key mechanism which detects when the brain needs an additional energy boost to support its activity has been identified in a study in mice and cells led by UCL scientists.
The scientists say their findings, published in Nature , could inform new therapies to maintain brain health and longevity, as other studies have found that brain energy metabolism can become impaired late in life and contribute to cognitive decline and the development of neurodegenerative disease. Our brains are made up of billions of nerve cells, which work together coordinating numerous functions and performing complex tasks like control of movement, learning and forming memories. All of this computation is very energy-demanding and requires an uninterrupted supply of nutrients and oxygen. When our brain is more active, such as when we’re performing a mentally taxing task, our brain needs an immediate boost of energy, but the exact mechanisms that ensure on-demand local supply of metabolic energy to active brain regions are not fully understood.” Alexander Gourine, Lead Author, Professor, UCL Neuroscience, Physiology & Pharmacology Prior research has shown that numerous brain cells called astrocytes appear to play a role in providing the brain neurons with energy they need. Astrocytes, shaped like stars, are a type of glial cell , which are non-neuronal cells found in the central nervous system. When neighbouring neurons need an increase in energy supply, astrocytes jump into action by rapidly activating their own glucose stores and metabolism, leading to the increased production and release of lactate. Lactate supplements the pool of energy that is readily available for use by neurons in the brain.
Professor Gourine explained: “In our study, we have figured out how exactly astrocytes are able to monitor the energy use by their neighboring nerve cells, and kick-start this process that delivers additional chemical energy to busy brain regions.”
In a series of experiments using mouse models and cell samples, the researchers identified a set of specific receptors in astrocytes that can detect and monitor neuronal activity, and trigger a signaling pathway involving an essential molecule called adenosine. The researchers found that the metabolic signaling pathway activated by adenosine in astrocytes is exactly the same as the pathway that recruits energy stores in the muscle and the liver, for example when we exercise.
Adenosine activates astrocyte glucose metabolism and supply of energy to neurons to ensure that synaptic function (neurotransmitters passing communication signals between cells) continues apace under conditions of high energy demand or reduced energy supply.
The researchers found that when they deactivated the key astrocyte receptors in mice, the animal’s brain activity was less effective, including significant impairments in global brain metabolism, memory and disruption of sleep, thus demonstrating that the signaling pathway they identified is vital for processes such as learning, memory and sleep.
First and co-corresponding author Dr Shefeeq Theparambil, who began the study at UCL before moving to Lancaster University, said: “Identification of this mechanism may have broader implications as it could be a way of treating brain diseases where brain energetics are downregulated, such as neurodegeneration and dementia.”
Professor Gourine added: “We know that brain energy homeostasis is progressively impaired in ageing and this process is accelerated during the development of neurodegenerative diseases such as Alzheimer’s disease. Our study identifies an attractive readily druggable target and therapeutic opportunity for brain energy rescue for the purpose of protecting brain function, maintaining cognitive health, and promoting brain longevity.”
The researchers were supported by Wellcome, and the study involved scientists at UCL, Lancaster University, Imperial College London, King’s College London, Queen Mary University of London, University of Bristol, University of Warwick, and University of Colorado.
Source:
University College London
Journal reference:
Theparambil, S. M., et al. (2024). Adenosine signalling to astrocytes coordinates brain metabolism and function. Nature . doi.org/10.1038/s41586-024-07611-w .
Discovery of cellular mechanism to maintain brain’s energy could benefit late-life brain health
by University College London Deletion of A2B receptors in hippocampal astrocytes. Credit: Nature (2024). DOI: 10.1038/s41586-024-07611-w A key mechanism which detects when the brain needs an additional energy boost to support its activity has been identified in a study in mice and cells led by UCL scientists.
The scientists say their findings, published in Nature , could inform new therapies to maintain brain health and longevity, as other studies have found that brain energy metabolism can become impaired late in life and contribute to cognitive decline and the development of neurodegenerative disease.
Lead author Professor Alexander Gourine (UCL Neuroscience, Physiology & Pharmacology) said, “Our brains are made up of billions of nerve cells , which work together coordinating numerous functions and performing complex tasks like control of movement, learning and forming memories. All of this computation is very energy-demanding and requires an uninterrupted supply of nutrients and oxygen.
“When our brain is more active, such as when we’re performing a mentally taxing task, our brain needs an immediate boost of energy, but the exact mechanisms that ensure on-demand local supply of metabolic energy to active brain regions are not fully understood.”
Prior research has shown that numerous brain cells called astrocytes appear to play a role in providing the brain neurons with energy they need. Astrocytes, shaped like stars, are a type of glial cell, which are non-neuronal cells found in the central nervous system.
When neighboring neurons need an increase in energy supply , astrocytes jump into action by rapidly activating their own glucose stores and metabolism, leading to the increased production and release of lactate. Lactate supplements the pool of energy that is readily available for use by neurons in the brain. Neuronal activity recruits cAMP–PKA signaling in astrocytes. Credit: Nature (2024). DOI: 10.1038/s41586-024-07611-w Professor Gourine explained, “In our study, we have figured out how exactly astrocytes are able to monitor the energy use by their neighboring nerve cells, and kick-start this process that delivers additional chemical energy to busy brain regions.”
In a series of experiments using mouse models and cell samples, the researchers identified a set of specific receptors in astrocytes that can detect and monitor neuronal activity, and trigger a signaling pathway involving an essential molecule called adenosine. The researchers found that the metabolic signaling pathway activated by adenosine in astrocytes is exactly the same as the pathway that recruits energy stores in the muscle and the liver, for example, when we exercise.
