Nature Knows and Psionic Success
God provides
Gut disorders and Alzheimer’s: Scientists find genetic link
Scientists have been investigating the link between Alzheimer’s disease and gut disorders. Gerville/Getty Images Studies have suggested that gastrointestinal health and Alzheimer’s disease (AD), the most common form of dementia worldwide , may be connected.
A recent Australian study has now identified a genetic link between Alzheimer’s disease and several gut disorders.
Many of the genes the scientists identified are involved in lipid metabolism, pointing to statins—which are used to control cholesterol—as a potential treatment for both AD and gut disorders.
The findings might also help doctors diagnose AD earlier, allowing better control of symptoms.
Alzheimer’s disease (AD) is the most common form of dementia in older adults. According to the World Health Organization, 60-70% of dementia cases may be caused by AD, the seventh leading cause of death in the United States.
AD is incurable, but there are treatments that may slow disease progression or alleviate the symptoms. Medications are more effective if they are started early, but diagnosis can take some time, during which the disease can progress without treatment.
A recent study developed an MRI-based machine learning system that may help with early diagnosis. Now, a finding from a team in Australia has suggested another possible route to earlier diagnosis and treatment of AD.
The researchers found genetic links between multiple gut disorders and AD, which, according to lead researcher Dr. Emmanuel Adewuyi “identifies new targets to investigate to potentially detect the disease earlier and develop new treatments for both types of conditions.”
The study, led by researchers from Edith Cowan University, Perth, Western Australia, is published in Communications Biology .
Hippocrates of Kos (c.460-377 BCE) is reputed to have said “All disease begins in the gut.” Increasingly, research is suggesting that the ancient Greek physician may have been right, at least in the case of several diseases.
Previous research studies on the gut-brain axis found that the gut microbiome may have an impact on the development of AD. In particular, some studies suggest that bacteria in the gut microbiota could influence the production of proinflammatory cytokines associated with AD pathogenesis.
A review of research studies on this topic concluded that “The convergence of gut-derived inflammatory response together with aging and poor diet in the elderly contribute to the pathogenesis of AD”.
The researchers of this new study set out to find out genetic associations underlying this observed association between the gut and AD. They analyzed genetic data from 15 large genome studies, most involving more than 400,000 people, containing information from AD and gut disorders.
They found certain genes were associated with having both AD and certain gut disorders—such as gastroesophageal reflux disease (GERD), peptic ulcer disease (PUD), gastritis-duodenitis, irritable bowel syndrome, and diverticulosis .
Although the researchers found significant genetic overlap and correlation between Alzheimer’s and some gastrointestinal disorders, they did not find evidence for a causal association.
The study’s senior author Prof. Simon Laws , the director of the Centre for Precision Health at Edith Cowan University, says that although the study did not find that gut disorders caused AD or vice versa, the findings were immensely valuable:
“These findings provide further evidence to support the concept of the ‘gut-brain’ axis, a two-way link between the brain’s cognitive and emotional centers, and the functioning of the intestines.”
Their study highlighted the genetic association of AD with not only gastrointestinal disorders but also the gut microbiome, reinforcing the findings of previous studies.
Commenting on the findings, the American Geriatrics Society said the study not only reveals a genetic link between Alzheimer’s disease and several gut-related disorders but that “the findings add to the evidence the gut-brain axis may play a role in the development of neurodegenerative disorders.”
The researchers also looked at the biological pathways in which these genes involved in both disorders acted, and found an overrepresentation of lipid-related and immune system-related pathways. Previous research has found a connection between the disruption of lipid homeostasis and AD .
This finding that involves lipid-related pathways, including cholesterol metabolism and transport, may suggest an association between abnormal cholesterol, gut disorders, and AD, as Dr. Adewuyi explained:
“Whilst further study is needed into the shared mechanisms between the conditions, there is evidence high cholesterol can transfer into the central nervous system, resulting in abnormal cholesterol metabolism in the brain.”
‘[E]levated cholesterol in the brain has been linked to brain degeneration and subsequent cognitive impairment,” he added.
Their findings suggest that drugs to control lipid homeostasis and inflammation may be potential treatments for AD. So, the authors suggest that cholesterol-lowering medications (statins) may prove useful in treating both conditions.
Dr. Mansi Shah , a licensed clinical integrative pharmacist, certified functional medicine practitioner, and CEO of the Functional Wellness Network, said the findings could help scientists develop new treatments.
“The study found that the risk of developing AD is increased in individuals with gastrointestinal disorders and that the two conditions share common genetic risk factors. The findings of this study may help to improve our understanding of the causes of AD and lead to the development of new treatment strategies,” she told MNT . The study states that while the findings do not indicate that AD and gastrointestinal tract disorders will always co-occur, it reveals a possible “shared biology.” “Thus, early detection of AD may benefit from probing impaired cognition in GIT disorders,” the authors conclude.Perhaps an awareness of this genetic association might lead physicians to assess people with gut disorders and cognitive impairment, leading to earlier diagnosis of AD in some.
Study finds no link between low serotonin and depression

For decades, people have been deluged with information suggesting that depression is caused by a “chemical imbalance” in the brain – namely an imbalance of a brain chemical called serotonin. And big pharma which has been pushing such information has been making tons of money from their prescribed antidepressants.
But, a recent research review from University College London shows that the evidence does not support it. And the antidepressants that they have pushed us to take may not be an effective way of treating depression.
Authors of a large systemic umbrella review, published in Molecular Psychiatry, argue that there is no support for this hypothesis. They have also questioned the high prescribing rates of antidepressants. Our new review is the first to systematic overview of all the main areas of research and concludes there is no evidence of a link between low serotonin and depression https://t.co/fujIfAtD91 THREAD — Dr Joanna Moncrieff (@joannamoncrieff) July 20, 2022 Here’s what the study’s lead author Dr. Joanna Moncrieff said, according to The Guardian: “Many people take antidepressants because they have been led to believe their depression has a biochemical cause, but this new research suggests this belief is not grounded in evidence. It is always difficult to prove a negative, but I think we can safely say that after a vast amount of research conducted over several decades, there is no convincing evidence that depression is caused by serotonin abnormalities, particularly by lower levels or reduced activity of serotonin.” The research team examined 17 studies, including 12 systemic reviews and meta-analyses, and found “no consistent evidence of there being an association between serotonin and depression and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.”
The Daily Caller report explained it further:
The evidence also showed that long-term antidepressant use may be associated with lowering serotonin levels. Moncrieff argued the public should be informed that antidepressants may not be the ideal way to treat depression because of the side effects and withdrawal symptoms associated with the medications. Not all experts agree with the conclusion. “Antidepressants are an effective, Nice-recommended treatment for depression that can also be prescribed for a range of physical and mental health conditions,” a spokesperson for the Royal College of Psychiatrists said. “We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their GP.”
Antidepressants are a big ticket item for pharmaceutical companies, and their use has skyrocketed in the U.S. since 1999, according to the Berkeley Political Review. One in six Americans is on an antidepressant of some kind, NBC News reported .
The global antidepressant market was worth more than $26 billion in 2020, according to Business Wire.
Even if the serotonin hypothesis isn’t true, that doesn’t mean antidepressants that target brain chemistry aren’t an effective way to treat depression, according to Dr. Michael Bloomfield, a University College London psychiatrist who was not involved in the research. “Many of us know that taking paracetamol can be helpful for headaches, and I don’t think anyone believes that headaches are caused by not enough paracetamol in the brain,” he told The Guardian. “The same logic applies to depression and medicines used to treat depression.”
Antidepressants can cause side effects and some may cause withdrawal symptoms when stopped, Moncrieff said. The authors recommended that withdrawal from antidepressants should be done under the supervision of a clinician.
Analysis: Big Pharma jacked up drug prices 1,186 times in 2022 alone
( Natural News ) An analysis done by an advocacy group found that pharmaceutical companies have jacked up drug prices by over a thousand times in 2022 alone.
Patients For Affordable Drugs (PFAD) penned the July 20 report , which revealed that the U.S. drug industry raised the prices of various drugs a combined 1,186 times this year. P4AD seeks to curb the skyrocketing cost of prescription drugs.
Between June 24 and July 5, drug firms increased the prices of 133 products – with a median price increase of five percent. PFAD added that for the month of July alone, 64 drug companies increased the prices of their products.
Drug manufacturer Amgen has increased the price of its autoimmune disease drug Enbrel twice this year, for a total increase of 9.4 percent. Since acquiring the rights for the drug in 2002, the California-based company had increased Enbrel’s price 27 times – bringing its monthly cost to $5,554.96 in 2020. The drug’s price swelled by 457 percent between 2002 and 2020.
Chicago resident Kip Burgess, who takes Enbrel for his psoriatic arthritis, said: “No one should have to worry about how they will afford the medications they need to live.” He told P4AD that he does not experience any symptoms and can live his life fully when taking Enbrel.
GSK also increased the price of its lupus drug Benlysta four times since the pandemic, bringing its monthly price to $4,282. Thanks to 7.4 percent of total price hikes this year, more than $3,500 was added to Benlysta’s price tag.
The higher price of Benlysta spelled bad news for Morgantown, West Virginia resident Ashley Suder.
