Nature Knows and Psionic Success
God provides
Memory loss ‘can be reversed by simple diet changes’

Memory loss can be reversed by increasing intake of foods such as green tea, apples and berries, new research suggests.
The study is the first to show that a diet with insufficient flavanols – nutrients found in certain fruits and vegetables – stops the brain functioning at its best, and drives memory loss.
Flavonols are present in many foods including green leafy vegetables, blackcurrants, onions, apples, berries, cherries, peaches, soybeans, citrus foods, tea, chocolate, lettuce, peppers, grapes and even wine.
The study by US researchers found that over-60s who already consumed sufficient flavanols saw no benefit when they added more, but those with deficits recorded memory improvements of an average of 16 per cent in a year.
“The improvement among study participants with low-flavanol diets was substantial and raises the possibility of using flavanol-rich diets or supplements to improve cognitive function in older adults,” said Dr Adam Brickman, professor of neuropsychology at Columbia University.
Experts said the finding supports the idea that the ageing brain requires specific nutrients to stay functioning well, just as the developing brain of children requires specific nutrients for proper growth.
Previous studies in animals have shown that flavanols boost the growth of neurons and blood vessels in the hippocampus – a region of the brain which is crucial for learning and developing new memories.
For the study, more than 3,500 healthy older adults were randomly assigned to receive a daily flavanol supplement pill or placebo pill for three years.
The active supplement contained 500 mg of flavanols, a daily amount that adults are advised to get from food.
Such a dose could be achieved naturally through one mug of tea, six squares of dark chocolate , and a couple of servings of berries or apples. ‘Really important’ research
At the beginning of the study, all participants completed a survey that assessed the quality of their diet, and performed a series of web-based activities in their own homes, designed to test their short-term memory.
The tests were then repeated after years one, two, and three.
At the end of the first year of taking the flavanol supplement, participants who reported consuming a poorer diet and had lower baseline levels of flavanols saw their memory scores increase by an average of 10.5 per cent, compared to those who took the placebo pill, and 16 per cent compared to their memory at baseline.
And the improvement lasted for at least two more years.
Commenting on the research, Prof Aedin Cassidy, Chair in Nutrition & Preventative Medicine at Queen’s University Belfast (QUB), said: “This is a really important study showing that [a] dose of flavonoids called flavanols, present in tea, cocoa, apples, and berries, is key for improving memory in the ageing brain.
“Supplementing with flavanols reversed the lower memory in the participants who had low diet quality after one year of intake and this was sustained throughout the three year intervention period.
“So when habitual diets are not as healthy as they could be, we now have evidence that simple additions to the diet like flavanols can contribute to maintaining brain health as we age.”
The team said they could not definitively conclude that low dietary intake of flavanols alone causes poor memory performance, because they did not conduct an experiment where they removed flavanol to see if it made memory worse.
To find out for sure, they now want to conduct a clinical trial in which they restore flavanol levels in adults with severe flavanol deficiency to see if it improves memory.
“Age-related memory decline is thought to occur sooner or later in nearly everyone, though there is a great amount of variability,” said Dr Scott Small, Professor of Neurology at Columbia University.
“If some of this variance is partly due to differences in dietary consumption of flavanols, then we would see an even more dramatic improvement in memory in people who replenish dietary flavanols when they’re in their 40s and 50s.”
The research was published in the journal PNAS.
Sign up to the Front Page newsletter for free: Your essential guide to the day’s agenda from The Telegraph – direct to your inbox seven days a week.
Rhythmically stimulating the brain with electrical currents could boost cognitive function, according to analysis of over 100 studies
(THE CONVERSATION) – Figuring out how to enhance a person’s mental capabilities has been of considerable interest to psychology and neuroscience researchers like me for decades . From improving attention in high-stakes environments, like air traffic management, to reviving memory in people with dementia, the ability to improve cognitive function can have far-reaching consequences. New research suggests that brain stimulation could help achieve the goal of boosting mental function.
In the Reinhart Lab at Boston University, my colleagues and I have been examining the effects of an emerging brain stimulation technology – transcranial alternating current stimulation, or tACS – on different mental functions in patients and healthy people.
During this procedure, people wear an elastic cap embedded with electrodes that deliver weak electrical currents oscillating at specific frequencies to their scalp. By applying these controlled currents to specific brain regions, it is possible to alter brain activity by nudging neurons to fire rhythmically .
Why would rhythmically firing neurons be beneficial? Research suggests that brain cells communicate effectively when they coordinate the rhythm of their firing. Critically, these rhythmic patterns of brain activity show marked abnormalities during neuropsychiatric illnesses. The purpose of tACS is to externally induce rhythmic brain activity that promotes healthy mental function, particularly when the brain might not be able to produce these rhythms on its own.
However, tACS is a relatively new technology, and how it works is still unclear. Whether it can strengthen or revive brain rhythms to change mental function has been a topic of considerable debate in the field of brain stimulation. While some studies find evidence of changes in brain activity and mental function with tACS, others suggest that the currents typically used in people might be too weak to have a direct effect.
When faced with conflicting data in the scientific literature, it can be helpful to conduct a type of study called a meta-analysis that quantifies how consistent the evidence is across several studies. A previous meta-analysis conducted in 2016 found promising evidence for the use of tACS in changing mental function. However, the number of studies has more than doubled since then. The design of tACS technologies has also become increasingly sophisticated .
We set out to perform a new meta-analysis of studies using tACS to change mental function. To our knowledge, this work is the largest and most comprehensive meta-analysis yet on this topic, consisting of over 100 published studies with a combined total of more than 2,800 human participants.
After compiling over 300 measures of mental function across all the studies, we observed consistent and immediate improvement in mental function with tACS. When we examined specific cognitive functions, such as memory and attention, we observed that tACS produced the strongest improvements in executive function , or the ability to adapt in the face of new, surprising or conflicting information.
We also observed improvements in the ability to pay attention and to memorize information for both short and long periods of time. Together, these results suggest that tACS could particularly improve specific kinds of mental function, at least in the short term.
To examine the effectiveness of tACS for those particularly vulnerable to changes in mental function, we examined the data from studies that included older adults and people with neuropsychiatric conditions. In both populations, we observed reliable evidence for improvements in cognitive function with tACS.
Interestingly, we also found that a specialized type of tACS that can target two brain regions at the same time and manipulate how they communicate with each other can both enhance or reduce cognitive function . This bidirectional effect on mental function could be particularly useful in the clinic. For example, some psychiatric conditions like depression may involve a reduced ability to process rewards, while others like bipolar disorder may involve a highly active reward processing system . If tACS can change mental function in either direction, researchers may be able to develop flexible and targeted designs that cater to specific clinical needs.
Developments in the field of tACS are bringing researchers closer to being able to safely enhance mental function in a noninvasive way that doesn’t require medication. Current statistical evidence across the literature suggests that tACS holds promise, and improving its design could help it produce stronger, long-lasting changes in mental function.
Copyright 2022 Nexstar Media, Inc. All rights reserved. This material may not be published, broadcast, rewritten, or redistributed.
For the latest news, weather, sports, and streaming video, head to KRQE NEWS 13 – Breaking News, Albuquerque News, New Mexico News, Weather, and Videos.
This Emerging Brain Stimulation Technology Could Boost Cognitive Function

Figuring out how to enhance a person’s mental capabilities has been of considerable interest to psychology and neuroscience researchers like me for decades . From improving attention in high-stakes environments, like air traffic management, to reviving memory in people with dementia, the ability to improve cognitive function can have far-reaching consequences. New research suggests that brain stimulation could help achieve the goal of boosting mental function.
In the Reinhart Lab at Boston University, my colleagues and I have been examining the effects of an emerging brain stimulation technology – transcranial alternating current stimulation, or tACS – on different mental functions in patients and healthy people.
During this procedure, people wear an elastic cap embedded with electrodes that deliver weak electrical currents oscillating at specific frequencies to their scalp. By applying these controlled currents to specific brain regions, it is possible to alter brain activity by nudging neurons to fire rhythmically .
Why would rhythmically firing neurons be beneficial? Research suggests that brain cells communicate effectively when they coordinate the rhythm of their firing. Critically, these rhythmic patterns of brain activity show marked abnormalities during neuropsychiatric illnesses. The purpose of tACS is to externally induce rhythmic brain activity that promotes healthy mental function, particularly when the brain might not be able to produce these rhythms on its own.
