Learn about brain health and nootropics to boost brain function
A Personalized Brain Implant Curbed a Woman’s OCD
Amber Pearson has had a severe form of obsessive compulsive disorder since she was in high school. She would wash her hands so much they became raw and bled. Her bedtime routine easily took 45 minutes because it involved checking that all the doors and windows were closed and the stove was off. She was so afraid of food contamination that she couldn’t eat next to other people. Even on holidays, she ate on the couch away from her family. Therapy and medication didn’t help.
“Every decision I made was based on my OCD. It was always in the back of my mind,” Pearson says.
In her twenties, she developed epilepsy. After suffering a serious seizure that caused her to lose consciousness, her doctors considered treating her with deep brain stimulation, or DBS. The procedure involves surgically implanting a device that delivers electrical pulses to a specific brain region. Scientists think DBS works by resetting abnormal brain circuits, similar to what a pacemaker does for the heart.
DBS has been used for the past three decades to control tremors in people with Parkinson’s disease, and researchers are currently exploring it to restore upper body movement to stroke survivors and as a treatment for some psychiatric disorders . The US Food and Drug Administration permits its use for OCD as a last resort. Pearson wondered if the implant might help treat both of her conditions, so in 2019, she underwent an experimental brain surgery at Oregon Health & Science University.
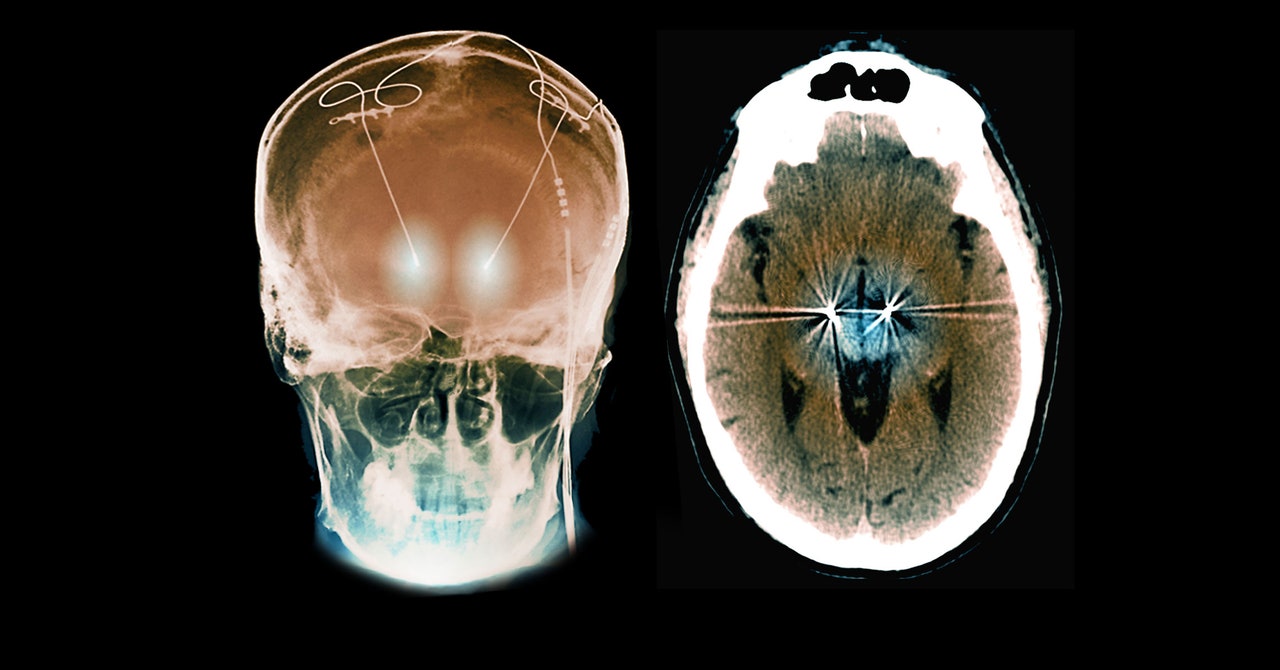
In a study published this month in the journal Neuron , Pearson’s medical team reported that a single 32-millimeter-long electrode, tuned to detect her unique neural signals, was able to control both. Unlike traditional DBS, which provides constant stimulation, Pearson’s device is a “responsive” one; it only delivers jolts of electricity when it detects irregular patterns in her brain associated with the start of a seizure or compulsive thoughts.