“Without this drug, my immune system attacks my healthy tissue, resulting in painful inflammation that damages my skin, joints, blood vessels and brain,” she told PFAD. “I’ve had to spend my entire paycheck on my medication and, with the price increasing again, I worry about how I’ll make ends meet while still affording my drugs.” Pfizer jacked up drug prices despite record profits
Pfizer also raised prices for 23 of its prescription drugs in July alone. The New York-based drugmaker already posted record profits in 2021, thanks to its mRNA Wuhan coronavirus (COVID-19) vaccine made in partnership with German company BioNTech. (Related: PLAGUE PROFITS: Pfizer executive admits the company wants to profit off vaccines and will soon raise prices. )
According to a February report from the Guardian , Pfizer made almost $37 billion in sales from the COVID-19 vaccine in 2021. Contracts for the vaccine contributed to the firm’s $81.3 billion overall revenue for that year. Pfizer’s projected revenue this year is between $98 billion and $102 billion.
The leukemia treatment Besponsa was among the drugs included in Pfizer’s price hikes. Since the start of the COVID-19 pandemic, the company increased its price four times that a single vial of Besponsa now retails at $21,056.
“Americans are struggling with record inflation and the continued challenges of [the] pandemic. Yet Big Pharma continues to raise drug prices with no regard for [people’s] health and financial well-being,” said PFAD Founder David Mitchell. “We must put an end to drug corporations’ unfettered ability to dictate prices at the expense of patients.”
Mitchell is an apt representative for those campaigning for lower drug prices, as he himself suffers from incurable blood cancer. The drugs he needs to address his condition forces him to shell out more than $900,000 annually.
A report by Russia Today outlined the blatant greed of Big Pharma in a July 20 piece: “The US has the highest-priced healthcare in the world, despite yielding worse health outcomes than any other developed nation.” It also pointed out that “the life expectancy of Americans is lower than all of their industrialized peers, even as their doctors are better-paid than doctors in other developed countries.”
Visit BigPharmaNews.com for more stories about the greed of drug companies.
Watch California Rep. Katie Porter below rebuking a Big Pharma executive for putting profits over health. No compatible source was found for this media. More related stories:
Big Pharma BOOM: Drug prices SOARED in 2017 and you’ll never guess who’s getting YOUR medicine rebates.
Generic drug companies conspired to fix drug prices and rake in billions by cheating customers, lawsuit says.
Bill to lower drug prices blocked by senator who received major donations from Big Pharma.
Sources include:
RT.com
Video games promote brain activity and decision making – healing practice

Effects of video games on the brain
Video games aren’t just a teen hobby anymore. Meanwhile, almost all age groups enjoy versatile games. From a health perspective, however, video games tend to get a bad rap. Wrongly? An ongoing study highlights the positive aspects of regular gaming on PC, XBox, Playstation, Switch and Co.
In a recent study, researchers from Georgia State University (USA) found that people who regularly play video games have better sensorimotor decision-making abilities and increased activity in key regions of the brain compared to to non-players. The results were recently published in the specialist journal “Neuroimage”. Health effects of video games are unclear
“Video games are played more than three hours a week by the overwhelming majority of our teenagers, but the positive effects on decision-making and the brain are not well understood,” says the study leader and professor of neurology, Mukesh Dhamala.
According to him, ongoing research is providing the first answers to these questions. “Playing video games can be used effectively for training – for example, to train decision-making skills and for therapeutic interventions,” the brain expert points out. course of the study
The research project at Georgia State University involved 47 young adults. 28 of the participants regularly played video games, 19 played rarely or not at all. All subjects underwent a special test.
They had to track a dot using mirrors and decide by pressing a button whether the dot would move left, right, or not at all. During this time, the participants’ brain activity was measured. Study results
People who regularly play video games were able to respond faster and more accurately in this test than participants who did not play games. This was also confirmed by brain scan results, which showed higher activity in certain brain regions in the players.
“These results indicate that playing video games can enhance several subprocesses of sensation, perception, and attribution to action in order to increase decision-making capacity,” summarize the study authors. Video games as decision-making training
For the first time, the results provide insight into the possible effects of regular computer game play on the brain and how the brain is trained while playing.
According to the scientists involved, the results suggest that video games could be a useful tool for training perceptual decisions, both in terms of speed and accuracy. (vb) Author and source information
Show now
This text corresponds to the specifications of the specialized medical literature, medical guidelines and current studies and has been verified by health professionals.
Author:
Graduate editor (FH) Volker Blasek
Sources:
Georgia State University: Video Game Players Show Improved Brain Activity, Decision-Making Skill (Published 7/11/2022), news.gsu.edu Timothy Jordana, Mukesh Dhamala, et al. : Video game players improved their decision-making abilities and enhanced brain activities; in: Neuroimage (2022), sciencedirect.com
Important note:
This article contains general advice only and should not be used for self-diagnosis or treatment. It cannot substitute a visit to the doctor.
Feeling Foggy? What Is Brain Fog and How Can You Get Rid of It?

It’s 9:00 a.m., and you’re at your desk. You’ve got a ton of work to do, but you just can’t seem to focus on it. Your eyesight’s fine — you can see the words on the page or screen in front of you, but for some reason they’re just… not going in .
You’re not sick, hungover, or preoccupied, and you got plenty of sleep last night — so you know it’s not that. It isn’t just a case of the Mondays either, because — well, it’s Tuesday.
Yup, you’ve got brain fog. What is Brain Fog?
Brain fog isn’t a medical condition, but rather a generalized feeling of being unfocused, spaced out, and lacking mental clarity. It can be caused by any number of underlying health issues — including long COVID [1] — so you should definitely see a doctor if it’s become a chronic problem for you.
That said, we all get it from time to time, and it’s usually nothing to worry about. But that doesn’t make it any less uncomfortable and inconvenient, especially when you’ve got stuff to do that requires your full attention. 5 Ways to Fight the Fog
If your doctor has ruled out any serious health concerns, it’s likely your brain just isn’t functioning at the peak of its performance capacity. Fortunately, there are a few things that can help you achieve the mental tune-up you need. (Consult your doctor before adopting an exercise regimen or taking a dietary supplement.) Here are five of them: Exercise
Take a hike, buddy!
There’s nothing like fresh air and exercise — even a quick stroll through the park — to blow away the cobwebs. Studies have shown that physical activity improves cognitive function by reducing cortisol (stress hormone) levels, and that physical fitness promotes growth in the hippocampus — the part of the brain responsible for learning and memory. [2]
But we don’t need studies to tell us what we already know through common sense. Your brain is an organ like any other; it needs a good supply of oxygenated blood to be at the top of its game, and a brisk walk in nature is a tried-and-true way to fill your lungs with clean air and get your heart pumping.
But if that doesn’t help… Caffeine
…there’s always coffee.
“I can’t get anything done until I’ve had my morning coffee!” We’ve all heard it — and probably said it — at some point in our working lives. And there’s a reason for that; the caffeine in a good ol’ cup of joe (between 40 and 150mg per serving) is a stimulant that temporarily improves lower cognitive functions like attention, vigilance, and reaction time. Around 80 percent of adult Americans depend on it to get through their daily workload. [3]
But caffeine is only a quick fix for mental underperformance, and too much of it can have the opposite effect, making you jittery and distracted. L-Theanine
If you’re not a fan of coffee, consider a refreshing cup of green tea.
Green tea is caffeinated too, but much less so (about 33mg per serving). Rich in antioxidants, it also contains a high concentration (~25mg) of L-theanine — an amino acid with proven neuroenhancement benefits.
In a recent Japanese clinical trial, a single dose of L-theanine was found not only to increase the subjects’ reaction time, but to improve their scores on memory tests as well. [4] It’s also a neuroprotective agent — meaning that it fortifies the brain against degeneration — according to a study published in the Journal of Neuroscience , whose authors suggested that L-theanine could one day be harnessed as a therapy for substance abuse-related brain damage. [5] Mangiferin
The mango leaf extract mangiferin was all the rage when it hit the supplements market under the trade name Zynamite back in 2018 — and rightly so.
Touted by the manufacturer, Nektium, as a caffeine-free nootropic that boosts cognition, mental performance, and reactivity, as well as reducing fatigue, [6] mangiferin has been dubbed “a natural miracle” by an international team of scientists who studied its many health benefits, which may even include the potential to prevent brain cancer. [7] Pending further clinical investigation, medical researchers think mangiferin shows promise as an effective treatment for neurodegenerative disorders like Alzheimer’s and Parkinson’s. [8]
Unlike caffeine, mangiferin has no known cardiovascular side effects, so it shouldn’t give you the jitters you get from drinking too much coffee. [9] Salidroside
Salidroside is another plant-derived nootropic — a bioactive compound found in the adaptogenic herb Rhodiola rosea (roseroot). This, too, is being talked about as a side-effect-free candidate for neurological rehabilitation therapy. [10]
A 2009 scientific review of salidroside-rich roseroot extract SHR-5 by the Swedish Herbal Institute concluded that there was “strong scientific evidence” that SHR-5 “improved attention, cognitive function and mental performance” in human subjects, [11] while pure salidroside’s powerful neuroprotective effects are well documented in preclinical tests on rodents. [12]
Many commercially-available roseroot supplements contain only trace amounts of salidroside, however, so be sure to check that it’s specifically mentioned on the label. Concluding Advice
When it comes to brain fog, most people haven’t the foggiest idea what to do about it. Fortunately, having read this blog, you’re not one of them!
