Nature Knows and Psionic Success
God provides
Study: Older adults who regularly use the internet have LESS DEMENTIA RISK than non-regular users

Who was behind the Gaza hospital blast a visual investigation. Advertisement
Regular internet usage is often painted as a negative, but research has found a positive to the practice – especially in the case of older users .
A longitudinal study of a large group of older adults showed that regular internet users had approximately half the risk of dementia compared to their same-age peers who did not use the internet regularly. Participants using the internet between six minutes and two hours per day had the lowest risk of dementia, according to the study published in the Journal of the American Geriatrics Society .
The authors said public discussions about internet use often revolve around problematic internet use – particularly among children and adolescents. But they noticed that this difference remained even after controlling for education, ethnicity, sex, generation and signs of cognitive decline at the start of the study. (Related: Too much internet use can lead to depression in young people .)
Studies often link large amounts of time spent on the internet with various adverse conditions . However, the internet also forms the backbone of modern economy and entertainment – providing lots of cognitively engaging content that is relatively easy to access.
Additionally, scientists have previously shown that online engagement can make individuals more resilient against brain decay or physiological damage to the brain that develops as people age.
This can, in turn, help older adults compensate for brain aging and reduce the risk of dementia. In this way, internet use can help extend the cognitively healthy lifespan.
Indeed, previous studies have shown that internet users tend to have better overall cognitive performance , verbal reasoning and memory than non-users.
However, most of these studies did not track changes over time or tracked them for very short periods. Thus, it could not be determined whether internet use helps maintain cognitive functioning or whether individuals with better cognitive functioning were more likely to use the internet.
In this paper, corresponding study author Dr. Virginia Chang and her colleagues wanted to examine how the risk of developing dementia is associated with whether adults regularly use the internet.
They were also interested in how this association changes over time and how the total period of internet use in late adulthood is associated with the risk of dementia.
Finally, they wanted to see if there might be an adverse effect of excessive internet use by examining the association between the risk of dementia and the daily number of hours spent on the internet. How the study was done
The researchers followed more than 18,000 dementia-free adults and analyzed data from The Health and Retirement Study – an ongoing longitudinal survey of a nationally representative sample of U.S. older-age adults aged 50 and over.
All 18,154 participants were born before 1966 and were aged between 50 and 65 years at the start of the analysis period. The median follow-up period of participants whose data were analyzed in this study was eight years, but it went up to 17 years with some.
Data analyses were conducted from September 2021 to November 2022. The researchers examined the relationship between internet usage and education, race-ethnicity, sex and generation.
Moreover, they examined whether the risk of dementia varied by the cumulative period of internet usage to see if starting or continuing usage in old age modulated subsequent risk.
The study interviewed participants every second year since 2002 about their internet usage, including frequency, duration and purpose of internet use.
Assessments of dementia were also conducted every second year through the modified Telephone Interview for Cognitive Status. Study authors calculated how long participants survived without dementia. They also used various demographic data about participants in their analysis. What the study showed
Over the years, internet usage was monitored as was cognitive decline. Data statistics showed the following: 65 percent of participants were regular internet users and 35 percent were non-regular users
21 percent changed their internet use habits during the study period while 53 percent did not change them
26 percent dropped out
Eight percent died during the follow-up period or experienced another event and were excluded from further analysis
Five percent of participants developed dementia during the study period
Regular internet users had a 1.54 percent chance of developing dementia. This risk was 10.45 percent for non-regular users.
When time until the development of dementia was analyzed, results showed that the risk of dementia of regular internet users was 57 percent lower than the risk non-regular users had of developing dementia.
Findings showed the relationship between dementia risk and daily hours of internet usage was U-shaped.Adults using the internet between six minutes and two hours per day were found to have the lowest risk of dementia. This risk was much higher in adults who did not use the internet at all but also increased gradually with more daily internet use beyond two hours.The study authors said: “Our findings show evidence of a digital divide in the cognitive health of older-age adults. Specifically, adults who regularly used the internet experienced approximately half the risk of dementia than adults who did not, adjusting for baseline cognitive function, self-selection into baseline internet usage, self-reported health and a large number of demographic characteristics.”The study had limitations that needed to be taken into account. Notably, the dementia assessment used might not completely agree with clinical diagnoses of dementia.Additionally, the study included only individuals without dementia at the start of the study and excluded individuals who developed dementia early . Results might not have been the same if such individuals, who are part of the general population, were included in the study.Watch this video explaining why the internet must go . LEAKED: The Internet Must GoThis is a modal window.No compatible source was found for this media.This video is from the Puretrauma357 channel on Brighteon.com . More related stories: Violent video games and certain internet use cause aggression and other negative outcomes. Excess weight in teen girls linked to internet, alcohol and lack of sleep. Online safety: How to avoid common internet scams. Sources include: […]
Study: Compounds in seaweeds show promise in cancer research

Advertisement
Seaweeds can be used as food and treatment for common ailments. They are used to treat boils, dropsy or edema (swelling caused by fluids trapped in the body), fever, hemorrhoids, lumps, orchitis (inflammation of one or both testicles), scrofula (an infection in the lymph nodes in the neck), urination problems and many more.
Now, studies have shown that seaweeds and certain compounds in them show promise when it comes to treating cancer. One of the studies, which documented how people had been saved by seaweeds , was published in the Journal of Applied Phycology.
Another study published in Marine Drugs described seaweeds as a good source of vitamins (A, B1, B2, B9, B12, C, D, E, and K), essential minerals (calcium, copper, fluoride, iodine, iron, magnesium, manganese, phosphorus, potassium, selenium and zinc), dietary fibers and protein.
Moreover, seaweeds have been found to be rich in essential amino acids, polyphenols, polysaccharides, sterols, terpenoids and several other bioactive compounds, which exhibit anticancer, antidiabetic, anti-inflammatory, antimicrobial and antioxidant properties.
Some of the bioactive compounds that have been attributed to the effective treatment of a multitude of conditions, diseases and disorders in various fields of medicine, particularly cancer research include carotenoids like fucoxanthin and zeaxanthin; iodine; phycolloids, including agar, alginate, carrageenan; polyphenols, such as phlorotannins; and polysaccharides, including fucoidan and laminarin.
Seaweeds are a healthy, low-calorie and nutritious food – possessing a low-lipid content, but enriched in polyunsaturated fatty acids. (Related: Supercharge your health with seaweed .) Seaweeds in the oncology arena
Seaweeds are a rich source of bioactive metabolites whose properties exhibit anti-tumoral and anti-metastatic activities (by preventing the adhesion of tumor cells), including inducing tumor cell apoptosis or cell death, against some types of cancer lines without affecting healthy cells negatively.
Here are the compounds in seaweeds that can help treat cancer , according to research. Fucoxanthin (brain cancer)
Researchers in the European Union (EU)-funded project GENIALG (GENetic diversity exploitation for Innovative macro-ALGal biorefinery) found that the compound fucoxanthin , a type of carotenoid pigment found in brown seaweeds, also known as sugar kelp ( Saccharina latissima ) could help treat one of the most common and aggressive forms of malignant brain tumor.
The study found that fucoxanthin inhibits cancer cell groups by itself but also improves the effectiveness of certain anti-proliferative pharmaceutical medicines used in cancer treatment.
“The compound could provide an effective treatment against glioblastoma multiforme (GBM), the most common and aggressive form of malignant brain tumor, with an annual incidence of three to four cases per 100,000 people in Europe,” said Dr. David Baily, director of IOTA Pharmaceuticals.
With an average survival rate of 12 months after diagnosis, Baily added that GBM remains an incurable disease – even with the improvement of knowledge of its genetic causes. He attributed part of the poor prognosis to tumor heterogeneity – different parts of the tumor have different characteristics, so it tends to respond differently to treatment.
As a result, a single treatment may kill some of the cancerous cells, while others continue to grow. Therefore, it is important to find and develop combination therapies that can tackle all parts of the tumor, explained Baily. Fucoidan (breast cancer)
A study published in the Molecules demonstrated how the compound fucoidan exhibits antioxidant, antiviral, immune-modulatory and anticancer or cancer-preventive activity against a wide range of malignancies. (Related: Seaweed extract outperforms chemo drug in shrinking breast tumors – but without the toxic side effects .)
Fucoidan prompts cell cycle arrest and apoptosis, blocks metastasis and angiogenesis as well and modulates physiological signaling molecules – thereby inhibiting tumorigenesis or the gain of malignant properties in normal healthy cells, following a step-by-step progression that eventually leads to metastasis or the spread of cancer to other parts of the body.
