Nature Knows and Psionic Success
God provides
Brain Implant Translates Thoughts Into Words Faster Than Ever

A new technology that is able to translate our brain signals into speech has been developed by a team of neuroscientists, neurosurgeons and engineers at Duke University in North Carolina.
The device—known as a speech prosthetic—is significantly faster than the best speech-decoding technologies available today. It offers hope to patients who have lost their ability to speak.
“This technology would help patients suffering from debilitating neurological disorders such as ALS [amyotrophic lateral sclerosis] and locked-in-syndrome, who have lost the ability to speak and communicate,” Gregory Cogan told Newsweek. He is a professor of neurology at Duke University and one of the lead researchers on this project. “The current tools available to allow them to communicate are generally very slow and cumbersome.” Brain decoder For this project, Cogan teamed up with fellow Duke researcher Jonathan Viventi. He runs a biomedical engineering lab that specializes in creating high-density, ultra-thin and flexible brain sensors. For this project, the team packed 256 microscopic brain sensors onto a piece of flexible, medical-grade plastic the size of a postage stamp.
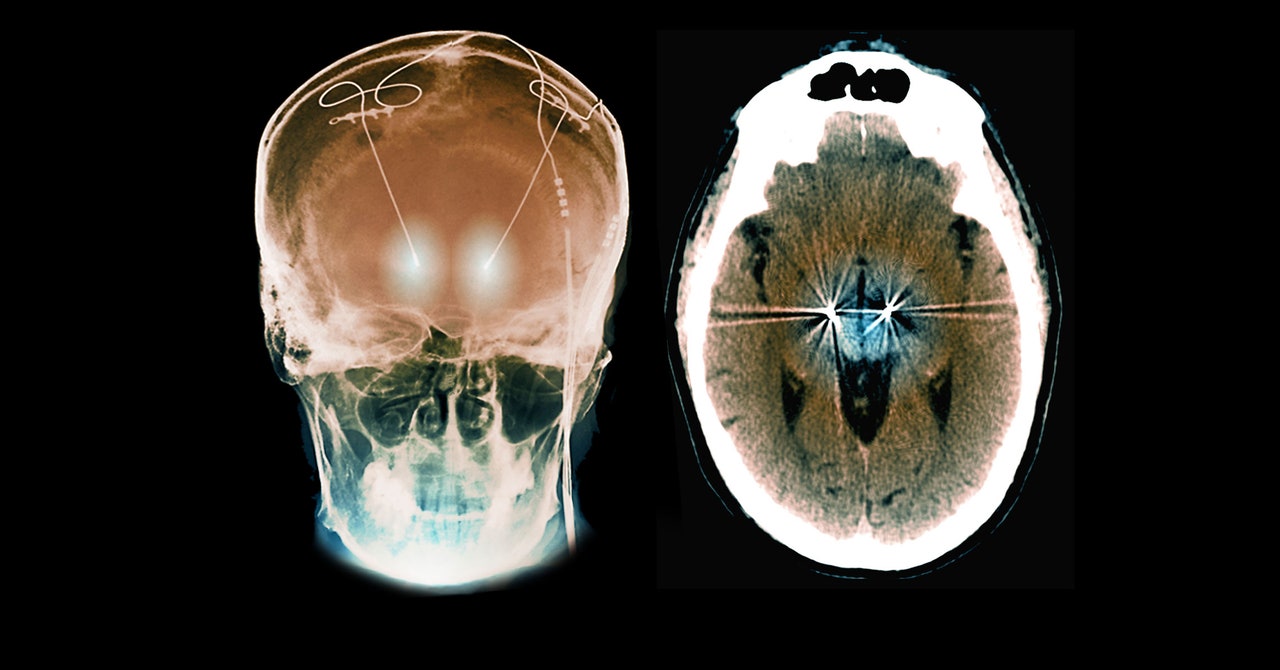
“Neural speech prostheses work by directly reading the brain signals that control speech motor movement, and then translate these signals directly into readable outputs that can be used to create speech sounds,” Cogan said. “They read your intentions to speak and translate this intention to sound. “These devices would be fitted through a small craniotomy in the skull and implanted directly onto the motor cortex of the brain. We are currently working on a project that will allow for one of these devices to work wirelessly, so that patients could move around freely while using it,” Cogan added.
To test the implant, the team recruited four patients who were already undergoing brain surgery for other conditions. The experiment was fast-paced and involved the team placing the device temporarily in the patients’ brains and asking them to repeat a series of simple words out loud.
“I like to compare it to a NASCAR pit crew,” Cogan said. “We don’t want to add any extra time to the operating procedure, so we had to be in and out within 15 minutes. As soon as the surgeon and the medical team said ‘Go!’, we rushed into action and the patient performed the task.”
Afterwards, Suseendrakumar Duraivel, a biomedical engineering graduate student at Duke, fed this data into a machine learning algorithm to see how accurately it could predict the sounds that were being made based solely on the patients’ recorded brain activity. The results were published in the journal Nature Communications on November 6.
Sign up for Newsweek’s daily headlines
“We were surprised at how good the results were,” Cogan said. “[This] technology demonstrates a very large improvement over current technology: we achieved 57 times higher spatial resolution and 48 percent higher neural signal strength compared to standard recordings. This increased signal quality improved our ability to read speech brain signals by 35 percent compared to standard tools.
“We expected results that were better than previous methods, but it is very promising to see the results pan out and it really opens the door for better neural speech prostheses in the near future,” Cogan added.
Overall, the decoder was accurate 40 percent of the time. The team members hope to resolve their technology further, while also developing a wireless version of the device to allow patients to move around without restrictions.
“We’re at the point where it’s still much slower than natural speech,” Viventi told Duke Magazine . “But you can see the trajectory where you might be able to get there.”
“The next steps are to get FDA [Food and Drug Administration] approval for our devices, so that we can put them in patients long-term to enable the restoration of their speech and communicative abilities,” Cogan said.
Request Reprint & Licensing Submit Correction View Editorial Guidelines
The Secret Behind Passing Out: New Brain-Heart Connection Identified

Researchers have identified the genetic pathway between the heart and brain responsible for fainting, revealing a two-way communication that could lead to new treatments for syncope-related disorders. Neurobiologists have discovered sensory neurons that regulate fainting, providing a foundation for targeted treatments for related disorders.
Syncope, commonly known as fainting, affects nearly 40 percent of people at least once in their lifetime. These transient losses of consciousness can be precipitated by various triggers such as pain, fear, heat, or hyperventilation, and they are a substantial cause of emergency room visits. Despite their prevalence, the fundamental mechanisms underlying syncope have largely remained enigmatic. Breakthrough in Genetic Pathways
Publishing a new report in Nature , University of California San Diego researchers, along with colleagues at The Scripps Research Institute and other institutions, have for the first time identified the genetic pathway between the heart and brain tied to fainting.
One of their unique approaches was to think of the heart as a sensory organ rather than the longstanding viewpoint that the brain sends out signals and the heart simply follows directions. School of Biological Sciences Assistant Professor Vineet Augustine, the paper’s senior author, applies a variety of approaches to better understand these neural connections between the heart and brain. An image of a heart labeled by vagal sensory neurons. In a new study published in the journal Nature , UC San Diego researchers and their colleagues found that these neurons trigger fainting, laying a foundation for addressing fainting-related disorders. Credit: Augustine Lab, UC San Diego
“What we are finding is that the heart also sends signals back to the brain, which can change brain function,” said Augustine. Information resulting from the study could be relevant to better understanding and treating various psychiatric and neurological disorders linked with brain-heart connections, the researchers note in their paper. “Our study is the first comprehensive demonstration of a genetically defined cardiac reflex, which faithfully recapitulates characteristics of human syncope at physiological, behavioral, and neural network levels.” Study on the Bezold-Jarisch Reflex
Augustine, along with Biological Sciences Staff Research Associate Jonathan Lovelace and Graduate Student Jingrui Ma, the first authors of the paper, and their colleagues studied neural mechanisms related to Bezold-Jarisch reflex (BJR), a cardiac reflex first described in 1867. For decades researchers have hypothesized that the BJR, which features reduced heart rate, blood pressure, and breathing, may be associated with fainting. But information lacked in proving the idea since the neural pathways involved in the reflex were not well known. Researchers at UC San Diego and collaborating institutions have highlighted the immense crosstalk between the heart and the nervous system. The video displays heart activity dramatically slowing down with stimulation of vagal sensory neurons, which were found to trigger fainting. Credit: Augustine Lab, UC San Diego
The researchers focused on the genetics behind a sensory cluster known as the nodose ganglia, which are part of the vagus nerves that carry signals between the brain and visceral organs, including the heart. Specifically, vagal sensory neurons, or VSNs, project signals to the brainstem and are thought to be associated with BJR and fainting. In their search for a novel neural pathway they discovered that VSNs expressing the neuropeptide Y receptor Y2 (known as NPY2R) are tightly linked to the well-known BJR responses. Optogenetic Studies and Findings
Studying this pathway in mice, the researchers were surprised to find that when they proactively triggered NPY2R VSNs using optogenetics, a method of stimulating and controlling neurons, mice that had been freely moving about immediately fainted. During these episodes, they recorded from thousands of neurons in the brains of the mice, as well as heart activity and changes in facial features including pupil diameter and whisking.
They also employed machine learning in several ways to analyze the data and pinpoint features of interest. Once NPY2R neurons were activated, they found, mice exhibited rapid pupil dilation and the classic “eye-roll” seen during human fainting, as well as suppressed heart rate, blood pressure, and breathing rate. They also measured reduced blood flow to the brain, an area of collaboration with Professor David Kleinfeld’s laboratory in the UC San Diego Departments of Neurobiology and Physics.
“We were blown away when we saw how their eyes rolled back around the same time as brain activity rapidly dropped,” the researchers reported in a paper summary. “Then, after a few seconds, brain activity and movement returned. This was our eureka moment.”
Further testing showed that when NPY2R VSNs were removed from mice, the BJR and fainting conditions vanished. Previous studies have shown that fainting is caused by a reduction in brain blood flow, which the new study also found to be true, but the new evidence indicated that brain activity itself could be playing an important role. The findings, therefore, implicate the activation of the newly genetically identified VSNs and their neural pathways not only with BJR, but more centrally in overall animal physiology, certain brain networks, and even behavior. Implications and Future Research
Such findings were difficult to tease out previously because neuroscientists study the brain and cardiologists study the heart, but many do so in isolation of the other. “Neuroscientists traditionally think the body just follows the brain, but now it is becoming very clear that the body sends signals to the brain and then the brain changes function,” said Augustine.
As a result of their findings, the researchers would like to continue tracking the precise conditions under which vagal sensory neurons are triggered into action.
“We also hope to more closely examine cerebral blood flow and neural pathways in the brain during the moment of syncope, to better understand this common but mysterious condition,” they note.
They also hope to use their research as a model to develop targeted treatments for fainting-associated conditions.
The study was funded by UC San Diego, Scripps Research Institute, the Helen Dorris Foundation, the National Institutes of Health, the American Heart Association Early Faculty Independence Award, the Mallinckrodt Foundation, the Dorris Scholarship, the Dorris-Skaggs Fellowship, and the Shurl and Kay Curci Foundation Fellowship.
DOUBLE TROUBLE: Studies show elevated stroke risk in patients who received flu and COVID-19 vaccines together

Advertisement
The Wuhan coronavirus (COVID-19) vaccine and the flu vaccine each come with their own set of potential side effects, but when these two risky jabs are administered together, the risks may be even higher. A growing body of evidence is now pointing to one very dangerous side effect in particular: stroke.