Of all the fog-fighting methods listed above, you should definitely try getting more exercise first. But if you’re still battling with brain fog, and your doctor gives the go-ahead, natural nootropics like L-theanine, mangiferin, and salidroside are showing real promise as potent brain-boosters that can help improve mental clarity when you need it most.
References:
> health.harvard.edu/blog/brain-fog-memory-and-attention-after-covid-19-202203172707 ncbi.nlm.nih.gov/pmc/articles/PMC6234274/ sciencedirect.com/science/article/pii/S0149763416300690 liebertpub.com/doi/10.1089/jmf.2020.4803 jneurosci.org/content/41/4/739.long nektium.com/zynamite/ lipidworld.biomedcentral.com/articles/10.1186/s12944-017-0449-y sciencedirect.com/science/article/abs/pii/S1043661819304360 sciencedirect.com/science/article/pii/S0378874119345416 dovepress.com/pharmacological-activities-mechanisms-of-action-and-safety-of-salidros-peer-reviewed-fulltext-article-DDDT doi.org/10.2174/157488409789375311 link.springer.com/article/10.1007/s10571-020-00801-w
Alzheimer’s breakthrough: Genetic link to gut disorders confirmed
People with gut disorders may be at greater risk of developing Alzheimer’s Disease (AD).
A world-first Edith Cowan University (ECU) study has confirmed the link between the two, which could lead to earlier detection and new potential treatments.
AD destroys memory and thinking ability and is the most prevalent form of dementia.
It has no known curative treatments and is expected to affect more than 82 million people and cost US$2 trillion by 2030.
Previous observational studies have suggested a relationship between AD and gastrointestinal tract disorders, but what underpins these relationships had been unclear — until now.
ECU’s Centre for Precision Health has now provided new insights into these relationships by confirming a genetic link between AD and multiple gut disorders.
The study analysed large sets of genetic data from AD and several gut-disorder studies — each of about 400,000 people.
Research lead Dr Emmanuel Adewuyi said it was the first comprehensive assessment of the genetic relationship between AD and multiple gut disorders.
The team discovered people with AD and gut disorders have genes in common — which is important for many reasons.
“The study provides a novel insight into the genetics behind the observed co-occurrence of AD and gut disorders,” Dr Adewuyi said.
“This improves our understanding of the causes of these conditions and identifies new targets to investigate to potentially detect the disease earlier and develop new treatments for both types of conditions.”
Centre for Precision Health director and study supervisor Professor Simon Laws said whilst the study didn’t conclude gut disorders cause AD or vice versa, the results are immensely valuable.
“These findings provide further evidence to support the concept of the ‘gut-brain’ axis, a two-way link between the brain’s cognitive and emotional centres, and the functioning of the intestines,” Professor Laws said.
Is cholesterol a key?
When researchers conducted further analysis into the shared genetics, they found other important links between AD and gut disorders — such as the role cholesterol may play.
Dr Adewuyi said abnormal levels of cholesterol were shown to be a risk for both AD and gut disorders.
“Looking at the genetic and biological characteristics common to AD and these gut disorders suggests a strong role for lipids metabolism, the immune system, and cholesterol-lowering medications,” he said.
“Whilst further study is needed into the shared mechanisms between the conditions, there is evidence high cholesterol can transfer into the central nervous system, resulting in abnormal cholesterol metabolism in the brain.
“There is also evidence suggesting abnormal blood lipids may be caused or made worse by gut bacteria (H.pylori), all of which support the potential roles of abnormal lipids in AD and gut disorders.
“For example, elevated cholesterol in the brain has been linked to brain degeneration and subsequent cognitive impairment.”
Hope for the future
The cholesterol link could prove vital in treating AD in the future.
While there are currently no known curative treatments, the study’s findings suggest cholesterol lowering medications (statins) could be therapeutically beneficial in treating both AD and gut disorders.
“Evidence indicates statins have properties which help reduce inflammation, modulate immunity and protect the gut,” Dr Adewuyi said.
However, he said there was a need for more studies and patients needed to be assessed individually to judge whether they would benefit from statin use.
The research also indicated diet could play a part in treating and preventing AD and gut disorders.
Music May Alter Connectivity in the Brain

Research from Psyche Loui, director of Northeastern’s Music Imaging and Neural Dynamics lab, provides insight into how music changes the connective pathways in the brain. Credit: Matthew Modoono/Northeastern University When Paul McCartney wrote “Get Back,” he never would have predicted how useful or relevant the song would become for music therapists.
The song’s refrain—“Get back to where you once belonged”—might as well be a therapist encouraging a dementia patient to recall a distant memory. In new research, Psyche Loui , an associate professor of music, is attempting to do exactly that.
Published in Nature’s Scientific Reports , Loui found that for older adults who listened to some of their favorite music, including The Beatles, connectivity in the brain increased. Specifically, Loui—and her multi-disciplinary team of music therapists, neurologists and geriatric psychiatrists—discovered that music bridged the gap between the brain’s auditory system and reward system, the area that governs motivation.
“There’s something about music that is this functional connectivity between the auditory and reward system, and that’s why music is so special and able to tap into these seemingly very general cognitive functions that are suddenly very engaged in folks with dementia who are hearing music,” said Loui, who directs the Music Imaging and Neural Dynamics Lab.
The original idea for this research came out of Loui’s own experiences playing music in nursing homes. She recalled how people who couldn’t finish a sentence or thought would suddenly harmonize and sing along to a song she was playing.
“[Music] seems to engage the brain in this way that’s different than everything else,” Loui said.
The researchers had a group of older adults between the ages of 54 and 89 from the Boston area listen to a playlist for an hour every day for eight weeks and journal about their response to the music afterward. Loui and the team would scan the participants’ brains before and after listening in order to measure their neurological response.
Playlists were highly personalized and featured a combination of the participants’ self-selected songs, which ranged from The Beatles to Bruce Springsteen, and a preselected mix of classical pieces, pop and rock songs and new compositions created by Hubert Ho, an associate teaching professor of music at Northeastern. Participants would then rate each song based on how much they liked it and how familiar it was.
“The most important lesson that we learned from the music therapist was that there is no one-size-fits-all for what kind of music works best,” Loui said.
What the researchers found was striking: Music was essentially creating an auditory channel directly to the medial prefrontal cortex, the brain’s reward center. Notably, the medial prefrontal cortex “is one of the areas to lose its activity and functional connectivity in aging adults, especially in folks with dementia,” Loui said.
Music that was both familiar and well-liked tended to activate the auditory and reward areas more. However, the music that participants selected themselves provided an even stronger connection between these two areas of the brain.
“This might be the central mechanism for what changes happen in the brain when you’re listening to music and when you’re consistently, persistently and mindfully listening to music over the course of an intervention,” Loui said.
Loui hopes this study, which is one of the first to document neurological changes from extended exposure to music-based intervention, could have a significant impact in a field that has quickly risen in prominence. The National Institute of Health is currently pushing initiatives around music therapy, and AARP’s Global Council on Brain Health recently convened a panel, which Loui served on, to examine evidence of music’s influence on brain health. The panel ultimately formed recommendations for how people ages 50 and over can incorporate music into their lives to promote mental wellness.
Music’s ability to calm older adults and people with mental illness is well-documented, Loui said; but what’s less known is how and to what extent music can help improve memory, cognition and executive function.
“That’s something we’re working on right now, and I think there might be something about the fact that music is an art that unfolds over time,” Loui said. “For example, you’re listening for a beat and then you can tap your toes to the beat. That kind of process engages the brain’s reward systems and cognitive systems in ways that might be beneficial for long-term cognitive functions.”
Moving forward, Loui hopes to extend her study to older adults who have cognitive and neurodegenerative disorders, people who might benefit even more from the effects of music therapy.
“We’re trying to design these new therapies to take advantage of the rhythmic properties of music and the rhythmic properties of the brain,” Loui said, “and the tuning of neural populations towards the acoustic signals of the music might be useful for improving cognition.”
Reference : Quinci MA, Belden A, Goutama V, et al. Longitudinal changes in auditory and reward systems following receptive music-based intervention in older adults. Sci Rep . 2022;12(1):11517. doi: 10.1038/s41598-022-15687-5
This article has been republished from the following materials . Note: material may have been edited for length and content. For further information, please contact the cited source.
Advertisement
Doctrine of Signatures: Probability or Providence?