Fucoidan exists mainly in the cell wall matrix of various species of brown seaweed, such as bladderwrack, kombu, limunoii, mozuko and wakame. (Related: Wakame: An iodine-rich seaweed with impressive fat-burning properties .)
Researchers also found various forms of fucoidan in some marine invertebrates, such as sea cucumbers and sea urchins. Carotenoids (colorectal cancer)
In a study of 893 adults who were tested having colorectal endoscopy, researchers from Japan’s Red Cross Kyoto Daiichi Hospital reported that zeaxanthin and other seaweed carotenoids , such as fucoxanthin and its deacetylated metabolite fucoxanthinol, reduce the incidence of colorectal cancer among Japanese adults.
Researchers noted that men who had higher circulating levels of zeaxanthin had over 30 percent fewer incidence of colorectal cancer and about 50 percent fewer incidence of polyps than those who had lower circulating levels of zeaxanthin. Phenolic compounds bromophenols and phlorotannins and fucoxanthin (gastric cancer and several others)
Research from the Science University of Tokyo found that seaweed extracts inhibit five different human cancer lines , including gastric cancer.
After testing extracts from 16 different species from the Danish coastlines for free radical scavenging, a study from Denmark’s National Food Institute and the Technical University of Denmark found that their phenolic content and sulfated polysaccharide content enabled them to produce significant antioxidant and radical scavenging effects . The results of this study were published in the journal Food Chemistry.
This has been confirmed by researchers from the Daniel K. Inouye College of Pharmacy at the University of Hawaii at Hilo , who published their findings in Scientific Reports. In the course of studying the anti-cancer effects of seaweeds, they found that phenolic compounds – such as bromophenols and phlorotannins , along with their fucoxanthin content – contribute to an antioxidant effect that prevents different cancer forms.
Visit Anticancer.news for more stories about anticancer food.
Watch this video about the benefits of bladderwrack seaweed . Bladderwrack Seaweed Benefits
This is a modal window.No compatible source was found for this media.This video is from the Holistic Herbalist channel on Brighteon.com . More related stories: Seaweed found to accelerate excretion of dioxins from the body . Sodium alginate from seaweed could help with weight loss . Things to know about seaweed . Sources include: NaturalHealth365.com Springer.com MDPI.com 1 Cordis.Europa.eu MDPI.com 2 PlantMedicine.org MDPI.com 3 ScienceDirect.com 1 ScienceDirect.com […]
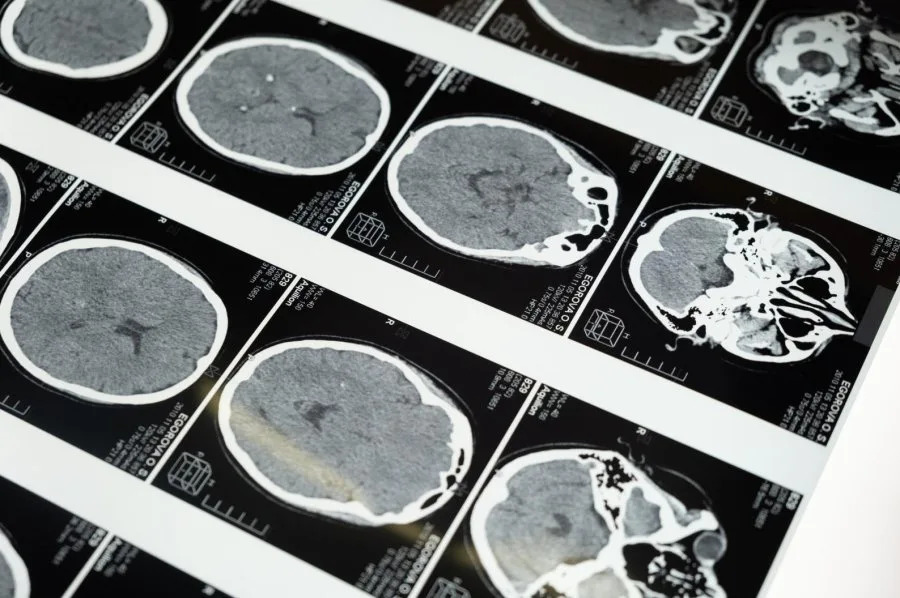
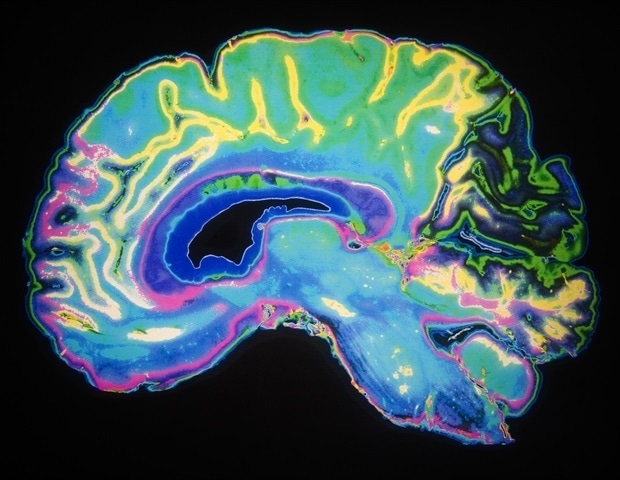
Converting brain immune cells into neurons helps mice recover after stroke
Researchers at Kyushu University have discovered that turning brain immune cells into neurons successfully restores brain function after stroke-like injury in mice. These findings, published on October 10 in PNAS, suggest that replenishing neurons from immune cells could be a promising avenue for treating stroke in humans.
Stroke, and other cerebrovascular diseases, occur when blood flow to the brain is affected, causing damage to neurons. Recovery is often poor, with patients suffering from severe physical disabilities and cognitive problems. Worldwide, it’s one of the most common causes for needing long-term care.
“When we get a cut or break a bone, our skin and bone cells can replicate to heal our body. But the neurons in our brain cannot easily regenerate, so the damage is often permanent,” says Professor Kinichi Nakashima, from Kyushu University’s Graduate School of Medical Sciences. “We therefore need to find new ways to replace lost neurons.”
One possible strategy is to convert other cells in the brain into neurons. Here, the researchers focused on microglia, the main immune cells in the central nervous system. Microglia are tasked with removing damaged or dead cells in the brain, so after a stroke, they move towards the site of injury and replicate quickly.
“Microglia are abundant and exactly in the place we need them, so they are an ideal target for conversion,” says first author, Dr. Takashi Irie from Kyushu University Hospital.
In prior research, the team demonstrated that they could induce microglia to develop into neurons in the brains of healthy mice. Now, Dr. Irie and Professor Nakashima, along with Lecturer Taito Matsuda and Professor Noriko Isobe from Kyushu University Graduate School of Medical Sciences, showed that this strategy of replacing neurons also works in injured brains and contributes to brain recovery.
To conduct the study, the researchers caused a stroke-like injury in mice by temporarily blocking the right middle cerebral artery — a major blood vessel in the brain that is commonly associated with stroke in humans. A week later, the researchers examined the mice and found that they had difficulties in motor function and had a marked loss of neurons in a brain region known as the striatum. This part of the brain is involved in decision making, action planning and motor coordination.
The researchers then used a lentivirus to insert DNA into microglial cells at the site of the injury. The DNA held instructions for producing NeuroD1, a protein that induces neuronal conversion. Over the subsequent weeks, the infected cells began developing into neurons and the areas of the brain with neuron loss decreased. By eight weeks, the new induced neurons had successfully integrated into the brain’s circuits.
At only three weeks post-infection, the mice showed improved motor function in behavioral tests. These improvements were lost when the researchers removed the new induced neurons, providing strong evidence that the newly converted neurons directly contributed to recovery.
“These results are very promising. The next step is to test whether NeuroD1 is also effective at converting human microglia into neurons and confirm that our method of inserting genes into the microglial cells is safe,” says Professor Nakashima.
Furthermore, the treatment was conducted in mice in the acute phase after stroke, when microglia were migrating to and replicating at the site of injury. Therefore, the researchers also plan to see if recovery is also possible in mice at a later, chronic phase.
Turning brain immune cells into neurons restores brain function after stroke-like injury in mice

Researchers at Kyushu University have discovered that turning brain immune cells into neurons successfully restores brain function after stroke-like injury in mice. These findings, published on October 10 in PNAS, suggest that replenishing neurons from immune cells could be a promising avenue for treating stroke in humans.
