Nature Knows and Psionic Success
God provides
Exercise Can Slow Brain Aging Cognitive Decline

Summary: A new study shows that exercise can reverse aging effects in the brain. Researchers found that physical activity alters gene expression in microglia, making them resemble those of younger brains.
Exercise also helps reduce harmful T cell presence in the hippocampus, enhancing memory and learning. These findings highlight the importance of exercise for maintaining cognitive health during aging.
Key Facts:
> Gene Expression : Exercise reverts aged microglia gene expression to youthful patterns.
Microglia Role : Essential for exercise-induced formation of new neurons in the hippocampus.
T Cells Reduction : Exercise prevents/reduces T cell presence in the aging hippocampus.
Source: Wiley
New research published in Aging Cell provides insights into how exercise may help to prevent or slow cognitive decline during aging.
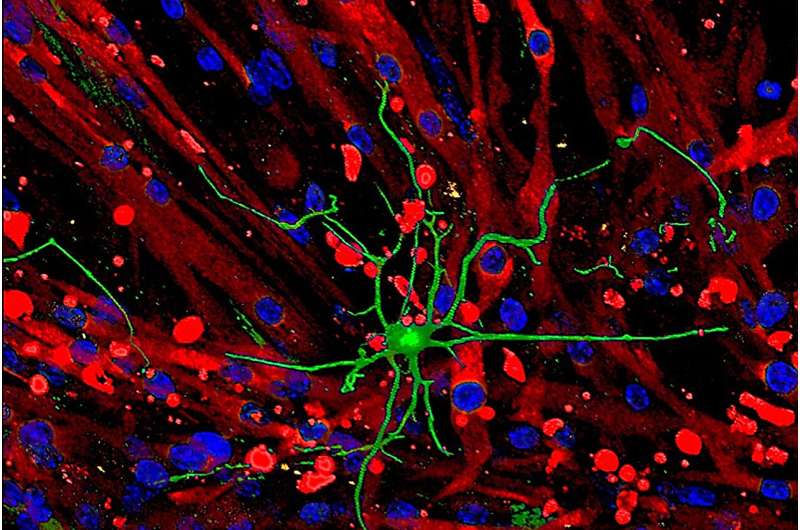
For the study, investigators assessed the expression of genes in individual cells in the brains of mice. The team found that exercise has a significant impact on gene expression in microglia, the immune cells of the central nervous system that support brain function. These immune cells are not typically found in the brain during youth, but they increase with age. Credit: Neuroscience News Specifically, the group found that exercise reverts the gene expression patterns of aged microglia to patterns seen in young microglia.
Treatments that depleted microglia revealed that these cells are required for the stimulatory effects of exercise on the formation of new neurons in the brain’s hippocampus, a region involved in memory, learning, and emotion.
The scientists also found that allowing mice access to a running wheel prevented and/or reduced the presence of T cells in the hippocampus during aging. These immune cells are not typically found in the brain during youth, but they increase with age.
“We were both surprised and excited about the extent to which physical activity rejuvenates and transforms the composition of immune cells within the brain, in particular the way in which it was able to reverse the negative impacts of aging,” said co–corresponding author Jana Vukovic, PhD, of The University of Queensland, in Australia.
“It highlights the importance of normalizing and facilitating access to tailored exercise programs. Our findings should help different industries to design interventions for elderly individuals who are looking to maintain or improve both their physical and mental capabilities.” About this aging, exercise, and cognition research news
Author: Sara Henning-Stout
Source: Wiley
Contact: Sara Henning-Stout – Wiley
Image: The image is credited to Neuroscience News
Original Research: Open access.
“ Exercise rejuvenates microglia and reverses T cell accumulation in the aged female mouse brain ” by Jana Vukovic et al. Aging Cell
Abstract
Exercise rejuvenates microglia and reverses T cell accumulation in the aged female mouse brain
Slowing and/or reversing brain ageing may alleviate cognitive impairments. Previous studies have found that exercise may mitigate cognitive decline, but the mechanisms underlying this remain largely unclear.
Here we provide unbiased analyses of single-cell RNA sequencing data, showing the impacts of exercise and ageing on specific cell types in the mouse hippocampus.
We demonstrate that exercise has a profound and selective effect on aged microglia, reverting their gene expression signature to that of young microglia.
Pharmacologic depletion of microglia further demonstrated that these cells are required for the stimulatory effects of exercise on hippocampal neurogenesis but not cognition.
Strikingly, allowing 18-month-old mice access to a running wheel did by and large also prevent and/or revert T cell presence in the ageing hippocampus.
Taken together, our data highlight the profound impact of exercise in rejuvenating aged microglia, associated pro-neurogenic effects and on peripheral immune cell presence in the ageing female mouse brain.
Study finds astrocytic pH regulator can repair blood-brain barrier, reverse brain damage caused by ischemic stroke
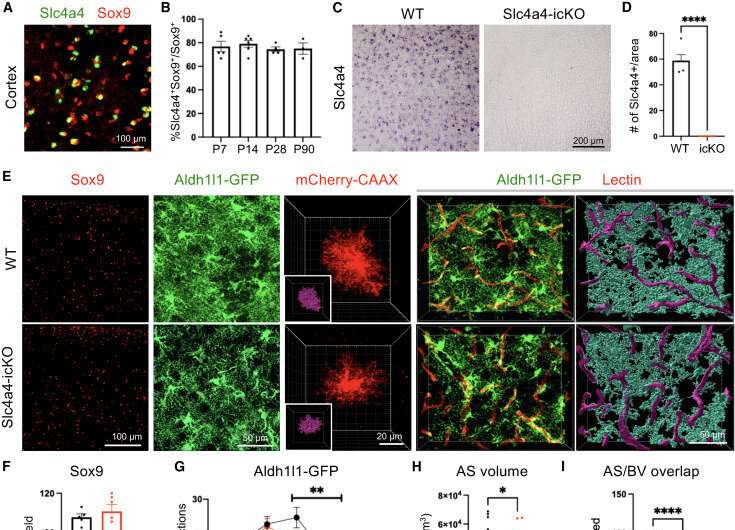
Slc4a4 is required for morphological complexity and proper Ca2+ propagation in the adult brain. Credit: Cell Reports (2024). DOI: 10.1016/j.celrep.2024.114193 Ischemic stroke is a leading cause of death and disability, affecting about 15 million worldwide each year. Among the various factors contributing to the pathogenesis of this condition is the loss of the blood-brain barrier, a highly selective protective cellular barrier that prevents harmful chemicals from entering the brain through the blood.
Understanding the mechanisms that regulate the integrity of the blood-brain barrier , developing strategies to repair it, and reversing brain damage will have far-reaching benefits for patients suffering from stroke and related neurological conditions.
A recent study from the laboratory of Dr. Hyun Kyoung Lee, associate professor at Baylor College of Medicine and an investigator at the Jan and Dan Duncan Neurological Research Institute (Duncan NRI) at Texas Children’s Hospital, has found that an ion transporter protein that regulates the pH of specific brain cells can repair the blood-brain barrier and restore normal brain function after ischemic stroke .
The study, published in Cell Reports , is the first to reveal novel and specific therapeutic targets for ischemic stroke and related brain conditions for which no targeted treatments exist currently. The blood-brain barrier and pH regulation are disrupted in stroke and other neurological conditions
“Disruption of blood-brain barrier integrity is a pathophysiological hallmark of stroke and several devastating neurological disorders,” Dr. Lee, a Cynthia and Anthony G. Petrello Endowed Scholar in Neurological Research, said.
“A damaged blood-brain barrier often leads to severe consequences such as brain edema, neuronal damage, and eventually, motor and cognitive deficits. Very little was known about how stroke damages the blood-brain barrier prior to this study.”
While endothelial cells form the core of the blood-brain barrier, emerging evidence suggests astrocytes, which are the most abundant and diverse type of support cells in the central nervous system, play a critical role in maintaining the integrity of this structure.
In addition to this barrier, a strict balance of pH (a measure of acidity or alkalinity of a solution) within the brain cells and their surrounding environment is crucial for optimal brain function. Dysregulation of pH homeostasis in the brain is often implicated in a range of neurological conditions.
Ischemic stroke injury is associated with a drastic reduction in pH. However, until this study, the precise reason for this alteration and the role of astrocytes in this process was not known. Astrocytic Slc4a4 plays a critical role in the maintenance of the blood-brain barrier
Previous studies have demonstrated that a sodium-carbonate cotransporter 1 (Slc4a4), which is enriched in the astrocytes, is responsible for shuttling acid-base ions across the cell membrane in a bidirectional manner to regulate both intra- and extracellular pH in response to internal and external stimuli. Moreover, patients with Slc4a4 variants have been associated with many brain disorders, including ischemic stroke.
This is the first study to investigate whether and how Slc4a4 governs astrocyte-endothelial cell interaction in blood-brain barrier maintenance and repair after stroke.
To test the biological role of Slc4a4, the Duncan NRI team generated a conditional mouse model of Slc4a4 using which they could specifically delete the expression of this gene in the brain astrocytes during development and in adult mice.
Using this mouse model , they found that deleting Slc4a4 from astrocytes altered their structure and function.
“We found that the brain vasculature was altered in the absence of astrocytic Slc4a4—there was >40% increase in the diameter of the blood vessels in the brain, a three-fold increase in the number of small molecules that were able to infiltrate the brain along with the loss of junctional markers—which together provided compelling evidence that the blood-brain barrier was disrupted in the absence of astrocytic Slc4a4 in these mice,” Dr. Qi Ye, lead author and postdoctoral fellow in the Lee lab said. Slc4a4 is critical for remodeling the blood-brain barrier after ischemic stroke
To test if astrocytic Slc4a4 was important for remodeling the blood-brain barrier after ischemic stroke, they used a cortical photothrombotic stroke model in Slc4a4 animal models. This stroke injury model in animals closely mimics the size, location, as well as reactive gliosis, a scar-like inflammatory response to ischemic stroke injury in human brains.
In this model using multi-omics analyses, they found that loss of astrocytic Slc4a4 increased the secretion of a CCL2, a pro-inflammatory molecule, which activated the CCR2 receptor present on the nearby endothelial cells to increase permeability, damaging the blood-brain barrier and increasing leakage between the two cell types. Finally, they found this breakdown of the blood-brain barrier was mediated by increased levels of specific metabolites (arginine and nitrous oxide) caused by changes in astrocytic pH levels.
“By revealing the precise mechanism and key players involved in the breakdown of the blood-brain barrier after stroke, this study has opened potential new avenues to treat ischemic stroke and several associated brain pathologies,” Dr. Lee said.
“It is promising that key players identified in this pathway—the Slc4a4 transporter protein, the CCL2-CCR2 axis as well the metabolites—are ‘druggable’ and can be developed into potential therapeutic targets.”
Provided by Texas Children’s Hospital
An astrocytic pH regulator that can repair the blood-brain barrier and reverse brain damage caused by ischemic stroke
Ischemic stroke is a leading cause of death and disability, affecting about 15 million worldwide each year. Among the various factors contributing to the pathogenesis of this condition is the loss of the blood-brain barrier, a highly selective protective cellular barrier that prevents harmful chemicals from entering the brain through the blood. Understanding the mechanisms that regulate the integrity of the blood-brain barrier, developing strategies to repair it, and reversing brain damage will have far-reaching benefits for patients suffering from stroke and related neurological conditions.
A recent study from the laboratory of Dr. Hyun Kyoung Lee, associate professor at Baylor College of Medicine and an investigator at the Jan and Dan Duncan Neurological Research Institute (Duncan NRI) at Texas Children’s Hospital, has found that an ion transporter protein that regulates the pH of specific brain cells can repair the blood-brain barrier and restore normal brain function after ischemic stroke.
The study, published in Cell Reports , is the first to reveal novel and specific therapeutic targets for ischemic stroke and related brain conditions for which no targeted treatments exist currently.