Nature is constantly giving a silent and unmistakable witness to the human race. We live in an age of electron microscopes and mass spectrometry devices. But before this, humans had to figure out what foods were best to eat by using our senses. The art of botanical discovery led humans to discover that a food’s healing properties corresponded to the body parts they resemble or to the condition they treated. This led to the “signatures” found in the common names of healing plants. (1, 2) The Doctrine of Signatures
English Walnut
The walnut is a uniquely shaped nut, and what does it resemble? Of course, the brain! You can see the left and right hemisphere, upper and lower cerebrum, and the pronounced folds that mimic the neocortex! Didn’t remember? Not to worry, but perhaps you need to eat more walnuts because they are the richest nut source of Omega-3 ALA. This essential fatty acid helps improve brain health, including memory and the production of over 3 dozen neurotransmitters. (1) They also provide a host of neuro-protective nutrients such as gallic acid, vitamin E isomers, melatonin, folate, and polyphenols. Horsetail
As the name so eloquently suggests, this herb resembles a horse’s tail. Think of the beautiful flowing tail of a healthy horse. Horsetail is exceptionally high in silica (second only to bamboo) which is essential for promoting healthy hair, skin, and nails. And silica also keeps our bones pliable, not brittle, and is an important ingredient in the fight against osteoporosis. (2) The stems also have a practical use as a scorching pad, like some cultures also do with horses’ tails to swat flies. Avocado
Avocado is certainly a fatty fruit and at first glance brings to mind the pregnant mother’s womb with her fetus. Interestingly, research reveals that eating just one avocado a week, a woman can significantly improve her health. Among other things, avocados aid hormone balance and detoxification, protect the cervix from cancer, and even promote healthy weight loss. Interestingly, it takes a full 9 months for the blossom to fully ripen into the soft fruit! (3) Carrot
Yes, the carrot is a familiar veggie and a staple in many cultural dishes. What could the carrot represent? Here’s a hint: cut it in half and look at the cross-section. What do you see? Yes! The cross section of the carrot looks similar to the pupil, iris and radiating lines of the human eye. Coincidentally, it’s packed with loads of pro-vitamin A (beta-carotene) and increases the blood flow to the eyes. Eat your carrots! It’s easy with Roasted Carrot Spread or Carrot Cake Breakfast Bowl .
Chinese Ginseng
This “king of the herbs” is also called panax ginseng. Panax comes from the Latin root word “cure-all” or “panacea,” Indeed, ginseng has become world-renowned for its powerful adaptogenic and energizing effects on the entire human body. Is it any wonder then that the root itself has a homomorphic appeal– head, legs, arms and all? As such, ginseng has been used for thousands of years as a tonic to rejuvenate every organ. (4) Amazingly, this includes the nervous, skeletal, circulatory, endocrine and genito-urinary systems. Pomegranates
The microscope reveals many minute details that the human eye can’t discern, such as the connective tissues of the body. Clearly, they resemble the flat and tightly-packed fleshy seeds of the pomegranate fruit. Amazingly, the astringent effects that pomegranate juice has in the mouth is felt in every artery in the body. Studies show that after several months of drinking the juice, atherosclerotic plaque in the carotid arteries begins to reverse! (5) Kidney Bean
Obviously, the name is a dead giveaway. Clearly reflecting the Doctrine of Signatures, kidney beans look like little kidneys! Supporting the “signatures” theory, modern research shows that these legumes help to reduce blood cholesterol and support overall kidney function. (6) Careful, though! Beans should never be eaten raw. Mucuna Pruriens
Though mucuna is a well-known herb, you may not have heard its common name: velvet bean. Mucuna graces the Ayurvedic tradition, where people have used it for centuries as an agent for health. How does the doctrine of signatures apply here? Well, compare mucuna to the human spinal cord. They look very similar! In fact, you’ll see that this bean resembles the spine even down to the very spinal nerves of the central nervous system.
When crushed into a powder, the seed pod works as a natural anti-stimulant to help calm anxiety, lift the mood, and restore proper dopamine levels in the brain. In fact, recent research validates this practice, as it is proven to help with Parkinson’s Disease patients due to its exceptionally high levels of L-Dopa and ability to stimulate Human Growth Hormone. (7) Tomato
Last but not least, we have the tomato plant! The bright red tomato has the shape and color of the blood-filled heart muscle. Additionally, it has four chambers as does the atriums and ventricles of the human heart! Botanically speaking, the tomato plant is a fruit and has the phytochemical called lycopene, which aids in supporting the heart. (8) Can You Find More Signatures?
So now, have we whetted your appetite — or maybe your curiosity? Be creative and put together a platter of food for all your human parts.
What other common, or not so common, foods and herbs can you think of that correspond to the human body? Investigation is key! Let us know what you find in the comments section below!
Quercetin can protect you from the harmful effects of pesticides
( Natural News ) More than a thousand different chemicals are used as pesticides in the United States. These harmful pesticides are used on at least 20,000 different products. Unfortunately, pesticides are also often used in homes, gardens, lawns, parks and schools.
Studies have confirmed that excessive and prolonged exposure to pesticides is linked to cancer, endocrine disorders, respiratory problems, birth defects and organ failure. Pesticide exposure is also associated with neurodegenerative conditions like Alzheimer’s disease and Parkinson’s disease.
Fortunately, a beneficial plant pigment called quercetin can help naturally negate the damage from toxic pesticides and protect against their adverse effects. Organophosphate pesticides threaten human health
According to researchers, organophosphate pesticides are very harmful. They warned that pregnant women, the elderly, children and those with compromised immune systems are most at risk from exposure.
Studies have found that prenatal or early childhood exposure to organophosphates also increased the risk of neurological damage and learning disorders, such as attention deficit hyperactivity disorder (ADHD).
This is not surprising because organophosphate pesticides were originally developed for use in biological warfare. The pesticide targets the nervous system just like nerve gas.
Organophosphates inhibit cholinesterase, an enzyme that breaks down the neurotransmitter acetylcholine, so acetylcholine builds up in the nerves. This buildup makes it hard to breathe, which can then cause death.
Organophosphates are also harmful to wildlife. According to the Environmental Protection Agency (EPA), organophosphate can also harm bees. Pesticides may cause neurodegenerative disease
Exposure to pesticides is linked to many adverse effects, such as altered moods, decreased vision, impaired motor skills, memory loss and poor coordination.
Recent studies also suggest a link between chronic pesticide exposure and the increased prevalence of dementia.
To illustrate, dichlorodiphenyltrichloroethane (DDT), an insecticide banned in the U.S. since 1972, can still be ingested through imported foods. You can also be exposed to DDT if you live near farmlands where DDT was previously sprayed.
People with Alzheimer’s have been shown to have 3.8 times more DDT metabolites in their blood than those without Alzheimer’s disease.
Additionally, 76 percent of those with Parkinson’s were found to have detectable amounts of the pesticide beta-hexachlorocyclohexane (beta-HCH) in their blood compared to 40 percent of non-Parkinson’s patients. The link between beta-HCH and Parkinson’s is so pronounced that researchers used the pesticide to reliably predict a diagnosis. Quercetin activates natural defense systems
Quercetin is a flavonoid and a powerful antioxidant that can be found naturally in plants. The flavonoid also helps protect plants against disease, temperature extremes and toxins.
Scientists believe that quercetin can also offer benefits for humans and they have found that quercetin shows great promise in helping suppress the negative side effects of exposure to pesticides .
Quercetin protects through different mechanisms. The flavonoid preserves the metabolism of energy, fatty acids and sex hormones. Quercetin also reduces oxidative stress, protects against damage to cellular DNA and helps boost kidney and liver function. Studies confirm quercetin’s neuroprotective effects
Research has also confirmed that quercetin has neuroprotective effects.
According to a 2016 study published in the journal NeuroReport , researchers discovered that the oral administration of quercetin-enriched onion powder for four weeks significantly improved memory in participants with early-stage Alzheimer’s.
In a 2015 study published in the journal Acta Pharmaceutica Sinica , findings revealed that quercetin helped reduce the toxicity of beta amyloid proteins that accumulate in the brains of patients with Alzheimer’s and cause dementia and memory loss.
According to animal studies, quercetin protects brain-cell function and prevents brain-cell death. The antioxidant also helps boost natural defense systems by activating glutathione, the body’s premier antioxidant.
A different study revealed that quercetin protects brain cells against toxicity from the pesticide endosulfan by reducing oxidative stress and mitochondrial swelling. Findings showed that quercetin did more than “improve” levels of beneficial enzymes and antioxidants. Quercetin also helped reverse the deficits and restored the substances to normal, healthy levels. Boost your dietary intake of quercetin to help protect against pesticide exposure
You can increase your dietary intake of quercetin by eating a variety of foods full of this beneficial plant pigment such as: Brussels sprouts
Asparagus (Cooked contains slightly more quercetin.)
Bell peppers (Green and yellow)
Berries
Black tea Broccoli Buckwheat Cabbage Capers (The most concentrated source of quercetin.) Cherries Citrus fruits Elderberry tea Grapes Green tea Kale Nuts (Like almonds and pistachios.) Red apples Red onion (The highest vegetable source of quercetin.) Red wine Scallions Shallots Tomatoes (Organically grown tomatoes contain at least 79 percent more quercetin than conventionally grown tomatoes.) You can also take quercetin in capsule and tablet form. The usual dosages range from 150 to 400 mg a day.Pesticides are a constant threat to your overall health, but you can boost your intake of foods rich in quercetin to counteract the adverse effects of pesticide exposure.Visit Superfoods.news to learn more about fruits and vegetables that are rich in quercetin.Watch the video below to know more about how quercetin can boost your brain health . No compatible source was found for this media.This video is from the Holistic Herbalist channel on Brighteon.com . More related stories: Fight off viral infections with the power of quercetin . Quercetin: A natural painkiller for people with IBS . Sources include: NaturalHealth365.com
How Running Boosts Left Brain-Right Brain Communication

Running and REM sleep kickstart rapid-fire communication between the left and right cerebral hemispheres.
Distinct 140-Hz brainwave rhythms facilitate the turbocharged communication triggered by running and dreaming.
140-Hz brainwaves act like interwoven spline gears that coordinate left-brain, right-brain communication like a well-oiled machine.
Source: PopTika/Shutterstock New research sheds light on how running and rapid eye movement (REM) sleep enhance communication between the left and right cerebral hemispheres.