Stroke, and other cerebrovascular diseases, occur when blood flow to the brain is affected, causing damage to neurons. Recovery is often poor, with patients suffering from severe physical disabilities and cognitive problems. Worldwide, it’s one of the most common causes for needing long-term care. When we get a cut or break a bone, our skin and bone cells can replicate to heal our body. But the neurons in our brain cannot easily regenerate, so the damage is often permanent. We therefore need to find new ways to replace lost neurons.” Professor Kinichi Nakashima, from Kyushu University’s Graduate School of Medical Sciences One possible strategy is to convert other cells in the brain into neurons. Here, the researchers focused on microglia, the main immune cells in the central nervous system. Microglia are tasked with removing damaged or dead cells in the brain, so after a stroke, they move towards the site of injury and replicate quickly.
“Microglia are abundant and exactly in the place we need them, so they are an ideal target for conversion,” says first author, Dr. Takashi Irie from Kyushu University Hospital.
In prior research, the team demonstrated that they could induce microglia to develop into neurons in the brains of healthy mice. Now, Dr. Irie and Professor Nakashima, along with Lecturer Taito Matsuda and Professor Noriko Isobe from Kyushu University Graduate School of Medical Sciences, showed that this strategy of replacing neurons also works in injured brains and contributes to brain recovery.
Neuroscience eBook Compilation of the top interviews, articles, and news in the last year. Download the latest edition
To conduct the study, the researchers caused a stroke-like injury in mice by temporarily blocking the right middle cerebral artery – a major blood vessel in the brain that is commonly associated with stroke in humans. A week later, the researchers examined the mice and found that they had difficulties in motor function and had a marked loss of neurons in a brain region known as the striatum. This part of the brain is involved in decision making, action planning and motor coordination.
The researchers then used a lentivirus to insert DNA into microglial cells at the site of the injury. The DNA held instructions for producing NeuroD1, a protein that induces neuronal conversion. Over the subsequent weeks, the infected cells began developing into neurons and the areas of the brain with neuron loss decreased. By eight weeks, the new induced neurons had successfully integrated into the brain’s circuits.
At only three weeks post-infection, the mice showed improved motor function in behavioral tests. These improvements were lost when the researchers removed the new induced neurons, providing strong evidence that the newly converted neurons directly contributed to recovery.
“These results are very promising. The next step is to test whether NeuroD1 is also effective at converting human microglia into neurons and confirm that our method of inserting genes into the microglial cells is safe,” says Professor Nakashima.
Furthermore, the treatment was conducted in mice in the acute phase after stroke, when microglia were migrating to and replicating at the site of injury. Therefore, the researchers also plan to see if recovery is also possible in mice at a later, chronic phase.
Source:
Kyushu University
Journal reference:
Irie, T., et al. (2023). Direct neuronal conversion of microglia/macrophages reinstates neurological function after stroke. PNAS . doi.org/10.1073/pnas.2307972120 .
Decoding Humanity: The 3,000+ Brain Cell Types Revealing Our Secrets
Researchers, through a massive collaboration supported by the BRAIN Initiative, unveil detailed studies on human and primate brain cellular structures, identifying over 3,000 distinct brain cells and contributing to the expansive Human Cell Atlas project. You have 3,000+ different kinds of brain cells, and more insights from the largest human brain cell atlases created to date.
Scientists have just unveiled a massive effort to understand our own brains and those of our closest primate relatives.
In a suite of 21 papers published on October 12 in the journals Science (12) , Science Advances (8) , and Science Translational Medicine (1) , a large consortium of researchers shares new knowledge about the cells that make up our brains and the brains of other primates. It’s a huge leap from previously published work, with studies and data that reveal new insights about our nervous systems’ cellular makeup across many regions of the brain and what is distinctive about the human brain.
Watch on
The research consortium is a concerted effort to understand the human brain and its modular, functional nature. It was brought together and is funded by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies ® (BRAIN) Initiative . Hundreds of scientists from around the world worked together to complete a range of studies exploring the cellular makeup of the human brain and those of other primates, and to demonstrate how a transformative new suite of scalable techniques can be used to study the detailed organization of the human brain at unprecedented resolution.
Understanding our brain at the cellular level is key to understanding how our brains function and who we are as a species, as well as more accurately pinpointing the cellular roots of brain diseases and disorders—knowledge that could ultimately lead to better treatments for those diseases.
Scientists at the Allen Institute for Brain Science, a division of the Allen Institute, led five of these studies and made significant contributions to three others, including a study that greatly expands on existing knowledge about the number of types of cells in the adult human brain. Scientists at Karolinska Institute and the Allen Institute studied the genes switched on in individual brain cells, a technique known as single-cell transcriptomics, revealing an astonishing diversity of cell types: we have more than 3,000 different kinds of brain cells.
Sr. Investigator, Ed Lein and Sr. Scientist, Meanhwan Kim observe live brain tissue on a multi-patch rig, while in the electrophysiology lab at the Allen Institute. Credit: Erik Dinnel / Allen Institute
“I view this as a pivotal moment in neuroscience, where new technologies are now allowing us to understand the very detailed cellular organization of the human brain and of other primate brains,” said Ed Lein, Ph.D., Senior Investigator at the Allen Institute for Brain Science, who led several of the newly published studies. “At its core, this body of work is a triumph of molecular biology: Differential gene usage can be used to define cell types, and the tools of genomics could be used to create the first drafts of high-resolution, annotated maps of the cells that make up the entire human brain.”
The studies also tackle a range of important questions such as: How different are individual people’s brains at the cellular level? How different are our brains from those of our closest ape relatives? How many kinds of brain cells do we have? What are the properties of these cells? How do these cells emerge and mature in development?
Building off previous work mapping brain cell types in high resolution in single regions of the human cortex, the outermost shell of the brain, the newly published package expands those studies to dozens up to a hundred regions across the entire brain. Where the single region studies found over 100 different brain cell types, the newly released data shows thousands of different kinds of brain cells across the entire brain. For many parts of the brain, that complexity and variety had never before been described.
These studies are part of the NIH’s BRAIN Initiative Cell Census Network, or BICCN, a five-year funding program that was launched in 2017 to create a catalog of brain cell types. This body of work demonstrated the scalability of cutting edge cellular and molecular approaches to tackle the challenges of size and complexity of the human brain, and has set the stage for the next phase of this cell census effort. This next phase, part of which is underway at the Allen Institute, will build much more comprehensive atlases of human and other primate brains through the BRAIN Initiative’s Cell Atlas Network, or BICAN.
“The present suite of studies represents a landmark achievement that continues to build an important bridge toward illuminating the complexity of the human brain at the cellular level,” said Dr. John Ngai, Director of the NIH BRAIN Initiative. “The scientific collaborations forged through BICCN, and continuing in the next phase in BICAN, are propelling the field forward at an exponential pace; the progress – and possibilities – have been simply breathtaking.”
The human studies used postmortem tissue from people who had donated their brains to science, as well as healthy living tissue donated from patients who had undergone brain surgery and donated tissue to research.
The data from the newly released studies will also feed into the Human Cell Atlas , an international effort that is building a comprehensive reference atlas of cells across all organs, tissues, and systems of the human body.
The five Allen Institute-led studies include: An exploration of the variability in brain cell types between individual people . In this study, the scientists looked at brain cells by the levels of the genes they switch on in one region of the cortex, the middle temporal gyrus, across 75 different adult donors. This was one of the first human brain studies to compare a large number of individual people using single-cell techniques. The researchers found that while we all have the same basic cellular parts list, the proportions of certain kinds of cells and the genes switched on in those […]
5 brain-boosting snacks that are perfect for the workplace

Morning and after-lunch snacks are important at work because they keep your concentration going during the workday.
“To keep your brain sharp during the workday, it’s important to choose snacks that provide a balance of nutrients, including complex carbohydrates, healthy fats, and protein,” Sarah Heckler, MS, RD, a dietitian with Anne Till Nutrition Group in Raleigh, North Carolina, told FOX Business.
Nutrition experts say to pick these brain-bossing snack ideas over empty calories like candy, another cup of coffee or a sugary carb-laden snack selection.
Check out these five. 1. Greek yogurt
Most offices have a fridge — and this snack choice is an easy way to stay on a healthy track.
“Greek yogurt is high in protein, which can help keep you feel full and provide a steady release of energy,” said Heckler.
She suggested adding some blueberries, strawberries or raspberries for extra flavor and antioxidants, which she noted may improve cognitive function. Nutritionists say these snacks are brain-boosting in the workplace. 2. Nuts and seeds
Almonds, walnuts, and pumpkin seeds are rich in omega-3 fatty acids and antioxidants, which support brain health, said Heckler.