Researchers from Kaiser Permanente have found that there is a heightened risk of stroke for individuals under the age of 65 who receive a flu shot and the Pfizer COVID-19 vaccine on the same day. In the study, scientists identified 373 strokes in patients in the 42 days after receiving bivalent vaccination; after 42 days, 1511 strokes were reported.
Meanwhile, researchers from the Food and Drug Administration (FDA) have admitted to identifying an elevated risk of stroke for elderly individuals who receive the Pfizer or Moderna vaccines at the same time as the flu vaccine. The finding came from a self-controlled case series involving Medicare beneficiaries who received both vaccines.
They found that people aged 85 and older who received the Pfizer vaccine with their flu shot had higher risks of non-hemorrhagic stroke and transient ischemic attacks, while the elevated risk for those who received the Moderna jab was seen in those aged 65 to 74. Both types of strokes seen in the study are caused by blood clots that block the flow of blood to the brain.
All recipients aged 65 and older experienced a higher risk of non-hemorrhagic stroke 22 to 42 days after receiving a flu and Pfizer COVID vaccine combo; a higher risk of transient ischemic attack was seen in the first 21 days for those who received the flu vaccine and Moderna COVID-19 vaccine combination.
These results are being blamed largely on the high-dose flu vaccine that the patients who were studied received, which is formulated to rev up their immune system. Known as Fluzone, it contains quadruple the flu protection provided by a normal flu jab.
One high-ranking FDA official, Dr. Peter Marks, told a conference that he believes the flu, COVID-19 and RSV vaccines should be spaced out to reduce the risk of adverse events. He noted: “Oftentimes, we suggest if you want to minimize the chance of interactions and minimize confusing side effects from one with another, you wait about two weeks between the vaccines.”
Researchers in Australia have reached a similar conclusion. They note that more adults have reported experiencing negative side effects after getting a flu vaccine and Pfizer’s COVID-19 vaccine at the same time than those that are reported after receiving either of these vaccines on their own. COVID-19 vaccines can raise blood pressure
Although it is not fully clear how a vaccine raises the risk of stroke, studies have demonstrated an increase in blood pressure after getting a COVID-19 shot, which forces the heart to work harder than usual. This stress can damage the inner lining of blood vessels and cause arteries to narrow, which fosters the development of clots. Another risk of the vaccine is the potential to spur an abnormal immune response that results in severe inflammation that blocks the flow of blood to the brain.
On top of the risk of stroke, another concern is the possibility of one vaccine impacting the response of another. For example, one study showed that vaccines that are co-administered create lower levels of antibodies, which means recipients are not getting the full benefits.
It is worth noting that some studies have found that receiving the flu and COVID-19 vaccines simultaneously does not appear to raise stroke risk . However, researchers have acknowledged that more studies are needed to reach a more definitive conclusion about this connection and what may be causing it.
Sources for this article include:
TheEpochTimes.com
Brain health in those over age 50 deteriorated more rapidly during the pandemic, new research finds

Credit: Pixabay/CC0 Public Domain Brain health in people over age 50 deteriorated more rapidly during the pandemic, even if they didn’t have COVID-19, according to major new research linking the pandemic to sustained cognitive decline.
Researchers looked at results from computerized brain function tests from more than 3,000 participants of the online PROTECT study, who were aged between 50 and 90 and based in the UK. The remote study, led by teams at the University of Exeter and the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London, tested participants’ short-term memory and ability to complete complex tasks.
Through analyzing the results from this large data set, researchers found that cognitive decline quickened significantly in the first year of the pandemic , when they found a 50% change to the rate of decline across the study group . This figure was higher in those who already had mild cognitive decline before the pandemic, according to the research published in The Lancet Healthy Longevity .
This continued into the second year of the pandemic, suggesting an impact beyond the initial 12-month period of lockdowns. The researchers believe this sustained impact to be particularly relevant to ongoing public health and health policy .
The cognitive decline seems to have been exacerbated by a number of factors during the pandemic, including an increase in loneliness and depression, a decrease in exercise, and higher alcohol consumption. Previous research has found that physical activity , treating existing depression, getting back into the community, and reconnecting with people are all important ways to reduce dementia risk and maintain brain health.
Anne Corbett, Professor of Dementia Research and PROTECT Study Lead at the University of Exeter, said, “Our findings suggest that lockdowns and other restrictions we experienced during the pandemic have had a real lasting impact on brain health in people aged 50 or over, even after the lockdowns ended. This raises the important question of whether people are at a potentially higher risk of cognitive decline which can lead to dementia.
“It is now more important than ever to make sure we are supporting people with early cognitive decline , especially because there are things they can do to reduce their risk of dementia later on. So if you are concerned about your memory, the best thing to do is to make an appointment with your GP and get an assessment. Our findings also highlight the need for policymakers to consider the wider health impacts of restrictions like lockdowns when planning for a future pandemic response.”
Professor Dar Aarsland, Professor of Old Age Psychiatry at King’s IoPPN, added, “This study adds to the knowledge of the long-standing health-consequences of COVID-19, in particular for vulnerable people such as older people with mild memory problems. We know a great deal of the risks for further decline, and now can add COVID-19 to this list. On the positive note, there is evidence that lifestyle changes and improved health management can positively influence mental functioning. The current study underlines the importance of careful monitoring of people at risk during major events such as the pandemic.”
More information: Cognitive decline in older adults in the UK during and after the COVID-19 pandemic: a longitudinal analysis of PROTECT study data, The Lancet Healthy Longevity (2023).
Provided by University of Exeter
New Map Shows How Our Neurons Communicate
Summary: Researchers from Cleveland Clinic and OHSU have unveiled a pioneering technique for charting the intricate conversations occurring within our brains. Such insights are key to decoding behavioral alterations in neurological disease patients.
The innovative tool, CaMPARI, allows scientists to witness brain activity in real-time, marking active neurons red and inactive ones green. This breakthrough could offer pathways to better treatments and understanding of diseases like Alzheimer’s.
Key Facts:
> The study, using the CaMPARI system, can map real-time brain activity by highlighting active neurons in red and inactive ones in green.
This research is significant for understanding behavior and personality changes in Alzheimer’s disease and related disorders.
The team’s findings, recently published in Nature Communications, have the potential to shape the future of cognitive neuroscience, with the promise of improved treatment options.
Source: Cleveland Clinic
A research team led by Cleveland Clinic and Oregon Health and Science University (OHSU) has developed a new method for mapping how the parts of the brain “speak” to each other, critical to understanding behavior changes in patients with neurological disease.
Diseases like Alzheimer’s disease change how patients communicate and act, affecting their relationships and well-being. Cleveland Clinic’s Hod Dana, PhD, is collaborating with Jacob Raber, PhD, an OHSU behavioral neuroscientist, on mapping out the electrical paths that connect and coordinate the parts of the brain needed to complete different tasks. Decision-making, forming a memory or completing a task all involve brainwaves, signaling pathways that use cells called neurons. Credit: Neuroscience News “Effects on behavior and personality in Alzheimer’s disease and related disorders are caused by changes in brain function,” Dr. Dana says. “If we can understand exactly how the changes occur, we may figure out how to slow down the process or to stop it. Recording brain activity patterns that underlie behavioral changes is the first step to bridging the gap.”
Decision-making, forming a memory or completing a task all involve brainwaves, signaling pathways that use cells called neurons. To study how brainwaves influence behavior and decision making, researchers observe as neurons turn “on” and “off” across the organ in different situations.
Current technologies are unable to map the whole brain while still identifying the single cells. CaMPARI images can be captured during behavior, highlighting neurons that are active as red and inactive neurons as green.
After the test is completed, the red and green markers remain bright for several days. This allows researchers to capture a series of images to track the brain’s activity by mapping where the red appears within the brain.
The team recently published results in Nature Communications on using a calcium sensor system called CaMPARI (Calcium-modulated photoactivatable ratiometric integrator) to map brain activity in preclinical models while completing cognitive tasks. Drs. Dana and Raber plan to use CaMPARI in preclinical work to see how Alzheimer’s-related genes affect the way our neurons signal through our brains in learning and memory.
Drs. Dana and Raber say they hope to take what they learn from their results to develop tests and interventions that can improve the quality of life for patients, providing better treatment options.
“We now have the capability to study the relationship between brain activation and cognitive performance at an unprecedented level,” says Dr. Raber.
“These are the first steps in developing strategies to reverse those changes and improve cognitive performance in those affected by neurological conditions. The future of behavioral and cognitive neuroscience looks bright.”
Funding: This work was funded by NIH R21AG065914 and U01NS123658. About this neuroscience research news
Author: Alicia Reale
Source: Cleveland Clinic
Contact: Alicia Reale – Cleveland Clinic
Image: The image is credited to Neuroscience News
Original Research: Open access.
“ Large-scale recording of neuronal activity in freely-moving mice at cellular resolution ” by Hod Dana et al. Nature Communications
Abstract
Large-scale recording of neuronal activity in freely-moving mice at cellular resolution
Current methods for recording large-scale neuronal activity from behaving mice at single-cell resolution require either fixing the mouse head under a microscope or attachment of a recording device to the animal’s skull.
Both of these options significantly affect the animal behavior and hence also the recorded brain activity patterns.
Here, we introduce a different method to acquire snapshots of single-cell cortical activity maps from freely-moving mice using a calcium sensor called CaMPARI. CaMPARI has a unique property of irreversibly changing its color from green to red inside active neurons when illuminated with 400 nm light.We capitalize on this property to demonstrate cortex-wide activity recording without any head fixation, tethering, or attachment of a miniaturized device to the mouse’s head. Multiple cortical regions were recorded while the mouse was performing a battery of behavioral and cognitive tests.We identified task-dependent activity patterns across motor and somatosensory cortices, with significant differences across sub-regions of the motor cortex and correlations across several activity patterns and task parameters.This CaMPARI-based recording method expands the capabilities of recording neuronal activity from freely-moving and behaving mice under minimally-restrictive experimental conditions and provides large-scale volumetric data that are currently not accessible otherwise.Join our Newsletter I agree to have my personal information transferred to AWeber for Neuroscience Newsletter ( more information )Sign up to receive our recent neuroscience headlines and summaries sent to your email once a day, totally free.
Study: RUNNING boosts mental health and helps treat depression

Advertisement
For those experiencing anxiety and depression, lacing up their running shoes proves to be a better choice instead of taking drugs, according to a study.
The May 15 study published in the Journal of Affective Disorders found that running as therapy for anxiety and depression outperforms the effects of prescription antidepressants on mental and physical health and overall well-being – without negative side effects.
The study authors from the Netherlands gave 141 participants with anxiety and/or depression a real-life choice of treatments for their condition – medication or exercise – for a 16-week period. The medication group took escitalopram (an antidepressant that belongs to a group of medicines known as selective serotonin reuptake inhibitors or SSRIs that work by increasing the activity of “happy hormone” serotonin in the brain) and were told to adhere to their prescribed medication. Meanwhile, the exercise group aimed for two to three closely supervised 45-minute group sessions per week for 16 weeks.
At the end of the trial, researchers reported that around 44 percent of both groups showed an improvement in anxiety and depression. Significant improvements in blood pressure, heart function, weight and waist circumference were also reported in the running group. On the other hand, a tendency toward a slight deterioration in these metabolic markers was observed and reported in the antidepressant group. (Related: Exercise: The Miracle antidepressant drug? )
While the physical benefits of running as exercise have been well-established, there is plenty of scientific evidence suggesting that running can also improve your mental health and well-being. Here are some studies that support this belief. Running is a great stress reliever
Dr. David Linden, a professor of neuroscience at Johns Hopkins University School of Medicine, gives credit to a group of neurotransmitters called “endocannabinoids” – biochemical substances produced naturally by the body. These chemicals travel in and around the brain for the stress-reducing effects of a good run.