A first-of-its-kind study in rats and mice conducted by Omar Ahmed’s Lab at the University of Michigan found that when a laboratory mouse or lab rat runs quickly on a spinning wheel, its left and right cerebral hemispheres commence rapid-fire communication on a specific electrical frequency (140-Hz rhythms) within a single theta cycle.
The researchers also found that when lab animals who run on a spinning wheel during waking hours enter a REM sleep phase, their left and right brain hemispheres communicate on the same 140-Hz frequency. These findings ( Ghosh et al., 2022 ) on how running and REM sleep facilitate better interhemispheric communication between “left brain-right brain” were published on July 5 in the peer-reviewed journal Cell Reports . Running and REM Sleep Turbocharge Left Brain-Right Brain Communication
As someone who’s been a long-distance runner since 1983, I realized many moons ago that running often creates a waking dream state. If my daily jog takes me off the beaten path and is more adventurous than usual, I often dream about that day’s run in my sleep. Most dreaming occurs during REM sleep as part of a whole-brain process that facilitates the consolidation of long-term memories and mastery of skills practiced the previous day.
When I wrote The Athlete ‘s Way in the early aughts, an entire subsection of “The Brain Science of Sports” chapter was dedicated to the parallels between brain states that occur during bipedal aerobic activity and REM sleep. On an EEG, the brainwaves that occur during REM sleep and the brain’s low-voltage, high-frequency state when someone’s “in the zone” during a cardio workout mirror one another.
Over the past four decades, I’ve learned via lived experience that running changes how my brain works. When I’m in the zone and enter a state of frictionless flow during a run, the fluidity of my body’s movements and the fluidity of my mind’s thinking seem to go hand in hand. Running helps me connect the dots between seemingly unrelated ideas, boosts cognitive capacity, and improves problem-solving abilities.
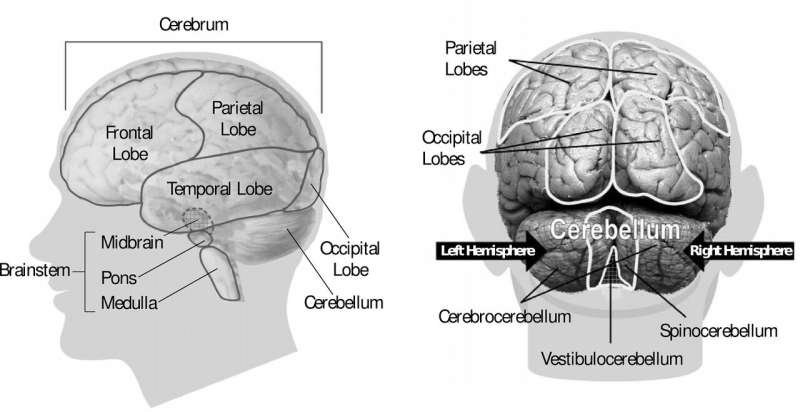
In addition to promoting creative thinking , jogging makes my brain ripe for having “Aha!” or “Eureka, I’ve found it!” moments. But why? How does running alter brain function, and why does running promote superfluid thinking ? For years, I’ve speculated that running optimizes the functional connectivity between the brain’s four hemispheres in ways that help us think better. The cerebrum and cerebellum both have left and right hemispheres. Colloquially, the term “left brain-right brain” refers to the cerebral hemispheres. Current research tends to focus on interhemispheric communication between the cerebrum’s two halves, but the cerebellar hemispheres are increasingly a region of interest for neuroscientists. Source: Magic mine/Shutterstock
When I refer to the brain’s four hemispheres , I’m talking about both cerebral hemispheres (colloquially known as left brain-right brain) and both cerebellar hemispheres. The cerebellum (Latin “little brain”) has two hemispheres that are tucked beneath the cerebrum (Latin “big brain”). Most interhemispheric brain research focuses solely on the interplay between the two cerebral hemispheres. Deciphering the interhemispheric dynamics between left brain-right brain is key to understanding how we think. 140-Hz Brainwaves Act Like Spline Gears
The latest (2022) research suggests that turbocharged left brain-right brain communication during running and dreaming is facilitated by 140-Hz rhythms that drive rapid and extremely precise neuronal firing across cerebral hemispheres. Ghosh et al. (2022) call the 140-Hz brain rhythms that occur at distinct points in a single theta cycle “splines” because they coordinate neural communication like interlocking teeth on mechanical gears. When a lab animal runs or enters a REM sleep phase, splines boost whole-brain functions by improving interhemispheric cortical communication between “right brain-left brain.” Source: Ghosh et al., 2022 Cell Reports/Open Access (CC BY-NC-ND 4.0)
Like a well-oiled machine, the 140-Hz brainwave frequency acts like a spline gear that allows both halves of the cerebrum to coordinate seamlessly and communicate rapidly without any friction or viscosity. Hence, Omar Ahmed’s Lab calls the neuronal rhythms that promote better interhemispheric communication within one theta cycle “splines” because they resemble the interlocking teeth on mechanical gears and give the brain more torque.
“These spline brain rhythms are faster than all other healthy, awake brain rhythms,” first author Megha Ghosh said in a July 2022 news release . “Splines also get stronger and even more precise when running faster. This is likely to help the left brain and right brain compute more cohesively and rapidly when an animal is moving faster and needs to make faster decisions.”
“Previously identified brain rhythms are akin to the left brain and right brain participating in synchronized swimming: The two halves of the brain try to do the same thing at the exact same time,” senior author Omar Ahmed added. “Spline rhythms, on the other hand, are like the left and right brains playing a game of very fast and precise ping pong.” This neural ping pong represents a different way for the left brain and right brain to communicate.
Optimizing interhemispheric communication improves whole-brain functions. From an evolutionary perspective, it makes sense that the mammalian brain has survival-promoting spline mechanisms that enable both cerebral hemispheres to work in unison like a well-oiled machine when an animal is on the go (hunting, foraging, evading predators) and needs to think fast. Because the brain uses REM sleep to encode memories and weaves the previous day’s lived experience into dreams, it’s not surprising that these 140-Hz brainwaves reappear during dream-state sleep. What Are the Clinical Implications of Spline-Driven Brain Communication?
Clinical depression , post- traumatic stress disorder ( PTSD ), and Alzheimer’s disease are all associated with impaired interhemispheric communication. Now that Ahmed and colleagues […]
Researchers evaluate the brain circuits involved in social defeat stress-induced sleep in mice

The stress surrounding being defeated by another mouse activates mouse midbrain cells, promoting sleep and reducing anxiety, according to a new study. The results highlight a neurological circuit in the brain, targeting of which “may help steer future interventions in rodents and perhaps even humans after stressful experiences, be it through cognitive therapy or pharmacotherapy or maybe, one day, genetic interference,” write Marian Joëls and E. Ronald de Kloet in a related Perspective.
Although stress can cause insomnia, the opposite is also true; chronic stress is known to increase rapid eye movement (REM) sleep. These observations have led some to hypothesize that sleep is an important adaptive response to stressful situations, helping ameliorate its negative physiological and mental impacts. In mice, social defeat stress (SDS) – a stress response caused by losing a social confrontation – is often used as a model for psychosocial stress. Researchers have found that SDS can cause some defeated animals to subsequently fall asleep. However, the mechanisms underlying how these events trigger enhanced sleep remain elusive. Here, Xiao Yu can colleagues evaluated the brain circuits involved in SDS-induced sleep in mice.
Yu et al. discovered a small group of neurons in the ventral tegmental area (VTA) of the midbrain that is dedicated to detecting stress after SDS and inducing restorative sleep. According to the findings, a subset of gamma-aminobutyric acid (GABA)-somatostatin neurons receive stress input, which, when activated, promote enhanced REM and non-REM sleep for several hours while also inhibiting the release of corticotropin-releasing factor (CRF). Together, sleep initiated through this process alleviated stress levels and mitigated stress-induced anxiety in mice, restoring mental and body functions. Anxiety and corticotrophin levels remained heightened after stress for mice deprived of SDS-induced sleep.
In the related Perspective, Joëls and de Kloet note that “Not all individuals may respond to social defeat with a bout of sleep.” They say this individual variation “requires further investigation in larger groups of mice, which would also be helpful to probe the robustness of the current explorative study.”
Is Depression a Sign of Low Brain Energy?
New science offers a practical model for understanding and treating depression.
New research suggests that depression could be caused by reductions in energy metabolism in the brain.
The human brain is incredibly energy intensive; even small deficits in energy production can have major consequences.
Improving our lifestyle habits is a powerful tool for preventing or reversing depression by up-regulating our brain’s energy potential.
One of the most promising new theories for understanding depression is as the result of impaired brain energy metabolism (1). The human brain is an incredibly energy-intensive organ. Weighing in at a mere 3 pounds or so—just 1-3 percent of total body weight for most people—the brain accounts for a remarkable 25 percent of the body’s total energy consumption when we are at rest. Realizing the massive energy demands of the brain, it becomes clear that even small deficits in brain energy metabolism could have potentially dire implications for how we feel and function.
Brain energy metabolism is essential to life and depends on the ability of brain cells (neurons) to convert fuel sources (e.g., food and calorie-containing beverages) into a specific form of cellular energy called adenosine triphosphate (ATP). What many people don’t realize about brain metabolism is that the ATP process can be impaired even when there is plenty of fuel available. Known as metabolic dysfunction, this results from neuronal changes that compromise their ability to create ATP.