These types of snacks store well in your desk drawer or handbag — and can also work well for on-the-go jobs. 3. Hummus with veggies
Hummus is a good source of protein and healthy fats, said Heckler.
“Pair hummus with carrot sticks, cucumber slices, or bell pepper strips for a satisfying and nutritious snack,” she said. Hummus can be a good source of protein and healthy fats. 4. Whole grain crackers and cheese
Taking a snack break can recharge your afternoon, especially when your snack offers a blend of nutrition benefits.
“Whole grain crackers provide complex carbohydrates — and cheese offers protein and healthy fats,” Heckler said.
The best part of this snack choice is you can mix and match crackers and cheese varieties so you don’t fall into a snack rut. 5. Apple and peanut butter
Great snack picks are a balance of carbs, healthy fat, protein and fiber, and the apple and peanut butter combo fits the bill, said Julie Lopez, RD, owner of Virtual Teaching Kitchen and based in New Jersey.
Packaged sliced apples and individual peanut butter cups can make this snack option a cinch. Picking better snacks has impactful benefits
Research shows how eating nutritious foods like fruits and vegetables throughout the day boosts brainpower, mood, engagement and productivity.
In addition to creating a better snack plan, stay hydrated throughout the day by drinking plenty of water, Heckler recommended.
What do you think? Post a comment.
“Dehydration can negatively impact cognitive function,” she said.
Also, keep your snack breaks snack-sized.
“Portion control is also important to avoid feeling sluggish after snacking,” Heckler said.
New atlas of brain cells offers insight on disorders like autism and ADHD
SCOTT SIMON, HOST:
Scientists are one step closer to understanding the human brain. NPR’s Jon Hamilton reports on a new atlas that catalogs more than 170 billion brain cells that allow us to walk, talk and think.
JON HAMILTON, BYLINE: The atlas arrived in the form of more than 20 research papers in three different scientific journals. Together, the papers map out the location, structure and function of at least 3,000 types of brain cells. Ed Lein of the Allen Institute for Brain Science is one of several hundred researchers who worked on the project.
ED LEIN: We really need this kind of information if we’re going to understand what makes us unique as humans or what makes us different as individuals, or how does the brain develop.
HAMILTON: Lein says the atlas also offers a way to study conditions ranging from Alzheimer’s to depression.
LEIN: You can use this map to understand what actually happens in disease and what kinds of cells may be vulnerable or affected.
HAMILTON: The atlas still isn’t finished. Researchers expect to find even more types of cells, and they don’t fully understand some of the ones they’ve already found, like splatter neurons. Lein says the name describes what these highly complex cells look like when they’re represented in two dimensions instead of three.
LEIN: When you do that with these types of neurons, it looks a bit like a Rorschach test. It’s a splatter of these types of cells.
HAMILTON: Like bugs on a windshield. Lein says the atlas in its current form amounts to a first draft.
LEIN: But it really has set the stage to show that this is a definable system.
HAMILTON: And already, the atlas is offering a way to see how the human brain differs from animal brains. Dr. Trygve Bakken of the Allen Institute says humans have some specialized cells for processing visual information that mice don’t.
TRYGVE BAKKEN: We share kind of a basic plan with mice, but we see specializations in primates that we don’t necessarily see in a mouse.
HAMILTON: Those specializations are present in primates like chimps and gorillas, whose brains were also mapped as part of the atlas project. But Bakken says in those species, scientists found subtle differences in the brain areas that humans use to process language.
BAKKEN: What we found in this study is that there really is a conserved set of cell types that we share with chimpanzees and gorillas, but the gene expression has changed in those cells.
HAMILTON: In ways that suggest humans’ language abilities are the result of a different wiring, not different brain cells. The atlas project is funded largely by the National Institutes of Health as part of its BRAIN Initiative, which was launched a decade ago by President Obama. One of its goals is to find new treatments for brain disorders. Bing Ren of the University of California San Diego says these disorders often occur when our DNA undergoes subtle changes.
BING REN: Interpreting those changes actually has been the hard part because we lacked the dictionary to understand what they are.
HAMILTON: So as part of the atlas project, Ren and his team have been creating a dictionary that links genetic changes to specific types of brain cells.
REN: For example, we found that late-onset Alzheimer’s disease are particularly associated with a type of cell we call microglia.
HAMILTON: An immune cell that’s known to be activated in Alzheimer’s patients. Ren says the dictionary also connected genes that raise the risk of major depressive disorder with one particular set of neurons.
REN: By contrast, a different set of neurons are being linked to the risk of schizophrenia.
HAMILTON: Ren says this sort of information could lead to treatments that target specific types of cells. The new research papers appear in the journals Science, Science Advances and Science Translational Medicine.
Jon Hamilton, NPR News.
(SOUNDBITE OF MUSIC) Transcript provided by NPR, Copyright NPR.
NPR transcripts are created on a rush deadline by an NPR contractor. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.
Social media use linked to TEENAGE DEPRESSION, warn mental health experts
Advertisement
For many teenagers, spending several hours on their phones scrolling through social media is considered normal, even boring at times. But health experts are worried, especially because of the growing link between frequent social media use, teenage depression and mental health .
Scientists are starting to uncover alarming connections between social media use and depression. According to data, every additional hour spent on social media sites is linked with more depressive symptoms.
Because the prevalence of major depressive episodes among adolescents increased from 8.1 percent to 15.8 percent between 2009 and 2019, mental health experts started studying the factors contributing to this change.
Jean M. Twenge, a professor of psychology at San Diego State University , explained that there are many causes of depression and that they often interact.
Twenge added that while some individuals have a genetic predisposition to depression, they might only become depressed if “the environment creates the right conditions.” Unfortunately, spending too much time on social media could be one of those factors. Social media, connections and isolation
Social media may trigger depression by doing the opposite of what it was allegedly created to do: Fostering a sense of community and helping people maintain friendships.
Roger McFillin, board-certified in behavioral and cognitive psychology, warned that the rise of social media has caused some young people to become less socially adept, instead isolating themselves behind screens rather than experiencing real life firsthand.
To illustrate, sports participation has decreased significantly since 2008. According to the National Survey of Children’s Health, only 24 percent of six- to 17-year-olds engage in at least 60 minutes of physical activity per day, which is down from 30 percent a decade earlier. (Related: Poll: Parents most concerned about excessive use of SOCIAL MEDIA and mobile devices as kids return to school .)
After all, children and teens might feel less inclined to play a sport, which is often “physically, psychologically and relationally challenging,” when the alternative is social media, where you can have the illusion of participation without being challenged in many ways, added McFillin.
Research proves this disconnect. According to a 2023 study published in the journal Health Psychology and Behavioral Medicine , those using social media primarily to maintain relationships “feel lonelier than those using it for other reasons.”
The report revealed that even if social media facilitates social contact to a degree, it still does not “facilitate the type of contact sought by those who use social media primarily for this reason.” This supports previous findings that Facebook users are often lonelier than nonusers.
McFillin explained that “[g]enuine engagement occurs in person” and that excessive social media can often perpetuate feelings of loneliness, especially because heavy users may withdraw from the real world.
In a 2017 study published in the American Journal of Preventive Medicine , researchers reported that young adults who used social media excessively ” feel more socially isolated than their counterparts” who weren’t as active on social media.
While social media promises connection, it can’t replace in-person interaction. Additionally, overreliance on social media may undermine the real relationships humans need to feel connected to their loved ones.
A different study from 2023 published in the journal Brain Sciences backs this. For this study, scientists instructed 30 volunteers to list 20 of their loved friends or relatives, 20 loved influencers or celebrities and 20 people they felt no closeness to.
The volunteer’s brain activity was recorded via EEG as they viewed the names. Data showed that the brain wave response to loved ones was much greater than to influencers.
According to the researchers, brain imaging revealed that “there is nothing like a real friend.”
Read more news related to depression and mental health at DepressionSymptoms.news .
Watch the video below to learn about the negative side effects of social media addiction . Social Media Addiction Downside
This is a modal window.
No compatible source was found for this media.
This video is from the HappeningsandArt channel on Brighteon.com . More related stories:
10 Small changes that can help you deal with burnout .
British Education chief wants to BAN students from using phones in schools .