The blood-brain barrier and pH regulation are disrupted in stroke and other neurological conditions
“Disruption of blood-brain barrier integrity is a pathophysiological hallmark of stroke and several devastating neurological disorders,” Dr. Lee, a Cynthia and Anthony G. Petrello Endowed Scholar in Neurological Research, said. “A damaged blood-brain barrier often leads to severe consequences such as brain edema, neuronal damage, and eventually, motor and cognitive deficits. Very little was known about how stroke damages the blood-brain barrier prior to this study.
While endothelial cells form the core of the blood-brain barrier, emerging evidence suggests astrocytes, which are the most abundant and diverse type of support cells in the central nervous system, play a critical role in maintaining the integrity of this structure.
In addition to this barrier, a strict balance of pH (a measure of acidity or alkalinity of a solution) within the brain cells and their surrounding environment is crucial for optimal brain function. Dysregulation of pH homeostasis in the brain is often implicated in a range of neurological conditions.
Ischemic stroke injury is associated with a drastic reduction in pH. However, until this study, the precise reason for this alteration and the role of astrocytes in this process was not known.
Astrocytic Slc4a4 plays a critical role in the maintenance of the blood-brain barrier
Previous studies have demonstrated that a sodium-carbonate cotransporter 1 (Slc4a4), which is enriched in the astrocytes, is responsible for shuttling acid-base ions across the cell membrane in a bidirectional manner to regulate both intra- and extracellular pH in response to internal and external stimuli. Moreover, patients with Slc4a4 variants have been associated with many brain disorders, including ischemic stroke.
This is the first study to investigate whether and how Slc4a4 governs astrocyte-endothelial cell interaction in blood-brain barrier maintenance and repair after stroke.
To test the biological role of Slc4a4, the Duncan NRI team generated a conditional mouse model of Slc4a4 using which they could specifically delete the expression of this gene in the brain astrocytes during development and in adult mice.
Using this mouse model, they found that deleting Slc4a4 from astrocytes altered their structure and function. “We found that the brain vasculature was altered in the absence of astrocytic Slc4a4 — there was >40% increase in the diameter of the blood vessels in the brain, a three-fold increase in the number of small molecules that were able to infiltrate the brain along with the loss of junctional markers — which together provided compelling evidence that the blood-brain barrier was disrupted in the absence of astrocytic Slc4a4 in these mice,” Dr. Qi Ye, lead author and postdoctoral fellow in the Lee lab said.
Slc4a4 is critical for remodeling the blood-brain barrier after ischemic stroke
To test if astrocytic Slc4a4 was important for remodeling the blood-brain barrier after ischemic stroke, they used a cortical photothrombotic stroke model in Slc4a4 animal models. This stroke injury model in animals closely mimics the size, location, as well as reactive gliosis, a scar-like inflammatory response to ischemic stroke injury in human brains.
In this model using multi-omics analyses, they found that loss of astrocytic Slc4a4 increased the secretion of a CCL2, a pro-inflammatory molecule, which activated the CCR2 receptor present on the nearby endothelial cells to increase permeability, damaging the blood-brain barrier and increasing leakage between the two cell types. Finally, they found this breakdown of the blood-brain barrier was mediated by increased levels of specific metabolites (arginine and nitrous oxide) caused by changes in astrocytic pH levels.
“By revealing the precise mechanism and key players involved in the breakdown of the blood-brain barrier after stroke, this study has opened potential new avenues to treat ischemic stroke and several associated brain pathologies,” Dr. Lee said. “It is promising that key players identified in this pathway — the Slc4a4 transporter protein, the CCL2-CCR2 axis as well the metabolites — are ‘druggable’ and can be developed into potential therapeutic targets.”
Exercise stimulates brain function thanks to its effect on muscles, study suggests
Exercise gives the brain a boost, and may help protect against cognitive decline, but why? Image credit: NICK VEASEY/SCIENCE PHOTO LIBRARY/Getty Images. Exercise can stimulate brain-boosting molecules when muscles are active, a new study found.
By innervating muscle-tissue models, researchers found that the same nerves that signal muscles to move can also send neurotrophic factors — a type of biomolecule — into the brain.
Some evidence suggests that exercise can reverse or delay the cognitive decline associated with aging, but experts say future studies should allow for time and variations among individuals to see how physical activity can affect this.
Exercise plays a role in brain health by triggering molecules involved in cognitive function to be released by muscles, a recent study has shown.
The study, published in Proceedings of the National Academy of Sciences , shows that when nerves that stimulate muscles are activated, they also send signals to the brain by secreting bioactive molecules and nanoparticles that enhance brain function.
The findings illustrate the importance of maintaining musculoskeletal health, not just for cardiovascular health or mobility, but also to counteract neurological degeneration, Hyunjoon Kong, PhD , Robert W Schafer Professor in the Department of Chemical and Biomolecular Engineering at the University of Illinois Urbana-Champaign, corresponding author of this study, told Medical News Today .
He explained that: “Maintaining neuronal innervation is crucial for muscles to produce biological factors beneficial to the brain. With regular muscle contractions, muscles not only secrete these beneficial factors but also help sustain the innervation necessary for nerves to continue signaling muscles. This signaling is essential for regulating the release of neurotrophic factors into the brain.” The study involved stimulating muscles with glutamate to see how nerve function would respond. Researchers used models of muscle tissue, one that was innervated and one that was not, and discovered that the innervated tissue sent more signals to the brain.
Since some of the neuron function in muscles can decrease with age or injury, researchers were interested in discovering how this loss would affect brain health. How does exercise affect brain function?
In this study, the researchers did not observe people exercising. Rather, they looked at muscle models, meaning that it was not possible to draw immediate conclusions about particular forms of exercise and how they may vary in the way they interact with brain health.
Kong said that previous studies on exercise and brain health have found direct correlations between the size of the hippocampus and regular physical activity. But for this new study, the researchers examined the nervous system and musculoskeletal functions to achieve further understanding of brain-body interactions.
“Our study didn’t prove how exercise can improve cognitive function directly,” Kong cautioned. ”Several studies have already demonstrated that regular exercise can enhance cognitive function in adults. In these studies, participants were asked to do regular exercise, and the changes in the size of their hippocampi were monitored.” “Findings indicate that individuals who perform aerobic exercises regularly tend to have larger hippocampi and exhibit improved performance on spatial memory tests. What we focused on was how neurons connected with muscle influence one of the cross-talk routes between muscle and brain.”
– Hyunjoon Kong, PhD Ryan Glatt, CPT, NBC-HWC , senior brain health coach and director of the FitBrain Program at Pacific Neuroscience Institute in Santa Monica, CA, not involved in this research, told MNT that it would certainly take time to fully comprehend the effects of exercise on the brain, and future studies that used human participants would have to allow for that.
“The duration needed to observe the effects of exercise on cognitive function can vary based on the type, intensity, and frequency of exercise, as well as individual differences in age, baseline cognitive function, and health status,” Glatt said.
“Research typically indicates observable effects within a range of a few weeks to several months. It’s crucial for subsequent studies to consider these variables to accurately assess the timeframe,” he noted. What types of exercise are best for brain health?
There are some notable benefits to regular exercise for brain health. Boxing, for example, has been used to help people with Parkinson’s disease .
Glatt acknowledged that certain forms of exercise may be more effective than others for enhancing brain health, especially activities that require cognitive function.
“Aerobic exercises, like running, swimming, and cycling, which improve cardiovascular health, are widely noted for their positive impacts on brain function,” he said.
“However, activities that combine physical and cognitive demands — such as dance and team sports — may offer additional benefits due to their requirement for coordination, rhythm, and executive functions,” he added. Can exercise reverse or delay cognitive decline?
Kong suggested that physical activity can potentially reverse or delay the cognitive decline associated with getting older.
“As individuals age, they gradually lose the well-formed neuromuscular junctions between nerves and muscles, impairing the muscles’ ability to be regulated by nerve signals and subsequently reducing their capacity to secrete factors critical for brain function,” Kong explained.
“With appropriate training or stimulation for muscle contractions, muscles can produce factors that help maintain these neuromuscular junctions, thus preventing denervation. As a result, elderly individuals can still possess functional innervated muscles capable of producing important factors that enhance cognitive function in the brain,” he noted.
Glatt pointed out that a sedentary lifestyle, with relatively low levels of physical activity, can be associated with a higher risk of cognitive decline.
But he cautioned that there are a number of variations among individuals regarding genetics, lifestyle choices, and environmental factors.
“Exercise is increasingly recognized as a supportive intervention for individuals with compromised cognitive functions, including those affected by age-related declines or conditions like Alzheimer’s disease. Physical activity can enhance blood flow to the brain, reduce inflammation, and stimulate the release of growth factors, which may help to maintain or improve cognitive function,” Glatt said.
“While exercise is beneficial for maintaining cognitive health and potentially slowing the progression of decline, the evidence on its ability to reverse existing cognitive impairment is still inconclusive. Most studies suggest that exercise can contribute to […]
6 Things to Add to Your Routine to Maintain Brain Fitness as You Age

Westend6/Getty Images We all want to age gracefully. We’ll do just about anything to do it. From eating for heart health to deciding which exercises to focus on or improving vision , most people know that maintaining many aspects of physical health is crucial for longevity. What you might not think about regularly is your brain fitness as you age.
Cognition declines over time due to several factors, such as age-related structure changes, brain injuries or excess stress hormones. According to the Centers for Disease Control and Prevention, one in nine American adults over 65 reports cognitive decline.
“The parts of our brain that help with learning information and remembering can become smaller, and the brain can weigh less as we age,” said Colleen Marshall , chief clinical officer for Two Chairs .
While we will all experience health changes as we age, cognitive decline doesn’t happen at the same rate for everyone. By prioritizing brain fitness now, you can help slow the change and keep your mind sharp as you age. Start doing these 6 things to nourish your brain for healthy aging
Solve puzzles
We’ll start with the easiest strategy to integrate into your daily life: puzzles. Solving puzzles can benefit the brain in several ways, from improving memory to boosting problem-solving skills.
“They may slow the rate of cognitive decline and how quickly the brain decreases in size as we age,” Marshall said.
A study published in the journal Neurology reported that playing games like checkers or completing jigsaw puzzles can delay the onset of Alzheimer’s by about five years . Different research supports the idea that solving crossword puzzles or journaling can lower the risk of dementia .
Experts suggest that puzzles help curb cognitive decline because they expand the brain’s cognitive reserve , or the ability to solve and cope with problems. Activities to try include putting together jigsaw puzzles or solving other types of puzzles, such as Sudoku, crosswords, memory games and math problems. Learn a new skill
Like stimulating the brain by playing games or solving puzzles, learning a new skill has short-term and long-term advantages. By learning a new skill, you’re strategically activating several parts of your brain simultaneously. You’re also promoting neuroplasticity by creating new pathways and strengthening those connections as you continue honing the skill.
It could be learning a new language, painting or trying out a new sport. Just make sure it’s challenging or complex, and continue to practice for the best brain results. Vladimir Vladimirov/Getty Images Prioritize sleep
Sleep is one of the most important things you can do for your body. While I’m not saying there’s a right or wrong way to sleep, research suggests that how much sleep you get and the quality of your sleep influence your risk for dementia . According to a study published in the Journal of Neuroscience, a single night of sleep deprivation can age your brain .
A lot goes on in the brain while we sleep, including clearing out toxins and creating new neural pathways. If you don’t get enough sleep, your brain doesn’t have time to carry out these functions and cognition suffers.
Establishing a bedtime routine can have a big impact on your sleep quality . From reading a book to practicing yoga before bed, integrating relaxation into your night can help boost your sleep . Focus on your nutrition
What you eat also will influence the rate of cognitive decline you experience as you age. Studies have found that people who follow the Mediterranean and MIND (Mediterranean-Dash Intervention for Neurodegenerative Delay) diets tend to have fewer cognitive impairments and dementias compared to those following other diets. More research is needed to conclude why this is true. However, it might have something to do with the way those diets prioritize foods that protect the brain with anti-inflammatory and antioxidant properties .
Read more: Master the Mediterranean Diet With the Help of These Tips and Recipes
No matter if you choose to follow a strict diet or just improve your current meal rotation, you’ll want to focus on improving your blood sugar and dropping high levels of LDL cholesterol to reduce your risk of dementia.