Endocannabinoids are produced in higher-than-normal concentrations during your runs and once they get into the brain, they exhibit the ability to reduce feelings of anxiety and encourage calm.
Unlike endorphins – biochemicals or hormones your body releases during pleasurable activities such as eating, exercise, massage and even sex – endocannabinoids can move easily through the cellular barrier separating the bloodstream from the brain, where these mood-improving neuromodulators promote short-term psychoactive effects, such as reduced anxiety and feelings of calm, Linden explained.
By making running a regular part of your healthy lifestyle routine, “you stand to earn more than just physical gains over time,” said Linden.
A study published in the journal Biochemical Pharmacology concluded that present findings point to the “endocannabinoid system as a pivotal neuromodulatory pathway relevant in the pathophysiology of mental disorders.” Running improves mood
A team of scientists at the University of Tsukuba in Japan completed a study published in the journal Scientific Reports , which provided evidence that a 10-minute single-bout of moderate-intensity running evokes a positive mood and increased executive function by enhancing arousal levels with activation in prefrontal subregions involved in mood regulation.
Researchers reported that running increased local blood flow to various parts of the prefrontal cortex – the gray matter of the anterior part of the frontal lobe that is highly developed in humans and plays a major role in the regulation of behavioral, cognitive and emotional functioning. Running promotes better sleep quality
Running also improves sleep quality , which can in turn boost your mental health. A study of 51 adolescents with a mean age of 18.3 years has found that 30 minutes of daily morning moderate-intensity running for three consecutive weeks improved sleep and psychological functioning in healthy adolescents, compared with control subjects. The study was published in the Journal of Adolescent Health . Running helps you better process your emotions
Running has been found as a perfect way to separate yourself from a situation for a little while. The key takeaway of a study involving 1.2 million Americans, published in The Lancet: Psychiatry , is that “if you run regularly, you probably experience better mental health days than not.”
Researchers found people who exercise regularly have 43.2 percent fewer days of “not good” mental health per month – characterized by heightened emotional stress –compared to those who don’t exercise regularly.
According to a study published online by JAMA Psychiatry , physical activity has an important and “potentially causal role” in reducing your risk for depression . Data suggests that if you replaced 15 minutes per day of sitting with 15 minutes of vigorous activity like running, you may be able to “outrun” depression. Running builds self-esteem
Researchers in a study published in the journal Neuropsychiatric Disease and Treatment has found that physical activities like running and jogging are directly related to better self-esteem as runners (or joggers) physically grow stronger and surer of themselves with each and every foot strike.
They added that running could provide a feeling of empowerment and freedom by knowing that your body, legs and mind are strong and capable, which can lead to improved perceptions of fitness and body image.
Visit BeatDepression.news for more similar stories.
Watch this video about how running is linked to improved mental health . This video is from the Daily Videos channel on Brighteon.com . More related stories:
Lifting weights could ward off dementia and make you smarter.
9 Herbs that can support mental health.
Brain food: Nutrient therapy can help address mental health issues.
Battle mental orders with these natural herbs.
Adapt to stress with these 5 adaptogenic herbs. Sources include: DailyMail.co.uk ScienceDirect.com 1 HopkinsMedicine.org ScienceDirect.com 2 Nature.com ScienceDirect.com 3 JAHOnline.org BrooksRunning.com TheLancet.com ScienceDaily.com Dovepress.com Brighteon.com
Nanowire ‘brain’ network learns and remembers ‘on the fly’
( Nanowerk News ) For the first time, a physical neural network has successfully been shown to learn and remember ‘on the fly’, in a way inspired by and similar to how the brain’s neurons work. The result opens a pathway for developing efficient and low-energy machine intelligence for more complex, real-world learning and memory tasks. Key Takeaways
The nanowire-based system can learn and remember ‘on the fly,’ processing dynamic, streaming data for complex learning and memory tasks.
This advancement overcomes the challenge of heavy memory and energy usage commonly associated with conventional machine learning models.
The technology achieved a 93.4% accuracy rate in image recognition tasks, using real-time data from the MNIST database of handwritten digits.
The findings promise a new direction for creating efficient, low-energy machine intelligence applications, such as real-time sensor data processing.
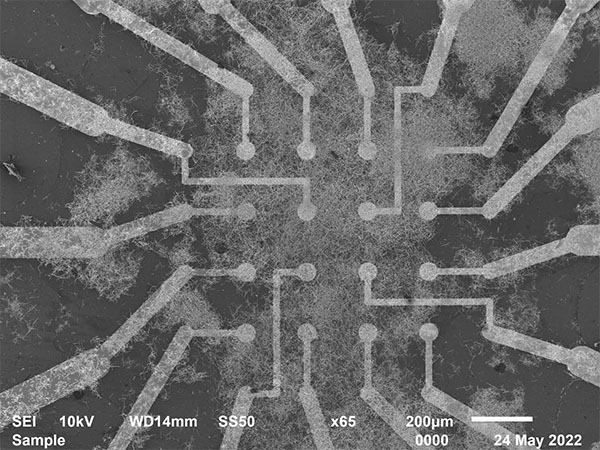
Electrodes interact with the nanowire neural network at the heart of the chip. (Image: University of Sydney) The Research
Published in Nature Communications ( “Online dynamical learning and sequence memory with neuromorphic nanowire networks” ), the research is a collaboration between scientists at the University of Sydney and University of California at Los Angeles. Lead author Ruomin Zhu, a PhD student from the University of Sydney Nano Institute and School of Physics, said: “The findings demonstrate how brain-inspired learning and memory functions using nanowire networks can be harnessed to process dynamic, streaming data.” Nanowire networks are made up of tiny wires that are just billionths of a metre in diameter. The wires arrange themselves into patterns reminiscent of the children’s game ‘Pick Up Sticks’, mimicking neural networks, like those in our brains. These networks can be used to perform specific information processing tasks. Memory and learning tasks are achieved using simple algorithms that respond to changes in electronic resistance at junctions where the nanowires overlap. Known as ‘resistive memory switching’, this function is created when electrical inputs encounter changes in conductivity, similar to what happens with synapses in our brain. In this study, researchers used the network to recognise and remember sequences of electrical pulses corresponding to images, inspired by the way the human brain processes information. Supervising researcher Professor Zdenka Kuncic said the memory task was similar to remembering a phone number. The network was also used to perform a benchmark image recognition task, accessing images in the MNIST database of handwritten digits, a collection of 70,000 small greyscale images used in machine learning. “Our previous research established the ability of nanowire networks to remember simple tasks. This work has extended these findings by showing tasks can be performed using dynamic data accessed online,” she said. “This is a significant step forward as achieving an online learning capability is challenging when dealing with large amounts of data that can be continuously changing. A standard approach would be to store data in memory and then train a machine learning model using that stored information. But this would chew up too much energy for widespread application. “Our novel approach allows the nanowire neural network to learn and remember ‘on the fly’, sample by sample, extracting data online, thus avoiding heavy memory and energy usage.” Mr Zhu said there were other advantages when processing information online. “If the data is being streamed continuously, such as it would be from a sensor for instance, machine learning that relied on artificial neural networks would need to have the ability to adapt in real-time, which they are currently not optimised for,” he said. In this study, the nanowire neural network displayed a benchmark machine learning capability, scoring 93.4 percent in correctly identifying test images. The memory task involved recalling sequences of up to eight digits. For both tasks, data was streamed into the network to demonstrate its capacity for online learning and to show how memory enhances that learning. Source: Universityy of Sydney (Note: Content may be edited for style and length) Nanowerk Newsletter
Get our daily Nanotechnology News to your inbox! Subscribe Loading… Thank you!
You have successfully joined our subscriber list.
Nanowire ‘brain’ network learns and remembers ‘on the fly’
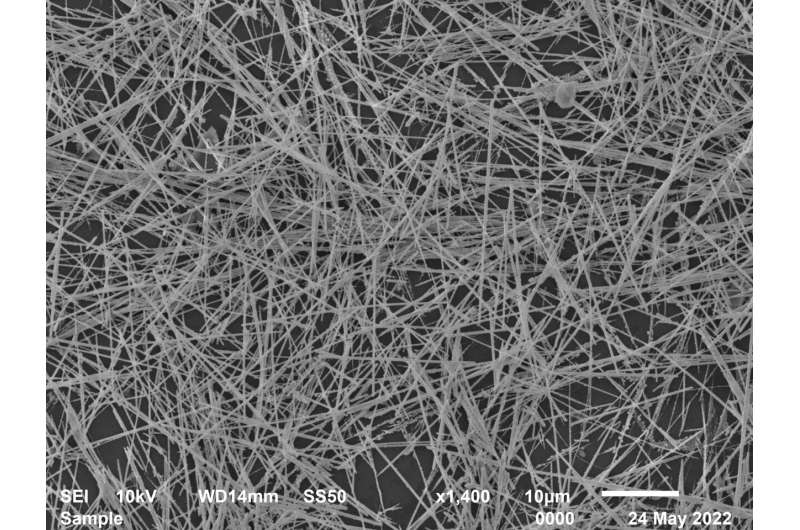
Electron microscope image of the nanowire neural network that arranges itself like ‘Pick Up Sticks’. The junctions where the nanowires overlap act in a way similar to how our brain’s synapses operate, responding to electric current. Credit: The University of Sydney For the first time, a physical neural network has successfully been shown to learn and remember “on the fly,” in a way inspired by and similar to how the brain’s neurons work.
The result opens a pathway for developing efficient and low-energy machine intelligence for more complex, real-world learning and memory tasks .
Published today in Nature Communications , the research is a collaboration between scientists at the University of Sydney and University of California at Los Angeles.
Lead author Ruomin Zhu, a Ph.D. student from the University of Sydney Nano Institute and School of Physics, said, “The findings demonstrate how brain-inspired learning and memory functions using nanowire networks can be harnessed to process dynamic, streaming data.”
Nanowire networks are made up of tiny wires that are just billionths of a meter in diameter. The wires arrange themselves into patterns reminiscent of the children’s game “Pick Up Sticks,” mimicking neural networks, like those in our brains. These networks can be used to perform specific information processing tasks.
Memory and learning tasks are achieved using simple algorithms that respond to changes in electronic resistance at junctions where the nanowires overlap. Known as “resistive memory switching,” this function is created when electrical inputs encounter changes in conductivity, similar to what happens with synapses in our brain. Detail of larger image above: nanowire neural network. Credit: The University of Sydney In this study, researchers used the network to recognize and remember sequences of electrical pulses corresponding to images, inspired by the way the human brain processes information.
Supervising researcher Professor Zdenka Kuncic said the memory task was similar to remembering a phone number. The network was also used to perform a benchmark image recognition task, accessing images in the MNIST database of handwritten digits, a collection of 70,000 small greyscale images used in machine learning .
“Our previous research established the ability of nanowire networks to remember simple tasks. This work has extended these findings by showing tasks can be performed using dynamic data accessed online,” she said.
“This is a significant step forward as achieving an online learning capability is challenging when dealing with large amounts of data that can be continuously changing. A standard approach would be to store data in memory and then train a machine learning model using that stored information. But this would chew up too much energy for widespread application.”