Parents and school officials of small Irish town unite to BAN SMARTPHONES for children as old as 13 . Sources include: TheEpochTimes.com PubMed.NCBI.NLM.nih.gov TAndFOnline.com AJPMOnline.org Brighteon.com
This Is The Largest Map of The Human Brain Ever Made
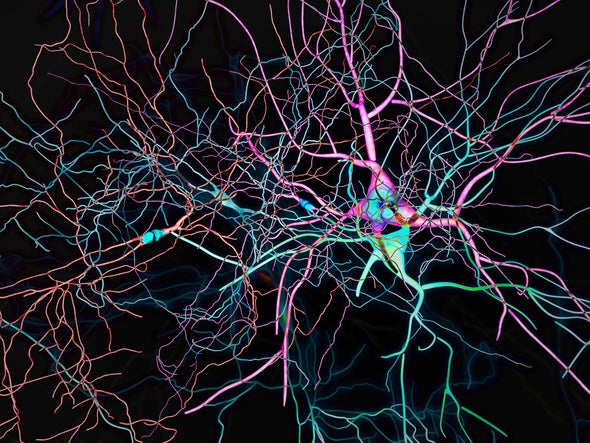
Insights into thousands of types of brain cell could improve understanding of diseases and cognition. Credit: Researchers have created the largest atlas of human brain cells so far, revealing more than 3,000 cell types — many of which are new to science. The work, published in a package of 21 papers today in Science , Science Advances and Science Translational Medicine , will aid the study of diseases, cognition and what makes us human, among other things, say the authors.
The enormous cell atlas offers a detailed snapshot of the most complex known organ. “It’s highly significant,” says Anthony Hannan, a neuroscientist at the Florey Institute of Neuroscience and Mental Health in Melbourne, Australia. Researchers have previously mapped the human brain using techniques such as magnetic resonance imaging, but this is the first atlas of the whole human brain at the single-cell level, showing its intricate molecular interactions, adds Hannan. “These types of atlases really are laying the groundwork for a much better understanding of the human brain.”
The research is part of the US National Institutes of Health’s Brain Research through Advancing Innovative Neurotechnologies Initiative — Cell Census Network (BICCN), a collaboration between hundreds of scientists. The programme’s goals include cataloguing brain cell types across humans, non-human primates and mice to improve understanding of the cellular mechanisms behind poorly understood brain disorders. The data from the 21 studies have been made publicly available on the Neuroscience Multi-omic Archive online repository. Cellular menagerie
Kimberly Siletti, a neuroscientist now at the University Medical Center Utrecht in the Netherlands, and her team laid the cornerstone for the atlas by sequencing the RNA of more than 3 million individual cells from 106 locations covering the entire human brain, using tissue samples from three deceased male donors. They also included one motor cortex dissection from a female donor that had been used in previous studies. Their analysis documented 461 broad categories of brain cell that included more than 3,000 subtypes. “I was surprised at how many different cell types there were,” says Siletti.
Neurons — cells in the brain and nervous system that send and receive signals — varied widely in different parts of the brain, suggesting different functions and developmental histories. The mix of neurons and other cell types also differed across each region; some cells were only found in specific locations. The brainstem — a relatively under-studied structure connecting the brain to the spinal cord — harboured a particularly high number of neuron types, says study co-author Sten Linnarsson, a molecular systems biologist at the Karolinska Institute in Stockholm, Sweden. “One of the big surprises here is how incredibly complex the brainstem is.”
Other studies drilled into the mechanisms of gene regulation and expression in different cells. Joseph Ecker, a molecular biologist at the Salk Institute for Biological Studies in La Jolla, California, and his colleagues investigated the brain through an epigenetic lens using tissue samples from the same three donors. They analysed chemical markers that switch genes on or off in more than 500,000 individual cells. The various molecules that acted as switches enabled the team to identify nearly 200 brain cell types. Even the same gene in the same type of cell could have different characteristics across the brain. One gene was turned on with one switch at the front of the brain and with another at the back. “There are remarkable regional differences,” says study co-author Wei Tian, a computational biologist at the Salk Institute.
Pinpointing the switches that activate or block gene expression in brain cells could be useful for diagnosing brain disorders and developing tailored treatments, says Ecker. “That’s another tool that comes out of the toolbox we’re building,” he says. Disease risk
Improving understanding of how genetic switches might contribute to disease risk was also a focus for Bing Ren, a molecular biologist at the University of California, San Diego, and his team. They analysed how more than one million brain cells from the three donors access and use genetic information. The researchers uncovered links between certain brain cell types and neuropsychiatric disorders, including bipolar disorder, depression and schizophrenia.
Ren and his colleagues used the cell-type data to predict how the genetic switches influence gene regulation and increase the risk of neurological diseases. For instance, in cells called microglia , which clear away dead or damaged cells, the presence of some genetic switches was strongly linked to risks of Alzheimer’s disease. Such findings can be used to test whether particular genes or faulty switches contribute directly to the onset of disease. “This is made possible because we have — for the first time — delineated the genetic switches for hundreds of different cell types,” says Ren.
The next step for the BICCN team is to sequence more cells from all parts of the brain, says Ren. The researchers will also work with more tissue samples to build a picture of how the human brain can vary across populations and age groups. “This is only the beginning,” says Ren.
This article is reproduced with permission and was first published on October 12, 2023. Sign up for Scientific American ’s free newsletters. ABOUT THE AUTHOR(S)
MICROPLASTIC INVASION: Researchers find microplastics in human heart tissue

Mike Adams – Israel & Hamas: What the HECK is Wrong With Our People? Advertisement
Microplastic pollution is a growing issue globally because of its negative effects on the environment, especially marine animals. These tiny plastic fragments persist in nature and have been shown to cause deleterious changes in fish and other ocean inhabitants when ingested, often resulting in their death.
Microplastics can also absorb harmful pollutants from the environment which they can transfer to the human food chain. Aside from contaminating seafood , microplastics enter the human body via plant- and animal-based foods, plastic food packaging and everyday products that contain or are made of plastic.
Over the years, studies have warned that microplastics can accumulate in human tissues and cause serious health problems , such as gastrointestinal disorders, immune and respiratory issues, chromosomal alterations and infertility.
More recently, alarming reports from around the world have emerged with direct evidence of the presence of microplastics in human blood samples and even in the hearts of cardiac surgery patients . Microplastics circulate in the human body
In a 2022 study published in the journal Environment International , researchers from the Netherlands successfully identified and quantified plastic polymers in blood samples taken from 22 healthy volunteers. They were testing a new sampling and analytical method which they developed specifically to measure plastic particles at least 700 nanometers in size in human blood.
Their analysis showed that “plastic particles are bioavailable for uptake into the human bloodstream,” with polyethylene terephthalate (PET), polyethylene (PE) and various polymers of styrene having the highest concentrations in the blood samples. The maximum concentrations measured for PET, PE and polystyrene (PS) in the blood samples were 2.4 micrograms (mcg)/milliliter (mL), 7.1 mcg/mL and 4.8 mcg/mL, respectively.
PE and PET are industrial plastics commonly used for packaging (e.g., plastic bags, films and bottles), while styrene polymers like PS can be found in medical products, electronics, food packaging and common household products. It should be noted that while research on the health risks associated with microplastics are limited, the presence of microplastics in human blood could be damaging to healthy tissues and organs, if studies on animals are anything to go by.
An earlier study reported that microplastics can “latch onto the outer membranes of red blood cells” and interfere with their ability to transport oxygen to vital organs. Meanwhile, studies on mice suggest that microplastics in the bloodstream could also breach the blood-brain-barrier and potentially increase a person’s risk of developing neurodegenerative disease. (Related: Study: Microplastics accumulate in the brain and cause behavioral changes associated with dementia .)
A recent study using cells derived from the human brain confirmed this risk, noting that weathered microplastics produced from the breakdown of microplastics in the environment by wind and ultraviolet light, can increase the activation of brain immune cells (microglial cells) and pathways that lead to neurodegeneration. Overactivation of microglial cells triggers severe brain inflammation, which is said to play a crucial role in the development and progression of neurodegenerative diseases like Alzheimer’s and Parkinson’s. Microplastics are infiltrating human organs
Aside from the brain, the heart and its surrounding tissues are also in danger of sustaining damage due to the presence of microplastics. In a study published in the journal Environmental Science & Technology , Chinese researchers reported detecting various microplastics in heart tissue samples collected from 15 cardiac surgery patients.
The tissues sampled included the pericardium , the membrane enclosing the heart; the epicardial adipose tissue , which is the fat depot located between the pericardium and the myocardium; the myocardium , or the cardiac muscle; the pericardial adipose tissue , the fat depot located outside the pericardium; and the left atrial appendage , an ear-shaped outpouching of the muscular wall of the left atrium that receives oxygenized blood.