However, tACS is a relatively new technology, and how it works is still unclear. Whether it can strengthen or revive brain rhythms to change mental function has been a topic of considerable debate in the field of brain stimulation. While some studies find evidence of changes in brain activity and mental function with tACS, others suggest that the currents typically used in people might be too weak to have a direct effect.
When faced with conflicting data in the scientific literature, it can be helpful to conduct a type of study called a meta-analysis that quantifies how consistent the evidence is across several studies. A previous meta-analysis conducted in 2016 found promising evidence for the use of tACS in changing mental function. However, the number of studies has more than doubled since then. The design of tACS technologies has also become increasingly sophisticated .
We set out to perform a new meta-analysis of studies using tACS to change mental function. To our knowledge, this work is the largest and most comprehensive meta-analysis yet on this topic, consisting of over 100 published studies with a combined total of more than 2,800 human participants.
After compiling over 300 measures of mental function across all the studies, we observed consistent and immediate improvement in mental function with tACS. When we examined specific cognitive functions, such as memory and attention, we observed that tACS produced the biggest improvements in executive function , or the ability to adapt in the face of new, surprising, or conflicting information.
We also observed improvements in the ability to pay attention and memorize information for both short and long periods of time. Together, these results suggest that tACS could particularly improve specific kinds of mental function, at least in the short term.
To examine the effectiveness of tACS for those particularly vulnerable to changes in mental function, we examined the data from studies that included older adults and people with neuropsychiatric conditions. In both populations, we observed reliable evidence for improvements in cognitive function with tACS.
Interestingly, we also found that a specialized type of tACS that can target two brain regions at the same time and manipulate how they communicate with each other can both enhance or reduce cognitive function . This bidirectional effect on mental function could be particularly useful in the clinic. For example, some psychiatric conditions like depression may involve a reduced ability to process rewards, while others like bipolar disorder may involve a highly active reward processing system . If tACS can change mental function in either direction, researchers may be able to develop flexible and targeted designs that cater to specific clinical needs.
Developments in the field of tACS are bringing researchers closer to being able to safely enhance mental function in a noninvasive way that doesn’t require medication. Current statistical evidence across the literature suggests that tACS holds promise, and improving its design could help it produce bigger, long-lasting changes in mental function.
This article was originally published on The Conversation by Shrey Grover at Boston University. Read the original article here .
Health officials delayed report linking fluoride to brain harm

Last May, the National Toxicology Program (NTP), a federal research agency, was set to release its eagerly awaited report into the cognitive and neurodevelopmental impacts on humans from fluoride exposure.
The report was anticipated for several reasons, including its review of studies linking fluoridated water to cognitive harm in children. Water fluoridation is the long-established public policy of adding fluoride to drinking water to fight tooth decay. The report was also set to play a key role in an ongoing lawsuit , filed by government accountability nonprofit Food & Water Watch, to get the Environmental Protection Agency to regulate water fluoridation because of fluoride’s possible neurotoxic harm. More than two years ago, the judge put the case on hold in expectation of the NTP report’s public release.
Before the NTP could release the report, however, “They were blocked,” said Linda Birnbaum, NTP director until 2019. According to Freedom of Information Act (FOIA) records obtained by the plaintiffs and shared with Capital & Main, the U.S. Department of Health and Human Services (HHS) held back the release of the report after criticism of its findings from health and dental organizations that advocate for community water fluoridation. Those groups challenged the report’s scientific validity and expressed concern that it could jeopardize water fluoridation, which they said could especially impact the dental health of low income communities.
Advertisement:
The report found that a link between typical levels of fluoride added to water and possible harm to brain development is unclear, with a recommendation for more studies, according to records. But the report did find a possible link to cognitive harm at approximately two times the current recommended water fluoridation level, records show. Some health experts believe this finding makes current water fluoridation levels potentially unsafe for developing fetuses and young children. Because many common foods and drinks contain fluoride, consuming them along with fluoridated water could amount to harmful exposure levels, these experts say.
Leading up to the report’s intended release, individuals from dental organizations including the American Dental Association (ADA) scrutinized the report’s scientific credibility in communications with staff from other dental groups and health agencies including the National Institutes of Health and the NTP, divisions of HHS, records show.
Advertisement:
This January, Birnbaum issued a scathing legal declaration as part of the lawsuit, writing, “The decision to set aside the results of an external peer review process based on concerns expressed by agencies with strong policy interests on fluoride suggests the presence of political interference in what should be a strictly scientific endeavor.” Birnbaum said she issued the legal declaration in part over concerns the report might never be publicly released.
The NTP has announced that it will now release the report on March 15, alongside an updated version of the same document that includes the NTP’s responses to what it describes as a “significant number” of comments and criticisms received from experts at various federal health agencies.
Birnbaum, however, remains adamant that the science proves there is “no real benefit” from ingesting fluoride. “The benefit from fluoride is from topical applications,” she said.
* * *
Advertisement:
Water fluoridation is described as one of the 10 greatest public health achievements of the 20th century for its part in reducing tooth decay in adults and children by roughly 25%. According to the latest figures , nearly 73% of people connected with community water systems receive fluoridated water, accounting for more than 200 million people, or just under two-thirds of the overall U.S. population. Advocates argue that fluoridation is especially needed in low income communities where rates of tooth decay are generally higher than in wealthier neighborhoods.
At the same time, a growing body of research links fluoride exposure to neurotoxicological impacts in humans, including IQ loss and a higher prevalence of ADHD in children.
The NTP has been working since 2016 on its systematic review of the science into these impacts. By the time the report was set for release last May, it had already undergone more rounds of peer review than is typically the case for such a document, court records show — twice with the National Academies of Sciences, Engineering, and Medicine (NASEM), and external peer review by five experts in the field. According to Birnbaum, similar reports are typically sent out for public comment, peer reviewed by an on-site panel, then finalized by the NTP.
Advertisement:
Despite this unusually rigorous review process, a network of health officials and influential dental groups argued that the NTP had failed to address several issues raised by the NASEM review committee. These issues include a need to consider more studies in the review, and a failure to properly account for bias among some of the studies selected. One key health official wrote that if the Centers for Disease Control and Prevention (CDC) had been given the option to clear the report, “We would have non-concurred,” records show.
Birnbaum said she strongly disagrees that the NTP had failed to address NASEM’s concerns. In her declaration, Birnbaum wrote that various sources told her the five external peer reviewers agreed with what was then the final report’s conclusions, and that “NTP’s staff and leadership considered the monograph to be complete and ready for publication by May 2022.”
The report’s critics also feared its findings could erode public trust in water fluoridation, with the head of one leading dental research organization calling it “potentially very bad fluoride news.”
Advertisement:
In April of last year, American Fluoridation Society President Johnny Johnson wrote an open letter to “Oral Health Advocates and Public Health Leaders” warning how the NTP’s findings were already causing public health officials to second guess their stance on community water fluoridation (CWF).
“In at least one U.S. state the NTP’s draft Monograph has led to that state’s Toxicologist not being willing to support CWF as safe, when in the past that same Toxicologist was supportive. This is directly due to the NTP’s report,” Johnson wrote.
In response to questions, Johnson wrote in an email that “since the NTP report is not yet publicly available, it would be premature to comment on something that […]
Can multivitamins improve memory? A new study shows ‘intriguing’ results

The brain requires a large number of nutrients for optimal health and efficiency, but micronutrients are typically absorbed better through foods than through supplements. Americans spend billions of dollars on supplements each year, and roughly 1 in 3 adults report taking a multivitamin. But there is a debate about whether this helps promote good health.
A team of researchers wanted to assess how a daily multivitamin may influence cognitive aging and memory. They tracked about 3,500 older adults who were enrolled in a randomized controlled trial. One group of participants took a placebo, and another group took a Silver Centrum multivitamin, for three years. The participants also took tests, administered online, to evaluate memory.
At the end of the first year, people taking a multivitamin showed improvements in the ability to recall words. Participants were given lists of words — some related, some not — and asked to remember as many as possible. (List-learning tests assess a person’s ability to store and retrieve information.)
People taking the multivitamin were able to recall about a quarter more words, which translates into remembering just a few more words, compared to the placebo group.
“We estimate that the effect of the multivitamin intervention improved memory performance above placebo by the equivalent of 3.1 years of age-related memory change,” the authors write in their paper, which was published this week in the American Journal of Clinical Nutrition . And the authors point to a sustained benefit.