One of the common sources of metabolic dysfunction occurs when brain mitochondria—the energy-producing powerhouses inside neurons—can no longer create enough ATP to keep up with energy demands. When mitochondrial dysfunction takes place, it is the equivalent of a plant losing the capacity to convert sunshine into energy or a stove incapable of burning wood to produce heat. In the case of neurons, cellular processes vital to health, thinking, and feeling may cease entirely or continue only in a diminished capacity.
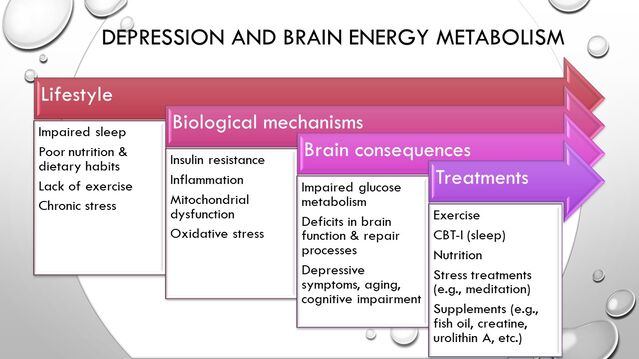
Given the latter, it is perhaps not surprising that neuroimaging, genomic, and metabolic research has identified mitochondrial dysfunction in the brain as a potential cause of depression, as well as being a possible common cord connecting depression to overlapping conditions, such as cognitive impairment, hypothyroidism, and even aging (2). This research also suggests that the people most vulnerable to depression caused by impaired brain metabolism are those with other metabolic health conditions (e.g., diabetes/pre-diabetes, insulin resistance, fatty liver, obesity, PCOS, hypertension) and lifestyle factors putting them at risk for metabolic diseases. How health habits become brain function. Source: Thomas Rutledge
The image above illustrates a general causal model for how depression and brain energy metabolism deficits may begin years or even decades earlier from unhealthy lifestyle patterns. These factors, over time, trigger adverse physiological processes that can lead to metabolic diseases in the body and metabolic dysfunction in the brain. As these processes advance, neuronal function gradually becomes compromised to such a degree that it may eventually manifest in subjective symptoms, such as lack of energy or motivation , memory and concentration difficulties, and other depressive symptoms that are likely to vary from person to person.
Because this chain of events begins in most cases from modifiable health behaviors, it follows that behavioral interventions should theoretically be amongst the best methods to reverse these processes, improve brain metabolism, and treat depression. Recent clinical trials research supports this theory strongly. In fact, the emergence of brain metabolic dysfunction as a theory for depression offers an appealing model for understanding how behavioral treatments as seemingly different as exercise, CBT for insomnia (CBT-i), meditation , and dietary changes such as intermittent fasting have each been shown to improve depression for many individuals. All of these—through a combination of biological mechanisms—improve brain metabolism and mitochondrial function.
Five ways to promote brain health, slow cognitive decline

A recent study shows strong evidence that a healthier heart is connected to a healthier brain. Exercise is crucial as you age. As Alzheimer’s & Brain Awareness Month in June wraps up, the Alzheimer’s Association is encouraging all Americans to adopt healthy lifestyle behaviors that can help reduce the risk of cognitive decline.
There are now more than 6 million Americans age 65 and older living with Alzheimer’s, including 230,000 Illinois residents.
Age is the greatest risk factor for Alzheimer’s disease. In fact, 1 in 3 seniors age 85 and older will have Alzheimer’s disease. While some brain changes are inevitable as we age, there is a growing body of research to suggest adopting healthy lifestyle behaviors, including healthy eating, exercising regularly, not smoking and staying cognitively engaged may help us age healthier and help reduce the risk of cognitive decline.
“Understanding the role healthy behaviors may play in reducing cognitive decline is a robust area of research currently,” said Delia Jervier, executive director of Alzheimer’s Association’s Illinois Chapter. “Researchers are working to determine what may be the optimal lifestyle ‘recipe’ to reduce cognitive decline, but there are steps we can take now to age well and help reduce the risk of cognitive decline.”
The Alzheimer’s Association offers these five tips to promote better brain health and help reduce the risk of cognitive decline:
Exercise regularly: Regular cardiovascular exercise helps increase blood flow to the body and brain, and there is strong evidence regular physical activity is linked to better memory and thinking.
Maintain a heart-healthy diet: Stick to a meal schedule full of fruits and vegetables to ensure a well-balanced diet. Some evidence suggests a healthful diet is linked to cognitive performance. The Mediterranean and DASH diets, which emphasize whole grains, green leafy vegetables, fish and berries, are linked to better cognitive functioning, and help reduce risk of heart disease as well.
Get proper sleep: Maintaining a regular, uninterrupted sleep pattern benefits physical and psychological health, and helps clear waste from the brain. Adults should get at least seven hours of sleep each night and try to keep a routine bedtime.
Stay socially and mentally active: Meaningful social engagement may support cognitive health, so stay connected with friends and family. Engage your mind by doing activities that stump you, like completing a jigsaw puzzle or playing strategy games. Or challenge yourself further by learning a new language or musical instrument.
Keep your heart healthy: Recent study shows strong evidence that a healthier heart is connected to a healthier brain. The study shows that aggressively treating high blood pressure in older adults can help reduce the development of mild cognitive impairment, or MCI.
“Incorporating these behaviors become especially important as we age, but they are good guidelines to follow at any age,” Jervier said. “Research suggests incorporating these behaviors in combination will have the greatest benefit, but even if you begin with one or two you’re moving in the right direction.”
To learn more about ways to reduce your risk of cognitive decline by making lifestyle changes, go to alz.org.
10 Superfood sources of biotin to help boost your overall health

( Natural News ) You may have already seen biotin supplements at the supplement aisle of a grocery store. They can be sold independently, but biotin can also be included in multivitamin blends, such as prenatal vitamins.
If you want to boost your biotin intake or prevent deficiency, it’s important to know which foods are rich in this beneficial nutrient . Why is biotin important?
According to Amy Shapiro, a registered dietitian and founder of Real Nutrition, biotin (vitamin B7) has a role in the conversion of food into energy. Biotin is crucial for keeping your skin, hair, eyes, liver and nervous system healthy. (Related: Stages of hair growth and superfoods that promote hair health .)
During pregnancy, getting enough biotin is even more important because the nutrient has a role in embryonic development, added Shapiro.
According to Jessica Cording, also a registered dietitian, the average adult needs 30 micrograms (0.03 milligrams) of biotin each day. But if you are pregnant or lactating, you need at least 35 micrograms.
These are the baseline daily levels (i.e., Recommended Dietary Allowance (RDA)) issued by the National Academies.
Biotin is important for your overall well-being because it has many functions ranging from blood sugar to beauty benefits. Biotin may help normalize blood glucose levels, a role that has been supported by preclinical research demonstrating the nutrient’s ability to support pancreatic beta-cell function and improve glucose tolerance.
Biotin’s most notable role is linked to cellular energy production. Vitamin B7 is a coenzyme for carboxylases, enzymes that help metabolize macronutrients.
Carboxylases are involved in the process of insulin release and gluconeogenesis, or the synthesis of glucose .
Whether you’re pregnant or not, getting enough biotin is important for your well-being . Below are 10 superfoods that will help boost your daily intake of biotin to prevent deficiencies. Bananas
While bananas contain less biotin than the other superfoods on this list, the benefits of this fruit go beyond their biotin content.
Additionally, you can eat bananas raw, which is important when it comes to biotin consumption. According to Shapiro, cooking methods may break down biotin and consuming some of these foods in their raw forms prove more bioavailable. Cauliflower
Cauliflower is a versatile vegetable with a muted flavor, making it a great ingredient for any side dish.
Like bananas, cauliflower doesn’t contain a high amount of biotin. However, you can make it part of a balanced diet to reap many benefits.
If you want a quick snack, dip raw cauliflower into your favorite healthy dip. During the holidays, prepare roasted cauliflower with your go-to seasoning blend.
You can also use cauliflower to make delicious cauliflower gnocchi. Certain nuts
Certain nuts like almonds , peanuts, pecans and walnuts also contain biotin. Nut butters can also be a great source of biotin, along with protein and healthy fats. Egg yolks
Egg yolks are a great source of biotin. The average cooked egg yolk contains at least 10 micrograms of biotin, which is equivalent to about 33 percent of the recommended daily intake of biotin for the average adult.
Egg yolks are also great for brain health. Start your day with a nutritious breakfast and prepare some cooked eggs. Mushrooms
To make a biotin-rich meal, saute vegetables like cauliflower, mushrooms and sweet potatoes. If you use at least one cup of fresh, chopped button mushrooms, you’ll be adding 19 percent of the daily recommended value of biotin to your meal.
Saute mushrooms, stuff them with your preferred ingredients like lean meat and other vegetables or eat them raw as a savory salad topping. Oats
If you’re following a vegan or vegetarian diet , oats are a great plant-based option for biotin.
But if you think oats are too bland, here are some suggestions on how to make oats taste better : Make oatmeal pancakes if you’re craving a tasty breakfast option.
Make overnight oats or a yogurt bowl for breakfast.
Prep homemade granola for a healthy snack.