“Our novel approach allows the nanowire neural network to learn and remember ‘on the fly,” sample by sample, extracting data online, thus avoiding heavy memory and energy usage.” Electron microscope image of electrode interaction with the nanowire neural network. Credit: The University of Sydney Mr. Zhu said there were other advantages when processing information online.
“If the data is being streamed continuously, such as it would be from a sensor for instance, machine learning that relied on artificial neural networks would need to have the ability to adapt in real-time , which they are currently not optimized for,” he said.
In this study, the nanowire neural network displayed a benchmark machine learning capability, scoring 93.4 percent in correctly identifying test images. The memory task involved recalling sequences of up to eight digits. For both tasks, data was streamed into the network to demonstrate its capacity for online learning and to show how memory enhances that learning.
More information: Online dynamical learning and sequence memory with neuromorphic nanowire networks, Nature Communications (2023). DOI: 10.1038/s41467-023-42470-5
Personalized Deep Brain Stimulation Device May Offer Relief for Severe OCD

Some cases of OCD are notoriously difficult to treat. Responsive deep brain stimulation may help. Making sure a stovetop isn’t left on or readjusting an askew picture frame is often a natural response when something feels off. Yet, for over two million Americans living with obsessive-compulsive disorder (OCD), this nagging, unsettling feeling is a constant, debilitating presence marked by obsessions, persistent distressing thoughts, and compulsions, which result in repetitive behaviors people feel driven to perform.
Cognitive behavioral therapy and antidepressants can mellow out the obsessions and compulsions that people with OCD experience, but about one-third of those living with OCD don’t see improvement with either therapeutic treatment or medication. These cases are called treatment-resistant OCD, and for these people, there usually isn’t a whole lot that can be done outside of these standard (and unfortunately ineffective) remedies. But a new emerging treatment may provide some much-needed relief. Known as “deep brain stimulation,” this therapy delivers jolts of electricity to the brain in the hopes of fading those persistent, nagging thoughts into a distant memory.
In a study published earlier this month in the journal Neuron , researchers at the University of Pennsylvania used a type of brain stimulation called “responsive deep brain stimulation” to treat a 34-year-old woman with treatment-resistant OCD. Using a brain implant surgically placed to treat her epilepsy, the researchers taught the device to recognize a unique pattern of abnormal brain activity — a potential neural biomarker of OCD — and stimulate it any time it appeared. Within months, the woman’s severe obsessions and compulsions were significantly reduced. Two years after her first treatment, the researchers say her disorder no longer eats up hours of her day.
“This study is a proof-of-principle that we’re very close to finding a marker of OCD that seems to go up and down with effective deep brain stimulation,” Martijn Figee , director of the Mount Sinai Interventional Psychiatry Program, who was not involved in the study, tells Inverse . Resetting the brain
Since the mid-1980s, deep brain stimulation has been used to treat movement disorders like Parkinson’s disease or severe tremors and, in more recent years, Alzheimer’s disease , severe depression , binge eating , and now treatment-resistant OCD have also seen positive results.
About half of people with treatment-resistant OCD who try deep brain stimulation get much better, but the results aren’t consistent. Much of that has to do with the fact that we don’t fully understand how deep brain stimulation works. What scientists do know is that delivering a continuous electrical current through an electrode implanted in the brain helps reset and normalize communication between different areas involved in OCD. This incomplete understanding leads to challenges in fine-tuning deep brain stimulation in a way that’s effective for people dealing with treatment-resistant OCD. People with compulsive hand washing perform excessive and repetitive washing in an attempt to relieve severe distress associated with their fears of contamination. LittleCityLifestylePhotography/E+/Getty Images “We know that when we deliver a therapy continuously, the brain can sort of develop a tolerance to it, and that needs to be changed over time, complicating the therapy,” Casey Halpern , an associate professor of neurosurgery at the University of Pennsylvania who led the study, tells Inverse .
This is where the “responsive” piece of the deep brain stimulation puzzle fits in. Instead of sending electrical signals continuously, responsive deep brain stimulation only stimulates the brain when it picks up certain brain activity. Think of it like a smart thermostat that turns on the heat only when the temperature drops too low. This method of adjusting to the person’s brain activity has been tried before with certain types of epilepsy and depression , so scientists hoped people with treatment-resistant OCD would benefit as well. A smarter deep brain stimulator
For this new study, Halpern and his team worked with a 34-year-old woman with a history of OCD so severe she couldn’t eat around other people out of fear her own food would get contaminated (seafood was one major trigger). She would wash her hands so much to the point of bleeding, and she couldn’t leave her home or go to bed without checking all the doors and windows. The woman’s OCD took up eight hours of her day, and she was unable to live independently. And like other treatment-resistant OCD cases, therapy and medications didn’t seem to help at all.
In 2019, she had a neurostimulation device called a NeuroPace RNS System implanted on top of her skull with electrodes leading into her brain to manage her seizures. After getting the seizures under control, Halpern and his team set to work finding a particular brain signal they could train the implant to recognize. They recorded brain data as the woman went about her day-to-day tasks and in the lab as she interacted, in real life and in virtual reality, with objects meant to provoke her OCD.
Previous studies with deep brain stimulation and people with OCD found a low-frequency brainwave appearing in the basal ganglia — an area of the brain involved in coordinating movement, cognition, and emotion often targeted by stimulation therapies — whenever someone engaged with their obsessions or compulsions.
Halpern and his colleagues came across the same low-frequency electrical activity with the person they were treating for OCD. Specifically, they identified a brain circuit involving the nucleus accumbens, which is part of the basal ganglia associated with motivation and action, and the ventral pallidum, also located in the basal ganglia and is a central hub in the brain’s reward circuits. The researchers called these two regions the NAc-VeP circuit. The researchers recorded brain data while the woman interacted with objects, including those in virtual reality, meant to provoke her OCD. Casey Halpern / University of Pennsylvania After the first day of treatment targeting this circuit whenever it went haywire, Halpern says her patient saw marked improvement in several OCD tendencies, including her urge to check windows and doors at night.
After 24 weeks, according to the study, her patient with OCD reported a […]
A Personalized Brain Implant Curbed a Woman’s OCD
Amber Pearson has had a severe form of obsessive compulsive disorder since she was in high school. She would wash her hands so much they became raw and bled. Her bedtime routine easily took 45 minutes because it involved checking that all the doors and windows were closed and the stove was off. She was so afraid of food contamination that she couldn’t eat next to other people. Even on holidays, she ate on the couch away from her family. Therapy and medication didn’t help.
“Every decision I made was based on my OCD. It was always in the back of my mind,” Pearson says.
In her twenties, she developed epilepsy. After suffering a serious seizure that caused her to lose consciousness, her doctors considered treating her with deep brain stimulation, or DBS. The procedure involves surgically implanting a device that delivers electrical pulses to a specific brain region. Scientists think DBS works by resetting abnormal brain circuits, similar to what a pacemaker does for the heart.
DBS has been used for the past three decades to control tremors in people with Parkinson’s disease, and researchers are currently exploring it to restore upper body movement to stroke survivors and as a treatment for some psychiatric disorders . The US Food and Drug Administration permits its use for OCD as a last resort. Pearson wondered if the implant might help treat both of her conditions, so in 2019, she underwent an experimental brain surgery at Oregon Health & Science University.
In a study published this month in the journal Neuron , Pearson’s medical team reported that a single 32-millimeter-long electrode, tuned to detect her unique neural signals, was able to control both. Unlike traditional DBS, which provides constant stimulation, Pearson’s device is a “responsive” one; it only delivers jolts of electricity when it detects irregular patterns in her brain associated with the start of a seizure or compulsive thoughts.
Responsive DBS is already used for epilepsy, but Pearson’s medical team says it’s the first time it’s been used for OCD, as well as to simultaneously treat two conditions.
“This is pretty remarkable,” says Rachel Davis, an associate professor of psychiatry and neurosurgery at the University of Colorado School of Medicine, who researches DBS but was not involved in the new study.
Pearson’s seizures were occurring in a part of the brain called the insula, so her neurosurgeon, Ahmed Raslan, thought he could target a small region there for her epilepsy, plus the ventral striatum, which sits just above and behind the eyes. This contains the nucleus accumbens—an area associated with motivation and action, including compulsive urges. “It was an area that could be targeted with the same electrode,” Raslan says.
The team used a device made by a company called NeuroPace, based in Mountain View, California. Other electrodes used for deep brain stimulation only emit electrical pulses. This one also collects brain signals and delivers electricity only when it is programmed to detect a certain trigger.
First, the Oregon team used the device to get Pearson’s epilepsy under control. Next, Raslan sought out Casey Halpern, an associate professor of neurosurgery at Penn Medicine who is studying the nucleus accumbens as a DBS target for psychiatric conditions. To program the stimulation for Pearson’s OCD, Halpern and his team first needed to figure out what neural trigger they were looking for.
To do this, they needed to know which neural signatures in Pearson’s brain activity corresponded with her experience of obsessive thoughts. As she went about her ordinary life at home, Pearson would swipe a magnet over her head when she felt obsessive thoughts, and her implanted device would time-stamp the moment of each event.
Halpern and his colleagues also worked with Pearson in the lab, intentionally exposing her to items that triggered her OCD. For example, because one of Pearson’s triggers was seafood contamination, the team gave her seafood to handle while monitoring her brain activity as she became distressed.
By analyzing these brain recordings, Halpern was able to identify a unique neural signature in the ventral striatum that corresponded to times when Pearson felt she had to act on her compulsions. “We found that low-frequency oscillations would elevate in power during those moments,” Halpern says. This low-frequency signal was the same whether Pearson was experiencing a distressing situation in the lab or at home.
The researchers programmed her device to only deliver stimulation when it detects this type of brain activity—and only briefly. After a few seconds to a minute, it shuts off. The goal, Halpern says, is to restore normal function to abnormal neural circuits.
Over the next six to eight months, Pearson’s OCD symptoms decreased significantly, and her brain activity triggered the stimulation less often. She told her doctors that before, she was sometimes spending eight hours a day performing compulsions. Now, she estimates that it’s more like 30 minutes. The effects have persisted over the two years since the stimulation has been turned on. “It wasn’t instantaneous. It took a few months to notice changes,” she says. “I slowly started noticing things disappearing from my routine. Then, more things would disappear.”
Pearson doesn’t wash her hands as often, and now her knuckles don’t bleed. Her bedtime routine takes just 15 minutes. The best part, she says, is that her relationships with her friends and family are a lot better. She can enjoy a meal with them without feeling distressed.
“What this highlights is that OCD is a disorder of the brain, just like epilepsy and Parkinson’s,” Halpern says. “This isn’t a disorder of will. There’s a pathological signal that we’re seeing in the brain.”
Davis says she was initially skeptical of the idea that OCD could be treated with occasional bursts of stimulation. “Often people with OCD have a baseline level of dread or anxiety,” she says. For that reason, she assumed patients would need constant stimulation to keep their brain circuits regulated. Her center has implanted nine OCD patients with traditional DBS devices that provide steady stimulation. Although the Neuron report is just one case study, she thinks it’s impressive that Pearson’s symptoms […]
Study finds LAUGHTER THERAPY offers benefits for people with coronary artery disease

Advertisement
Laughter has many proven benefits, especially for your lungs, heart, immune system and mental health. According to a new study by researchers in Brazil, laughter provides substantial benefits to people with heart disease as it could significantly boost their cardiovascular function .