“This is intriguing,” says Dr. Jeffrey Linder, chief of general internal medicine at Northwestern University Feinberg School of Medicine, who was not involved in the study. But he says the overall effect found in the study was quite small. “It seems like a pretty modest difference,” Linder says. And he points out that the multivitamins had no effect on other areas of cognition evaluated in the study, such as executive function, which may be more important measures.
Study author Dr. JoAnn Manson , who is chief of the division of preventive medicine at Brigham and Women’s Hospital, says this is not the first study to show benefits from multivitamins. She points to a study published last year in Alzheimer’s & Dementia that showed participants who took a daily multivitamin performed better, overall, on global cognitive function on tests measuring story recall, verbal fluency, digit ordering, as well as executive function.
“It is surprising that such a clear signal for benefit in slowing age-related memory loss and cognitive decline was found in the study, ” Manson says. “Those receiving the multivitamin did better than those receiving the placebo.”
Our bodies and brains require many nutrients for optimal health and efficiency. Manson says if people have deficiencies in these nutrients it may influence memory loss or speed cognitive decline. So, she says taking a multivitamin may help someone prevent a deficiency if they’re not getting all the nutrients they need from their diet.
“It’s important to highlight that a multivitamin will never be a substitute for a healthy diet,” Manson says, since micronutrients are typically better absorbed through foods than through supplements.” But it may be a complementary approach or strategy for maintaining cognitive health among older adults,” she says.
Linder says he will continue to tell his patients that if they eat a healthy diet they are unlikely to benefit much from a multivitamin. “If you’re taking too much of a particular supplement and your body doesn’t need it, you’re just peeing it out,” he says. He wrote an editorial, published in JAMA, arguing that vitamins and supplements could be a waste of money for a lot of people. He argues that we should help people adopt a better pattern of eating.
“Eating a diet that has plenty of fruits and vegetables is associated with longevity and better function and better quality of life,” Linder says. There’s plenty of research to show a healthy diet is linked to better heart health, and when it comes to protecting cognitive function, “the current thinking is that all of the stuff that’s good for your heart is also good for your brain,” he says.
When Linder talks to his patients about healthy aging, he focuses on good sleep habits, physical activity and a healthy diet. “My big concern with all of the focus that people have on vitamins is that it’s distracting them from things that actually will help them stay healthy,” Linder says.
“If someone is taking a multivitamin, I’m not going to tell them to stop,” says Dr. R. Sean Morrison , who is a geriatrician at Mount Sinai Health System in New York. But he says he would not encourage the use of multivitamins as a way to protect against memory loss, because he says the effects measured in the studies are not very convincing. “I don’t think it’s the magic bullet that people are looking for,” Morrison says. When talking to his patients, he too focuses on the importance of healthy habits and good social relationships.
The study was funded, in part, by the National Institutes of Health and other grants. The vitamins were provided by Pfizer Inc. and Haleon, the makers of Centrum, the brand of multivitamins taken by participants in the study. The study authors say the funders had “no role” in the study design, analysis or interpretation.
Copyright 2023 NPR. To see more, visit https://www.npr.org.
Walking improves brain connectivity, memory in older adults, finds study

Representative Image . Image Credit: ANI A new research from the University of Maryland School of Public Health shows that walking increases connections within and between three brain networks, including one linked to Alzheimer’s disease, adding to the increasing body of data that exercise benefits brain health. Published this month in the Journal for Alzheimer’s Disease Reports, the study examined the brains and story recollection abilities of older adults with normal brain function and those diagnosed with mild cognitive impairment, which is a slight decline in mental abilities like memory, reasoning and judgment and a risk factor for Alzheimer’s.
“Historically, the brain networks we studied in this research show deterioration over time in people with mild cognitive impairment and Alzheimer’s disease,” said J. Carson Smith, a kinesiology professor with the School of Public Health and principal investigator of the study. “They become disconnected, and as a result, people lose their ability to think clearly and remember things. We’re demonstrating that exercise training strengthens these connections.” The study builds upon Smith’s previous research, which showed how walking may decrease cerebral blood flow and improve brain function in older adults with mild cognitive impairment. Thirty-three participants, who ranged between 71 and 85 years old, walked while supervised on a treadmill four days a week for 12 weeks. Before and after this exercise regimen, researchers asked participants to read a short story and then repeat it out loud with as many details as possible. Participants also underwent functional magnetic resonance imaging (fMRI) so researchers could measure changes in communication within and between the three brain networks that control cognitive function:
Default mode network – Activates when a person isn’t doing a specific task (think daydreaming about the grocery list) and is connected to the hippocampus — one of the first brain regions affected by Alzheimer’s disease. It’s also where Alzheimer’s and amyloid plaques, a prime suspect for Alzheimer’s disease found around nerve cells, show up in tests. Frontoparietal network — Regulates decisions made when a person is completing a task. It also involves memory.
Salience network — Monitors the external world and stimuli and then decides what deserves attention. It also facilitates switching between networks to optimize performance. After 12 weeks of exercise, researchers repeated the tests and saw significant improvements in participants’ story recall abilities.
“The brain activity was stronger and more synchronized, demonstrating exercise actually can induce the brain’s ability to change and adapt,” Smith said. “These results provide even more hope that exercise may be useful as a way to prevent or help stabilize people with mild cognitive impairment and maybe, over the long term, delay their conversion to Alzheimer’s dementia.” (ANI)
(This story has not been edited by Devdiscourse staff and is auto-generated from a syndicated feed.)
Walking improves brain connectivity, memory in older adults, finds study

Representative Image . Image Credit: ANI A new research from the University of Maryland School of Public Health shows that walking increases connections within and between three brain networks, including one linked to Alzheimer’s disease, adding to the increasing body of data that exercise benefits brain health. Published this month in the Journal for Alzheimer’s Disease Reports, the study examined the brains and story recollection abilities of older adults with normal brain function and those diagnosed with mild cognitive impairment, which is a slight decline in mental abilities like memory, reasoning and judgment and a risk factor for Alzheimer’s.
“Historically, the brain networks we studied in this research show deterioration over time in people with mild cognitive impairment and Alzheimer’s disease,” said J. Carson Smith, a kinesiology professor with the School of Public Health and principal investigator of the study. “They become disconnected, and as a result, people lose their ability to think clearly and remember things. We’re demonstrating that exercise training strengthens these connections.” The study builds upon Smith’s previous research, which showed how walking may decrease cerebral blood flow and improve brain function in older adults with mild cognitive impairment. Thirty-three participants, who ranged between 71 and 85 years old, walked while supervised on a treadmill four days a week for 12 weeks. Before and after this exercise regimen, researchers asked participants to read a short story and then repeat it out loud with as many details as possible. Participants also underwent functional magnetic resonance imaging (fMRI) so researchers could measure changes in communication within and between the three brain networks that control cognitive function:
Default mode network – Activates when a person isn’t doing a specific task (think daydreaming about the grocery list) and is connected to the hippocampus — one of the first brain regions affected by Alzheimer’s disease. It’s also where Alzheimer’s and amyloid plaques, a prime suspect for Alzheimer’s disease found around nerve cells, show up in tests. Frontoparietal network — Regulates decisions made when a person is completing a task. It also involves memory.
Salience network — Monitors the external world and stimuli and then decides what deserves attention. It also facilitates switching between networks to optimize performance. After 12 weeks of exercise, researchers repeated the tests and saw significant improvements in participants’ story recall abilities.
“The brain activity was stronger and more synchronized, demonstrating exercise actually can induce the brain’s ability to change and adapt,” Smith said. “These results provide even more hope that exercise may be useful as a way to prevent or help stabilize people with mild cognitive impairment and maybe, over the long term, delay their conversion to Alzheimer’s dementia.” (ANI)
(This story has not been edited by Devdiscourse staff and is auto-generated from a syndicated feed.)