Bake oatmeal muffins. Try making baked oatmeal. Add oats to a morning smoothie to boost your fiber intake. Replace breadcrumbs with oats and make savory dishes like chicken tenders or meatballs. Organ meats Organ meats contain a significant amount of biotin. A three-ounce serving of beef liver contains 103 percent of the amount of biotin you need daily. Salmon Salmon , which is part of the popular Mediterranean diet, offers many health benefits. A three-ounce serving of canned pink salmon contains 17 percent of the daily recommended biotin value.Salmon is full of healthy fats, especially omega-3 fatty acids. Sweet potato Sweet potatoes are a staple vegetable that’s full of nutrients like beta-carotene, biotin, fiber, iron, potassium and vitamin B6.Sweet potatoes are another versatile vegetable and you can easily incorporate them into a balanced diet. Roast chopped sweet potatoes and toss them into a salad or rice bowl to make it more satisfying.Alternatively, you can coat sweet potatoes in maple syrup and cinnamon for a sweet treat. Sunflower seeds A one-fourth cup serving of sunflower seeds contains nine percent of the daily recommended value of biotin.Additionally, savory sunflower seeds are rich in magnesium. This is important because according to studies, at least 43 percent of Americans don’t meet their daily baseline needs for magnesium.Add sunflower meals to savory dishes for extra crunch and serve them seasoned and roasted or raw.While most people living in developed countries with access to unprocessed foods can meet the daily recommended biotin value, it’s always good to know which superfoods are full of this beneficial nutrient.If you are concerned about consuming enough biotin or you want to boost your daily intake for key aspects of health, you can also use a high-quality supplement with biotin .Watch the video below to know more about the benefits and uses of biotin . No compatible source was found for this media. More related stories: Shiny hair, stronger nails: Add these 8 biotin-rich foods to your diet . Vitamin B7 (biotin) is essential for hair, skin and nails – and also supports metabolism, gut health, immunity and more . More than good hair and clear […]
Researchers show how the liver can control the brain and behavior
Credit: CC0 Public Domain A new Yale study has found that the liver plays a major role in regulating feeding behavior in mice, a discovery that could have implications for people with eating disorders and metabolic diseases. The study, which was done in collaboration with colleagues in Germany, also adds to a growing body of evidence that shows the most advanced part of the brain, the cerebral cortex, is affected by the rest of the body, not just the other way around.
“One takeaway of this work is that the classical way of trying to understand brain functions by only looking at the brain itself is not giving you the full picture,” said Tamas Horvath, the Jean and David W. Wallace Professor of Comparative Medicine at Yale School of Medicine and a senior author of the study published June 27 in Nature Metabolism .
In a series of experiments, the research team uncovered a circuit by which the brain and liver communicate with—and control—each other. The two key participants of this conversation are a group of cells known as agouti-related protein (AgRP) neurons, which are found in the hypothalamus region of the brain, and a type of lipid secreted by the liver called lysophosphatidyl choline (LPC).
AgRP neurons, which communicate with the cerebral cortex , the outer layer of the brain associated with complex behaviors and abilities, are essential for promoting feelings of hunger . But they also communicate with other parts of the body, like the liver and pancreas; when humans are hungry, these neurons play a critical role in releasing lipids from fat stores in the body.
Once LPC is secreted by the liver, an enzyme in the blood quickly converts it to lysophosphatidic acid, or LPA. Other researchers have shown that LPA can alter neuronal activity in the brain.
In this study, the researchers observed that after fasting, mice had higher levels of LPA in both the blood and the cerebrospinal fluid, the special liquid found within the central nervous system. This rise in LPA levels caused an increase in neuronal activity in the cortex, which triggered a heightened post-fasting appetite. And all of these effects were dependent on AgRP neuron function.
These findings suggest a circuit wherein AgRP neurons regulate the liver and lipid release and in which those lipids cycle back to the brain where they affect the cortex and its functions.
Horvath says more research is needed to determine if a similar circuit exists in humans, but he and his colleagues did find some evidence that it might. Mice that experience a mutation leading to greater LPA-induced neuronal activity eat more and weigh more than their typical mouse counterparts. Humans with this same genetic mutation tend to have higher body mass indexes and a greater prevalence of Type 2 diabetes than people without the mutation.
“We still need to more rigorously explore whether these mechanisms are relevant for humans, but if they are then we can start to investigate whether we can exploit the mechanisms in order to treat eating disorders and other conditions,” said Horvath. “But this shows the liver can be a major driver of behavior. And it adds to the argument that staying in the brain to understand the brain is not sufficient.”
Other Yale authors on the study are Bernardo Stutz, Zhong-Wu Liu, and Matija Sestan-Pesa.
Provided by Yale University
6 Brain Health Habits To Include In Your Daily Routine

iStock We hear a lot about the importance of heart health, gut health and taking care of our overall health, but one area often overlooked is brain health. “Your brain is a unique organ like a muscle, the more you use it the more it develops,” Dr. Walid Wazni , a Neurologist and Medical Director of the Stroke Center at Dignity Health St. Mary Hospital in Long Beach tells us. Having good brain health enhances your ability to effectively communicate, problem solve, make good decisions and live a productive life. “The health of one’s brain is the most important goal for a happy and functional life. Anyone with a family member with advanced dementia is aware of how dehumanizing it is to be without a well-functioning brain,” Dr. Mark Liker MD Neurosurgeon with Dignity Health Northridge Hospital adds. Eat This, Not That! Health spoke with neurologists who explain why it’s important to rewire your mind and daily habits to include in your daily routine that are good for the brain. Read on—and to ensure your health and the health of others, don’t miss these Sure Signs You’ve Already Had COVID . Shutterstock Dr. Liang Wang , MD Neurology, Dignity Health Northridge says, “As a neurologist, I am always searching for the latest in evidence-based medicine so that I can provide the most current recommendations regarding brain health to my patients. We as human beings have a brain that is most extraordinary and capable of astonishing things: our brains have led us to the moon, composed beautiful music (that get stuck in our heads coincidentally), and make the most complicated acrobatic movements look easy. Yet we were all born without these abilities; that’s where neuroplasticity comes in-one of the most important concepts in neuroscience and neurology. No, our brains aren’t made of plastic (though some days we might feel that way); it simply means our brain is constantly reorganizing and rewiring itself. Think of it like your smartphone’s operating system, constantly changing its functions depending on how you use it, without ever needing periodic updates. Pretty neat! Not every change is for the better however. Sadly, many readers likely have experienced a most tragic loss of a loved one due to declining mental function resulting in dementia, robbing someone of a dignified living as a person. This is all in large part due to neurodegeneration that has either hijacked or overcome the potential of neuroplasticity to ill effect, causing permanent brain damage. Which is why maintaining brain health and avoiding detrimental changes to our neuroplasticity will help ensure we remain our optimal selves for as long as possible.” Shutterstock Dr. Liker states, “Nowadays the significant changes in the daily circadian and therefore brain rhythms have been disrupted by a variety of influences and we are seeing that in the increased rates of psychological disease affecting both young and old. Rewiring the brain is a loose term that can be better defined as rectifying the functional connectivity that has gone awry due to whatever exogenous influence whether it be separation from friends and loved ones, increased drug and alcohol use, reduced physical activity, excess use of social media, change in eating or sleep habits, illness or financial stresses etc. . The most effective way to reconstitute the normal functional connectivity of the brain is to resume a healthy lifestyle. It requires a return to structured and healthy habits that we perhaps forgot or dismissed due to recent societal changes. Because of the natural diurnal changes in many brain hormones and neurochemicals, a set of regular habits will stand to benefit the brain in the long term. That means returning to the things that we all know make us feel better and improve brain function such as eating and sleeping at regular times, reducing exogenous and endogenous stimulation, getting regular exercise, eating a balanced diet. The pandemic and its effects have uncovered a great deal of psychopathology that has been “submarined” in the pre pandemic period because of loss of some regular coping mechanisms that were interfered with due to the effects of the pandemic. Depression (adult, adolescent and pediatric), anxiety, OCD, addictive behavior, pain syndromes, effects of prior head trauma can all become more burdensome in recent times. One promising technology involves non-invasive and gentle transcranial magnetic stimulation (TMS), an FDA approved therapy for some of these diseases but which also has shown surprisingly good outcomes in off-labeled applications. The general concept behind TMS is the transmission of energy to the brain surface (cortical layer) in the form of a magnetic current that rectifies the abnormal circuitry and brain oscillations that have emerged because of the above negative factors. Improvements in objective brain wave patterns (electroencephalography) and more subjective clinical behavior can be identified after the series of treatments needed to provide lasting benefit. It is a technology more common in Europe but recent developments such as MRI-guided brain navigation and personalized treatment based on abnormal EEG patterns have made the technology much more effective.” iStock Dr. Wang reminds us, “We live in a stressful and unpredictable time right now, so I will start with this. I tell my patients that even in the face of all the stressors and negativity in life, they should face it with a positive attitude; not only will they feel better, but it also helps their brain as well! Coping with stressors and maintaining mental health have been shown in studies to improve neuroplasticity and significant stress have been shown to decrease it. Talking about mental health is no longer a taboo topic, and in fact has become a hot button issue since the era of Covid. Make time and effort daily to be mindful!” Shutterstock Dr. Wazni explains, “Both the quantity and quality—is crucial to our brain health. Poor sleeping habits have been linked to numerous neurological diseases such as stroke, cognitive aging, dementia, Parkinson’s disease.”