Foods to incorporate into your diet for better brain health : Leafy greens like spinach, kale and lettuce
Salmon
Dark berries
Nuts
Greek yogurt
Dark chocolate
Green tea
Vegetables like broccoli and carrots
Exercise Studies have found that following an active lifestyle is associated with lower cognitive decline over time. Your heart rate increases when you exercise, which increases blood flow to the brain. This can help spark new development of nerve cells, a process called neurogenesis . Exercise also promotes increased connections between cells, making the brain more adaptive.Generally, any exercise that’s good for the body will also help the mind. It doesn’t have to be lifting weights; walking, swimming and dancing also achieve the same results. Read more : How Exercise Helps Boost Your Memory-Brain Health as You Age Halfpoint Images/Getty Images Make connections with others Marshall pointed out that prioritizing high-quality relationships with others can benefit the brain. According to a meta-analysis of longitudinal cohort studies , limited or poor relationships were associated with cognitive decline.Prioritizing social contact is an essential part of aging well. Whether spending time with your family or putting yourself out there at your local community center, staying connected is an integral part of aging gracefully. Too long; didn’t read? Our brains change as we age; there is no way around it. However, integrating any of these easy habits into your routine can help nourish and safeguard your brain for the future.There are also a few things you should avoid to keep your brain in top shape. Heavy cigarette smoking has been associated with cognitive decline in middle age. Marshall added that heavy drinking , poor diet and unmanaged high blood pressure can also negatively impact the brain as we age.Don’t worry; there’s still time to turn it around. Even if you smoke now, quitting has […]
Mindful Extracts: ‘Shroom Boom’ hits the High Street

Functional mushrooms have been used in traditional medicine throughout Asia for centuries and the rest of the world is finally catching on – the global market was valued at nearly 30 million USD in 2023. Market research indicates the mushroom supplement sector is growing at 10 per cent CAGR and many are calling this rapid growth in the sector the ‘Shroom Boom’.
Mindful Extracts’ range of functional mushroom supplements is now available on the high street, at Holland & Barrett stores nationwide.
Working with a leading mycologist, Mindful Extracts has formulated each product to be highly potent, dual extracting the mushrooms in hot water and alcohol to concentrate the beneficial compounds including beta-glucans and triterpenes. The products are independently lab tested for any pollutants and are certified organic.
The range includes Organic Reishi, Organic Lion’s Mane, Organic Chaga and an Organic Mushroom Blend. Mindful Extracts’ Team Celebrate Launch at Holland & Barrett Stores Reishi is one of the most celebrated functional mushrooms in Chinese medical literature. Also known as the ‘mushroom of immortality’, it is believed to promote vitality, longevity and homeostasis (balance) in our system.
One of the key benefits of Chaga is its powerful antioxidant properties which may support the body’s natural defence mechanisms and promote overall well-being. Chaga is packed full of antioxidants, vitamins, and minerals, which can reduce inflammation, support a strong immune system, aid heart health and promote good digestion.
Lion’s Mane is a natural nootropic and can help boost cognitive ability. Many people claim Lion’s Mane improves their focus and concentration, similar to a strong coffee but without the stimulating and jittery effects. It can also promote improvements in mood and general wellbeing, as well as feeling more in the present moment.
Research has shown that Lion’s Mane can increase Nerve Growth Factor (NGF), which is responsible for the maintenance and growth of neurons in the brain. Many neurological diseases such as Dementia, Parkinson’s and Huntington’s disease are linked to the degeneration of neurons over time, and it is thought that neurotrophic factors like NGF may play a role in preventing these conditions. Mindful Extracts Reishi The Mindful Extracts Organic Mushroom Blend includes Lion’s Mane, Reishi, Chaga and Shiitake. Each medicinal mushroom brings a huge range of benefits to balance your body and mind: Lion’s Mane, the super mushroom reported to boost memory and support cognitive function. Reishi promotes vitality and longevity with its immune system boosting properties and indications that it can reduce inflammation. Chaga, packed full of antioxidants, is said to reduce inflammation, support a strong immune system and promote good digestion. Shiitake, full of fibre, vitamins and minerals, contains polysaccharides and terpenoids, which have immune-boosting and cholesterol-lowering effects.
The range is available in-store at Holland & Barrett and online .
Can Anxiety Relief Come at the Cost of Cognitive Health?

Key points
Long-term use of benzos can lead to addiction & cognitive impairments.
Older people are particularly vulnerable to the impairing effects of long-term benzodiazepine use.
A recent study revealed the mechanism by which benzos interfere with plasticity and cognitive abilities.
Other treatments such as CBT & life-style changes can alleviate anxiety without the use of benzodiazepines.
Benzodiazepines, often referred to as “benzos,” are commonly prescribed medications used to treat conditions such as anxiety and insomnia . These include drugs like Ativan, Xanax, and Clonazepam. In the United States alone, millions of people use these anti- anxiety medications. Over the past decade, research has indicated that prolonged use of these drugs may be associated with addiction and cognitive impairments, including dementia , particularly in individuals aged 60 and above.
For instance, a study published in the British Medical Journal discovered a correlation between dementia and the use of anti-anxiety medications like benzos. The study followed nearly 9,000 older adults for six years after they began using the medication for insomnia or anxiety. The findings suggested that those who used benzos were 51 percent more likely to develop dementia, and the risk increased the longer the drugs were used (1).
Another study compared over 70,000 non-institutionalized Finnish men and women diagnosed with dementia from 2005-2010 with a larger demographic-matched group without dementia (2). The researchers concluded that individuals taking benzodiazepines and related drugs had a slightly increased risk of developing dementia.
The type of benzo taken did not affect the dementia risk. However, many of the individuals taking benzos were also on antidepressants or antipsychotic drugs, which could have also contributed to the development of dementia. The authors advised against the use of benzos, especially in older individuals.
In September 2020, the FDA announced that they would update the “black box warning” for benzodiazepines to include information about the risks of physical dependence, withdrawal reactions, misuse, abuse, and addiction (3). This was in addition to a previous warning about the risks of taking benzodiazepines concurrently with opiates, which could lead to death (4).
While these studies do not establish a cause-and-effect relationship, they do suggest a strong correlation between long-term benzo use and dementia. The mechanism for how long-term use of benzo could lead to cognitive impairments has been unknown.
However, a study published in 2022 shed some light on a possible mechanism by which benzos lead to dementia . Researchers at the Australian Nuclear Science and Technology Organization (ANSTO) conducted a study showing how diazepam, a commonly prescribed benzo, can impair the structural plasticity of dendritic spines, leading to cognitive impairments in mice.
The researchers used a unique lab model called “Guwiyang Wurra-TSPO knockout,” a healthy mouse lacking a protein present in the mitochondrion, the cell’s energy-providing organelle (5). Anti-anxiety drugs like diazepam bind to TSPO on the surface of microglial cell organelles. Microglial cells are the brain’s first immune responders and are implicated in dementia, long COVID , chronic fatigue and other cognitive impairments.
In animal models without TSPO, the physiological impairments associated with cognitive impairment from diazepam use were not observed. In addition, the study found that TSPO-mediated loss of dendritic spines accelerated cognitive decline . This is in contrast to the traditional view that benzos work by enhancing the inhibitory GABA synapses in the brain, thus calming the mind.
Anti-anxiety drugs may promote cognitive decline directly and indirectly in several ways:
> Impact on microglial cells: For example, promoting the movement of microglial cells interferes with dendritic spines’ plasticity (areas in synaptic connections critical for learning, memory , and plasticity).
Alteration to brain wiring: Long-term use of benzos alters the complex wiring of the brain. For example, the supporting microglial cells indirectly help maintain the functions of these circuits. Benzos interfere with glial cells.
Side-effects of the medications: Benzos have side effects such as confusion, clouded thinking, and memory lapses. These side-effects can make learning, which is essential for protecting the brain against cognitive decline, challenging.
Other mechanisms: Although one mechanism has been revealed, other mechanisms may also be involved.
Unsurprisingly, both the Harvard Health Publishing News and the American Geriatric Association have listed benzos as inappropriate for older adults. Fortunately, other options for treating anxiety exist. Alternative treatments include:
> Cognitive behavioral therapy (CBT): CBT is a well-established therapeutic approach for anxiety. It focuses on identifying and changing negative thought patterns and behaviors. A trained therapist can guide you through this process.
Mindfulness and meditation : Mindfulness practices, such as meditation, deep breathing exercises, prayers, and progressive muscle relaxation, can help reduce anxiety. They promote relaxation and self-awareness.
Physical activity : Regular exercise has been shown to reduce anxiety. It releases endorphins, which are natural mood lifters. Physical exercise also keeps the brain fit . Choose an activity you enjoy, whether it’s walking, yoga, dancing, or swimming.
Limit caffeine and alcohol and avoid recreational drugs : Alcohol and recreational drugs can exacerbate anxiety. Reducing or avoiding them can make a difference. Caffeine can elicit many of the physiological symptoms that can trigger anxiety, such as rapid heartbeat.
Sleep hygiene : Lack of sleep can worsen anxiety. Prioritize good sleep habits, such as maintaining a consistent sleep schedule and creating a relaxing bedtime routine. The authors of an article published in Neurotherapeutics in 2019 recommend that doctors be “very cautious” before prescribing benzos to older people and recommend encouraging good sleep hygiene to alleviate the symptoms of anxiety and insomnia (6).
In conclusion, while further research is needed to categorically conclude that long-term use of benzos causes dementia, the evidence strongly points to the perils of long-term use of benzos. This warning is even more credible after recent studies have shed light on the specific mechanisms by which benzos may lead to cognitive impairment. Fortunately, successful alternative treatments exist. Note: Do not stop taking your prescribed anti-anxiety medications without consulting with a doctor. References(1) Billioti de Gage, S., Moride, Y., Ducruet, T., et al. (2014). Benzodiazepine use and risk of Alzheimer’s disease: case-control study. BMJ 349, g5205.(2) Tapiainen, V., Taipale, H., Tanskanen, A., et […]
Study suggests eating these superfoods can help you live longer

Over the years, numerous observational studies have reported a strong link between higher intakes of flavonoid-rich foods and a lower risk of chronic disease and mortality.
Flavonoids, sometimes called vitamin P , are polyphenolic compounds commonly found in colorful fruits and vegetables, as well as in plant-based food products like cocoa, tea and wine. These naturally occurring chemicals possess many health-supporting properties, such as antioxidant, anti-inflammatory and even anticancer activities.
In a recent study published in the journal BMC Medicine , an international team of researchers explored how a high-flavonoid diet can impact longevity and found that increasing your consumption of certain flavonoid-rich foods can reduce your risk of early death . Eat these foods to live a long and healthy life
Flavonoids are some of the most studied bioactive compounds in plant-based foods. They are hailed for their role in protecting against many chronic diseases, which stems from their ability to neutralize free radicals and fight oxidative stress.
Oxidative stress, defined as an imbalance between the levels of oxidants (free radicals) and antioxidants inside the body, has long been linked to the development of chronic disease , primarily due to the irreversible damage it causes on healthy cells and tissues.
As compounds with naturally high antioxidant activities, flavonoids are capable of suppressing disease-causing free radical activity, making them valuable and highly desirable components of the human diet.
Human knowledge is under attack! Governments and powerful corporations are using censorship to wipe out humanity’s knowledge base about nutrition, herbs, self-reliance, natural immunity, food production, preparedness and much more. We are preserving human knowledge using AI technology while building the infrastructure of human freedom. Use our decentralized, blockchain-based, uncensorable free speech platform at Brighteon.io . Explore our free, downloadable generative AI tools at Brighteon.AI . Support our efforts to build the infrastructure of human freedom by shopping at HealthRangerStore.com , featuring lab-tested, certified organic, non-GMO foods and nutritional solutions.
While most plant-based foods contain flavonoids, some boast uniquely high concentrations of these phytochemicals. Apples, berries, citrus fruits, dark chocolate, green tea and red wine are some common examples of flavonoid-rich superfoods . (Related: The mighty BLUEBERRY, a superfruit with anticancer properties .)