40 Hz vibrations reduce Alzheimer’s pathology, symptoms in mouse models
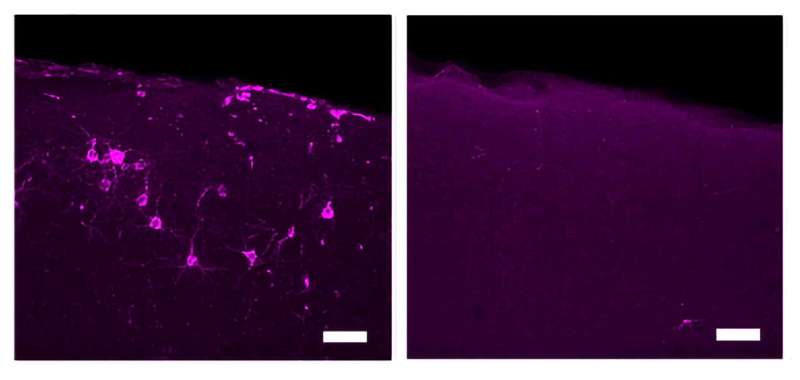
An enlarged detail from a figure in the paper highlights reductions in phosphorylated tau (magenta) in primary somatosensory cortical neurons in Tau P301S model mice treated with 40 Hz tactile stimulation (right). An image from an untreated control is on the left. Credit: Tsai Lab/MIT Picower Institute Evidence that non-invasive sensory stimulation of 40 Hz gamma frequency brain rhythms can reduce Alzheimer’s disease pathology and symptoms, already shown with light and sound by multiple research groups in mice and humans, now extends to tactile stimulation. A new study by MIT scientists shows that Alzheimer’s model mice exposed to 40 Hz vibration an hour a day for several weeks showed improved brain health and motor function compared to untreated controls.
The MIT group is not the first to show that gamma frequency tactile stimulation can affect brain activity and improve motor function , but they are the first to show that the stimulation can also reduce levels of the hallmark Alzheimer’s protein phosphorylated tau, keep neurons from dying or losing their synapse circuit connections, and reduce neural DNA damage.
“This work demonstrates a third sensory modality that we can use to increase gamma power in the brain,” said Li-Huei Tsai, corresponding author of the study, director of The Picower Institute for Learning and Memory and the Aging Brain Initiative at MIT, and Picower Professor in the Department of Brain and Cognitive Sciences (BCS).
“We are very excited to see that 40 Hz tactile stimulation benefits motor abilities, which has not been shown with the other modalities. It would be interesting to see if tactile stimulation can benefit human subjects with impairment in motor function.”
Ho-Jun Suk, Nicole Buie, Guojie Xu and Arit Banerjee are lead authors of the study in Frontiers in Aging Neuroscience and Ed Boyden, Y. Eva Tan Professor of Neurotechnology at MIT, is a co-senior author of the paper. Boyden, an affiliate member of The Picwoer Institute, is also appointed in BCS as well as the Departments of Bioengineering and Media Arts and Sciences, the McGovern Institute for Brain Research, and the K. Lisa Yang Cener for Bionics. Feeling the vibe
In a series of papers starting in 2016, a collaboration led by Tsai’s lab has demonstrated that light flickering and/or sound clicking at 40 Hz (a technology called GENUS for Gamma Entrainment Using Sensory stimuli), reduces levels of amyloid-beta and tau proteins, prevents neuron death and preserves synapses and even sustains learning and memory in a variety of Alzheimer’s disease mouse models.
Most recently in pilot clinical studies the team showed that 40 Hz light and sound stimulation was safe, successfully increased brain activity and connectivity and appeared to produce significant clinical benefits in a small cohort of human volunteers with early-stage Alzheimer’s disease.
Other groups have replicated and corroborated health benefits of 40 Hz sensory stimulation and an MIT spin-off company, Cognito Therapeutics, has launched stage III clinical trials of light and sound stimulation as an Alzheimer’s treatment.
The new study tested whether whole-body 40 Hz tactile stimulation produced meaningful benefits in two commonly used mouse models of Alzheimer’s neurodegeneration, the Tau P301S mouse, which recapitulates the disease’s tau pathology, and the CK-p25 mouse, which recapitulates the synapse loss and DNA damage seen in human disease.
The team focused its analyses in two areas of the brain: the primary somatosensory cortex (SSp), where tactile sensations are processed, and the primary motor cortex (MOp), where the brain produces movement commands for the body.
To produce the vibration stimulation, the researchers placed mouse cages over speakers playing 40 Hz sound, which vibrated the cages. Non-stimulated control mice were in cages interspersed in the same room so that all the mice heard the same 40 Hz sound. The differences measured between the stimulated and control mice were therefore made by the addition of tactile stimulation.
First the researchers confirmed that 40 Hz vibration made a difference in neural activity in the brains of healthy (i.e. non-Alzheimer’s) mice. As measured by expression of c-fos protein, activity increased two-fold in the SSp and more than 3-fold in the MOp, a statistically significant increase in the latter case.
Once the researchers knew that 40 Hz tactile stimulation could increase neural activity, they assessed the impact on disease in the two mouse models. To ensure both sexes were represented, the team used male P301S mice and female CK-p25 mice.
P301S mice stimulated for three weeks showed significant preservation of neurons compared to unstimulated controls in both brain regions. Stimulated mice also showed significant reductions in tau in the SSp by two measures, and exhibited similar trends in the MOp.
CK-p25 mice received six weeks of vibration stimulation. These mice showed higher levels of synaptic protein markers in both brain regions compared to unvibrated control mice. They also showed reduced levels of DNA damage.
Finally the team assessed the motor abilities of mice exposed to the vibration vs. not exposed. They found that both mouse models were able to stay on a rotating rod significantly longer. P301S mice also hung on to a wire mesh for significantly longer than control mice while CK-p25 mice showed a positive, though non-significant trend.
“The current study, along with our previous studies using visual or auditory GENUS demonstrates the possibility of using non-invasive sensory stimulation as a novel therapeutic strategy for ameliorating pathology and improving behavioral performance in neurodegenerative diseases,” the authors concluded.
More information: Ho-Jun Suk et al, Vibrotactile stimulation at gamma frequency mitigates pathology related to neurodegeneration and improves motor function, Frontiers in Aging Neuroscience (2023). DOI: 10.3389/fnagi.2023.1129510
Provided by Massachusetts Institute of Technology
Board-certified pathologist Dr. Ryan Cole: Spike protein in mRNA vaccines causes unusual clumping in the bloodstream
( Natural News ) Board-certified pathologist Dr. Ryan Cole talked about how the spike protein in Wuhan coronavirus (COVID-19) mRNA vaccines trigger unusual clumping in the bloodstream at a recent White Coat Summit.
“So, this is really unusual in clotting mechanisms,” Cole explained. “To see something like this and a protein that will do this in the absence of other things that are usually necessary for a clot is very unusual. And again, concerning.”
In relation to this, Dr. Resia Pretorius from South Africa showed that spike protein can cause proteins to clump together if you take platelets out of the blood.
Cole warned during his presentation that the mRNA vaccine’s spike protein is toxic , causing adverse health outcomes in the short term and also for future generation. The spike protein creates blood clots that impede the flow of blood to the heart and other organs vital to human health.
According to Cole, the mRNA vaccines caused a 200 percent hike in the rate of myocarditis. He also noted that Pfizer’s mRNA vaccine caused a 16 percent decline in fertility in rats. The pathologist shared that placentas delivered to his office contain spike proteins and are not properly sized in accordance with the age of gestation. Placenta is important in the development of the fetus during pregnancy.
The mRNA vaccines appear to have caused the placentas to calcify, likely as a result of the spike protein. Additional analysis revealed the placentas also have considerable inflammation and antibodies, essentially becoming a post-jab toxic stew that is not conducive to health or survival.
Additionally, whistleblower and renowned writer Naomi Wolf revealed that some midwives told her that the placentas of vaccinated mothers are shrunken and have a silver-gray color. These signs mean that the placentas are not big enough to sustain a normal baby. (Related: Naomi Wolf: No more normal placentas since COVID-19 vaccine rollout .)
“It’s an experiment, an emergency authorization, not approved. Humanity is the phase 3 trial . What is the risk for cancer after the shot? What is the risk of autoimmune disease after the shot? What is the risk of impairing fertility for a lifetime? We don’t know,” Cole said. “So why in the world are we really pushing forward at the pace rate we’re going without knowing these things? It’s a complete attack on science and a complete attack on us.” Spike proteins can also damage the brain
The spike proteins induced by the mRNA vaccines can also cause neurological damage . This was according to retired neurosurgeon Russell Blaylock.
“This [COVID-19] injection is an injection of artificial exosomes. The brain is one of the most complex things in the entire universe and people in the medical profession really don’t understand this injection. They don’t understand what it does to the neurological apparatus of the brain and spinal cord,” Blaylock said.
He explained that when there’s systemic inflammation or any kind of trauma occurs in the body, it produces inflammation and activation of the immune system. “This sends a signal to the brain within minutes and starts activating the microglia, which is the inflammatory, cytotoxic cell in the brain,” he said, adding that this is what would happen following the first dose of the COVID-19 injection.