According to Dr. Wang, “Restful sleep is essential for neuroplasticity as well as overall bodily health; lack of sleep, […]
Walking gives the brain a ‘step-up’ in function for some

Credit: Unsplash/CC0 Public Domain It has long been thought that when walking is combined with a task—both suffer. Researchers at the Del Monte Institute for Neuroscience at the University of Rochester found that this is not always the case. Some young and healthy people improve performance on cognitive tasks while walking by changing the use of neural resources. However, this does not necessarily mean you should work on a big assignment while walking off that cake from the night before.
“There was no predictor of who would fall into which category before we tested them, we initially thought that everyone would respond similarly,” said Eleni Patelaki, a biomedical engineering Ph.D. student at the University of Rochester School of Medicine and Dentistry in the Frederick J. and Marion A. Schindler Cognitive Neurophysiology Laboratory and first author of the study out now in Cerebral Cortex . “It was surprising that for some of the subjects it was easier for them to do dual-tasking—do more than one task—compared to single-tasking—doing each task separately. This was interesting and unexpected because most studies in the field show that the more tasks that we have to do concurrently the lower our performance gets.”
Improving means changes in the brain
Using the Mobile Brain/Body Imaging system, or MoBI, researchers monitored the brain activity , kinematics and behavior of 26 healthy 18 to 30-year-olds as they looked at a series of images, either while sitting on a chair or walking on a treadmill. Participants were instructed to click a button each time the image changed. If the same image appeared back-to-back participants were asked to not click.
Performance achieved by each participant in this task while sitting was considered their personal behavioral “baseline”. When walking was added to performing the same task, investigators found that different behaviors appeared, with some people performing worse than their sitting baseline—as expected based on previous studies—but also with some others improving compared to their sitting baseline. The electroencephalogram, or EEG, data showed that the 14 participants who improved at the task while walking had a change in frontal brain function which was absent in the 12 participants who did not improve. This brain activity change exhibited by those who improved at the task suggests increased flexibility or efficiency in the brain.
“To the naked eye , there were no differences in our participants. It wasn’t until we started analyzing their behavior and brain activity that we found the surprising difference in the group’s neural signature and what makes them handle complex dual-tasking processes differently,” Patelaki said. “These findings have the potential to be expanded and translated to populations where we know that flexibility of neural resources gets compromised.”
Edward Freedman, Ph.D., associate professor of Neuroscience at the Del Monte Institute led this research that continues to expand how the MoBI is helping neuroscientists discover the mechanisms at work when the brain takes on multiple tasks. His previous work has highlighted the flexibility of a healthy brain, showing the more difficult the task the greater the neurophysiological difference between walking and sitting. “These new findings highlight that the MoBI can show us how the brain responds to walking and how the brain responds to the task,” Freedman said. “This gives us a place to start looking in the brains of older adults, especially healthy ones.”
Expanding this research to older adults could guide scientists to identify a possible marker for “super agers” or people who have a minimal decline in cognitive functions. This marker would be useful in helping better understand what could be going awry in neurodegenerative diseases.
Provided by University of Rochester Medical Center
Reducing air pollution can support healthy brain development, study finds

Credit: Unsplash/CC0 Public Domain A new study finds that having a portable air cleaner in the home can reduce the negative impacts of air pollution on brain development in children.
Simon Fraser University researchers collaborated with U.S. and Mongolian scientists to study the benefits of using air filters to reduce exposure to air pollution during pregnancy, and assessed the impact on children’s intelligence.
The researchers note that their randomized controlled trial is the first study of its kind to document the impacts of air pollution reduction on cognition in children.
Beginning in 2014, the team recruited 540 pregnant women in Ulaanbaatar, Mongolia to participate in the Ulaanbaatar Gestation and Air Pollution Research (UGAAR) study. Ulaanbaatar has some of the worst air quality in the world, well exceeding guidelines set by the World Health Organization (WHO).
The women were less than 18 weeks into their pregnancies and non-smokers who had not previously used air filtering devices in their homes. They were randomly assigned to either the control or intervention group. The intervention group was provided with one or two HEPA filter air cleaners and encouraged to run the air cleaners continuously for the duration of their pregnancies. The air cleaners were removed from the home once the child was born.
The researchers later measured the children’s full-scale intelligence quotient (FSIQ) at four years of age using the Weschler Preschool and Primary Scale of Intelligence.
They found that the children born to mothers who had used the air cleaners had an average FSIQ that was 2.8-points higher than the group that did not use an air cleaner during pregnancy.
“These results, combined with evidence from previous studies, strongly implicate air pollution as a threat to brain development,” says Ryan Allen, professor of environmental health in SFU’s Faculty of Health Sciences. “But the good news is that reducing exposure had clear benefits.”
Children in the intervention group also had significantly greater average verbal comprehension index scores, which is consistent with results from previous observational studies. The research suggests that a child’s verbal skills may be particularly sensitive to air pollution exposure.
More than 90 per cent of the world’s population breathes air with particulate matter concentrations above the WHO guidelines. The researchers suggest the population-level impact of air pollution on brain development could be substantive even if the individual-level effects are modest.
Their study results indicate that reducing exposure to air pollution during pregnancy could improve children’s cognitive development around the world.
“Air pollution is everywhere, and it is preventing children from reaching their full potential,” adds Allen. “Air cleaners may provide some protection, but ultimately the only way to protect all children is to reduce emissions.”
Provided by Simon Fraser University
Un-beet-able: Study shows beetroot can boost athletic performance

( Natural News ) Beets are often used to make a sour soup called borscht or salads, but the root vegetable might soon be consumed by many athletes. According to a study conducted by researchers from the University of South Australia (UniSA), beets can naturally boost athletic performance .
Researchers conducted a meta-analysis of 118 studies from 25 countries and they assessed the performance effects of several foods considered to benefit aerobic performance. Results showed that beetroot , grapes, sour cherries and pine bark extract helped boost endurance exercise performance by improving nitric oxide availability in the body.
Beetroot’s high nitrate levels, which have been shown to improve blood circulation and increase oxygen and nutrient delivery to muscles during exercise, helped the athletes reach peak performance quicker. On the other hand, the polyphenols in cherries , grapes, and pine bark extract protected nitrate from degradation, which helped increase stamina.
Polyphenols are powerful antioxidants that can help reduce the impact of oxidative stress. These compounds also prevent or reverse cell damage caused by aging, environmental and lifestyle factors.
Noah D’Unienville, the study’s lead researcher, said the study findings prove that beets and certain foods are “natural endurance enhancers.”
A low-calorie vegetable, beets are full of essential vitamins and minerals .
Beets contain a bit of almost all of the vitamins and minerals your body needs to stay healthy. A 3.5-ounce (100-gram) serving of boiled beetroot contains 44 calories, 0.2 grams of fat, two grams of fiber, 1.7 grams of protein and 10 grams of carbs. The same serving also contains: Folate – 20 percent of the Daily Value (DV)
Manganese – 14 percent of the DV
Copper – eight percent of the DV
Potassium – seven percent of the DV
Magnesium – six percent of the DV
Iron – four percent of the DV
Vitamin B6 – four percent of the DV
Vitamin C – four percent of the DV
Beets are a great source of folate, a vitamin that has an important role in growth, development and heart health. Additionally, beets are rich in manganese, a nutrient with a role in bodily functions like bone formation, nutrient metabolism and brain function.
Beets are also full of copper, an essential mineral needed for energy production and the synthesis of certain neurotransmitters. Beets contain compounds with protective effects
D’Unienville explained that while there is a lot of interest in nitrate-rich and polyphenol-rich foods due to their potential to boost exercise performance, it doesn’t mean that containing these elements will automatically translate into an improvement in exercise performance.
For example, the UniSA study showed that beetroot can boost performance but other foods full of nitrates, like red spinach, rhubarb and Swiss chard did not offer similar benefits. At the same time, while grapes, sour cherries and pine bark extract helped boost the athletes’ performance, other foods full of polyphenols like blackcurrant, cocoa, ginseng and green tea did not.
There isn’t a lot of data on spinach, Swiss chard and rhubarb compared to beetroot, but D’Unienville said it’s possible those three vegetables did not show performance benefits even though they were full of nitrates because they are also lower in polyphenols than beetroot. (Related: Beetroot is packed with disease-fighting antioxidants, phytonutrients and essential nutrients .)
The protective effect of these antioxidants on the nitric oxide converted from the nitrate in the beetroot may make the difference, said D’Unienville. He added that in some studies where nitrates were removed from the beetroot, the vegetable still had a minor effect on exercise performance.
Jon Buckley, a study co-researcher, said that despite the benefits of foods like beetroot, grapes and sour cherries to exercise performance, their effects did discriminate. More significant effects were observed in the athletes who were less fit. Men were also more likely to benefit from beetroot, grapes and sour cherries than women.
If you want to boost your athletic performance, Buckley recommends training regularly and consuming beetroot juice.
Visit Veggie.news to learn more about the health benefits of beets and other amazing superfoods.
Watch the video below for 10 good reasons to eat more beets . No compatible source was found for this media. More related stories:
Better than sports drinks: Prevent dehydration with these 20 electrolyte-rich foods .
Athletes who want to boost their game are recommended to try beetroot . Perform better mentally AND physically with beets . Sources include:

