Learn about brain health and nootropics to boost brain function
Scientists discover new immunosuppressive mechanism in brain cancer
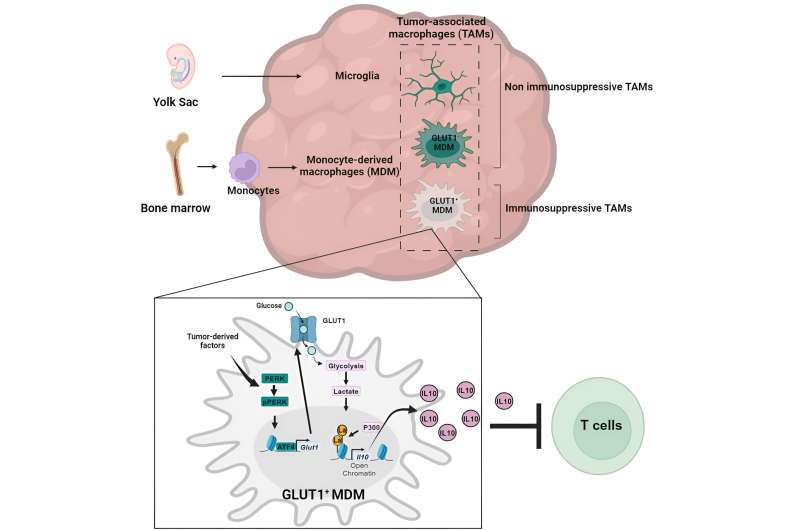
Graphical abstract. Credit: Immunity (2024). DOI: 10.1016/j.immuni.2024.04.006 The Wistar Institute assistant professor Filippo Veglia, Ph.D., and team, have discovered a key mechanism of how glioblastoma—a serious and often fatal brain cancer—suppresses the immune system so that the tumor can grow unimpeded by the body’s defenses.
The lab’s discovery was published in the paper, “Glucose-driven histone lactylation promotes the immunosuppressive activity of monocyte-derived macrophages in glioblastoma ,” in the journal Immunity .
“Our study shows that the cellular mechanisms of cancer’s self-preservation, when sufficiently understood, can be used against the disease very effectively,” said Dr. Veglia.
“I look forward to future research on metabolism-driven mechanisms of immunosuppression in glioblastoma, and I’m hopeful for all that we will continue to learn about how to best understand and fight this cancer.”
Until now, it has been poorly understood how monocyte-derived macrophages and microglia create an immunosuppressive tumor microenvironment in glioblastoma.
The Veglia lab investigated the cellular “how” of glioblastoma immunosuppression and identified that, as glioblastoma progressed, monocyte-derived macrophages came to outnumber microglia—which indicated that monocyte-derived macrophages’ eventuality to becoming the majority in the tumor microenvironment was advantageous to the cancer’s goal of evading immune response.
Indeed, monocyte-derived macrophages, but not microglia, blocked the activity of T cells ( immune cells that destroy tumor cells), in preclinical models and patients. The team confirmed this finding when they assessed preclinical models of glioblastoma with artificially reduced numbers of monocyte-derived macrophages.
And as the group expected, the models with fewer malicious macrophages in the tumor microenvironment showed improved outcomes relative to the standard glioblastoma models.
Glioblastoma accounts for slightly more than half of all malignancies that originate in the brain, and the prognosis for those diagnosed with the cancer is quite poor: Only 25% of patients who receive a glioblastoma diagnosis will survive beyond a year. Glioblastoma is inherently dangerous due to its location in the brain and its immunosuppressive tumor microenvironment, which renders glioblastoma resistant to promising immunotherapies.
By programming certain immune cells like macrophages, (such as monocyte-derived macrophages and microglia), to work for—rather than against—the tumor, glioblastoma fosters a tumor microenvironment for itself that enables the cancer to grow aggressively while evading anticancer immune responses. Wistar Insitute’s Dr. Filippo Veglia. Credit: The Wistar Institute Having confirmed the role of monocyte-derived macrophages, the Veglia lab then sought to understand just how the cancer-allied immune cells were working against the immune system.
They sequenced the macrophages in question to see whether the cells had any aberrant gene expression patterns that could point to which gene(s) could be playing a role in immunosuppression, and they also investigated the metabolic patterns of macrophages to see whether the macrophages’ nonstandard gene expression could be tied to metabolism.
The team’s twin gene expression & metabolic analysis led them to glucose metabolism . Through a series of tests, the Veglia lab was able to determine that monocyte-derived macrophages with enhanced glucose metabolism and expressing GLUT1, a major transporter for glucose (a key metabolic compound), blocked T cells’ function by releasing interleukin-10 (IL-10).
The team demonstrated that glioblastoma-perturbed glucose metabolism in these macrophages induced their immunosuppressive activity.
The team discovered the key to macrophages’ glucose-metabolism-driven immunosuppressive potency lies in a process called “histone lactylation.” Histones are structural proteins in the genome that play a key role in which genes—like IL-10—are expressed in which contexts.
As rapidly glucose-metabolizing cells, monocyte-derived macrophages produce lactate, a by-product of glucose metabolism. And histones can become “lactylated” (which is when lactate becomes incorporated into histones) in such a way that the histones’ organization further promotes the expression of IL-10—which is effectively produced by monocyte-derived macrophages to help cancer cells to grow.
But how can the glucose-driven immunosuppressive activity of monocyte-derived macrophages be stopped? Dr. Veglia and his research team identified a possible solution: PERK, an enzyme they had identified as regulating glucose metabolism and GLUT1 expression in macrophages.
In preclinical models of glioblastoma, targeting PERK impaired histone lactylation and immunosuppressive activity of macrophages, and in combination with immunotherapy blocked glioblastoma progression and induced long-lasting immunity that protected the brain from tumor re-growth—a sign that targeting PERK-histone lactylation axis may be a viable strategy for fighting this deadly brain cancer.
Provided by The Wistar Institute
Read more at medicalxpress.com