The researchers found nine types of microplastics across the five types of heart tissue they collected, with the largest measuring 469 micrometers in diameter. They also detected nine types of microplastics with a maximum diameter of 184 micrometers in blood samples taken from the patients before and after cardiac surgery. (Related: Microplastics are EVERYWHERE: Yes, even in your gut and the food you eat, warn scientists .)
The researchers noted that the type and diameter distribution of microplastics in the blood samples varied before and after surgery, suggesting that some of the microplastics may have entered the patients’ bloodstreams during their operations . The researchers believe these microplastics came directly from the air in the operating rooms, citing previous research that reported the same happening.
On the other hand, they detected the presence of polymethyl methacrylate (PMMA), a transparent plastic used in car windows and smartphone screens, in samples taken from the left atrial appendage, epicardial adipose tissue and pericardial adipose tissue. The presence of PMMA in the samples cannot be attributed to accidental exposure during surgery, hence it provides “direct evidence of microplastics in patients undergoing cardiac surgery.”
“The detection of microplastics in vivo [in the living body] is alarming, and more studies are necessary to investigate how the microparticles enter the cardiac tissues and the potential effects of microplastics on long-term prognosis after cardiac surgery,” the study authors wrote in their report.
Although the present study is the first to report microplastics in the human heart, this is not the first instance researchers have found microplastics in a human organ. An earlier study published in the journal Science of The Total Environment reported finding airborne microplastics in human lung tissue samples . British researchers collected the samples from patients undergoing surgical resection for cancer or lung volume reduction surgery.
Using advanced infrared spectroscopy, the researchers identified 39 microplastics in 11 of the 13 lung tissue samples they analyzed. They noted that PET, resin and polypropylene, a commonly used thermoplastic, were the most abundant plastic polymers in the lungs of lung patients. Their findings prove that apart from ingestion, microplastics can also enter the human body via inhalation and accumulate in the lungs. Exposure to occupational levels of airborne microplastics in industrial settings has been shown to cause respiratory symptoms and […]
A new map of the human brain offers insights, clues to future treatments.
Ad:
Live
This is a modal window.
Beginning of dialog window. Escape will cancel and close the window.
End of dialog window.
This is a modal window. This modal can be closed by pressing the Escape key or activating the close button. In 21 papers published as a package Thursday, researchers have provided a new map of the human brain, refining the resolution, as one scientist described it, from a rough outline of a shoreline to a satellite view with topography.
They’re still far from a GPS guide to what’s inside our skulls. However, the new brain cell atlas offers more guidance for researchers desperate to find effective treatments for a wide range of disorders, including addiction, schizophrenia and Alzheimer’s.
The studies are part of the National Institute of Health’s BRAIN Initiative Cell Census Network, a five-year program launched in 2017 to create a catalog of brain cell types.
In the new studies, published Thursday in “Science” and related journals , the researchers identified more than 3,000 kinds of cells ‒ an order of magnitude beyond what scientists have known before.
“It’s the most complex cellular organ and we just haven’t had this basic understanding,” said Ed Lein, a senior investigator at the Allen Institute for Brain Science, who helped lead several of the studies. “If we don’t have a good understanding of the system, we’re not going to be able to treat diseases, to understand what really goes wrong.” Implications for disease research
These new maps are particularly useful for understanding the territory of brain diseases such as cancer, said Sten Linnarsson, a leader of some of the research and a professor of molecular systems biology at the Karolinska Institute in Sweden.
Cancer cells follow the same genetic programs found in normal brain cells, but in a distorted way, he said. Some cancer cells seem to repeat the pattern of early brain development, almost growing a new brain within a brain, he said. In other cancer cells, genes involved in wound healing are turned on, as if the brain senses there is something wrong and activates repair mechanisms.
We can get clues about how brain tumors behave, Linnarsson said, by comparing a brain with cancer to the “very organized architecture of the healthy, normal brain and brain development.”
Some of that was understood before, he said, but now researchers have a much higher resolution and more systematic map with a lot more cell types. Before, scientists could identify that there were cells called astrocytes involved; now, they can identify different kinds of astrocytes in different parts of the brain operating with different genetic programs.
“It will be the job for future work to figure out what that means for disease,” Linnarsson said.
Bing Ren, another research leader, said the brain atlas will allow researchers to compare healthy brains to the brains of people with neurological disorders, including schizophrenia, Alzheimer’s and addiction, and could eventually lead to advances in diagnoses and treatment.
Understanding which cells are involved and which genes are turned on and off in different brain conditions should allow more precise diagnoses for disorders that are now mainly identified by their symptoms, said Ren, also a professor at the University of California, San Diego. It can be difficult to test drugs for conditions like autism for which there is no objective diagnosis or measure of improvement; genetic analysis could provide that measure.
“The goal of the brain initiative is to really break that barrier and gain a fundamental understanding of the complex neurological disease mechanisms and to begin to develop strategies to mitigate such disorders,” Ren said. Delving deep into the brain
Just as sequencing the human genome was only the beginning of being able to understand the role of genes, so this map is just the first step toward understanding the brain, Ren said. “Interpreting the information is now the hard part.”
Every human brain has roughly 200 billion neurons ‒ the brain cells that send electrical signals.
When he was in college in the ’90s, Ren said, he was taught there were two types of neurons. In his new study, in which he and his colleagues examined 1.1 million brain cells, they found more than 90 different types of neurons ‒ but he suspects there might be thousands. “And we don’t have a very good idea of what they are and what they do.”
Plus, neurons are only one type of brain cell. Non-neuronal cells outnumber neurons by 5 or 10 to 1.
“We are looking at complicated brain maps and trying to gain a first glance of the variety of the cell types in the human brain in terms of their cell type identity, in terms of their anatomic locations and in terms of their connections among each other,” he said. “That’s a monumental job. We have to do it step by step.” Where the brains come from
Most brain research is done on tissue from people who agree to donate their brains after death.
Some of the studies in this package were also conducted on tissue donated by living patients who had brain surgery for epilepsy or cancer.
Laboratory tools now exist to enable never-before feasible genetic analysis of living tissue, said Lein from the Allen Insitute.”Part of what this package (of studies) is about is showing that the modern tools of the field that are normally only used in mouse can all now be applied to human,” he said. “It kind of opens up a whole new era of human neuroscience research where we can ask questions at a whole different level of granularity than has ever been possible.” How our brains compare to our cousins’ Several of the papers compared the human brain to the brains of our closest animal cousins, chimpanzees, gorillas, rhesus macaques, and common marmosets. Cell types are similar across primate brains, the studies found, but genetic activity differs among species.”The genes that really differentiate us from our closest relatives are related to the wiring of the brain and the function of neurocircuits,” Lein said.Evolution has sped up a bit in humans relative to primates, said Dr. Trygve Bakken, […]
Researchers unveil atlas of human brain
The ultimate goal of a new atlas of the brain released by researchers is to better understand the workings of the human brain — and what goes wrong in the range of neurological and psychiatric conditions that plague humans, from Alzheimer’s to depression to schizophrenia. Photo by cottonbro studio/Pexels After a massive five-year effort, researchers have unveiled an “atlas” that gives an unprecedented look at the intricacies of the human brain.
The atlas , which will be available to researchers everywhere, can be seen as similar to the atlases we all know: a book of maps.
But this one catalogues human brain cells and their striking diversity and complexity. Going forward, the atlas will help other researchers “navigate” the brain, said Bing Ren , a professor at the University of California, San Diego, who was part of the research effort.
The atlas encompasses more than 3,000 types of brain cells, and gives insight into how they vary from one person to another, how they differ from non-human primates’ brain cells, how particular brain cell types are related to specific diseases, and more.
The ultimate goal, Ren and other experts said, is to better understand the workings of the human brain — and what goes wrong in the range of neurological and psychiatric conditions that plague humans, from Alzheimer’s to depression to schizophrenia.
The publication of the brain cell atlas, Ren said, “is just the beginning.”
The work is detailed in a collection of 21 papers being published Friday in the journals Science, Science Advances and Science Translational Medicine. In all, the project involved hundreds of scientists from different countries, brought together under the U.S. National Institutes of Health’s BRAIN Initiative program.
The ambitious project was possible thanks to new technology that allows scientists to study features and functions of individual cells.
That kind of deep understanding of brain cells could eventually lead to new, highly targeted treatments for neuropsychiatric conditions — including ones no one has thought of yet, said Dr. Panos Roussos , a professor at Mount Sinai’s Icahn School of Medicine in New York City, who worked on the project.