For their study, the researchers looked at the associations between changes in the habitual intake of flavonoid-rich foods and the risk of all-cause and cause-specific mortality. They focused specifically on how eight-year changes in intakes of individual flavonoid-rich foods and the “flavodiet” scores of individual participants affected their longevity. The flavodiet refers to a novel composite measure of flavonoid-rich foods and drinks.
All the data analyzed in the study came from 55,786 American females from the Nurses’ Health Study (NHS) and 29,800 American males from the Health Professionals Follow-up Study (HPFS). These participants were all healthy and had no diagnosis of any chronic disease prior to the analyses.
The researchers reported that between 1986 and 2018, a total of 15,293 and 8,988 deaths were documented in the NHS and HPFS, respectively. Among the flavonoid-rich foods they evaluated, blueberries , red wine and peppers had the most significant impact on total and all-cause mortality risk. (Related: Is eating chili peppers the key to a longer life? Studies link chili consumption to lower risk of dying from heart disease, cancer .)
An increase of 3.5 servings per week in the intake of blueberries, red wine and peppers reduced the participants’ risk of all-cause mortality by five percent, four percent and nine percent, respectively. Meanwhile, an increase of seven servings per week of green tea lowered the participants’ all-cause mortality risk by three percent.
In addition, the researchers found that an increase of three servings per day in the participants’ flavodiet scores was associated with an eight percent lower risk of all-cause mortality and a 13 percent lower risk of death from neurological diseases. This suggests that you could add more to your lifespan and prevent diseases like Alzheimer’s by increasing your daily consumption of flavonoid-rich foods, specifically blueberries, peppers, red wine and green tea.
The researchers noted, however, that some flavonoid-rich foods had a completely opposite effect. In particular, they found that a 3.5 serving per week increase in the intake of onions and grapefruit was associated with a five percent and six percent higher risk of all-cause mortality, respectively. Strawberries and oranges also had a similar effect, suggesting that these foods should be consumed in moderation instead of in high amounts.
Although red wine had a favorable impact on mortality risk, it is still advisable to consume alcohol moderately. The American Heart Association recommends drinking no more than one (4 ounces) to two glasses per day for adult men and one glass per day for adult women. When consumed in moderation, red wine is said to provide cardioprotective benefits, thanks to a non-flavonoid polyphenol called resveratrol that is found in the skin of dark-colored grapes. Fight obesity with these flavonoid-rich foods
According to research, the average total flavonoid intake in the United States is only about 250 to 400 milligrams (mg) per day — lower than the average intake in the United Kingdom and Australia and about the same as in China and Europe, where the major food sources of flavonoids are tea, citrus fruits and juices, berries, wine and apples. (Related: Study: Citrus fruits can help you maintain healthy cognitive function as you age .)
Because of the many health benefits offered by flavonoid-rich foods, experts believe that increasing the consumption of such foods is one of the keys to improving the overall health of Americans. Statistics show that roughly two out of three adults in the U.S. are overweight or obese ; but studies have found that a diet high in flavonoids can help individuals shed extra pounds and maintain a healthy weight .
According to a study published in BMJ , foods that are rich in flavonols, flavan-3-ols, anthocyanins and flavonoid polymers are the best ones to add to a weight-loss diet. To increase your intake of these flavonoids, consider eating more of these superfoods:
Flavonol sources Onion
Kale
Lettuce
Tomatoes
Apples
Grapes
Berries
Green tea The most studied […]
Researchers demonstrate a new mechanism of neural plasticity underlying learning and memory processes
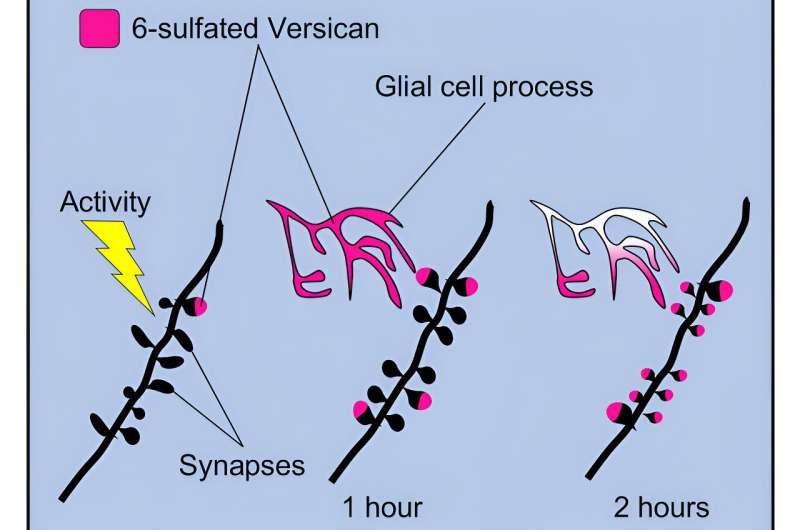
Graphical abstract. Credit: Cell Reports (2024). DOI: 10.1016/j.celrep.2024.114112 Neurons are important, but they are not everything. Indeed, it is “cartilage,” in the form of clusters of extracellular matrix molecules called chondroitin sulfates, located in the outside nerve cells, that plays a crucial role in the brain’s ability to acquire and store information.
A study published in Cell Reports describes a new mechanism of brain plasticity , or how nerve connections change in response to external stimuli. The paper is titled “Focal clusters of peri-synaptic matrix contribute to activity-dependent plasticity and memory in mice.”
The work stems from a collaboration between the Harvard Medical School, the University of Trento, and the German Center for Neurodegenerative Diseases (DZNE) in Magdeburg.
“Sensory skills and the ability to understand our surroundings depend on the activity of the brain, which enables us to perceive and process stimuli that come from the outside world. Through our brains we are able to acquire and store new information, and to remember information we have already acquired,” say Yuri Bozzi and Gabriele Chelini.
“This fascinating phenomenon is made possible by the brain’s ability to continuously change the structure and effectiveness of neuronal connections (synapses) in response to external stimuli . An ability that goes by the name of synaptic plasticity. Understanding how synaptic modifications occur and how they contribute to learning and memory is one of the great challenges in neuroscience.”
Yuri Bozzi is a professor at the University of Trento and co-senior author. Gabriele Chelini is the first author of the study. Chelini worked on this project starting in 2017, as a postdoctoral fellow in a lab directed by Sabina Berretta (McLean Hospital and Harvard Medical School, Boston), and completed the scientific publication during his years as a postdoctoral fellow in Bozzi’s lab at the University of Trento.
At the center of the research are chondroitin sulfates, molecules well known for their role in joints, which also play a crucial function in brain plasticity, being an integral part of the brain’s extracellular matrix, as was originally discovered in 2001 by Dr. Alexander Dityatev’s group.
In 2007, a Japanese study described the presence of clusters of chondroitin sulfates, circular in shape, scattered seemingly randomly in the brain. This work had slipped into oblivion, however, until Sabina Berretta’s translational neuroscience laboratory brought these structures back to the attention of the scientific community, renaming them CS-6 clusters (from chondroitin sulfate-6, which identifies their precise molecular composition) and demonstrating how these structures were associated with glial cells and were severely reduced in the brains of people with psychotic disorders .
Then in 2017, Gabriele Chelini, newly hired in Berretta’s lab, was tasked with revealing the function of these clusters.
“First we went to explore these structures in detail, visualizing them at very high resolution. We found that they are essentially clusters of synapses coated with CS-6 and organized in a clearly recognizable geometric shape. We then highlighted a new type of synaptic organization,” the scholars recount.
“At this point, we had to use some ‘experimental creativity’; with a combination of behavioral, molecular and refined morphological approaches, we realized that these connections encapsulated in CS-6 clusters change in response to electrical activity in the brain.”
“Finally, through collaboration with Alexander Dityatev at DZNE Magdeburg, and the efforts of Hadi Mirzapourdelavar from his group, we attenuated the expression of CS-6 in the hippocampus (the region of the brain responsible for spatial learning ), and demonstrated that the presence of CS-6 is necessary for synaptic plasticity and spatial memory,” Bozzi and Chelini point out.
“This work paves the way for a new way of thinking about brain functioning. It is possible that all synapses formed on different neurons within CS-6 clusters have the ability to respond chorally to specific environmental stimuli, and are involved in a common function aimed at learning and memory processes,” they note.
“They seem to represent a new substrate of information integration and association formation at the multicellular level,” add Dityatev and Berretta.
The work is the result of a collaboration between several laboratories, including the translational neuroscience laboratory (Sabina Berretta; McLean Hospital—Harvard Medical School, Boston), the neurodevelopmental disorders research laboratory (Yuri Bozzi; CIMeC—Centro Interdipartimentale Mente/Cervello, University of Trento) and the Molecular Neuroplasticity laboratory (Alexander Dityatev; DZNE Magdeburg).
Provided by University of Trento
‘Mathematical microscope’ reveals novel, energy-efficient mechanism of working memory that works even during sleep
Credit: Pixabay/CC0 Public Domain UCLA Health researchers have discovered a mechanism that creates memories while reducing metabolic cost, even during sleep. This efficient memory occurs in a part of the brain that is crucial for learning and memory, and where Alzheimer’s disease begins.
The discovery is published in the journal Nature Communications .
Does this sound familiar? You go to the kitchen to fetch something, but when you get there, you forget what you wanted. This is your working memory failing. Working memory is defined as remembering some information for a short period while you go about doing other things. We use working memory virtually all the time.
Alzheimer’s and dementia patients have working memory deficits, and it also shows up in mild cognitive impairment (MCI). Hence, considerable effort has been devoted to understand the mechanisms by which the vast networks of neurons in the brain create working memory.
During working memory tasks, the outermost layer of the brain, known as the neocortex, sends sensory information to deeper regions of the brain, including a central region called the entorhinal cortex, which is crucial for forming memories. Neurons in the entorhinal cortex show a complex array of responses, which have puzzled scientists for a long time and resulted in the 2014 Nobel Prize in medicine, yet the mechanisms governing this complexity are unknown. The entorhinal cortex is where Alzheimer’s disease begins forming.
“It’s therefore critical to understand what kind of magic happens in the cortico-entorhinal network, when the neocortex speaks to the entorhinal cortex which turns it into working memory. It could provide an early diagnostic of Alzheimer’s disease and related dementia, and mild cognitive impairment,” said corresponding author Mayank Mehta, a neurophysicist and head of the W. M. Keck Center for Neurophysics and the Center for Physics of Life at UCLA.
To crack this problem, Mehta and his co-authors devised a novel approach: a “mathematical microscope.”
In the world of physics, mathematical models are commonly used, from Kepler to Newton and Einstein, to reveal amazing things we have never seen or even imagined, such as the inner workings of subatomic particles and the inside of a black hole. Mathematical models are used in brain sciences too, but their predictions are not taken as seriously as in physics. The reason is that in physics, predictions of mathematical theories are tested quantitatively, not just qualitatively.
Such quantitatively precise experimental tests of mathematical theories are commonly believed to be unfeasible in biology because the brain is vastly more complex than the physical world. Mathematical theories in physics are very simple, involving very few free parameters and hence precise experimental tests. In contrast, the brain has billions of neurons and trillions of connections, a mathematical nightmare, let alone a highly precise microscope.
“To tackle this seemingly impossible challenge of devising a simple theory that can still explain the experimental of data of memory dynamics in vivo data with high precision, we hypothesized that cortico-entorhinal dialog, and memory magic, will occur even when the subjects are sleeping, or anesthetized,” said Dr. Krishna Choudhary, the lead author of the study. “Just like a car behaves like a car when it’s idling or going at 70 mph.”
The researchers then made another large assumption: The dynamics of the entire cortex and the entorhinal cortex during sleep or anesthesia can be captured by just two neurons. These assumptions reduced the problem of billions of neurons’ interactions to just two free variables—the strength of input from the neocortex to entorhinal cortex and the strength of recurrent connections within the entorhinal cortex. While this makes the problem mathematically tractable, it raises the obvious question—is it true?