Adenosine activates astrocyte glucose metabolism and supply of energy to neurons to ensure that synaptic function (neurotransmitters passing communication signals between cells) continues apace under conditions of high energy demand or reduced energy supply.
The researchers found that when they deactivated the key astrocyte receptors in mice, the animal’s brain activity was less effective, including significant impairments in global brain metabolism, memory and disruption of sleep, thus demonstrating that the signaling pathway they identified is vital for processes such as learning, memory and sleep.
First and co-corresponding author Dr. Shefeeq Theparambil, who began the study at UCL before moving to Lancaster University, said, “Identification of this mechanism may have broader implications as it could be a way of treating brain diseases where brain energetics are downregulated, such as neurodegeneration and dementia.”
Professor Gourine added, “We know that brain energy homeostasis is progressively impaired in aging and this process is accelerated during the development of neurodegenerative diseases such as Alzheimer’s disease. Our study identifies an attractive readily druggable target and therapeutic opportunity for brain energy rescue for the purpose of protecting brain function, maintaining cognitive health, and promoting brain longevity.”
The study involved scientists at UCL, Lancaster University, Imperial College London, King’s College London, Queen Mary University of London, University of Bristol, University of Warwick, and University of Colorado.
More information: Alexander Gourine, Adenosine signaling to astrocytes coordinaates brain metabolism and function, Nature (2024). DOI: 10.1038/s41586-024-07611-w . www.nature.com/articles/s41586-024-07611-w
Provided by University College London
Study finds brain stores motor memories differently based on decision uncertainty

A: Screen of the experiment, B: perturbation pattern. Credit: National Institute of Information and Communications Technology (NICT) A study published in the journal Nature Human Behaviour challenges the belief that identical physical actions are governed by the same motor memory, regardless of the decision-making process involved. Researchers from the National Institute of Information and Communications Technology (NICT) and HONDA R&D Co., Ltd. have discovered that the brain differentiates and stores motor memories based on the level of uncertainty experienced during decision-making.
In a football (soccer) penalty shootout, a player may decide to confidently kick the ball to the right corner upon observing the goalkeeper moving in the opposite direction. Alternatively, the player might make the same kick while being unsure about the goalkeeper’s movement.
Although the physical action—kicking the ball to the right—is identical in both scenarios, this new study reveals that the brain tags these actions differently based on the decision uncertainty involved. This discovery suggests that motor memories are not simply repetitions of the same action but are influenced by the cognitive processes leading up to them.
“This was a very surprising finding. This tells us that we cannot treat actions as something totally independent from the cognitive process. Both are combined to make the representation of action,” says Hagura Nobuhiro, a senior author of the paper.
This research opens up new avenues for developing novel training methods in sports. By associating skill training with various decision-making situations, athletes can enhance their performance by refining their motor memories in context-specific scenarios. Setup of the experiment. Credit: National Institute of Information and Communications Technology In the study, human volunteers decided whether a cloud of dots presented on a screen was moving to the left or to the right. They held a robotic handle in their right hand and moved the handle towards the target in the direction of their decision. The uncertainty of the decision was modulated by changing the coherence level of the dots’ motion.
When all the dots were moving to the left or to the right (100% coherent motion), the certainty of the decision was high. When only a small proportion of the dots were coherently moving and the other dots were moving in random directions, the situation was uncertain. Participants’ hand movement to express the decision was pushed by the robotic handle to deviate from the straight path, and under this perturbation, participants were instructed to make a straight movement by resisting the force.
In one of the experiments, participants were divided into two groups: the Certain Decision group and the Uncertain Decision group. The Certain Decision group learned to make a straight movement only after deciding on a high dot coherence level motion (100%). The Uncertain Decision group learned the same action, but only after deciding on a low coherence level motion (3%). A: The amount of force produced to resist the perturbation for both Certain and Uncertain conditions B: The amount of force produced for different uncertainty levels in both certain and uncertain conditions. Credit: National Institute of Information and Communications Technology Although both groups of participants successfully learned to make a straight movement in their respective decision contexts (certain or uncertain), their performance level dropped when they were asked to perform the same movement after decisions with different uncertainty levels (different motion coherence levels).
Participants in the Certain group could resist perturbation at the same level as during their practice after a certain decision, but not after an uncertain decision. Similarly, participants in the Uncertain group could perform well after an uncertain decision, but not after a certain decision. This indicates that decision and action are not independent; action is learned in association with the decision that led to the action.
In the other experiment, different types of perturbation (clockwise [CW] direction and counterclockwise [CCW] direction) were each associated with a different decision uncertainty level. If the decision uncertainty level did not differentiate the actions that followed the decision, participants would not be able to learn the two perturbations at the same time, since they would interfere with each other. However, if the decision uncertainty level “tagged” the action, participants would be able to learn the two perturbations simultaneously. A: The amount of force produced to resist the perturbation from the opposite direction, each associated with either certain or uncertain condition. B: The pattern of perturbation for each Certain and Uncertain condition. Credit: National Institute of Information and Communications Technology Participants were indeed able to learn the two perturbations at the same time, demonstrating that the actions following certain and uncertain decisions are treated as different things in the brain.
The researchers believe that this finding may open up new avenues for developing novel training methods in sports. By associating skill training with various decision-making situations, athletes can enhance their performance by refining their motor memories in context-specific scenarios.
More information: Kisho Ogasa et al, Decision uncertainty as a context for motor memory, Nature Human Behaviour (2024). DOI: 10.1038/s41562-024-01911-x
Provided by National Institute of Information and Communications Technology (NICT)