As the second dose is injected months later, primed microglia become fully activated. It will then release all the toxic components.
“You get chronically activated microglia [in] overactivated state, and there’s a threefold higher inflammatory reaction than you’d normally get with microglial activation,” he said.
Check out PharmaceuticalFraud.com for more news on Big Pharma’s dangerous vaccines.
Watch the video below where cardiologist Dr. Peter McCollough tackled the things you need to know about spike proteins . 3 Things You Need To Know About Spike Proteins
This is a modal window.
No compatible source was found for this media.
This video is from the High Hopes channel on Brighteon.com . More related stories:
Vaccine damage from spike protein jabs is inducing wave of health carnage across the globe.
Study: These two simple nutritional supplements trigger spike protein UNFOLDING and may neutralize its harmful properties.
How to DEFEAT micro blood clots and block the spike protein by protecting the QUALITY of your blood. Sources include:
NaturalHealth365.com
Rumble.com
ChildrensHealthDefense.eu
Expose-News.com
Brighteon.com
Spike proteins in COVID-19 vaccines can cause BRAIN DAMAGE, neurosurgeon reveals

( Natural News ) Retired American neurosurgeon Russell Blaylock recently shared his shocking discovery that the spike proteins, induced by the Wuhan coronavirus (COVID-19) vaccine, can cause neurological damage .
“When there’s systemic inflammation or any kind of trauma occurs in the body, it produces inflammation and activation of the immune system. This sends a signal to the brain within minutes and starts activating the microglia, which is the inflammatory, cytotoxic cell in the brain,” Blaylock explained.
“When there is a stimulation of the immune system, the ramified microglia go to the primed microglia stage. The pseudopodia are retracted and it becomes a more rounded-looking cell. Inside the primed microglia, there is an intense upregulation of cytokine, chemokine and excitotoxin production, but they’re not released from the cell so there may be some minor immune reaction, but otherwise, there’s not much sign of a reaction.”
According to Blaylock, this happens after getting the first dose of the injection. He added that it is important to note that chemokines attract macrophages, or white blood cells, to the brain. A macrophage in the brain looks exactly like microglia and can also undergo priming.
As the second dose is injected months later, primed microglia become fully activated and will then release all the toxic components. “You get chronically activated microglia, [an] overactivated state and there’s a threefold higher inflammatory reaction than you’d normally get with microglial activation,” Blaylock said.
He further explained that when one gets an infection and recovers from it, the microglia shift from the activated state back to the ramified state. In the ramified state, instead of releasing harmful chemicals the microglia release neurotrophins that repair the damage done during the activated state. Studies: Spike protein alters neurological functions
Blaylock also cited several published papers that pointed to the harmful effects of the shots, particularly how spike protein can alter neurological functions. (Related: Ben Armstrong: There’s plenty of evidence that COVID-19 vaccines can damage the brain .)
In one study, researchers placed the spike protein in a cell and it formed abundant exosomes that not only contained the spike protein but also two microRNAs. Blaylock said: “The spike protein contained in the exosome was shown to cause a sharp decline in [an interferon regulating, self-controlled, system] IRE9 in microglia making them infinitely more destructive.”
Another study found that antibodies to only a fragment of the spike protein induced neuroinflammation and impaired episodic memory in mice. This, according to Blaylock, is also happening in humans who’ve had this injection – they’re having impaired memory .
“The brain has a special anti-inflammatory system built into it … and what this does is it down-regulates all the inflammatory responses,” Blaylock explained. “And so, what they found, is after immunization with the spike protein, it develops these immune reactions to the spike protein, just of that fragment, and there was a loss in episodic memory in those animals. The second injection is always worse.”
Another research on the mitochondrial effects showed that the spike protein increased microglia mitochondrial activity , producing extremely high levels of reactive oxygen and reactive nitrogen species. This makes the microglia more destructive than they normally would be.
The paper concluded that there was a 64 percent increase in the principal inflammatory component (inflammasome) in a cell. It also showed that the spike protein impaired the ability of the brain to tolerate inflammation and greatly enhanced the brain cytokine storm.
Visit VaccineInjuryNews.com to learn more about the harmful effects of the COVID-19 vaccines.
Dr. Robert Malone, mRNA technology inventor, talks about the worst side effects of the COVID-19 vaccines in the video below. The Covid Vaccine Side Effects Are Worse Than Expected
This is a modal window.
No compatible source was found for this media.
This video is from the High Hopes channel on Brighteon.com . More related stories:
WALKING DEAD? Do Covid vaccines poke holes in the blood-brain barrier and cause neurodegenerative disorders like Alzheimer’s and Parkinson’s?
mRNA spike proteins found in heart, brain of deceased “fully vaccinated” man .
Vaccine damage from spike protein jabs is inducing wave of health carnage across the globe . Sources include:
Expose-News.com
ScienceDirect.com
Link.Springer.com
Brighteon.com
Immune cells of the brain are not all the same: New research could open novel therapeutic pathways
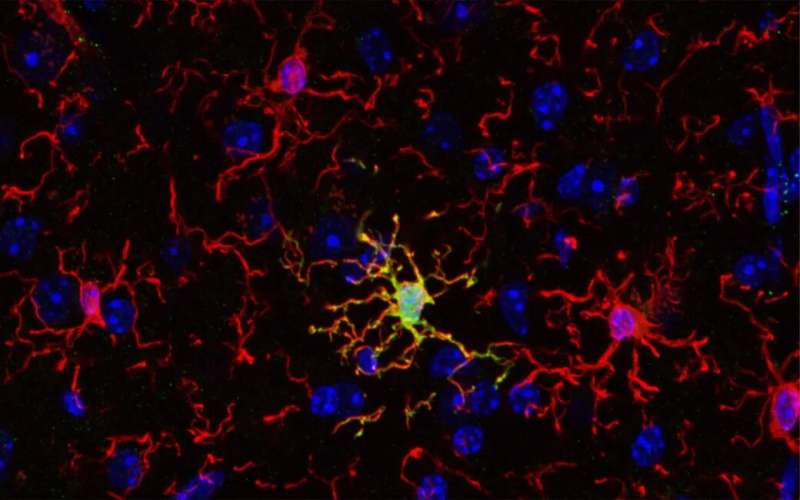
Microglia (in red) surround an ARG1+microglia cell (in yellow) that expresses the enzyme ARG1. Credit: Vassilis Stratoulias A recent study published in Nature Neuroscience indicates that, contrary to common belief, the immune cells of the brain, known as microglia, are not all the same. Researchers found that a unique microglial subset with unique features and function is important for establishing proper cognitive functions in mice. Evidence for such microglial subsets exists also for the human brain, opening exciting new possibilities for novel therapies.
An international collaboration led by researchers from University of Helsinki, Karolinska Institutet and University of Seville characterized ARG1 + microglia , a subset of microglial cells, that produces the enzyme called arginase-1 (ARG1). Using advanced imaging techniques, the team found that ARG1 + microglia are abundant during development and less prevalent in adult animals. Strikingly, these ARG1 + microglia are located in specific brain areas important for cognitive functions such as learning, thinking and memory.
“Cognition and memory are crucial components of what makes us human, and microglia are necessary for proper brain development and function. Cognitive decline is a common feature of neurodegenerative and psychiatric conditions like Alzheimer’s and Parkinson’s disease, schizophrenia and depression,” says Dr. Vassilis Stratoulias, senior researcher at the University of Helsinki and lead author of the study.
“Microglia are involved in virtually all brain pathologies, making them prime candidates for novel drug targets and innovative therapeutic approaches. Understanding the fundamental biology of these cells will be the way to produce new directions for drug development to treat currently untreatable diseases of the brain,” adds co-author, Dr. Mikko Airavaara from the University of Helsinki. Abnormal behavior reveals cognitive deficits
The researchers found that mice lacking the microglial protein ARG1 were less willing to explore new environments. This abnormal rodent behavior is linked to cognitive deficits and, more specifically, to impairments in the hippocampus, a part of the brain important for learning and memory.
The researchers could not identify any differences in the shape of ARG1 + microglia when compared to neighboring microglia that do not express ARG1, suggesting a reason why these microglia have not been studied before. Using a technology that allows for comparison of the RNA profiles between cell populations, ARG1 + microglia were found to be significantly different from neighboring ARG1-negative microglia on the molecular level.