“If we test our theory quantitatively on data in vivo, then these are just interesting mathematical games, not a solid understanding of memory-making magic,” said Mehta.
The crucial experimental tests of this theory required sophisticated experiments by Dr. Thomas Hahn, a co-author who is now professor at Basel University and a clinical psychologist.
“The entorhinal cortex is a complicated circuit. To really test the theory we needed experimental techniques that can not only measure the neural activity with high precision, but also determine the precise anatomical identity of the neuron,” said Hahn.
Hahn and Dr. Sven Berberich, also a co-author, measured the membrane potential of identified neurons from the entorhinal cortex in vivo, using whole cell patch clamp technique and then anatomical techniques to identify the neuron. Simultaneously they measured the activity of the parietal cortex, a part of the neocortex that sends inputs to the entorhinal cortex.
“A mathematical theory and sophisticated in vivo data are necessary and cool, but we had to tackle one more challenge—how does one map this simple theory onto complex neural data?” said Mehta.
“This required a protracted period of development, to generate a ‘mathematical microscope’ that can directly reveal the inner workings of neurons as they make memory,” said Choudhary. “As far as we know, this has not been done before.”
The authors observed that like an ocean wave forming and then crashing onto a shoreline, the signals from the neocortex oscillate between on and off states in intervals while a person or animal sleeps. Meanwhile, the entorhinal cortex acted like a swimmer in the water who can move up when the wave forms and then down when it recedes. The data showed this and the model captured this as well. But using this simple match the model then took a life of its own and discovered a new type of memory state known as spontaneous persistent inactivity, said Mehta.
“It’s as if a wave comes in and the entorhinal cortex said, ‘There is no wave. I’m going to remember that recently there was no wave so I am going to ignore this current wave and not respond at all.’ This is persistent inactivity,” Mehta said. “Alternately, persistent activity occurs when the cortical wave disappears but the entorhinal neurons remember that there was a wave very recently, and continue rolling forward.”
While many theories of working memory had shown the presence of persistent activity, which the authors found, the persistent inactivity was something that the […]
Nerves prompt muscle to release factors that boost brain health, study finds
Illinois researchers used a novel tissue model to examine the effect of nerve stimulation on muscle secretion of brain-boosting factors. The nerves, colored green, trigger the muscle to release hormones and mRNA packages that foster growth of and connection between neurons in the brain. Credit: Kai Yu Huang Exercise prompts muscles to release molecular cargo that boosts brain cell function and connection, but the process is not well understood. New research from the University of Illinois Urbana-Champaign has found that the nerves that tell muscles to move also prompt them to release more of the brain-boosting factors.
“The molecules released from the go into the bloodstream and then to the brain, producing so-called crosstalk between the muscle and brain. But the muscle itself is highly innervated. So we wondered, what is the effect of the neurons on this activity of the muscle, and further down to the communication between muscle and brain?” said chemical and biomolecular engineering professor Hyunjoon Kong, leader of the study published in the Proceedings of the National Academy of Sciences .
“As we get older, we lose these neurons from the muscle. And some people also lose these neurons to disease or injury. So understanding their role, and how these nerves to the muscle affect the brain, is important for older people or patients with neuromuscular injuries and diseases,” he said.
Research on exercise has found that muscles secrete hormones and extracellular vesicles, tiny packages that carry molecules between cells, containing small fragments of RNA that enhance connection, signal transmission and communication between brain cells. However, while much attention has been paid to the function of muscle-derived factors, the role of the nerves that stimulate the muscle is poorly understood, said graduate student Kai-Yu Huang, the first author of the study.
To fill this gap, the researchers compared two muscle tissue models—one with neuron innervation and one without. They found that the innervated muscle produced more molecules that promote brain neuron activity and regulate muscle development than the muscle without nerves.
Then, the researchers stimulated the nerves with glutamate, a neurotransmitter. They found that the innervated muscle had greater expression of a gene important for regulating secretion. Correspondingly, it emitted higher levels of the hormone irisin, which is associated with beneficial effects of exercise, and released more extracellular vesicles than plain muscle.
“We analyzed the cargo carried in the vesicles, and we found that there was a greater diversity of microRNA associated with impact on neurodevelopment,” said Huang. “These findings highlight the importance of neuron innervation. As we get older, we lose nerve supply to muscle, and our muscles start to break down and lose function. And somehow, this can further result in organ dysfunction. So understanding how to regulate or maintain muscle’s secreting behavior is very important.”
Next, the researchers plan to look further into mechanisms at the junction where the neurons meet the muscle cells to determine how nerve impulses are stimulating the muscle and whether they affect the production of the brain-boosting factors or just their release, an important distinction for possible treatments for those who have lost nerves or muscle. They also hope to explore using their tissue model as a platform for effectively producing the factors. Ultimately, they hope to have a complete picture of the brain-nerve-muscle loop and how to maintain it.
“It’s our individual organs talking to each other: The brain tells the nerves to stimulate the muscle, and the muscle releases back molecules beneficial for brain function,” Kong said. “It underscores the importance of exercise. Exercise creates a more robust interface between motor neurons and muscle, and now we know the nerves sending the signal into the muscle releases the molecules and extracellular vesicles that are beneficial to the brain. So we could look at the benefits of exercise focused on fostering that connection more than simply increasing the volume or strength of the muscle.”
Scientists Have Discovered Cognitive Benefits of Creatine

Researchers at Forschungszentrum Jülich have found that a high single dose of creatine can temporarily enhance cognitive functions impaired by sleep deprivation, specifically improving processing capacity and short-term memory. The study cautions against excessive creatine intake due to potential health risks, although it suggests future potential for cognitive enhancement with lower doses. Creatine, a widely used supplement among athletes to enhance physical performance, has been found to also temporarily boost cognitive abilities affected by sleep deprivation. This discovery was made in a scientific study conducted by researchers at Forschungszentrum Jülich , with the results published in the journal Scientific Reports . Processing capacity and short-term memory significantly improved
As part of the study, 15 test subjects were kept awake overnight and had to solve cognitive tasks during this time. Sleep deprivation leads to changes in brain metabolism that promote the cellular uptake of creatine. Beforehand, the test subjects had received a high single dose of creatine, an important metabolic product that is found in food and can also be produced by the body itself.
Three hours after taking the creatine, a positive effect on the brain metabolism and cognitive performance of the test subjects could already be observed. The effect reached its peak after four hours and lasted up to nine hours. In particular, improvements in processing capacity and short-term memory were seen.
“The results suggest that a single but high dose of creatine enhances thinking capacity and causes changes in the brain’s energy reserves during sleep deprivation,” says Dr. Ali Gordjinejad, coordinator of the study from the Institute of Neuroscience and Medicine (INM-2) at Forschungszentrum Jülich. Excessive intake of creatine not recommended
Various studies have already reported improvements in cognitive performance after a long creatine diet. The substance also counteracts the metabolic changes caused by sleep deprivation. This is why the Jülich researchers considered creatine a potential candidate for this study.
It had not previously been possible to prove the short-term effect that has now been observed, as the neuronal cells of the central nervous system (CNS) can only absorb creatine to a small extent. They normally cover their needs largely through their own synthesis. It was only by putting the brain in a “stressed” state through the experimental conditions in the Jülich study that the increased uptake of creatine in the cells was fostered.
“For the time being, however, it is not advisable for people to take such a high dose of creatine at home, as high doses of the substance put a heavy strain on the kidneys and can cause health risks,” says Dr. Gordjinejad. “However, if future studies show an increase in cognitive performance at lower doses, creatine might become a serious competitor to coffee during long working nights.”
Reference: “Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation” by Ali Gordji-Nejad, Andreas Matusch, Sophie Kleedörfer, Harshal Jayeshkumar Patel, Alexander Drzezga, David Elmenhorst, Ferdinand Binkofski and Andreas Bauer, 28 February 2024, Scientific Reports .
DOI: 10.1038/s41598-024-54249-9
Sleep resets brain connections for a few hours, but then what happens?
In a study involving zebrafish, a team of scientists led by the University College London (UCL) has explored how the brain manages synaptic connections during sleep .
The experts found that the brain weakens new neural connections that were forged during waking hours, but this process only accounts for the first few hours of sleep. Function of sleep is still unclear
“Although sleep is conserved across the animal kingdom, the precise functions of sleep remain unclear. As sleep deprivation leads to acute impairment of cognitive performance, many theories posit that synaptic plasticity associated with learning and memory preferentially occurs during sleep,” wrote the study authors.
“For example, the synaptic homeostasis hypothesis (SHY) proposes that synaptic potentiation during wakefulness results in an ultimately unsustainable increase in synaptic strength and number that must be renormalized during sleep through synaptic weakening and pruning. Such sleep-dependent renormalization has been postulated to broadly affect most excitatory synapses throughout the brain.” The synaptic homeostasis hypothesis
The findings support the synaptic homeostasis hypothesis, positing that sleep functions as a crucial reset mechanism for the brain, ensuring energy sustainability and readiness for new learning.
“Some studies examining either large neuronal populations or small patches of dendrites have found evidence consistent with the synaptic homeostasis hypothesis, but whether sleep merely functions as a permissive state or actively promotes synaptic downregulation at the scale of whole neurons is unclear,” wrote the researchers. The brain goes offline
“When we are awake, the connections between brain cells get stronger and more complex. If this activity were to continue unabated, it would be energetically unsustainable,” said senior author Jason Rihel, a professor in the UCL Cell & Developmental Biology department.
“Too many active connections between brain cells could prevent new connections from being made the following day. While the function of sleep remains mysterious, it may be serving as an ‘offline’ period when those connections can be weakened across the brain, in preparation for us to learn new things the following day.” Synaptic connections in the brain during sleep
The researchers used optically translucent zebrafish with genes that allow for easy imaging of synapses – the structures enabling communication between brain cells.
“To examine the scope and selectivity of sleep-linked synaptic plasticity, it is vital to comprehensively track the synaptic changes of individual neurons through sleep-wake states,” wrote the study authors.
“To that end, we used in vivo synaptic labeling tools in larval zebrafish to image the same neurons and their synapses repeatedly over long timescales, enabling us to map single-neuron synapse changes across sleep and wake states.” Significant changes in the first half of the night
By observing these fish over multiple sleep-wake cycles, they discovered that synaptic connections increase during wakefulness and decrease during sleep, particularly when sleep was postponed, indicating that sleep pressure intensifies this reduction.
The study revealed that the significant synaptic changes primarily occur during the first half of the night, coinciding with the peak period of slow-wave activity, a critical phase of the sleep cycle. Sleep dampens connections in the brain
“Our findings add weight to the theory that sleep serves to dampen connections within the brain, preparing for more learning and new connections again the next day,” said lead author Anya Suppermpool from UCL Cell & Developmental Biology and UCL Ear Institute.
“But our study doesn’t tell us anything about what happens in the second half of the night. There are other theories around sleep being a time for clearance of waste in the brain, or repair for damaged cells – perhaps other functions kick in for the second half of the night.”
This research not only deepens our understanding of sleep’s role in synaptic management but also poses new questions about the functions of its later stages, paving the way for future investigations into the full spectrum of sleep’s impact on brain health .
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap , a free app brought to you by Eric Ralls and Earth.com.
—–
Researchers unveil mechanism enhancing cellular fitness against aging and neurodegeneration

Researchers at Duke University Medical Center discover a mechanism to enhance the fitness of cells against aging and neurodegenerative diseases. This finding will pave the way for novel therapeutic approaches in neuroprotection against aging-related disorders and neurodegeneration.
Durham, North Carolina; USA; April 30, 2024. A research study by scientists at Duke University Medical Center uncovered activities of a target, called Ranbp2 that remodel the expression of chaperones in neuronal tissues prone to photo-damage and accelerated aging. The work of researchers led by Dr. Paulo Ferreira at Duke indicates that the remodeling of a network of chaperones by Ranbp2 preordains the protection of certain cells and tissues against noxious stressors, which compromise neuronal function and survival.