Many current medications for those diseases target neurotransmitters, chemicals that help brain cells communicate.
They help many people, but also “leave many others behind,” said Dr. Jeffrey Borenstein , president of the nonprofit Brain and Behavior Research Foundation in New York City.
Borenstein, who was not involved in the atlas project, called it “very important work.”
“It lays the foundation for scientists to better understand how the brain works, in both health and states of disease,” he said. “I think this offers tremendous hope for people who are living with psychiatric illnesses.”
Human brain cells, it’s fair to say, are diverse and complex. Each cell in the brain has the same DNA sequence, but different cell types use different genes, and in different amounts.
To give it an analogy, Ren said brain cells can be regarded as people living in different parts of the world: Depending on where they end up residing in the brain, they speak different languages.
A broad goal, Ren and Roussos said, is to better understand how those different brain cell types interact with one another, in health and in sickness, and to identify the cell types that are relevant to any given disease.
In their study, Ren’s team analyzed three human brains, looking in detail at more than 1 million cells in 42 brain regions. They identified 107 different brain cell subtypes, then were able to correlate certain aspects of cells’ molecular biology to specific diseases — including schizophrenia, bipolar disorder and Alzheimer’s disease.
Roussos and his colleagues, meanwhile, studied brain tissue from across the life span, from fetal development to adulthood. That’s critical, Roussos said, since different neuropsychiatric conditions have different ages of onset.
They, too, were able to map certain brain cell types to specific diseases. That included associations that were previously unknown — including linking Tourette syndrome to cells called oligodendrocytes and obsessive-compulsive disorder to astrocytes.
“If you know which cell type is related to a disease, then you can make hypotheses on causes,” Ren said.
He noted that his work, like some studies before it, point to the importance of cells called microglia in Alzheimer’s. Microglia are resident immune cells in the brain, and Ren and other researchers suspect that an abnormal set of “super-activated” microglia play a central role in causing Alzheimer’s, by attacking the brain’s neurons.
“So is there some way we can tone down that over-activation?” Ren said.
Among the project’s other findings: Researchers at the Allen Institute for Brain Science, in Washington, D.C., and other centers studied which genes are “turned on” in individual cells in the human brain — allowing them to categorize more than 3,000 different kinds of brain cells.
Individuals vary widely in their proportions of different kinds of brain cells, and in which genes are active within those cells.
Humans share the same basic brain cell type “architecture” with our closest primate relatives, chimpanzees and gorillas. Where we differ is in which genes those cells “use.” Specifically, those differences are seen in genes that allow brain cells to connect and form circuits.
In a statement, Dr. John Ngai , director of the NIH BRAIN Initiative, said the program’s scientific collaborations are “propelling the field forward at an exponential pace.””The progress, and possibilities, have been simply breathtaking,” he said. More information The U.S. National Institutes of Health has a primer on brain basics. Copyright © 2023 HealthDay. All rights reserved.
Cellular Map of Entire Brain Reveals What Makes Us Human

Summary: A groundbreaking suite of 21 papers has unveiled a momentous leap in our understanding of the brain, spotlighting the intricate cellular composition of human and primate brains through a consortium led by the BRAIN Initiative.
Utilizing innovative single-cell transcriptomics, researchers illuminated a stunning array of over 3,000 different brain cells and their distinctive functionalities. This extensive research not only dives into the distinctiveness of the human brain but also pioneers a suite of scalable techniques that offer an unparalleled, detailed organization view of the brain.
This pivotal moment in neuroscience sets a promising stage for the next phase in cellular census efforts, propelling towards a more profound understanding of the brain’s complexity and functionality.
Key Facts:
> Vast Cellular Diversity: Scientists discovered an astonishing array of more than 3,000 different kinds of brain cells through a technique called single-cell transcriptomics.
Global Collaboration: This massive research effort involved hundreds of scientists worldwide and is funded by the National Institutes of Health’s BRAIN Initiative, aiming to explore and catalog the complex cellular makeup of primate brains, including humans.
Comparative Study: The research also undertook a comparative study between human brains and those of our closest ape relatives, revealing both shared cellular architectures and significant variances in gene utilization within neuron connections and circuit formations.
Source: Allen Institute
Scientists have just unveiled a massive effort to understand our own brains and those of our closest primate relatives.
In a suite of 21 papers published today in the journals Science (12) , Science Advances (8) , and Science Translational Medicine (1) , a large consortium of researchers shares new knowledge about the cells that make up our brains and the brains of other primates. It’s a huge leap from previously published work, with studies and data that reveal new insights about our nervous systems’ cellular makeup across many regions of the brain and what is distinctive about the human brain.
The research consortium is a concerted effort to understand the human brain and its modular, functional nature. It was brought together and is funded by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies ® (BRAIN) Initiative.
Hundreds of scientists from around the world worked together to complete a range of studies exploring the cellular makeup of the human brain and those of other primates, and to demonstrate how a transformative new suite of scalable techniques can be used to study the detailed organization of the human brain at unprecedented resolution.
Understanding our brain at the cellular level is key to understanding how our brains function and who we are as a species, as well as more accurately pinpointing the cellular roots of brain diseases and disorders—knowledge that could ultimately lead to better treatments for those diseases.
Scientists at the Allen Institute for Brain Science, a division of the Allen Institute, led five of these studies and made significant contributions to three others, including a study that greatly expands on existing knowledge about the number of types of cells in the adult human brain.
Scientists at Karolinska Institute and the Allen Institute studied the genes switched on in individual brain cells, a technique known as single-cell transcriptomics, revealing an astonishing diversity of cell types: we have more than 3,000 different kinds of brain cells.
“I view this as a pivotal moment in neuroscience, where new technologies are now allowing us to understand the very detailed cellular organization of the human brain and of other primate brains,” said Ed Lein, Ph.D., Senior Investigator at the Allen Institute for Brain Science, who led several of the newly published studies.
“At its core, this body of work is a triumph of molecular biology: Differential gene usage can be used to define cell types, and the tools of genomics could be used to create the first drafts of high-resolution, annotated maps of the cells that make up the entire human brain.”
The studies also tackle a range of important questions such as: How different are individual people’s brains at the cellular level? How different are our brains from those of our closest ape relatives? How many kinds of brain cells do we have? What are the properties of these cells? How do these cells emerge and mature in development?
Building off previous work mapping brain cell types in high resolution in single regions of the human cortex, the outermost shell of the brain, the newly published package expands those studies to dozens up to a hundred regions across the entire brain.
Where the single region studies found over 100 different brain cell types, the newly released data shows thousands of different kinds of brain cells across the entire brain. For many parts of the brain, that complexity and variety had never before been described.
These studies are part of the NIH’s BRAIN Initiative Cell Census Network, or BICCN, a five-year funding program that was launched in 2017 to create a catalog of brain cell types. This body of work demonstrated the scalability of cutting edge cellular and molecular approaches to tackle the challenges of size and complexity of the human brain, and has set the stage for the next phase of this cell census effort.
This next phase, part of which is underway at the Allen Institute, will build much more comprehensive atlases of human and other primate brains through the BRAIN Initiative’s Cell Atlas Network, or BICAN.
“The present suite of studies represents a landmark achievement that continues to build an important bridge toward illuminating the complexity of the human brain at the cellular level,” said Dr. John Ngai, Director of the NIH BRAIN Initiative.
“The scientific collaborations forged through BICCN, and continuing in the next phase in BICAN, are propelling the field forward at an exponential pace; the progress – and possibilities – have been simply breathtaking.”
The human studies used postmortem tissue from people who had donated their brains to science, as well as healthy living tissue donated from patients who had undergone brain surgery and donated tissue to research.
The data from the newly released studies will also feed into the Human Cell Atlas, an international effort that […]
Digital Twin Brain: A bridge between biological and artificial intelligence
Recent developments in neuroscience and brain-inspired artificial intelligence have opened up new possibilities in understanding intelligence. Now, a research team led by Tianzi Jiang at the Institute of Automation of the Chinese Academy of Sciences has outlined the key components and properties of an innovative platform called the Digital Twin Brain, which could bridge the gap between biological and artificial intelligence and provide new insights into both. This research was published Sept. 22 in Intelligent Computing, a Science Partner Journal.
Network structure is something that biological and artificial intelligence have in common. Since the brain consists of biological networks, a digital model or “twin” of the brain built using artificial networks would allow researchers to feed knowledge about biological intelligence into the model. The ultimate goal is to “propel the development of artificial general intelligence and facilitate precision mental healthcare,” a feat calling for joint efforts from interdisciplinary scientists worldwide.