Another key finding of the study is that female animals exhibited more pronounced behavioral and hippocampal impairments caused by ARG1 microglial deficiency. Sex bias is present in many diseases including Alzheimer’s disease. In fact, women are more likely than men to suffer from Alzheimer’s disease—the most common neurodegenerative disease in which cognitive abilities are severely compromised.
Microglia have emerged as key players in Alzheimer’s illness in recent years, making the findings of this study relevant to this disease. Although more research is needed to demonstrate a link between Alzheimer’s disease and a specific microglial subset, this study could provide a new prism under which we see Alzheimer’s disease in specific—and brain diseases in general—and open new therapeutic pathways.
Dr. Bertrand Joseph, professor at Karolinska Institutet and senior author, says, “In addition to offering better understanding of brain development and the contribution of microglial diversity to that, the study could provide new clues about how to manage neurodevelopmental disorders or neurodegenerative disorders presenting a cognitive component and often differences between males and females.”
Provided by University of Helsinki
Understanding the speed of brain communication
It often was thought that the speed of information transmitted among regions of the brain stabilized during early adolescence. A study in Nature Neuroscience by Mayo Clinic researchers and colleagues from the Netherlands found transmission speeds continue to increase into early adulthood.
Because problems such asanxiety, depression and bipolar disorders can emerge in late adolescence and early adulthood, a better understanding of brain development may help clinicians offer therapies to treat these disorders.
“A fundamental understanding of the developmental trajectory of brain circuitry may help identify sensitive periods of development when doctors could offer therapies to their patients,” says Dora Hermes, Ph.D., a Mayo Clinic biomedical engineer and senior author of the study.
Called the human connectome, the structural system of neural pathways in the brain or nervous system develops as people age. But how structural changes affect the speed of neuronal signaling has not been well described.
“Just as transit time for a truck would depend on the structure of the road, so does the transmission speed of signals among brain areas depend on the structure of neural pathways,” Dr. Hermes explains. “The human connectome matures during development and aging, and can be affected by disease. All these processes may affect the speed of information flow in the brain. “In the study, Dr. Hermes and colleagues stimulated pairs of electrodes with a brief electrical pulse to measure the time it took signals to travel among brain regions in 74 research participants between the ages of 4 and 51. The intracranial measurements were done in a small population of patients who had electrodes implanted for epilepsy monitoring at University Medical Center Utrecht, Netherlands.
The response delays in connected brain regions showed that transmission speeds in the human brain increase throughout childhood and even into early adulthood. They plateau around 30 to 40 years of age.
The team’s data indicate that adult transmission speeds were about two times faster compared to those typically found in children. Transmission speeds also were typically faster in 30- or 40-year-old subjects compared to teenagers.
Brain transmission speed is measured in milliseconds, a unit of time equal to one-thousandth of a second. For example, the researchers measured the neuronal speed of a 4-year-old patient at 45 milliseconds for a signal to travel from the frontal to parietal regions of the brain. In a 38-year-old patient, the same pathway was measured at 20 milliseconds. For comparison, the blink of an eye takes about 100 to 400 milliseconds.
The researchers are working to characterize electrical stimulation-driven connectivity in the human brain. One of the next steps is to better understand how transmission speeds change with neurological diseases. They are collaborating with pediatric neurosurgeons and neurologists to understand how diseases change transmission speeds compared to what would be considered within the normal range for a certain age group.
The research is supported by the National Institute of Mental Health of the National Institutes of Health (R01MH122258).
Study: Omega-3 fatty acids key to maintaining healthy brain function

( Natural News ) Aging can be a scary part of life because it comes with an increased risk of health problems, such as Alzheimer’s disease. Although aging is inevitable, you can prevent many diseases and keep your brain healthy by exercising regularly and eating a well-balanced diet to ensure proper nutrition.
According to a recent study published in the journal Neurology , having healthy levels of omega-3 fatty acids, which are essential nutrients found in abundance in fatty fish as well as some nuts and seeds, is key to maintaining healthy brain function as you age.
The study, conducted by researchers from the University of Texas Health Science Center at San Antonio , investigated the link between omega-3 fatty acid concentrations in red blood cells and brain structure as well as cognitive function in midlife. The researchers also looked at the difference in omega-3 fatty acid levels between carriers of the APOE-e4 gene – the strongest risk factor gene for Alzheimer’s disease – and non-carriers, and how this affected their cognitive abilities. (Related: Keeping an aging brain sharp and avoiding late-life depression required certain nutrients .)
Data gathered from more than 2,000 dementia- and stroke-free participants with a mean age of 46 years suggested that high omega-3 fatty acid concentrations are related to better brain structure and cognitive function.
In non-carriers of the APOE-e4 gene, a high omega-3 index or high levels of the omega-3, docosahexaenoic acid (DHA), was linked to larger hippocampal volumes, while in carriers of the gene, high levels of eicosapentaenoic acid (EPA), also an omega-3, was linked to better abstract reasoning.
The study is one of the first to identify the relationship between omega-3 fatty acid levels and brain health in a younger population.
“The new contribution here is that, even at younger ages, if you have a diet that includes some omega-3 fatty acids, you are already protecting your brain for most of the indicators of brain aging that we see at middle age,” Claudia Satizabal, the study’s lead author, said in a statement.
Omega-3 fatty acids can be obtained largely from dietary sources like oily fish, omega-3-fortified foods and nutritional supplements. In the brain, DHA is incorporated into neuronal and glial cell membranes. Both DHA and EPA are metabolized into bioactive molecules involved in neurogenesis, neurotransmission and inflammation resolution.
In older adults, observational studies suggest that higher DHA and EPA intake may be protective against Alzheimer’s. Meanwhile, a study published in the journal Alzheimer’s & Dementia linked pro-inflammatory diets , which are low in omega-3s, to smaller brain volumes and other markers of brain aging in the elderly. Omega fatty acids offer brain benefits
Omega-3, omega-6 and omega-9 fatty acids are all important fats you need to get from your diet. These healthy fats offer brain benefits, but it is important to get the right balance between them.
Nutritionists recommend eating at least two portions of fatty fish per week and using extra virgin olive oil for cooking to get a balanced ratio of omega fatty acids. They also advise reducing your consumption of vegetable oils to limit your intake of omega-6 fatty acids which, at high amounts, are said to be pro-inflammatory . Omega-3 fatty acids
Omega-3 fatty acids are polyunsaturated fats, a type of fat your body can’t make, which is why they are referred to as “essential fats,” or fats you need to get from foods. The three types of omega-3s that you need for a healthy brain are: Eicosapentaenoic acid (EPA), which is needed for the production of eicosanoids that help reduce inflammation. EPA has also been found to help reduce symptoms of depression .
Docosahexaenoic acid (DHA), which makes up about eight percent of your brain weight and is required for healthy brain development and function.
Alpha-linolenic acid (ALA), which is converted, albeit inefficiently, into EPA or DHA inside the body. ALA benefits the heart, immune system and nervous system.
According to studies, EPA and DHA function exclusively via cell membranes and generate metabolites that provide protection to brain cells . While DHA plays a role in cell membrane fluidity and the release of important brain chemicals, EPA influences behavior and mood.
In older adults, EPA and DHA supplementation is deemed necessary because of their significant effect on brain performance. As reported by a study published in the journal Nutrients , EPA can improve blood flow to the brain “globally and on demand in activated brain regions,” which benefits both mood and cognition.
Meanwhile, DHA is said to protect against memory decline by preventing inflammatory brain cell death – the pathological basis for Alzheimer’s disease. By ensuring adequate blood flow and preventing the inflammatory degeneration of brain cells, both EPA and DHA can help older adults maintain optimal brain performance.
EPA and DHA can be obtained directly from fatty fish like salmon, tuna, mackerel and sardines. Vegans and vegetarians can get plenty of ALA from foods like chia seeds, flaxseeds, walnuts, avocados and some leafy greens. To ensure quality and safety, avoid farmed salmon and always opt for organic produce. Alternatively, you can get omega-3s from fish oil and algal oil supplements . Omega-6 fatty acids
Omega-6 fatty acids are also essential polyunsaturated fats that mainly provide energy.
The most common omega-6 is linoleic acid, which the body can convert into longer omega-6 fats like arachidonic acid. Arachidonic acid also produces eicosanoids, but unlike the eicosanoids derived from EPA, they are more pro-inflammatory , which is why experts don’t recommend high intakes of linoleic acid.