Chaperones belong to a family of diverse proteins, which play essential but complementary roles in maintaining the homeostasis of proteins in cells. Chaperones prevent the malfunctioning, damage, clumping, and deposits of proteins by associating with substrates and by promoting their stability. Chaperones also facilitate the proper degradation (turnover) of proteins. Impairment of protein homeostasis that causes protein deposits is a hallmark feature of neurodegenerative diseases, such as Age-Related Macular Degeneration (AMD), Alzheimer’s, Amyotrophic Lateral Sclerosis (ALS), Parkinson’s, and other diseases. Notably, aging also subdues the induction of chaperones. This outcome is thought to compromise cellular fitness and how cells cope against a wide spectrum of environmental stressors.
The researchers at Duke found that loss of a foldase activity linked to Ranbp2 induces the robust up-regulation of a subset of chaperones, called Crystallins. In addition, they found that the induction of Crystallins leads to a decline of proteins targeted for degradation with aging. Crystallins are conspicuously soluble, and they provide lifelong transparency and structural stability to the lens of the eye, where they predominate. Photodamage of the lens Crystallins leads to cataracts and vision impairment with aging.
The study found that basal levels of expression of Crystallins are found in other tissues, such as those lining the back of the eye – the retina and the retinal pigment epithelium (RPE). These tissues are critical for the initiation and processing of vision before visual signals are transmitted to the brain. These tissues are also highly prone to photodamage with aging. The confluence of these factors with genetic predispositions is associated with AMD disease, a prevalent neurodegenerative and blindness disease of the elderly.
The current findings uncover novel approaches for targeting therapeutically selective activities of Ranbp2 to enable the induction of critical chaperones and to promote cellular fitness. The research work indicates that the chaperones, Crystallins, will enhance the protection of the retina and RPE from damage, and improper degradation and clumping of proteins triggered by photo-oxidative stressors. These effects of Crystallins’ induction are anticipated to prevent or to delay the onset and progression of malfunction and degeneration of these tissues, and thereby preserve vision.
Source:
Duke University Medical Center
Journal reference:
Patil, H., et al. (2024). Proteostatic Remodeling of Small Heat Shock Chaperones─Crystallins by Ran-Binding Protein 2─and the Peptidyl-Prolyl cis–trans Isomerase and Chaperone Activities of Its Cyclophilin Domain. ACS Chemical Neuroscience . doi.org/10.1021/acschemneuro.3c00792 .
Scientists discover new immunosuppressive mechanism in brain cancer
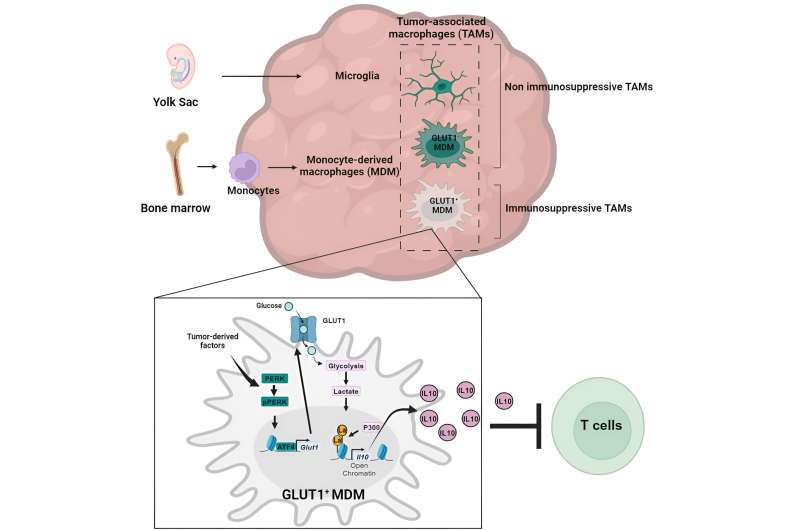
Graphical abstract. Credit: Immunity (2024). DOI: 10.1016/j.immuni.2024.04.006 The Wistar Institute assistant professor Filippo Veglia, Ph.D., and team, have discovered a key mechanism of how glioblastoma—a serious and often fatal brain cancer—suppresses the immune system so that the tumor can grow unimpeded by the body’s defenses.
The lab’s discovery was published in the paper, “Glucose-driven histone lactylation promotes the immunosuppressive activity of monocyte-derived macrophages in glioblastoma ,” in the journal Immunity .
“Our study shows that the cellular mechanisms of cancer’s self-preservation, when sufficiently understood, can be used against the disease very effectively,” said Dr. Veglia.
“I look forward to future research on metabolism-driven mechanisms of immunosuppression in glioblastoma, and I’m hopeful for all that we will continue to learn about how to best understand and fight this cancer.”
Until now, it has been poorly understood how monocyte-derived macrophages and microglia create an immunosuppressive tumor microenvironment in glioblastoma.
The Veglia lab investigated the cellular “how” of glioblastoma immunosuppression and identified that, as glioblastoma progressed, monocyte-derived macrophages came to outnumber microglia—which indicated that monocyte-derived macrophages’ eventuality to becoming the majority in the tumor microenvironment was advantageous to the cancer’s goal of evading immune response.
Indeed, monocyte-derived macrophages, but not microglia, blocked the activity of T cells ( immune cells that destroy tumor cells), in preclinical models and patients. The team confirmed this finding when they assessed preclinical models of glioblastoma with artificially reduced numbers of monocyte-derived macrophages.
And as the group expected, the models with fewer malicious macrophages in the tumor microenvironment showed improved outcomes relative to the standard glioblastoma models.
Glioblastoma accounts for slightly more than half of all malignancies that originate in the brain, and the prognosis for those diagnosed with the cancer is quite poor: Only 25% of patients who receive a glioblastoma diagnosis will survive beyond a year. Glioblastoma is inherently dangerous due to its location in the brain and its immunosuppressive tumor microenvironment, which renders glioblastoma resistant to promising immunotherapies.
By programming certain immune cells like macrophages, (such as monocyte-derived macrophages and microglia), to work for—rather than against—the tumor, glioblastoma fosters a tumor microenvironment for itself that enables the cancer to grow aggressively while evading anticancer immune responses. Wistar Insitute’s Dr. Filippo Veglia. Credit: The Wistar Institute Having confirmed the role of monocyte-derived macrophages, the Veglia lab then sought to understand just how the cancer-allied immune cells were working against the immune system.
They sequenced the macrophages in question to see whether the cells had any aberrant gene expression patterns that could point to which gene(s) could be playing a role in immunosuppression, and they also investigated the metabolic patterns of macrophages to see whether the macrophages’ nonstandard gene expression could be tied to metabolism.
The team’s twin gene expression & metabolic analysis led them to glucose metabolism . Through a series of tests, the Veglia lab was able to determine that monocyte-derived macrophages with enhanced glucose metabolism and expressing GLUT1, a major transporter for glucose (a key metabolic compound), blocked T cells’ function by releasing interleukin-10 (IL-10).
The team demonstrated that glioblastoma-perturbed glucose metabolism in these macrophages induced their immunosuppressive activity.
The team discovered the key to macrophages’ glucose-metabolism-driven immunosuppressive potency lies in a process called “histone lactylation.” Histones are structural proteins in the genome that play a key role in which genes—like IL-10—are expressed in which contexts.
As rapidly glucose-metabolizing cells, monocyte-derived macrophages produce lactate, a by-product of glucose metabolism. And histones can become “lactylated” (which is when lactate becomes incorporated into histones) in such a way that the histones’ organization further promotes the expression of IL-10—which is effectively produced by monocyte-derived macrophages to help cancer cells to grow.
But how can the glucose-driven immunosuppressive activity of monocyte-derived macrophages be stopped? Dr. Veglia and his research team identified a possible solution: PERK, an enzyme they had identified as regulating glucose metabolism and GLUT1 expression in macrophages.
In preclinical models of glioblastoma, targeting PERK impaired histone lactylation and immunosuppressive activity of macrophages, and in combination with immunotherapy blocked glioblastoma progression and induced long-lasting immunity that protected the brain from tumor re-growth—a sign that targeting PERK-histone lactylation axis may be a viable strategy for fighting this deadly brain cancer.
Provided by The Wistar Institute
Scientists Identify New Brain Circuit That Inhibits Appetite

Researchers have discovered a brain circuit in mice that inhibits eating when nauseous, pinpointing unique amygdala nerve cells that operate differently from those activated during satiety, highlighting the complex regulation of appetite. A neural pathway suppresses appetite when experiencing nausea.
Feeling full, nauseous, or anxious can all contribute to a decrease in appetite. Postponing meals may be the body’s natural way to avoid additional harm and allow for recovery. Scientists at the Max Planck Institute for Biological Intelligence have discovered a specific brain pathway that stops mice from eating when they experience nausea.
The decisive role is played by special nerve cells in the amygdala – a brain region involved when emotions run high. The cells are activated during nausea and elicit appetite-suppressing signals. The findings highlight the complex regulation of eating behavior, as the loss of appetite during nausea is controlled by different circuits than during satiety.
An upcoming exam, a boat trip on the high seas, or the next germ at the daycare center all have one thing in common: they can really upset our stomach. Stress, motion sickness, or certain infections can make us feel sick. It seems logical that we don’t eat in these circumstances and wait for the situation to improve. As a result, nausea and decreased appetite usually go hand in hand. Or have you ever felt sick and really wanted to eat at the same time? Specialized nerve cells in the amygdala are activated during nausea and elicit appetite-suppressing signals. Credit: MPI for Biological Intelligence/ Julia Kuhl What seems logical is a healthy defense mechanism of our body – but it has to be activated first. Clearly, the brain plays a central role in this: it is the control center for the body’s energy balance and regulates eating behavior.
So how does the brain prevent us from eating when we feel sick? Researchers in Rüdiger Klein’s department have gained new insights into this topic in mice. They focused on the amygdala, a brain region that regulates emotions, also those related to eating. It contains neurons that promote eating and those that inhibit appetite. For example, a known inhibitory cell type is activated when we are full, but how this works in the case of nausea is not well understood. Nausea activates nerve cells
Wenyu Ding, first author of the new study, now discovered another cell group in the amygdala that has a negative influence on appetite. Unlike the previously known cell type, these cells are not activated by satiety, but when feeling nauseous.
When the researchers artificially switched on the cells, even hungry mice stopped eating. Conversely, switching the cells off resulted in the mice eating, even when feeling sick. This Sketchnote summarizes the most important findings of the new paper. Credit: MPI for Biological Intelligence / Christina Bielmeier To better understand how this cell type exerts its appetite-suppressing function, the researchers analyzed the underlying circuit: where do the cells get their information from and to which cells and brain areas do they send their projections?
The following picture emerged: When a mouse feels sick, this information reaches the brain and eventually the amygdala. There, the new cell type is activated and sends its inhibitory signals to distant brain regions, including the so-called parabrachial nucleus, a brain stem region that receives a lot of information about the internal state of the body.
This stands in contrast to the circuit of the previously known cell type, which mainly interacts with neighboring cells within the amygdala. It becomes clear that the loss of appetite during satiety is not the same as the loss of appetite during nausea. In the brain, different cells and circuits are responsible for this – a complicated matter and perhaps a small consolation the next time we feel sick.
Most importantly, the new study provides important insights into how the brain and the amygdala in particular regulate eating behavior. This is the prerequisite for a better understanding of the many diseases associated with dysregulated eating behavior in humans.
Reference: “Nausea-induced suppression of feeding is mediated by central amygdala Dlk1-expressing neurons” by Wenyu Ding, Helena Weltzien, Christian Peters and Rüdiger Klein, 27 March 2024, Cell Reports .
DOI: 10.1016/j.celrep.2024.113990
Researchers at NYU Abu Dhabi’s Photonics Research Lab have developed a new two-dimensional material that can precisely manipulate light, promising enhancements in bandwidth for communication networks and optical systems. This breakthrough in tunable optical materials demonstrates potential applications in environmental sensing, optical imaging, and neuromorphic computing. (Artist’s concept.) Credit: SciTechDaily.com NYU Abu Dhabi researchers have unveiled a novel 2D material improving optical modulation for advanced systems and communications.