Responsive DBS is already used for epilepsy, but Pearson’s medical team says it’s the first time it’s been used for OCD, as well as to simultaneously treat two conditions.
“This is pretty remarkable,” says Rachel Davis, an associate professor of psychiatry and neurosurgery at the University of Colorado School of Medicine, who researches DBS but was not involved in the new study.
Pearson’s seizures were occurring in a part of the brain called the insula, so her neurosurgeon, Ahmed Raslan, thought he could target a small region there for her epilepsy, plus the ventral striatum, which sits just above and behind the eyes. This contains the nucleus accumbens—an area associated with motivation and action, including compulsive urges. “It was an area that could be targeted with the same electrode,” Raslan says.
The team used a device made by a company called NeuroPace, based in Mountain View, California. Other electrodes used for deep brain stimulation only emit electrical pulses. This one also collects brain signals and delivers electricity only when it is programmed to detect a certain trigger.
First, the Oregon team used the device to get Pearson’s epilepsy under control. Next, Raslan sought out Casey Halpern, an associate professor of neurosurgery at Penn Medicine who is studying the nucleus accumbens as a DBS target for psychiatric conditions. To program the stimulation for Pearson’s OCD, Halpern and his team first needed to figure out what neural trigger they were looking for.
To do this, they needed to know which neural signatures in Pearson’s brain activity corresponded with her experience of obsessive thoughts. As she went about her ordinary life at home, Pearson would swipe a magnet over her head when she felt obsessive thoughts, and her implanted device would time-stamp the moment of each event.
Halpern and his colleagues also worked with Pearson in the lab, intentionally exposing her to items that triggered her OCD. For example, because one of Pearson’s triggers was seafood contamination, the team gave her seafood to handle while monitoring her brain activity as she became distressed.
By analyzing these brain recordings, Halpern was able to identify a unique neural signature in the ventral striatum that corresponded to times when Pearson felt she had to act on her compulsions. “We found that low-frequency oscillations would elevate in power during those moments,” Halpern says. This low-frequency signal was the same whether Pearson was experiencing a distressing situation in the lab or at home.
The researchers programmed her device to only deliver stimulation when it detects this type of brain activity—and only briefly. After a few seconds to a minute, it shuts off. The goal, Halpern says, is to restore normal function to abnormal neural circuits.
Over the next six to eight months, Pearson’s OCD symptoms decreased significantly, and her brain activity triggered the stimulation less often. She told her doctors that before, she was sometimes spending eight hours a day performing compulsions. Now, she estimates that it’s more like 30 minutes. The effects have persisted over the two years since the stimulation has been turned on. “It wasn’t instantaneous. It took a few months to notice changes,” she says. “I slowly started noticing things disappearing from my routine. Then, more things would disappear.”
Pearson doesn’t wash her hands as often, and now her knuckles don’t bleed. Her bedtime routine takes just 15 minutes. The best part, she says, is that her relationships with her friends and family are a lot better. She can enjoy a meal with them without feeling distressed.
“What this highlights is that OCD is a disorder of the brain, just like epilepsy and Parkinson’s,” Halpern says. “This isn’t a disorder of will. There’s a pathological signal that we’re seeing in the brain.”
Davis says she was initially skeptical of the idea that OCD could be treated with occasional bursts of stimulation. “Often people with OCD have a baseline level of dread or anxiety,” she says. For that reason, she assumed patients would need constant stimulation to keep their brain circuits regulated. Her center has implanted nine OCD patients with traditional DBS devices that provide steady stimulation. Although the Neuron report is just one case study, she thinks it’s impressive that Pearson’s symptoms […]