The study’s remarkable findings were presented at the annual meeting of the European Society of Cardiology – the world’s largest heart conference – in Amsterdam last August. What laughter can do for your heart
Having a sense of humor is good for your heart. When you laugh, you don’t just increase your oxygen intake, which is great for your lungs, you also provide exercise for your heart. And people whose hearts are weakened by heart disease can greatly benefit from this cardio exercise. (Related: Walking 8,000 brisk steps once or twice a week found to boost heart health .)
Marco Saffi, a professor from the Hospital de Clínicas de Porto Alegre in Brazil who led the study, told the Guardian : “Our study found that laughter therapy increased the functional capacity of the cardiovascular system. Laughter therapy could be implemented in institutions and health systems like the NHS [National Health System of the UK] for patients at risk of heart problems.”
Saffi and his team conducted their study to find out if laughter therapy, a non-invasive, non-pharmacologic and easily implementable intervention , can improve cardiovascular health and reduce common symptoms of heart disease, which include a reduced ability of the heart to pump oxygen throughout the body and an impaired capacity of the arteries to expand.
The Brazilian researchers recruited 26 adults with an average age of 64 for their 12-week experiment. All the participants have been diagnosed with coronary artery disease (CAD), a condition caused by the accumulation of plague in the arteries that supply blood to the heart.
The researchers divided the participants into two groups, one of which was tasked to watch comedy programs every week for three months while the other watched serious documentaries about Nature or politics.
The study found that the participants who were assigned to watch comedy programs showed improvement in their cardiovascular function, as evidenced by a 10 percent increase in the amount of oxygen their hearts were able to pump into their bodies. Their arteries’ ability to dilate also improved after 12 weeks of laughter therapy.
Before and after the experiment, the researchers took blood samples from the participants to check their levels of inflammatory biomarkers and how much plaque is deposited in their arteries. Comparison of blood analysis results showed that those who received laughter therapy had greatly reduced inflammatory biomarkers at the end of the study, which meant that their risks of heart attack and stroke also went down .
“When patients with coronary artery disease arrive at [a] hospital, they have a lot of inflammatory biomarkers. Inflammation is a huge part of the process of atherosclerosis when plaque builds up in the arteries,” Saffi explained.
“This study found that laughter therapy is a good intervention that could help reduce that inflammation and decrease the risk of heart attack and stroke.” (Related: Do these exercises in the morning to boost your heart function and reduce your risk of heart disease and stroke .)
Saffi and his team believes that the cardiovascular improvements brought about by laughter therapy may have something to do with the increase in endorphins released by the brain. Endorphins are the “feel-good” chemicals released during pleasurable activities , such as exercise, eating and having sex. These happy hormones also help lower blood pressure and decrease the strain on your heart by reducing the levels of stress hormones like cortisol.
Because of their promising findings, Saffi and his team are optimistic about the prospect of laughter therapy becoming a widely implemented intervention for heart disease in the future. Saffi thinks it could also help reduce the dependence of heart disease patients on pharmaceutical medications, which cause unfavorable side effects. But more and larger studies are needed to validate their findings.
Laughter therapy is not just limited to TV programs. You can enjoy the benefits of laughter by hanging out with your friends and doing fun activities with your family and loved ones. Saffi recommends doing things that can make you laugh at least twice a week for best results. Other health benefits of laughter
A good laugh can provide plenty of short-term health benefits . For instance, laughing can stimulate your lungs, heart and muscles, and helps cool down your stress response. It can also increase then decrease your heart rate and blood pressure, leaving you with a pleasant, relaxed feeling afterward.
Laughing also helps relax the muscles of your body and promotes good blood circulation. In fact, a hearty laugh can leave your muscles relaxed for a good 45 minutes after . Thanks to these effects, laughter is the best natural medicine for stress and can help reduce some of its physical symptoms.
Frequent laughter also offers some amazing long-term benefits. According to psychiatrist Dr. William Fry, a professor at Stanford University , “mirthful laughter” markedly enhances your body’s resistance to illness . Research shows that people who laugh often tend to release more T cells from the spleen into the bloodstream. T cells are a type of immune cells whose functions include activating other immune cells, killing infected cells and regulating your immune response.
Laughter also promotes a positive mood via the release of more endorphins, which can help fight stress, anxiety and depression. This has the added benefit of improving your self-esteem and increasing your pain tolerance. (Related: Not all pain should be treated with NSAIDs .)
A study by Swiss researchers found that people who are laughing are able to keep their hands submerged in ice water longer than people who are not. This increased tolerance to pain remained 20 minutes after the participants had stopped laughing. The researchers attributed this effect to the release of endorphins and the reduction in muscular tension. This finding shows that laughter therapy could also help people who are suffering from chronic pain.
Laughter is one of the best […]
Neuroscientists are Tantalizingly Close to Mastering How Psychedelics Redesign Our Brains
The first-line pharmacological treatment for major depressive disorder (MDD) is antidepressant drugs known as selective serotonin reuptake inhibitors (SSRIs). However, a significant proportion of people don’t respond to these drugs.
Given that major depression is a global mental health problem that is on the r ise, it is important to find novel pharmacological treatments for those who do not respond to the current ones. But to do that, we need to understand exactly how the drugs work – which we currently don’t.
MDD is a debilitating and distressing mental health disorder, trapping sufferers in a rigid and negative state of mind. There’s even evidence suggesting that this lack of flexibility is associated with cognitive changes , including negative thoughts and biases and problems with learning and memory.
In our new study, published in Molecular Psychiatry , we show that an SSRI called ecitalopram may actually make brains more “plastic” — meaning more flexible and adaptive, more able to facilitate communication between neurons (brain cells). Brain plasticity is simply the ability of neural circuits to change through growth and reorganization. Learning involves brain plasticity, including changes in neural circuits, and can help people to recover from depression.
One novel treatment option for depression, approved by the US Food and Drug Administration, is intranasal esketamine (an anesthetic made from ketamine), although it has not as yet been approved for use by the NHS. The psychedelic drugs LSD and psilocybin are also being investigated for treatment-resistant depression in research studies but are not yet approved by regulatory bodies. When these studies are conducted, there is careful monitoring by a medical professional to ensure participant safety.
We know that both SSRIs and psychedelics target the same brain receptor (known as the 5HT-2A). By contrast, eskatamine, similar to ketamine, works on a different receptor (N-methyl-D-aspartate or NMDA) and affects the brain’s chemical glutamate.
So, how do SSRIs and psychedelics work to reduce symptoms of depression? At present, we don’t have the full picture. However, the 5HT-2A receptor is linked to the brain chemical serotonin, increasing levels of it in the brain. And a recent study has indeed shown that serotonin appears to be reduced in people with depression.
SSRIs, however, also affect the neurotransmitters GABA and glutamate. The latter has been linked to learning, cognition, and memory – suggesting SSRI may actually help to restore cognitive function . Although the exact mechanisms of psychedelics are not yet fully understood, their antidepressant effects seem to work in a similar way to SSRIs, given their effects on 5HT-2A receptors. However, there are also other reactions to psychedelics, such as hallucinations. Measuring brain plasticity
All these drugs have, therefore, been suggested to affect brain plasticity. However, in humans, it can be difficult to estimate levels of brain plasticity. One common method that scientists have used is to measure a protein called the brain-derived neurotrophic factor (BDNF) in blood samples.
BDNF helps brain plasticity by increasing the number of synapses (locations where neurons can communicate with each other), as well as the branches and growth of developing neurons. Synapses are particularly important in brain functioning as they allow the transmission of chemical and electrical signals from one neuron to another. Similarly, synapses also store brain chemicals for release.
There have been some studies showing that antidepressant drugs increase BDNF. However, better techniques are required to study plasticity in the human brain.
One approach to developing better drugs is to find antidepressant drugs with a faster mechanism of action. According to the NHS website, SSRIs usually need to be taken for two to four weeks before any benefit is felt.
We suspected that one reason for this delayed effect may be that brain plasticity needs to occur with SSRI treatment. As this process involves rewiring, such as the creation of synapses and circuits, it isn’t instant but is thought to take approximately 14-21 days.
In our study, which was a collaboration between the University of Cambridge and the University of Copenhagen, we used a novel technique to measure plasticity in the human brain following SSRI treatment for the first time.
Thirty-two participants underwent positron emission tomography (PET) scanning to detect the amount of a protein called “synaptic vesicle glycoprotein 2A”, or SV2A, in the brain. We know that SV2A is a marker of the presence of synapses. An increased amount would suggest that more synapses are present and, therefore, that brain plasticity is higher.
Our results showed a rise in this protein as a result of taking escitalopram (an SSRI). We found that, in those taking escitalopram, increased SV2A was associated with increased duration of the drug. Our findings suggest that brain plasticity increases over three to five weeks in healthy humans following daily intake of escitalopram.
This is the first real evidence in humans that SSRIs really do boost neuroplasticity – seen in the brain – and that this is one of the reasons it can treat depression. Similar evidence from studies in the human brain is still required for psychedelics.
It makes sense that if antidepressant treatment facilitates brain plasticity, this should make it easier for people taking these treatments to learn new things. We know that the ability to adopt new strategies and change them if they don’t work (supported by what researchers call cognitive flexibility) is key to recovering from depression .
This article was originally published on The Conversation by Barbara Jacquelyn Sahakian and Christelle Langley at the University of Cambridge. Read the original article here .
11 foods for improved brain function and health

timolina, AdobeStock Baked salmon garnished with asparagus and tomatoes with herbs. Fish and vegetables are among foods that promote brain health. Our happy hormone serotonin, is overwhelmingly produced — 95% — in our gastrointestinal tracts, according to Simply Neuroscience . Since digestion happens at a chemical level, what’s really in our food matters a ton. Knowing why certain foods are more beneficial than others can help us to be more intentional with what ends up on our dinner plates. Here are 11 foods that increase the health and function of the brain — and why. 1. Fatty fish
Important nutrients: Omega-3 fatty acids.
Benefits: Eating fatty fish is proven to slow mental degeneration and stabilize mood swings, per Senior Lifestyle . Alzheimer’s Research UK published a study that showed a correlation between healthier brain structures in middle-aged people and consumption of omega-3 foods. 2. Blueberries
Important nutrients: Anthocyanin.
Benefits: Dietitian Joyce Prescott told Cleveland Clinic , “Research shows that flavonoids are also powerful nutrients and may help explain why plant-based diets are consistently associated with health benefits. We think this is due, in part, to their antioxidant properties.” Anthocyanins are also found in strawberries, raspberries, purple vegetables and raspberries. 3. Eggs
Important nutrients: Choline, lutein and tryptophan.
Benefits: Though eggs have gotten a bad rap over the years due to their relatively high cholesterol levels, they also contain nutrients that promote brain development and can improve memory and motor function.
The Journal of Nutritional Science published a study in 2021, explaining that higher levels of choline in adults was correlated with “improved performance on tasks of processing speed, working memory, memory and visuomotor skill.”
Related 5 superfoods to boost brain health and memory
4. Dark chocolate
Important nutrients: Flavonoids
Benefits: Dr. Tian-Shin Yeh told Harvard Health , “Some studies have suggested flavonoids may offer protective effects for brain cells.” Several animal studies showed flavonol’s ability to decrease plaque growth and increase blood flow in the brain.
“Some studies found flavonoid intake is inversely related to cardiovascular disease, and what is good for the cardiovascular system is also good for the brain,” said Yeh. 5. Oranges
Important nutrients: Flavanoids and vitamin C.
Benefits: Longevity Technology reported on several benefits vitamin C has on the brain, saying it “plays a role in the synthesis of myelin, a fatty substance that accelerates the transmission of electrical signals in the brain,” which increases brain efficiency. They also reported on research that vitamin C may play a role in neuron development. 6. Spinach and green leafy vegetables
Important nutrients: B vitamin folate.