Responding to the increasing demand for efficient, tunable optical materials capable of precise light modulation to create greater bandwidth in communication networks and advanced optical systems, a team of researchers at NYU Abu Dhabi’s Photonics Research Lab (PRL) has developed a novel, two-dimensional (2D) material capable of manipulating light with exceptional precision and minimal loss.
Tunable optical materials (TOMs) are revolutionizing modern optoelectronics, electronic devices that detect, generate, and control light. In integrated photonics circuits, precise control over the optical properties of materials is crucial for unlocking groundbreaking and diverse applications in light manipulation. Two-dimensional materials like Transition Metal Dichalcogenides (TMDs) and graphene exhibit remarkable optical responses to external stimuli. However, achieving distinctive modulation across a short-wave infrared (SWIR) region while maintaining precise phase control at low signal loss within a compact footprint has been a persistent challenge.
In a new paper titled “Electro-Optic Tuning in Composite Silicon Photonics Based on Ferroionic 2D Materials” published in Nature Light Science & Application , the team of scientists, led by Research Scientist Ghada Dushaq, and Associate Professor of Electrical Engineering and Director of PRL Lab Mahmoud Rasras, have demonstrated a novel avenue for active light manipulation through the utilization of ferroionic, 2D material CuCrP 2 S 6 (CCPS). By integrating first-of-their-kind, two-dimensional, and atomically thin materials into minuscule ring structures on silicon chips, the team has enhanced the efficiency and compactness of the device.
When integrated onto silicon optical devices, these 2D materials exhibit a remarkable […]
8 Brain-Boosters for the Aging Mind

brain boosters Have you lost a step?
Feel like the years are finally catching up? Just looking to spruce things up and turn back the biological clock? Wish there was an easy way to recharge your brain?
Turns out, it’s not all just in your head. In fact, many studies point to the fact that Black men and women may be aging biologically faster than other races. While the exact reasons are unknown, researchers believe that socioeconomic barriers, such as stress, diet, and living conditions, may be to blame.
But it doesn’t have to be this way. Here are eight absolute brain-boosters to help as you age.
You May Also Like
If You or Someone You Love has Bladder Cancer, Learn More About These Studies 1. Brain & Memory Apps
Turns out technology isn’t just for youngins! If you’re looking for ways to get your gears turning, look no further than online applications. If you need some help getting access, just ask your kids or grandkids. Programs like Lumosity and BrainHQ have been linked to moderate improvements in memory and other cognitive abilities. Not only that, they’re fun and varied, keeping you entertained as you make real-life gains. 2. Monopoly Much?
Sometimes, it’s good to be puzzled. Whether it’s crossword puzzles, Poker, Chess, or math games like Sudoku, the best thing you can do for thinking is… to think! In fact, some studies have found a 15 percent reduction in dementia prevalence among seniors who regularly game it up. By creating new neural connections, puzzles and games can go a long way.
RELATED: The 7 Best Brain-Boosting Foods 3. Audiobooks
Remember the old days when we had to actually read books? Well, if you don’t have the time or just want to put something on in the background, consider audiobooks. Hey, as long as the narrator has a nice voice, what can go wrong? Audiobooks are useful because they improve time management, force us to multitask, and don’t allow us to reread like we would with normal books. This, in turn, allows your mind to comprehend language more rapidly. A win-win! 4. Socializing
Okay, so maybe your ‘clubbing’ days are over with, but that doesn’t mean you need to sit inside all day in front of your TV! If you’re finding your mind is losing its luster, now’s the time to get out. Many studies have linked socializing to improved cognitive performance, better mood, and a lower likelihood of developing Alzheimer’s and dementia. The reason? Simple. As we socialize, we engage many parts of our brain. We’re talking, looking, and constantly adapting to how others think, feel, and behave.
You May Also Like
Real Housewives Star Describes Terrifying Medical Experience!
Whether it’s just a little chat over lunch or a part-time job, being around others is good for you! 5. Cooking & Baking
Fire up the oven and get the brain cookin’!
Just think about it. Maybe you’re reading from a cookbook. Perhaps you’re measuring out ingredients. You’re adjusting dials on the stove, you’re boiling water, you’re creating sauces, you’re checking temperatures – you’re encountering various
smells, sounds, sights, textures, and tastes. It can be a lot, but all of that can do wonders for keeping your mind active and sharp.
So… Bon appétit! 6. Exercise
You already know exercise is important, but what if you’re physically limited due to age? Well, no need to rest on your laurels just yet. Simple walks, stretching, and even yoga and meditation are great ways to ease your body into activity. Take your time, never rush recovery, and enjoy the countless science-backed benefits of exercise! Your brain will thank you.
And speaking of benefits, a little weight lifting and weight resistance can also be great for aging bones.
You May Also Like
If You or Someone You Love has Bladder Cancer, Learn More About These Studies 7. Listening to Music
They don’t call it ‘music medicine’ for no reason. Whether it’s jazz, rock, pop, blues, country, rap, hip hop – or whatever – music does the mind (and soul) good. Overall, music is linked to many mental health benefits. It triggers memories and imagination. It stimulates blood flow to various brain regions, reducing anxiety and depression while boosting mood, memory, focus, and sleep.
So, what are you waiting for? Pop out that ol’ vinyl!
RELATED: 5 Activities to Keep Your Mind Sharp for Years to Come 8. Have a Chuckle
Life can get pretty dark, but your reaction to those tough moments is what ultimately matters. If you’re always tense and serious, your mind and body will act accordingly. Over time, the stress hormone cortisol can wear you down, causing damage to your brain and body. Chronic inflammation, disease, and mental degeneration can all occur as a result.
By having a laugh, watching comedy, and loosening up, you can preserve both your mind and body for longer.But that’s life, isn’t it? It’s all about rolling with the punches and keeping a healthy perspective. If you can learn to live and love, taking things in stride, you can keep your mind and body going strong.Don’t let aging get you down. Hold your head high and keep it up!
How the brain structure that produces norepinephrine also helps control visual attention

Credit: Pixabay/CC0 Public Domain The locus coeruleus (LC) is a small region of the brainstem that produces norepinephrine, a chemical with powerful effects on arousal and wakefulness which plays an important role in the body’s response to stress or panic. Now, research from the University of Chicago shows it plays a specific role in visual sensory processing as well.
In a study, titled “Locus coeruleus norepinephrine selectively controls visual attention ” and published in Neuron , neuroscientists artificially increased neuronal activity in the LC by briefly shining light on genetically modified neurons. They saw that this manipulation selectively enhanced performance in non-human primates performing a visual attention task, underscoring the crucial role that attention plays in sensory perception.
“We want to understand what changes in your brain when you pay attention to something in the environment, because attention greatly affects your ability to discern stimuli,” said John Maunsell, Ph.D., the Albert D. Lasker Distinguished Service Professor of Neurobiology and Director of the Neuroscience Institute at the University of Chicago, and co-author of the study.
“Now we have found a brain structure that has strong signals related to whether the subjects are paying attention to a stimulus or not, and we see big differences in how its neurons respond depending on where that attention is directed.”
Maunsell and co-author Supriya Ghosh, Ph.D., a postdoctoral researcher, focus their studies on how neurons in different areas of the brain change to represent sensory input when a subject is paying attention to a stimulus or not. For example, activity of neurons in the cerebral cortex may increase by 10–25% when a subject pays attention to the stimuli those neurons represent.
Previous research has shown that LC activation, coupled with its ensuing norepinephrine production, might improve performance on tasks that require attention to discern between visual stimuli.
Ghosh, who specializes in subcortical brain structures, suggested that the LC might be a good candidate to study for these effects. The team trained two monkeys to perform a visual task in which they paid attention to the left or right side of a screen. First, a sample image would appear on both sides of the screen.
Next, after a delay, a test image would appear on one side of the screen. The monkey would report if that image was oriented differently than the sample shown earlier on that side of the screen by moving its eyes to one of two targets. The researchers recorded neuron activity in the LC during the task and saw that activity increased greatly—and only—when the animal attended to the image that appeared on the side of the screen monitored by those neurons.
To see if there was a causal relationship between this increased activity and performance, they also used a method called optogenetics to increase activity in the LC while the animals were performing the task. Optogenetics allows researchers to selectively control the activity of norepinephrine-expressing cells via light.
First, they introduce a genetic modification that causes neurons to produce a light-sensitive protein called opsin, the same type of protein that photoreceptors in the eye use to detect light. When they shine a special light on these neurons, the opsin causes the neurons to fire.
Optogenetically boosting the responses of the neurons drastically improved the animals’ ability to differentiate the shapes on the corresponding half of the screen, without affecting motor processing.
“This kind of artificial enhancement of that activity did not interfere with other cognitive factors either, such as motor actions or decision-related activities,” Ghosh said. “So, it could selectively contribute to the perceptual sensitivity in a very precise way.”
Distinguishing the effects of attention from other factors, like decision-making or motor movements, is crucial, Ghosh said. Those processes take place in other parts of the brain, and can contribute to performance independently. Understanding how a relatively small brain structure like the LC impacts such an important function as attention is also one step toward solving the overall puzzle of the brain.
“Every time we get more information about the likely contribution of a given brain structure, or how broad the range of functions of a given structure might be, that gives us much more power to understand the relationships among them,” Maunsell said. “No one part of the brain does interesting behaviors by itself.”
Provided by University of Chicago
Noninvasive Brain Stimulation Shows Rapid Relief for Major Depression
0
Noninvasive transcranial alternating current stimulation (tACS) may lead to rapid improvement in major depressive disorder (MDD), results of a randomized, sham-controlled trial suggested. However, independent experts said more research is needed to confirm its benefit.
While both the active and sham tACS groups exhibited similar clinically significant improvements in self-reported depression severity, post hoc analyses showed active tACS was superior to sham in women and in those with high adherence to treatment.
“We can feel reasonably confident that tACS is an effective treatment for people with MDD, particularly for women, as long as people use it consistently,” study investigator Philip Gehrman, PhD, Department of Psychiatry, University of Pennsylvania Perelman School of Medicine, Philadelphia, told Medscape Medical News .
“Improvements in depression were seen as early as the first week of treatment, and these benefits were maintained for the duration of the study,” added co-investigator Kyle Lapidus, MD, PhD, with Affective Care in New York City.
The study was published online April 22 in the Journal of Clinical Psychiatry . Seeking FDA Approval
tACS is a form of wearable noninvasive brain stimulation that delivers a low intensity, pulsed, alternating current via scalp electrodes. The current study utilized the OAK (version 2.0) tACS device from Fisher Wallace Laboratories, which funded the study. The OAK tACS device. A total of 255 adults (185 women) meeting the criteria for MDD and having a score on the Beck Depression Inventory, Second Edition (BDI-II) between 20 and 63 (mean score, 34) were randomly allocated to at-home active or sham tACS for two, 20-minute treatment sessions daily for 4 weeks.
Both treatment groups showed similar clinically significant improvements in mean BDI-II scores at week 2 compared with baseline (the primary efficacy outcome), with no significant difference between groups ( P = .056).
Post hoc analysis of participants with 100% compliance in the first 14 days showed a significantly greater improvement in BDI-II scores at week 2 in the active vs sham tACS group ( P = .005), and this was true at 1 week ( P = .022) and 4 weeks ( P = .018).
In preplanned subgroup analyses, treatment effects were greatest among women for whom active tACS was superior to sham tACS across time points.
“Active tACS greatly exceeded the 17.5% threshold of minimally clinically important within-group difference established for the BDI-II. Side effects were minimal and mild,” the authors reported in their article.
“The speed of response is also impressive and suggests that tACS may be able to provide rapid relief in depression with very limited side effects. Given the risks associated with unmanaged MDD, rapid relief is essential,” said Lapidus .
The researchers noted that the large improvements in the sham group make it tough to know how much of the treatment effect was due to the direct effects of the tACS device vs placebo effects. Having participants in both groups engage in 20 minutes twice daily of calm activities during active and sham tACS may itself have therapeutic benefits irrespective of tACS.