On the other hand, research has found that increasing your intake of the omega-6, gamma-linolenic acid (GLA), can help reduce inflammation . A study published in the journal Pharmaceutical Biology also reported that GLA at low doses exerts an anti-aging effect on the brain. GLA protects against memory and learning impairments by inhibiting the production of advanced glycation end products (AGEs), a family of compounds believed to be responsible for the changes seen during aging as well as the development of many age-related morbidities.
However, unlike linoleic acid, GLA can only be obtained from a handful […]
Mike Adams interviews Robert F. Kennedy, Jr. – Border security, election integrity, America’s energy supply and healing America’s fractured society

( Natural News ) Robert F. Kennedy, Jr. is very approachable and extremely well informed about a vast spectrum of topics. He’s running for President of the United States on the Democrat ticket, and the Democrat establishment is going all-out to silence him by cancelling all debates and trying to sweep Joe Biden back into the White House.
You can learn more about RFK Jr’s run for the Oval Office (and join his email list) at www.Kennedy24.com
Although RFK and myself don’t agree on everything, I consider him to be a true American hero for his courage and perseverance in exposing the covid / vaccine / Fauci fraud.
He’s also a healer who, I believe, can help bring America back together from its current fractured status, where Big Government, Big Tech and the fake news media have worked incessantly to disrupt and destroy America from within.
I have publicly stated that I’m considering temporarily switching my party affiliate to Democrat solely to vote for RFK Jr. during the Democrat primary process, should the DNC even allow such a process to occur (never trust the establishment to follow the rules).
Interestingly, the DNC is trying to railroad RFK in much the same way the RNC is trying to railroad DJT. Both establishment parties despise real heroes like RFK or DJT , and they want them both to be silenced and shut out of the political process.
That’s why we must work hard to listen to these courageous men and share their message with others. My full interview with RFK Jr. is below, and I am publicly inviting Team Trump to join me for an interview about the Trump candidacy.
Here’s what I cover in today’s Brighteon Broadcast News, which includes the RFK interview:
– Robert F. Kennedy, Jr. discuss border security, election integrity, voter ID and more
– Covers the investigation and PROSECUTION of covid officials who committed fraud
– RFK achieves stunning CROSSOVER support from Republicans and conservatives
– Adams invites Trump team for an interview
– Mass homelessness in California getting WORSE as Biden’s economy crumbles
– Spike protein damages the BRAIN, explaining why vax booster proponents are so dumbed down
– California black groups demand $200 million in reparations payments to EACH black person
– Colorado bureaucrat wants to confiscate money from WHITE-owned businesses to subsidize BLACK businesses
– Interview with Paul Wittenberger, filmmaker and producer of “Fluoride – Poison on Tap” documentary
Brighteon: Brighteon.com/58f6b492-d708-4a4a-bfdb-d02a67505bcb
Rumble: Rumble.com/v2mvjc2-bbn-may-9-2023-robert-kennedys-vision-for-healing-a-fractured-america.html
Bitchute: Bitchute.com/video/5LpH5vZH0RNu/
Banned.Video: Banned.video/watch?id=645a6075b1e3f80b3295a01c
iTunes podcast: Healthrangerreport.com/brighteon-broadcast-news-may-9-2023-robert-kennedys-vision-for-healing-a-fractured-america Discover more interviews and podcasts each day at:
https://www.brighteon.com/channels/HRreport
Follow me on:
Brighteon.social: Brighteon.social/@HealthRanger (my breaking news gets posted here first)
Telegram: t.me/RealHealthRanger
Substack: HealthRanger.substack.com
Banned.video: Banned.video/channel/mike-adams
Truth Social: https://truthsocial.com/@healthranger
Twitter: @MikeAdamsHR
Gettr: GETTR.com/user/healthranger
Parler: Parler.com/user/HealthRanger Rumble: Rumble.com/c/HealthRangerReport BitChute: Bitchute.com/channel/9EB8glubb0Ns/ Clouthub: app.clouthub.com/#/users/u/naturalnews/posts Join the free NaturalNews.com email newsletter to stay alerted about breaking news each day.Download my current audio books — including Ghost World, Survival Nutrition, The Global Reset Survival Guide and The Contagious Mind — at: https://Audiobooks.NaturalNews.com/ Download my new audio book, “Resilient Prepping” at ResilientPrepping.com – it teaches you how to survive the total collapse of civilization and the loss of both the power grid and combustion engines.
Carrot carotenoids found to enhance and protect eye health

( Natural News ) Did you know that the retina of the eye is an extension of the human brain? And did you know that carrots, eggs, and leafy greens are loaded with nutrients that help protect and promote optimal eye health?
Of the 850 known carotenoids in the food supply, just three of them – lutein, zeaxanthin, and astaxanthin – are capable of crossing the blood-brain barrier. And it is these three that Dr. Joseph Mercola says are critical for producing macular pigment in your eyes.
It appears as though lutein in particular accumulates throughout the body, which draws from these stores to promote vision, cognitive function, and more. The others are important, too, and it is critical for you to understand that you must obtain these carotenoids from healthy foods because they do not occur naturally in the body.
Lutein has a protective, anti-inflammatory effect on the body. It is available both in supplement form as well as in dark leafy greens, avocados, egg yolks, tomatoes, and carrots, among other foods.
“Lutein concentrates in your macula – the part of your retina responsible for central vision,” Mercola writes. “Along with zeaxanthin and mesa-zeaxanthin (a metabolite of lutein), these three carotenoids form the retinal macular pigment, which not only is responsible for optimizing your visual performance but also serves as a biomarker for the risk of macular diseases.”
“Lutein is also found in the lens, where it helps protect against cataracts and other age-related eye diseases. Among carotenoids, lutein is the most efficient at filtering out blue light – the type that comes from cellphones, computers, tablets, and LED lights.”
(Related: Back in 2010, researchers found that fruit and vegetable carotenoids help to protect women against ovarian cancer.) Lutein deficiency linked to dementia, brain degradation
Blue light, in case you are unfamiliar with its detriments, is terrible for your eyes. It creates oxidative stress that can increase the risk of cataracts and other forms of macular degeneration and vision loss.
Lutein acts as a type of shield to protect your eyes against blue light damage, which is becoming even more of a problem as cities replace their orange-tinted street lights with blue light-emitting LEDs, which are white-looking, bright, and heavily straining on the eyes.
“As the peak wavelength of lutein’s absorption is around 460 nm which lies within the range of blue light, lutein can effectively reduce light-induced damage by absorbing 40 percent to 90 percent of incident blue light depending on its concentration,” reported a team of scientists out of Harvard Medical School and The University of Hong Kong , writing in the journal Nutrients .
“The outer plexiform layer of the fovea, where the majority of axons of rod and cone photoreceptor cells are located, is the retinal layer having the highest density of macular carotenoids including lutein. Hence the photoreceptors are protected against photo-oxidative damages from blue light.”
Another thing lutein does is protect the brain against dementia and other forms of degradation. It likewise suppresses the expression of vascular endothelial growth factor, or VEGF, which stimulates the formation of blood vessels that are capable of being upregulated in many types of cancerous tumors.
“As inflammation and abnormal angiogenesis in retinal vasculature are major pathogenic mechanisms of many ocular diseases, lutein’s functions in suppressing inflammatory response and VEGF expression make it effective in reducing the severity of these diseases,” the aforementioned research team further noted in their research.
The moral of the story, here, is to eat more carrots, dark leafy greens, pastured eggs, and other carotenoid-rich foods, which may help to protect your eyesight, not to mention the protective effects it offers in cancer prevention.
To keep up with the latest news about natural health and wellness, be sure to check out NaturalMedicine.news .
Sources for this article include:
TheEpochTimes.com
NaturalNews.com
You Can Improve Your Brain Health As You Age: Promising Research Tells Us How

he saying that “you can’t teach an old dog new tricks” can be (wrongfully) applied to humans, and with said application comes a lot of damaging—not to mention false—presumptions.
Researchers like Rachel Wu et al. , who recently published findings of two studies from the peer-reviewed journal Aging and Mental Health , challenge this stereotype with data. According to the research conducted in each of these studies, learning new things as you age is great for your health— especially when it comes to your brain.