Benefits: B vitamin folate reduces homocysteine levels, according to Taste of Home . Homocysteine is an amino acid that leads to blood clotting and is toxic to neurons. Foods that are high in B vitamin folate include broccoli, Brussels sprouts, kale, peas and kidney beans, according to the NHS . 7. Walnuts
Important nutrients: Omega-3 fatty acid (alpha-linolenic acid).
Benefits: ALA and omega-3 fatty acids are beneficial to the brain and the heart and have been linked to “lower blood pressure and cleaner arteries,” per Harvard Health . Harvard’s article also referenced a study done by UCLA linking walnuts to “improved cognitive test scores.” 8. Bone broth
Important nutrients: Amino acid glycine.
Benefits: Glycine fosters improved memory, reduced stress and better mental awareness, per Owl Venice . Glycine is a “neurotransmitter that has the ability to stimulate or quiet the brain,” and helps the consumer have more control staying alert while awake and calm while asleep. 9. Turmeric
Important nutrients: Turmerone.
Benefits: Alzheimers.org explained that turmerone stimulates the brain to create new cells, which could help with diseases like Alzheimer’s, where the brain faces deterioration. In mice studies, turmerone’s component curcumin seemed to be correlated with reduced oxidative stress and inflammation. 10. Coconut oil
Important nutrients: Medium-chain fatty acid.
Benefits: This fatty acid “creates ketone bodies, which act as an energy source in the brain and may benefit people who have or are developing impaired memory,” per Medical News Today . Coconut oil is great for brain health and has been known “to help with several brain disorders such as Alzheimer’s and epilepsy,” Neurotrition added. 11. Whole grains
Important nutrients: Complex carbohydrates. Benefits: High sugar intake is correlated to brain decline, per Cleveland Clinic . Memory and brain health specialist Babak Tousi explained, “As soon as you eat white bread, it breaks down quickly into sugar.”“Whole-grain bread does not.” He continued, “Try to avoid foods that release sugar very quickly into your body. Complex carbohydrates like whole grains are broken down more slowly, so sugar is released gradually, allowing your body to function more efficiently.”
Study finds INSUFFICIENT SLEEP negatively impacts cardiovascular health
Having a poor night’s sleep can not only affect your mood the next day, it can also negatively impact your cardiovascular system .
This was the finding of a study published in Scientific Reports. “Sleep restriction is associated with increased cardiovascular risk,” the study authors wrote, noting that “more than a third of U.S. adults sleep less than recommended seven to eight hours per night.
According to the researchers, female study participants who had a bad night’s sleep had abundant amounts of free radicals in the cells lining the inside of their blood vessels. Compared to participants who had sufficient sleep, the sleep-deprived subjects could not activate the necessary antioxidant response to clear out these free radicals. This is because insufficient sleep reduces the expression of a protein called DCUN1D3, which normally mediates antioxidant responses in the body. Why is getting enough sleep important?
There are two dimensions to sleep – quantity , which is how much sleep you get each night, and quality , which is the depth of your sleep experience, which is when you fall asleep quite easily, do not fully wake up during the night, do not wake up too early and feel refreshed and re-energized in the morning.
The American Heart Association recognizes lack of age-related adequate quality sleep as a risk factor for adverse cardiometabolic profiles and poor outcomes.
Numerous studies have shown substantial evidence that demonstrates how sleeping problems spark cardiovascular chaos , including chest pain (angina), high blood pressure (hypertension), high cholesterol, heart attack, heart failure, heart palpitations, stroke, unexplained chest pain, diabetes, obesity and more. Sleep and blood pressure
Your blood pressure drops during healthy, normal sleep and this is referred to as “nocturnal dipping.”
Research published in the World Journal of Cardiology indicated that a dip of 10 to 20 percent is considered normal .
“Blunted or absent dips” of less than 10 percent have been considered an adverse cardiovascular event. Those in excess of 20 percent are known as “exaggerated or extreme dipping.”
A study published in the journal Hypertension Research indicated that extreme dippers have a higher occurrence of deep white matter lesions, silent cerebral infarctions or stroke and silent myocardial ischemia or heart attack during sleep than normal dippers.
During extreme dipping, nocturnal hypoperfusion (shock) at the brain or heart may occur and lead to organ damage.
This is particularly of concern in older hypertensive patients with impaired cerebral auto-regulation, or the ability to maintain stable blood flow despite changes in blood pressure. Sleep and coronary heart disease
A short sleep duration of less than six hours can likely cause non-fatal cardiovascular events (e.g., angina pectoris or chest pain), myocardial infarction (e.g., a silent heart attack) or sudden cardiac death, as shown in a study published in the Korean Journal of Physiology & Pharmacology . Sleep and obesity
If you’re not getting enough quality sleep, your brain decreases leptin , which tells your brain when you’ve had enough to eat, and increases the production of ghrelin , which stimulates your appetite – leading you to overeat and gain weight.
Being overweight or obese is strongly associated with numerous cardiovascular and cardio-metabolic problems. Sleep and hormonal imbalances
Sleep deprivation or lack of sleep can cause hormonal imbalance and the imbalance of hormones can lead to more sleep deprivation – a vicious cycle . These imbalances can have widespread effects on your body.
For example, with menopause, your estrogen levels drop this decrease in estrogen may cause women to experience troublesome hot flashes, mood changes, night sweats and/or vaginal dryness – which then leads to disrupted sleep events.
Sleep deprivation (when sleep disruption is severe) contributes to elevated levels of the stress hormone cortisol and the connection goes both ways.
High cortisol levels in the evening can cause you to lack sleep hours and may also lead to sleep disorders, such as chronic insomnia and obstructive sleep apnea, in which your breathing stops and restarts many times while you sleep.
A sleep doctor explains that cortisol is not the enemy of your sleep because a healthy cortisol rhythm helps to keep your circadian or sleep cycle in check. This means you want higher cortisol levels in the morning to help you wake up and lower levels in the evening to help you fall asleep easily.
Chronic stress is not good news for your sleep because you will have high levels of cortisol at all times and sleep loss can hike your cortisol levels – trapping you in a vicious cycle of more sleep deprivation and more cortisol. (Related: Improve sleep quality to bolster your resilience against anxiety and depression .) Sleep, cortisol and insulin sensitivity
Aside from the hormone cortisol, insulin is an essential hormone that helps your body turn the food you consume into energy and controls your blood sugar.
Cortisol prepares your body for the burst of energy it needs for both “fight and flight” by increasing your blood sugar as an energy source.
During a cortisol-inducing stressful event (as mentioned earlier), you are able to access quick energy but the stress hormone would slow down insulin production so blood sugar won’t be stored so it can’t be used immediately and won’t be able to work as efficiently.
Sleep deprivation also contributes to elevated cortisol levels and if it remains high for an extended period of time, your body can remain in an insulin-resistant state.Over time, you’ll be more susceptible to chronic fatigue, weight gain and diabetes – in addition to other health problems. Keep your heart healthy by developing good sleep hygiene habits Sleep hygiene is a catchall term for habits and behaviors that can influence (or negatively impact) sleep – all the steps you take and daytime behaviors you engage in to help get a good night’s sleep.When your circadian rhythm and your sleep drive line up, your body is ready to sleep.Sleep drive tells you “you need to sleep” based on a build-up of adenosine (a byproduct of cellular metabolism) in the brain. The more active and alert […]
Study: Popular sugar substitute erythritol linked to CARDIOVASCULAR ISSUES

Advertisement
Erythritol is often used as a substitute for regular table sugar. However, a study has found that it can cause serious health issues .
The study published in Nature Medicine stated that erythritol is linked to various cardiovascular issues. “Sweeteners, like erythritol, have rapidly increased in popularity in recent years, but there needs to be more in-depth research into their long-term effects ,” said corresponding author Dr. Stanley Hazen, chairman for the Department of Cardiovascular and Metabolic Sciences at the Cleveland Clinic’s Lerner Research Institute.
Researchers from the Cleveland Clinic studied over 4,000 people in Europe and the United States to “look for new pathways that contribute to cardiac disease risk.”
Different compounds in patients’ blood samples were measured to see whether or not they predicted the future risk of heart attack, stroke or death.
Once the compounds’ structure was examined, erythritol was found to be at the very top of the list. Researchers noted that people with high blood levels of erythritol had an elevated risk for heart attack or stroke.
The researchers proceeded to conduct mechanistic studies by giving erythritol to animals and found that they developed thrombotic events like a heart attack or a stroke. There’s a clot in the vessel that feeds the heart or the brain. They also found that adding erythritol to blood increases the likelihood of clotting.
Blood clotting normally occurs when there’s damage to a blood vessel. Platelets immediately adhere to the cut edges of the blood vessel and release chemicals to attract even more platelets. One of the biggest problems that cardiologists face in cardiovascular disease is abnormal clotting.
If the clotting becomes obstructive to the heart , doctors call it a heart attack or if it’s an obstruction in the blood vessels that go into the brain, doctors call it a stroke. The authors noted the importance of follow-up studies to confirm their findings in the general population because their clinical observation studies “demonstrated association and not causation.”
Erythritol is a sugar alcohol that is about 70 percent as sweet as sugar and is found naturally in some fruits , like grapes, peaches, pears and watermelon. It is also found in some mushrooms. (Related: What is the difference between stevia, Truvia and PureVia ?)
The sugar alcohol erythritol can be produced commercially by food scientists via fermentation by yeast or produced inside yeast-like fungi via the pentose phosphate pathway (PPP), according to a study from Nutrients . That said, erythritol is also found in fermented foods, like beer, cheese, sake, soy sauce and wine. Limitations of the study
The study was primarily done with those who have cardiac risks, cardiovascular problems, those who have been treated, as well as those who have diabetes.
In untargeted metabolomics studies (large-scale studies of small molecules or metabolites within cells, biofluids, tissues or organisms), circulating levels of multiple polyol sweeteners, especially erythritol, were associated with a three-year incident risk for major adverse cardiovascular events (MACE), which may include nonfatal myocardial infarction or stroke or even death.
The researchers also found that erythritol may make it easier for blood clots to form but some health experts pointed out that the data only came from studies done in mice and a small cohort of eight healthy humans.
In the Cleveland Clinic study, 30 grams was enough to make blood levels of erythritol go up a thousandfold and it remained elevated above the threshold – necessary to trigger heightened clotting risk for the following two to three days.
These weren’t the only concerns health experts and specialists had about the study.
“The association between blood erythritol levels and heart disease risk may be due to participants incorporating more sugar substitutes in their diets to lower their health risks and without a comprehensive examination of dietary patterns – both before and after disease development – it is difficult to know whether there is some reverse causation,” explained dietitian Dr Maya Vadivello, an associate professor in nutrition and food sciences at the University of Rhode Island who was not affiliated with the study.
Head over to Sweeteners.news for more stories about erythritol and other sugar substitutes.
Watch Tim Pool of “Timcast” discussing an article by People magazine about erythritol causing blood clots and heart attacks below. People Magazine Blames Artificial Sweetener as Culprit for Blood Clots and Heart Attacks – Timcast
This is a modal window.
No compatible source was found for this media.
This video is from the The Prisoner channel on Brighteon.com . More related stories:
More CLOT SHOT COVER STORIES run by fake news CNN blaming erythritol for sudden deaths by heart attack and stroke .
Erythritol: A natural, low-calorie alternative to refined sugar .
On keto diet? Satisfy that sweet tooth with these keto-approved sweeteners .