Limitations of the study include reliance on self-reported patient outcome measures and the relatively short 4-week treatment period.
“The next step is to do a longer study to prove the duration of efficacy of tACS in MDD is longer than 4 weeks,” study investigator Eric Bartky, MD, with Bartky HealthCare Center, LLC, Livingston, New Jersey, told Medscape Medical News.
On that front, Fisher Wallace said a new 12-week study using their tACS device was designed by Maurizio Fava, MD, psychiatrist-in-chief at Massachusetts General Hospital, Boston, to assess the durability and effectiveness of treatment in men and women. The company intends to use the results of this 12-week study to seek US Food and Drug Administration (FDA) approval. Promising but Preliminary
Reached for comment, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto, Toronto, Canada, and head of the Mood Disorders Psychopharmacology Unit, said the efficacy being reported with tACS is “promising but needs to be replicated in a much larger study.”
McIntyre, who wasn’t involved in the study, told Medscape Medical News tACS is “an interesting approach, not only from the point of view of the therapeutic, but also the ecosystem. There is interest in identifying ways to improve access and availability to treatment for depression. Clearly that is the major problem confronting many Americans.”
“If we can democratize the access and have home-based care, that clearly would be an improvement over status quo, but, of course, it will need to be guided by best practices, safety, and efficacy, and I look forward to seeing more studies with it,” McIntyre added.
Flavio Frohlich, PhD, professor, Department of Psychiatry, University of North Carolina (UNC) at Chapel Hill and director of the Carolina Center for Neurostimulation, also emphasized the need for more study.
“In general, having portable, low amplitude, electric brain stimulation devices for psychiatric indications is really exciting. However, this study misses some of the things that we would typically see in gold standard clinical trials of depression treatments,” Frohlich, who also wasn’t involved in the study, told Medscape Medical News .
One is sole reliance on self-report. “While it’s important to get self-reports from patients, what we’re usually looking for is a clinician-administered rating scale, such as the Hamilton Depression Rating Scale, which would offer some more reassurance,” Frohlich said.
“It’s also important to note that the main analysis did not show a statistically significant difference between the active and the placebo group. There were some interesting exploratory findings, but overall, I would be very cautious in drawing major conclusions from it. It’s clear that much more study is needed,” Frohlich added.
The study was sponsored by Fisher Wallace Laboratories Inc. Gehrman, Lapidus and Bartky disclosed financial relationships with the company. McIntyre received speaker/consultation fees from Lundbeck, Janssen, Alkermes, Neumora Therapeutics, Boehringer Ingelheim, Sage, Biogen, Mitsubishi Tanabe, Purdue, Pfizer, Otsuka, Takeda, Neurocrine, Sunovion, Bausch Health, Axsome, Novo Nordisk, Kris, Sanofi, Eisai, Intra-Cellular, NewBridge Pharmaceuticals, Viatris, AbbVie, Atai Life Sciences. McIntyre is a CEO of Braxia Scientific Corp. Frohlich is the lead inventor of intellectual property issued to UNC and licensed to […]
Could menopause be delayed? The answer could lead to longer lifespans for women
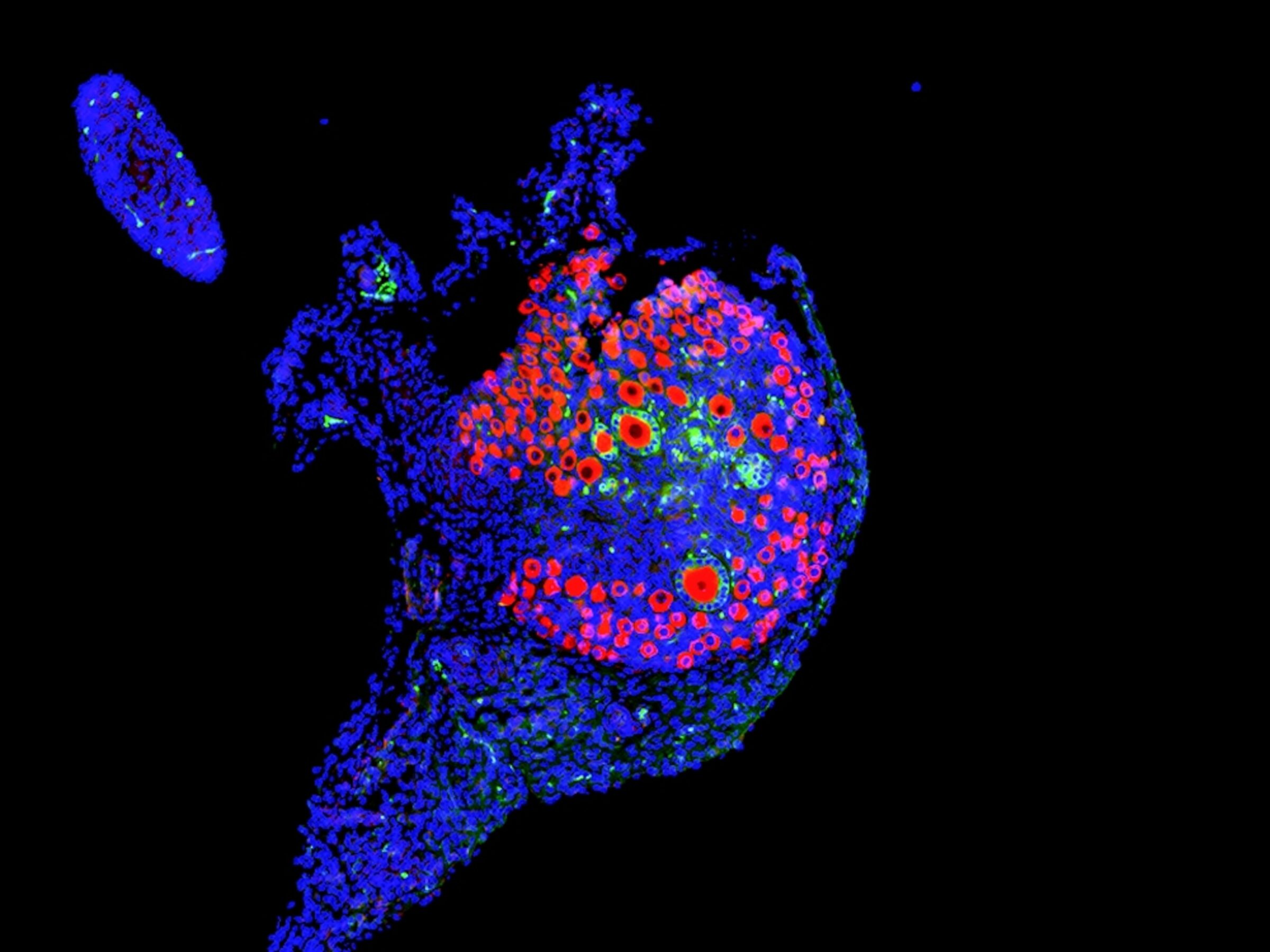
Scientists are learning that ovaries aren’t just important for making babies—they also keep the heart, brain, and bones healthy. A mouse ovary treated with a high dose of anti-Mullerian hormone (AMH)—a hormone naturally produced by follicles in the ovary—shows more small, dormant follicles and fewer larger ones. At high levels, AMH acts… Micrograph by David Pepin
When a woman goes through menopause—defined as not having a period for at least 12 months—the health impacts are immediate and dramatic.
That’s because ovaries (aside from their reproductive function) are endocrine organs. And when they stop pumping out the cocktail of chemicals that communicate with almost every tissue in the body, everything from the brain to the muscles to the skin is affected.
“Your risk of osteoporosis goes up overnight, your risk of cardiovascular disease goes up overnight,” says Jennifer Garrison, a neuroscientist at the Buck Institute for Research on Aging in California. And this seismic shift often hits between the ages of 45 and 55 (average age of onset is 51), coinciding with a woman’s peak years in the workforce. A study released by the Mayo Clinic estimates that in the United States, menopause is responsible for up to $1.8 billion in lost work time and more than $26 billion in medical costs.
“Ovaries are the architects of healthy aging in women,” Garrison says. So, it doesn’t make sense to talk about women’s health and longevity without considering reproductive longevity. For example, why do ovaries, which begin to show signs of age in a woman’s 30s, deteriorate decades earlier than other organs? Why do some people reach menopause earlier or later than average? And most importantly, if we could delay menopause, by keeping the ovaries functioning for longer, would that translate to more years of good health?
Unfortunately, for a long time research on reproductive health was laser-focused on fertility and the child-bearing years. David Pepin, a reproductive biologist at Harvard, recalls meeting with the U.S. Food and Drug Administration five years ago to discuss funding. A normal mouse ovary shows many immature eggs—or oocytes—in red. Larger oocytes surrounded by green hormone-producing granulosa cells indicate growing follicles; one oocyte will usually grow large enough to be released during ovulation. “I couldn’t convince them that having your ovaries function and make hormones is—in itself— important; that the ovaries are not just to make babies,” says Pepin. As a result, he’s had to be resourceful. Some of the work he’s done on the life cycle of ovaries has been funded by its applications for controlling the population of domestic cats .
But the tide is turning.
“There’s been an exponential increase in interest and research” in the last five years, says Garrison, who in 2020 co-founded the Global Consortium for Reproductive Longevity and Equality , an initiative that funds scientists, fosters collaborations, and educates the public about the crucial role of reproductive health in women’s health. “Suddenly, at aging research conferences, reproductive aging is represented now, whereas it wasn’t two or three years ago.” Why ovaries matter
Healthy ovaries produce a series of molecules that send signals to distant organs to help them function. Among the best studied is estrogen, which ebbs and flows with the menstrual cycle and peaks in the days before ovulation. But estrogen receptors—the molecules that grab estrogen, triggering downstream actions in cells and tissues—are present throughout the body, extending estrogen’s reach far beyond the reproductive organs.
When estrogen binds to its receptor, the resulting complex acts on DNA to switch some genes on, and others off. Estrogen, therefore, has its fingers in a lot of pies. In the cardiovascular system, the hormone helps widen blood vessels and ensure their lining is smooth and slippery , which lowers blood pressure and prevents clots from forming. In the brain, it’s neuroprotective — dampening inflammation, promoting healthy synapses, and clearing away misfolded proteins. In the musculoskeletal system, estrogen helps build and repair muscles as well as maintain bone.
( What happens during menopause? Science is finally piecing it together. )
The loss of estrogen, therefore, puts women at increased risk for developing diabetes , cardiovascular disease , dementia , osteoporosis , and more . On the flip side, individuals who become menopausal later in life compared to their peers tend to live longer and healthier. This benefit extends even to their male siblings , pointing to a potential genetic link between reproductive health and overall longevity. How ovaries age
Although scientists have characterized some consequences of ovarian failure—both premature and as a part of normal aging—the processes that drive it remain mysterious.
What we do know: At puberty, when the ovaries contain approximately 400,000 follicles, the brain begins to communicate with these organs and activates up to a thousand dormant follicles—fluid-filled sacs that house a developing egg—each month. Of these, a handful mature, producing hormones like estrogen and progesterone, which send signals to the brain to prepare the uterus for a possible pregnancy.
Most of the growing follicles wither and die; but each month one (and sometimes two or three) will fully mature and release an egg for potential fertilization. This process repeats every month until menopause, when fewer than a thousand follicles remain.
( Scientists are finally studying women’s bodies. This is what we’re learning. )
Years before menopause, however, the feedback mechanisms between the brain and the ovaries (and the follicles they contain) become chaotic as follicle numbers dwindle, Pepin explains. “But it’s a complete black box” as far as how this impacts the trajectory of ovarian aging or whether it differs in different people, he says.
If these feedback mechanisms are important, though, one way to preserve healthy ovarian function may be to hold onto the follicles you have.
Pepin demonstrated that anti-Müllerian hormone, which is made in the follicles and controls the number that are activated (and therefore eventually lost in a menstrual cycle), can do just that.
When mice exposed to chemotherapy (which seems to jumpstart the development of dormant follicles, increasing the pool of eggs that die in each cycle) were injected with the hormone, fewer follicles were activated and more […]