The studies conducted with adults over the age of 55 found that those who engaged in learning multiple skills simultaneously, such as learning a new language, photography, and how to use an iPad, showed significant improvement in cognitive functioning. (The approach was to select activities that cater to diverse interests and hold practical value in daily life, such as language learning, art, and music composition.) The studies conducted with adults over the age of 55 found that those who engaged in learning multiple skills simultaneously (such as learning a new language, photography, and how to use an iPad) showed significant improvement in cognitive functioning. What’s more, the results of this research specifically showed that learning multiple new things at once led to higher cognitive scores both three, six, and 12 months after the study had taken place. (I.e. participants showed lasting improvement up to an entire year later.) The participants scored cognitively similar to undergraduate college students who similarly been absorbing high amounts of information simultaneously.
As mentioned in the study’s discussion, “[These] findings are atypical compared to prior research, although they were predicted based on our lifespan theoretical framework.” Meaning the results of much of the prior research on cognitive functioning over time tells a different story, generally emphasizing the ways in which a person’s brain health stays the same or diminishes the same or decline over time. How learning impacts brain health as you age
“Neuroplasticity, the capacity of the human brain to adapt and learn new skills, remains an essential factor in promoting cognitive resilience and maintaining overall cognitive well-being throughout one’s life,” says Elisabeth Bahr, OTD, MS, OTR, a doctor of occupational therapy. Learning new skills simultaneously creates new neural pathways in the brain, so it makes sense that it would engage more parts of your brain than going about life as usual.
According to Dr. Bahr, when you think about learning multiple things at once, you also have to use parts of your brain that structure your time, remember items that you need, plan where and when you need to be, organize your memory of each subject, and build upon that knowledge. “The study focused on executive function, which encompasses working memory and cognitive control, and verbal episodic memory, both of which can be impacted by the natural aging process,” she says. The fact that older adults scored cognitively similarly to undergraduate students is promising, especially when considering the cognitive challenges older folks can face with age.
Related Stories ‘I’m a Brain Health Coach, and This Is Why Gaming Is One… Dr. Bahr adds that there are a lot of encouraging details about this (albeit small) study, and that those interested in optimizing their brain functioning as they age by engaging in new activities might considering seeking guidance from an occupational therapist. “They’re professionals in helping people participate, regain, or strategize accommodations they might need to incorporate into their lifestyle after an injury or to cope with an existing disability,” she says. What to know before diving ‘head first’
Some folks may need to proceed with caution when it comes to pursuing rehabilitative activities or cognitively engaging activities. “Namely, it’s important to have clearance from a care provider if you or a loved one is thinking about engaging in something similar and there is any injury, traumatic brain injury, cognitive condition, or other extenuating circumstance that could worsen as a result of increased exertion of mind or body,” says Dr. Bahr. “Namely, it’s important to have clearance from a care provider if you or a loved one is thinking about engaging in something similar and there is any injury, traumatic brain injury, cognitive condition, or other extenuating circumstance that could worsen as a result of increased exertion of mind or body,” says Dr. Bahr. It can also be emotionally challenging to embark on a journey of learning new things—and frustration can get in the way of committing to a practice long-term. Getting a good night’s sleep after an intensive learning experience can help the brain commit the lesson or experience to memory better than without quality sleep. “It’s important to prioritize shuteye following intensive learning sessions, as this enhances memory retention and the consolidation of new information,” says Dr. Bahr.
Sometimes it can feel silly to get super into a new hobby, or a few—but this research suggests there’s merit to retaining curiosity and a desire to learn new things. This is your sign to consider taking that extra trip to the art supply store or finally trying out water aerobics…a healthy brain loves having fun, after all.
The Wellness Intel You Need—Without the BS You Don’t
A Healthy Gut Might Mean a Happy Brain
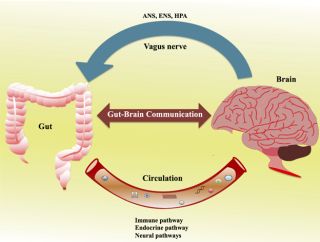
Cognitive and emotional centers in the brain are linked in two-way communication with our gut via the gut-brain axis (GBA).
Decreased diversity in the microbiome is associated with physical and psychological dysfunction.
Researchers found that the diversity of bacteria in the gut biome negatively correlated with using suppression as an emotion regulation strategy.
Suganya, Kanmani, and Byung-Soo Koo, CC BY 4.0 via Wikimedia Commons Have you ever had a “gut feeling,” an intuition based on something other than logic and reason, perhaps based on emotion? The phrase “gut feeling” became an idiomatic expression because most people report that they literally feel it in their gut. In fact, the cognitive and emotional centers in the brain are linked in two-way communication with our gut via what researchers call the “ gut-brain axis ” (GBA) (Carabotti et al., 2015). The figure in this post shows this GBA and how the brain and gut can influence one another.
Each of us has a unique microbiome , defined as the community of microorganisms that live either in us (our intestines) or on our skin. Some of these bacteria have beneficial effects on our bodies and minds. Others are associated with inflammation and disease. Both types of bacteria play an important role in our physical health and psychological well-being. We can influence the composition of the microbiome community through our diet and dietary supplements like “probiotics.”
A probiotic is a food or a supplement that contains bacteria and yeasts that help the body maintain a healthy and diverse gut microorganism community. The Gut Microbiome and Our Immune System
Decreased diversity in the microbiome is associated with physical and psychological dysfunction. Researchers estimate that 70 to 80 percent of our immune system resides in the gut, meaning that microorganisms that live in the gut are in contact with, and can influence, the immune system all the time. Rachelshoemaker, CC BY-SA 4.0 via Wikimedia Commons There is a link between gut dysbiosis (an imbalance in the composition of the bacteria or a lack of diversity in that community of microorganisms) and physical problems such as diabetes, colorectal cancer, Crohn’s disease, ulcerative colitis, and Celiac disease (Lozupone et al., 2012), as well as mental health problems like depression and anxiety (Shoubridge et al., 2022).
Research suggests that there might be a link between the well-known variability in response to antidepressant drug treatment with drugs like SSRIs (SSRI medication does not effectively treat as many as a third of depressed individuals) and the effects of these drugs on the community of bacteria in the gut. Researchers are now exploring the possibility that knowledge of the gut microbiome might help predict who will benefit from a specific drug treatment.
article continues after advertisement Gut Feelings and Emotional Coping Strategies
Ke et al. (2022) found a link between positive and negative emotions and the gut biome and an association between the diversity of the biome, and two cognitive coping strategies we might employ to help regulate our emotional responses.
These researchers asked a large sample of women (n = 206) who were already taking part in another, larger study to complete a series of surveys measuring their emotional responses, positive (feeling happy and hopeful about the future) and negative (feeling sad, hopeless, or lonely ). They also asked how the women coped with their emotional responses.
The researchers were particularly interested in how the women used cognitive reappraisal, a coping strategy involving changing one’s assessment of the emotion-provoking situation, or suppression (inhibiting behaviors) associated with emotion like laughing or crying or keeping information about one’s emotional responses from other people. Cognitive reappraisal is a healthy response, while suppression is generally maladaptive and is associated with increased inflammation levels and stress . The participants completed the surveys twice, one year apart. They also collected stool samples four times in the period between surveys.
They found that the diversity of bacteria in the gut biome negatively correlated with using suppression as an emotion regulation strategy. As suppression used as a coping strategy increased, gut biome diversity decreased. Happier, more positive emotions were associated with lower levels of bacteria previously reported to be linked with markers of ill health like increased inflammation and impaired insulin sensitivity. More negative emotions were associated with higher levels of these bacteria.
Our gut feelings may well provide important information about our psychological and physical health that can help doctors design effective treatment plans.
article continues after advertisement
References
Carabotti, M., Scirocco, A., Maselli, M.A., and Severi, C. (2015). The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology, 28 (2), 203- 209.
Lozupone, C.A., Stombaugh, J.I., Gordon, J.I., Jansson, J.K., and Knight, R. (2012). Diversity, stability and resilience of the human gut microbiota, Nature, 489 (7415), 229-230.
Shoubridge, A.P., Choo, J.M., Martin, A.M., Keating, D.J., Wong, M-L., Licinio, J., and Rogers, G.B. (2022). The gut microbiome and mental health: Advances in research and emerging priorities. Molecular Psychiatry , 27 , 1908-1919.
Ke, S., Guimond, A-J., Tworoger, S.S., Huang, T., Chan, A.T., Liu, Y-Y., and Kubzansky, L.D. (2023). Gut feelings: Associations of emotions and emotion regulation with the gut microbiome in women. Psychological Medicine , 10.1101/2022.05.26.493641