The truth about sugar alcohols: They are neither sugar nor alcohol, and they can destroy your health . Keto dessert recipe: This delicious low-carb cheesecake will satisfy your sweet tooth . Sources include: ChildrensHealthDefense.org Nature.com Newsroom.ClevelandClinic.org SagePub.com MDPI.com VeryWellHealth.com Brighteon.com
What happens if neurotechnology learns to read our minds?
Credit: CC0 Public Domain Advancements in neurotechnology could be at a turning point, but the new technology threatens to breach even the privacy of our brains. Looking at a recent case on this issue in the Supreme Court in Chile, Sydney Law School research addresses the need for Australia to protect our human rights and to reconsider many areas of law.
Neurotech law expert Dr. Allan McCay from the Sydney Law School said, “we are witnessing a time where neurotechnology is already starting to address neurological conditions such as Parkinson’s disease and epilepsy, and it may start to become a useful response to other conditions including stroke, dementia, or even various forms of mental illness.”
“But while the advances could tackle these conditions and perhaps change the way live and work, more focus is needed on the question of how the law should protect the integrity of our brain and minds, and there should also be more consideration of the broader legal implications of this emerging technology.”
The Law Society of England and Wales recently published Dr. McCay’s report, ” Neurotechnology, law and the legal profession: Recent developments ,” where he argues that while the potential of neuroscience to improve lives is enormous, the level of intrusion needed to realize these benefits is profound.
Dr. McCay said there needs to be more discussion about what happens as these capabilities move from medicine into a less regulated commercial world.
“An important question is how well-placed Australian law is to deal with challenges of technologies that monitor and/or influence the brain.” Protecting our brains
“Australia needs to consider what kind of response is needed here given that other countries’ governments have already moved to address such issues,” said Dr. McCay.
“In August this year, the Chilean Supreme Court handed down a historic judgment with respect to neurotechnology and human rights , which addressed the issue of the protection of brain data, drawing on their recently upgraded constitution.”
In 2021, Chile brought about the world’s first neurotech-inspired constitutional change and this modification inserted the following words into section 19 of the constitution:
Scientific and technological development will be at the service of people and will be carried out with respect for life and physical and mental integrity. The law will regulate the requirements, conditions and restrictions for its use in people, having to protect especially the brain activity, as well as the information coming from it.
The change was a milestone in the protection of neurodata (data derived from the brain or nervous system ) and has set a precedent, with other countries now also looking at constitutional change.
The Supreme Court’s decision was in relation to a product (marketed as Insight) which monitors the brainwaves of users. The device might be used to monitor cognitive performance including levels of attentiveness or stress or used to control devices.
Drawing on the 2021 constitutional change, the court ordered Emotiv, the company (which began in Australia) that produced the product to remove the appellant’s brain data from their portals and “The Cloud.”
The appellant, Guido Girardi, a former Chilean senator, was a driving force behind the 2021 constitutional change and strongly advocates for “neurorights.” Human Rights and neurotech
Dr. McCay says the Australian Human Rights Commission is now actively considering what Australia and the international community might do. Both the Human Rights Commissioner and the President of the Human Rights Commission have spoken at Australian events with a neurotechnology focus, and the Commission recently made a submission to the UN concerning neurotechnology and human rights.
“But it seems the consideration of Australia’s response to neurotechnology needs to expand,” said Dr. McCay.
“These devices might not just extract information but act upon our brains and nervous systems to influence them.
“Neurotechnology will challenge a variety of areas of law. This will require Law Reform Commissions in Australia look at the emerging challenges, and it also means that various regulators such as the Office of the Australian Information Commissioner should consider the technology’s implications.
“However, in addressing the legal issues, we must avoid a regulatory environment that stops the development of beneficial therapeutic neurotechnology—this technology must be supported rather than impeded.
“These matters will require political leadership. While in Australia, artificial intelligence is currently, at least to some extent, on the political agenda, the more specific issues relating to humans developing a much closer connection or even merging with technology are entirely absent from Australian political discourse.
“That now needs to change. It is critical that we give our full attention to laws that protect the privacy and integrity of our brains and consider the many other ways in which neurotechnology will impact upon the law.”
He adds that the Chilean developments are particularly significant for Australia, as there has been a recent increased commercial interest in neurotechnology.
“The level of investment alone suggests the time is right for Australia to further consider a response to neurotechnology,” said Dr. McCay.
Dr. McCay analyzes the significance of the case in more detail in this article in Law Society of NSW .
More information: Neurotechnology, law and the legal profession. www.lawsociety.org.uk/topics/r … -the-practice-of-law
Provided by University of Sydney
Brain Power Renewed: A Biomarker’s Predictive Magic on Neuron Regeneration
UC San Diego researchers discover a “molecular fingerprint” using single-cell RNA sequencing that predicts if neurons will regenerate after injury, offering new insights into understanding and enhancing neuronal regeneration. Findings could help scientists develop regenerative therapies for spinal cord injuries and other neurological conditions.
Neurons, the main cells that make up our brain and spinal cord, are among the slowest cells to regenerate after an injury, and many neurons fail to regenerate entirely. While scientists have made progress in understanding neuronal regeneration, it remains unknown why some neurons regenerate and others do not.
Using single-cell RNA sequencing, a method that determines which genes are activated in individual cells, researchers from University of California San Diego School of Medicine have identified a new biomarker that can be used to predict whether or not neurons will regenerate after an injury. Testing their discovery in mice, they found that the biomarker was consistently reliable in neurons across the nervous system and at different developmental stages. The study was published on October 16, 2023, in the journal Neuron . The Power of Single-Cell Sequencing
“Single-cell sequencing technology is helping us look at the biology of neurons in much more detail than has ever been possible, and this study really demonstrates that capability,” said senior author Binhai Zheng, PhD, professor in the Department of Neurosciences at UC San Diego School of Medicine. “What we’ve discovered here could be just the beginning of a new generation of sophisticated biomarkers based on single-cell data.”
The researchers focused on neurons of the corticospinal tract, a critical part of the central nervous system that helps control movement. After injury, these neurons are among the least likely to regenerate axons—the long, thin structures that neurons use to communicate with one another. This is why injuries to the brain and spinal cord are so devastating.
Neurons, shown here in red and yellow, are some of the slowest cells to regenerate after injury. In this section of a mouse brain, yellow neurons are regenerating while red neurons are non-regenerating. Credit: UC San Diego Health Sciences
“If you get an injury in your arm or your leg, those nerves can regenerate and it’s often possible to make a full functional recovery, but this isn’t the case for the central nervous system,” said first author Hugo Kim, PhD, a postdoctoral fellow in the Zheng lab. “It’s extremely difficult to recover from most brain and spinal cord injuries because those cells have very limited regenerative capacity. Once they’re gone, they’re gone.” Identifying the Biomarker
The researchers used single-cell RNA sequencing to analyze gene expression in neurons from mice with spinal cord injuries. They encouraged these neurons to regenerate using established molecular techniques, but ultimately, this only worked for a portion of the cells. This experimental setup allowed the researchers to compare sequencing data from regenerating and non-regenerating neurons.
Further, by focusing on a relatively small number of cells — just over 300 — the researchers were able to look extremely closely at each individual cell.
“Just like how every person is different, every cell has its own unique biology,” said Zheng. “Exploring minute differences between cells can tell us a lot about how those cells work.”
Hugo Kim, PhD (left) designed and executed the single-cell RNA sequencing experiments under the supervision of Binhai Zheng, PhD (right). Credit: UC San Diego Health Sciences
Using a computer algorithm to analyze their sequencing data, the researchers identified a unique pattern of gene expression that can predict whether or not an individual neuron will ultimately regenerate after an injury. The pattern also included some genes that had never been previously implicated in neuronal regeneration.
“It’s like a molecular fingerprint for regenerating neurons,” added Zheng. Validating the Regeneration Classifier
To validate their findings, the researchers tested this molecular fingerprint, which they named the Regeneration Classifier, on 26 published single-cell RNA sequencing datasets. These datasets included neurons from various parts of the nervous system and at different developmental stages.
The team found that with few exceptions, the Regeneration Classifier successfully predicted the regeneration potential of individual neurons and was able to reproduce known trends from previous research, such as a sharp decrease in neuronal regeneration just after birth.
“Validating the results against many sets of data from completely different lines of research tells us that we’ve uncovered something fundamental about the underlying biology of neuronal regeneration,” said Zheng. “We need to do more work to refine our approach, but I think we’ve come across a pattern that could be universal to all regenerating neurons.”
While the results in mice are promising, the researchers caution that at present, the Regeneration Classifier is a tool to help neuroscience researchers in the lab rather than a diagnostic test for patients in the clinic.
“There are still a lot of barriers to using single-cell sequencing in clinical contexts, such as high cost, difficulty analyzing large amounts of data and, most importantly, accessibility to tissues of interest,” said Zheng. “For now, we’re interested in exploring how we can use the Regeneration Classifier in preclinical contexts to predict the effectiveness of new regenerative therapies and help move those treatments closer to clinical trials.”
Reference: “Deep scRNA sequencing reveals a broadly applicable Regeneration Classifier and implicates antioxidant response in corticospinal axon regeneration” by Hugo J. Kim, Junmi M. Saikia, Katlyn Marie A. Monte, Eunmi Ha, Daniel Romaus-Sanjurjo, Joshua J. Sanchez, Andrea X. Moore, Marc Hernaiz-Llorens, Carmine L. Chavez-Martinez, Chimuanya K. Agba, Haoyue Li, Joseph Zhang, Daniel T. Lusk, Kayla M. Cervantes and Binhai Zheng, 16 October 2023, Neuron .
DOI: 10.1016/j.neuron.2023.09.019
Co-authors of the study include: Junmi M. Saikia, Katlyn Marie A. Monte, Eunmi Ha, Daniel Romaus-Sanjurjo, Joshua J. Sanchez, Andrea X. Moore, Marc Hernaiz-Llorens, Carmine L. Chavez-Martinez, Chimuanya K. Agba, Haoyue Li, Joseph Zhang, Daniel T. Lusk and Kayla M. Cervantes, all at UC San Diego.
Converting brain immune cells into neurons aids post-stroke recovery

Researchers have restored function in stroke-affected mice by converting brain immune cells to neuronsDepositphotos Researchers have converted brain immune cells into neurons, replacing damaged ones and restoring function in stroke-affected mice. The next step is to see if the same results can be achieved using human brain cells, opening the door to a potential treatment for stroke.
After a stroke or other cerebrovascular disease has deprived the brain of blood flow, neurons are either damaged or die, causing characteristic physical and mental deficits. Now, researchers from Kyushu University in Japan have converted microglia, the brain’s primary immune cells, into neurons to restore motor function in stroke-affected mice.
More Stories
“When we get a cut or break a bone, our skin and bone cells can replicate to heal our body,” said Kinichi Nakashima, a corresponding author of the study. “But the neurons in our brain cannot easily regenerate, so the damage is often permanent. We therefore need to find new ways to place lost neurons.”
The researchers knew from their previous research that microglia could be induced to develop into neurons in the brains of healthy mice. Following a stroke, microglia, responsible for removing damaged or dead brain cells, move towards the injury site and replicate quickly.
“Microglia are abundant and exactly in the place we need them, so they are an ideal target for conversion,” said Takashi Irie, the study’s lead author.
The researchers induced a stroke in mice by temporarily blocking the right middle cerebral artery, a major blood vessel in the brain commonly associated with stroke in humans. After a week, the mice were observed to have difficulties in motor function and a marked loss of neurons in the striatum, a region of the brain involved in decision-making, action planning and motor control.
They used a lentivirus – a subclass of retrovirus used as a viral vector – to insert DNA into microglial cells at the site of the stroke injury. The DNA contained instructions for producing NeuroD1, a protein that induces neuronal conversion. Over subsequent weeks, the cells developed into neurons. Production of the protein NeuroD1 in microglial cells induces their development into neurons (red), reducing areas of neuron loss (dark patches) At three weeks post-insertion of DNA, the mice showed improved motor function. By eight weeks, the newly induced neurons had successfully integrated into the brain’s circuitry. When the researchers removed the new neurons, motor function improvements were lost, confirming that the new neurons directly contributed to the mice’s recovery.
“These results are very promising,” Nakashima said. “The next step is to test whether NeuroD1 is also effective at converting human microglia into neurons and confirm that our method of inserting genes into the microglial cells is safe.”
Because the treatment was administered to the mice in the acute phase after stroke when microglia have migrated to the injury site, the researchers next plan to see if they can produce recovery in mice at a later stage.
Brain cell ‘atlas’ could boost research on neuropsychiatric conditions: Are we there yet?
In a collaborative study led by the University of California San Diego, scientists have examined over 1 million human brain cells to craft intricate maps of gene regulators specific to different brain cell types.
This research not only demonstrates the intricate links between distinct cell categories and prevalent neuropsychiatric disorders but also pioneers the use of artificial intelligence to predict the impact of high-risk gene variations within these cells, potentially unlocking insights into disease development.
This study forms a vital part of the National Institute of Health’s transformative BRAIN Initiative, initiated in 2014, which seeks to revolutionise our understanding of the mammalian brain by advancing innovative neurotechnologies for classifying various neural cell types.
A new study, published in a special edition of Science , highlights the connections between particular cell types and various prevalent neuropsychiatric conditions.
In the human brain, each cell possesses an identical DNA sequence, but various cell types utilise distinct genes in varying quantities.
This diversity results in the creation of numerous brain cell types and adds to the intricacy of neural networks.
Gaining insights into the molecular distinctions among these cell types is crucial for comprehending brain functionality and devising innovative approaches to address neuropsychiatric disorders, such as schizophrenia , bipolar disorder , Alzheimer’s disease , and major depression . Human brain not uniform, an intricate system
The human brain is not uniform in nature. It comprises an incredibly intricate system of neurons and non-neuronal cells, each with distinct roles.
Creating a comprehensive map of these diverse brain cell types and deciphering their collaborative functions will ultimately lead to the identification of novel treatments that can specifically target relevant cell types associated with particular diseases.
Four experts, not involved in this research, spoke to Medical News Today about its findings.
Dr. Ryan S. Sultan is an assistant professor of clinical psychiatry in the Department of Psychiatry at Columbia University Irving Medical Center and the New York State Psychiatric Institute. He noted that the current research “explores an important topic in neuroscience and genetics.”
Dr. Sultan explained that “the study is extensive, encompassing an analysis of chromatin accessibility in 1.1 million cells from various brain regions.”
The researchers pinpointed 107 unique subcategories of brain cells and established connections between aspects of their molecular characteristics and various neuropsychiatric disorders, such as schizophrenia, bipolar disorder, Alzheimer’s disease, and major depression.
Subsequently, the researchers constructed machine learning models aimed at forecasting how specific DNA sequence variations can impact gene regulation and contribute to the development of diseases.
Although these recent findings provide significant insights into the human brain and its disorders, scientists are still in the process of comprehensively mapping the brain.
Dr. James Giordano , the Pellegrino Center professor of neurology and biochemistry at Georgetown University Medical Center, commented on the Science special issue, published on October 13, 2023, which covers research based on The BRAIN Initiative.
He said that “these studies, published in a series of papers in notable medical journals, present the first comprehensive map of molecular mechanisms inherent to specific cell types in discrete areas of the human brain.” “Taken together, these studies, afford a ‘molecular atlas’ of nodes of cells that are genotypically correlated to the expression of certain structural and functional phenotypes that may be involved in a number of neuropsychiatric conditions.”
– Dr. James Giordano Dr. Consuelo Walss-Bass , professor of psychiatry and behavioral sciences and director of the Psychiatric Genetics program at UTHealth Houston, noted that “research of [the] human brain has been historically difficult because of limited ability to obtain human brain samples.”
“However, recently, advances in genomic technologies, coupled with increased availability of postmortem brain tissue, have facilitated the generation of multi-level omics data, including epigenomics, transcriptomics, proteomics, in [the] human brain,” she added. “This is a seminal example of the advances in technology, describing how it is now possible to identify, at the single cell level, DNA regions that are involved in regulating how genes are expressed (genes being ‘turned on or off’). Up till now, there was a lack of technology that allowed for this level of knowledge to be resolved at the individual cell level.”
– Dr. Consuelo Walss-Bass Future is promising, but more research needed
However, Dr. Stefan Ivantu , consultant psychiatrist at ADHD Specialist, said that he felt researchers still had a long way to go until compiling a true “brain cell Atlas.”
“[I]n my opinion,” he told us, “analyzing 1 million cells is considered a small sample given the complexity of the human brain. Very few [people] are aware that the human brain has on average 86 billion cells that are interacting with each other constantly.”
“What makes it even more difficult are the interactions between the cells, which are far more complex,” he added. “However, with more powerful imagistic and AI tool, we may be able to understand the patterns related to specific conditions.”
In Dr. Ivantu’s view, “[a] more promising field is quantum computing, which this linked with the recent AI advances may be more effective in understanding the human brain.”
Nevertheless, he noted that “[i]t is extremely encouraging that researchers are using more technology for the next steps in understanding the human brain, and I believe this is the right approach.”
Dr. Walss-Bass pointed out that the researchers “have identified areas of the genome in individual brain cells that determine whether a gene will become expressed, that is, turned into RNA and then protein, to perform specific functions.”“From this, the authors were then able to correlate genes that had been previously associated with schizophrenia and other psychiatric disorders to areas in the DNA where the expression of these genes is being regulated,” she explained. “Understanding how gene expression is regulated in specific cell types in the brain is a significant advancement that will help to shed light shed light on the neurobiological mechanisms of psychiatric disorders and could lead to development of new therapies to treat these disorders.”– Dr. Consuelo Walss-Bass Dr. Sultan explained that this “research has significant implications for patients and the public.” “It advances our understanding […]
White Matter Wonders: Re-imagining the Brain’s Silent Majority
Summary: Historically, scientific research has largely focused on the gray matter of the brain, leaving the equally important white matter understudied. However, a recent groundbreaking study has used fMRI to detect significant brain activity in white matter.
When subjects performed tasks, researchers observed increased BOLD signals throughout the white matter.
This discovery challenges conventional beliefs about the brain’s activity and emphasizes the potential importance of white matter in understanding various brain disorders.
Key Facts:
> The Vanderbilt team, led by John Gore, Ph.D., utilized fMRI to identify BOLD signals, indicative of brain activity, in the white matter—previously a little-researched area.
When subjects performed tasks during the study, there was a noticeable increase in BOLD signals in the white matter across the entire brain.
Despite the current lack of full understanding about these white matter signals, they’re believed to hold valuable insights, especially since many brain disorders, including epilepsy and multiple sclerosis, disrupt the brain’s “connectivity.”
Source: Vanderbilt University
The human brain is made up of two kinds of matter: the nerve cell bodies (gray matter), which process sensation, control voluntary movement, and enable speech, learning and cognition, and the axons (white matter), which connect cells to each other and project to the rest of the body.
Historically, scientists have concentrated on the gray matter of the cortex, figuring that’s where the action is, while ignoring white matter, even though it makes up half the brain. Researchers at Vanderbilt University are out to change that.
For several years, John Gore, Ph.D., director of the Vanderbilt University Institute of Imaging Science, and his colleagues have used functional magnetic resonance imaging (fMRI) to detect blood oxygenation-level dependent (BOLD) signals, a key marker of brain activity, in white matter.
In their latest paper, published Oct. 12 in the Proceedings of the National Academy of Sciences , the researchers report that when people who are having their brains scanned by fMRI perform a task, like wiggling their fingers, BOLD signals increase in white matter throughout the brain.
“We don’t know what this means,” said the paper’s first author, Kurt Schilling, Ph.D., research assistant professor of Radiology and Radiological Sciences at VUMC. “We just know that something is happening. There truly is a powerful signal in the white matter.”
It is important to pursue this because disorders as diverse as epilepsy and multiple sclerosis disrupt the “connectivity” of the brain, Schilling said. This suggests that something is going on in white matter.
To find out, the researchers will continue to study changes in white matter signals they’ve previously detected in schizophrenia, Alzheimer’s disease and other brain disorders. Through animal studies and tissue analysis, they also hope to determine the biological basis for these changes.
In gray matter, BOLD signals reflect a rise in blood flow (and oxygen) in response to increased nerve cell activity.
Perhaps the axons, or the glial cells that maintain the protective myelin sheath around them, also use more oxygen when the brain is “working.” Or perhaps these signals are somehow related to what’s going on in the gray matter.
But even if nothing biological is going on in white matter, “there’s still something happening here,” Schilling said. “The signal is changing. It’s changing differently in different white matter pathways and it’s in all white matter pathways, which is a unique finding.”
One reason that white matter signals have been understudied is that they have lower energy than gray matter signals, and thus are more difficult to distinguish from the brain’s background “noise.”
The VUMC researchers boosted the signal-to-noise ratio by having the person whose brain was being scanned repeat a visual, verbal or motor task many times to establish a trend and by averaging the signal over many different white matter fiber pathways.
“For 25 or 30 years, we’ve neglected the other half of the brain,” Schilling said. Some researchers not only have ignored white matter signals but have removed them from their reports of brain function.
The Vanderbilt findings suggest that many fMRI studies thus “may not only underestimate the true extent of brain activation, but also … may miss crucial information from the MRI signal,” the researchers concluded. About this neuroscience research news
Author: Bill Snyder
Source: Vanderbilt University
Contact: Bill Snyder – Vanderbilt University
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“ Whole-brain, gray, and white matter time-locked functional signal changes with simple tasks and model-free analysis ” by Kurt G. Schilling et al. PNAS Abstract Whole-brain, gray, and white matter time-locked functional signal changes with simple tasks and model-free analysis Recent studies have revealed the production of time-locked blood oxygenation level–dependent (BOLD) functional MRI (fMRI) signals throughout the entire brain in response to tasks, challenging the existence of sparse and localized brain functions and highlighting the pervasiveness of potential false negative fMRI findings.“Whole-brain” actually refers to gray matter, the only tissue traditionally studied with fMRI. However, several reports have demonstrated reliable detection of BOLD signals in white matter, which have previously been largely ignored.Using simple tasks and analyses, we demonstrate BOLD signal changes across the whole brain, in both white and gray matters, in similar manner to previous reports of whole brain studies.We investigated whether white matter displays time-locked BOLD signals across multiple structural pathways in response to a stimulus in a similar manner to the cortex. We find that both white and gray matter show time-locked activations across the whole brain, with a majority of both tissue types showing statistically significant signal changes for all task stimuli investigated.We observed a wide range of signal responses to tasks, with different regions showing different BOLD signal changes to the same task. Moreover, we find that each region may display different BOLD responses to different stimuli.Overall, we present compelling evidence that, just like all gray matter, essentially all white matter in the brain shows time-locked BOLD signal changes in response to multiple stimuli, challenging the idea of sparse functional localization and the prevailing wisdom of treating white matter BOLD signals as artifacts to be removed.