Using the Digital Twin Brain, researchers could explore the working mechanisms of the human brain by simulating and modulating the brain in different states for various cognitive tasks. For example, they could simulate how the brain functions properly in a resting state and how it malfunctions in disorders, or develop methods to shift it away from an undesirable state by modulating its activity.
Despite sounding like science fiction, the idea of the Digital Twin Brain stands on solid biological ground. It integrates three core elements: brain atlases serving as the structural scaffolds and biological constraints, multi-level neural models trained on biological data to simulate brain functions, and a spectrum of applications for evaluating and updating the current “twin.”
The three core elements are envisioned to evolve and interact in a closed loop. A dynamic brain atlas leads to improved neural models that generate more realistic function simulations. The current “twin,” consisting of these models, is then validated across an ever-expanding spectrum of practical applications, including disease biomarker discovery and drug tests. These applications complete the cycle by providing feedback to enhance the brain atlas.
The biological brain has intricate structures and complex dynamics. Therefore, highly nuanced brain atlases, including atlases at different scales, of multiple modalities, and even from different species, are needed for learning how to build its digital twin. With a comprehensive collection of atlases, various aspects of the brain, and the connections and interactions between different brain regions, as well as the fundamental principles of brain organization, can be explored in depth.
On the other hand, brain atlases are also constraints in the sense that neural models must be based on them for “biological plausibility,” and that poses technical challenges.
Jiang’s team suggests that the Brainnetome Atlas will be an important component for developing the Digital Twin Brain. Announced by researchers at the Institute of Automation of the Chinese Academy of Sciences in 2016, this atlas is a macroscale atlas encompassing 246 brain sub-regions and has been evolving towards an “extensive and detailed mapping” of the structure and connectivity of the human brain.
Meanwhile, given that existing brain simulation platforms fall short of their anatomical basis, the authors believe it is vital to design “an open-source, efficient, flexible, and user-friendly brain atlas-constrained” platform that is powerful enough to support multiscale and multimodal modeling. There are still many open questions to be addressed, such as how to effectively weave bits and pieces of biological knowledge into a digital twin, how to design better models for simulations, and how to integrate the Digital Twin Brain into practical scenarios.
In summary, the Digital Twin Brain represents a convergence of neuroscience and artificial intelligence. By integrating intricate brain atlases, dynamic neural models, and a multitude of applications, this platform is poised to revolutionize our grasp of both biological and artificial intelligence. With the collective efforts of scientists worldwide, the Digital Twin Brain holds the promise of advancing artificial general intelligence and revolutionizing precision mental healthcare, paving the way for transformative breakthroughs in our understanding of the human mind, the development of intelligent technologies, and the discovering of therapeutics for brain disorders.
Source:
Intelligent Computing
Journal reference:
Xiong, H., et al. (2023) The Digital Twin Brain: A Bridge between Biological and Artificial Intelligence . Intelligent Computing. doi.org/10.34133/icomputing.0055 http://doi.org/10.34133/icomputing.0055 .
BRAINSTORM: ‘Invisible’ brain disorder patients finding solutions at Aurora institute

Dr. Colin Buchanan goes over X-rays with patient Allison Reed, Sept. 28 at the Colorado Chiari Institute in Aurora. Dr. Buchanan executes approximately 50-75 surgeries a year correcting Chiari malformations. Photo by PHILIP B. POSTON / Sentinel Colorado. AURORA | Growing up, Allison Reed thought the shooting pain she experienced whenever she laughed, coughed or sneezed was nothing to worry about.
The pain raced down her neck and back. Since no one could explain the symptoms, she tried her best to shrug them off.
“You kind of think to yourself, maybe it’s normal,” Reed said. “Maybe everybody feels this level of pain when they’re coughing or laughing.”
In 2013, the Longmont mother of three suffered a head injury, and began experiencing migraine headaches that were not as easy to ignore.
An MRI of her injury showed that she also had a Chiari malformation — a developmental disorder that causes part of the brain to protrude out of the gap between the skull and the spine — but since her doctors were unfamiliar with the problems caused by the condition, they did not make a connection at the time between Reed’s headaches and her Chiari.
In 2022, Reed experienced two concussions back-to-back, and the once-occasional migraines turned into a nonstop barrage of debilitating neurological symptoms.
She was constantly nauseous and stopped eating, losing about 50 pounds. The pain in her head, neck and shoulder made it hard to sleep. She would stutter and hiccup uncontrollably, and she began to develop memory problems and had difficulties walking and swallowing.
The problems escalated to the point that she was forced to quit her job providing respite services for people with disabilities.
“I would almost compare it to having a brain injury,” she said. “I was so forgetful, and just so out of it, and I couldn’t function. I slept all the time, and I’m a mom of three. I can’t sleep all the time. I have to get up and take care of my kids…I couldn’t survive, and I kept trying to get help, and I kept getting turned away.”
Reed went to the emergency room, saw multiple doctors and was prescribed medication for her headaches. The symptoms continued and grew worse.
She said it was ultimately social media that led her to information about the effects of Chiari malformations and the Aurora practice of neurosurgeon Colin Buchanan, who leads the Colorado Chiari Institute at the Medical Center of Aurora.
Buchanan is one of a small number of surgeons in the region who specializes in treating Chiari malformations, and the Colorado Chiari Institute is similarly unique for its focus on a brain disorder that is widely known but not well understood by many medical practitioners.
Buchanan operated on Reed in February, removing one of her spinal vertebrae and inserting a metal plate in a procedure known as Chiari decompression surgery. Since then, Reed said her headaches and other symptoms have only improved.
“The biggest thing that I cried about and was shocked about was that I could feel each of my fingers, and I could feel my toes,” she said. “It’s completely changed my life. I’m able to go back out and be active again. I’m able to go hiking. I’m able to keep up with my kids. And that’s all because he knew how to treat this.” Dr. Colin Buchanan points to the location of a Chiari malformation on an X-ray, Sept. 28 at the Colorado Chiari Institute in Aurora. Chiari care gets a home in Colorado
In the early 2000s, neurosurgeon John Oro established the Colorado Chiari Institute at the Medical Center of Aurora, focusing on the brain disorder that is estimated to impact about 0.1% of the U.S. population, according to the American Association of Neurological Surgeons.
Many of those people don’t go on to develop symptoms. But for others, the pinching of the exposed section of brain between the skull and spine causes a buildup of fluid in the spinal cord as well as symptoms that can be crippling.
Buchanan said Oro’s work with Chiari patients inspired him to join the clinic. Oro has since retired, and for the past year, Buchanan has been the institute’s sole neurosurgeon.
“At the moment, we’re one of two or three centers like this in the U.S.,” he said. “What we’re trying to do is offer expertise in a condition that affects more people than we think. And we’re trying to take an approach that’s comprehensive and not just ruling people in or out for surgery. We’re trying to help guide people through this process, and educate them, and help them determine a treatment plan that makes sense for them. And that may or may not include surgery.”
Buchanan said the treatment options presented to patients depend on the presence of fluid-filled cysts called syrinxes on the spinal cord, which are caused by the blockage of spinal fluid. He said the condition can inflict permanent neurological damage if left unchecked.
For patients who don’t have a syrinx, he said non-surgical treatments such as physical therapy and botox injections can help manage the symptoms of Chiari. But for patients with a syrinx, Buchanan said he believes there “isn’t an acceptable alternative” to surgery.
After years of dealing with symptoms that had forced her to quit her job and impacted her ability to be present with her children, Reed said she was relieved when Buchanan recommended decompression surgery.
“It’s what I was hoping for,” she said. “I knew I needed it. And I felt like I won the lotto when he told me that I got to have brain surgery, which I know sounds crazy, but that’s where I was at. I hugged him because I was just so grateful that he was willing to treat me and take me on as a patient.”
Buchanan, who said he’s on track to perform between 50 and 75 decompression surgeries this year, also said Reed wasn’t alone in struggling to find medical professionals who understood the ins and outs of Chiari.
“I think it requires some exposure to this to understand what Chiari means for patients,” he […]
Nissan Used A Brain Stimulator To Improve Its Formula E Drivers’ Performance And It Worked!

Once the stuff of sci-fi novels and futurists’ ramblings, the idea of stimulating the brain with an external device to improve cognitive function has actually been found to work by Nissan, after its Formula E drivers became guinea pigs for the Brain to Performance program.
During the most recent season of the all-electric open-wheel racing series, Nissan hooked its factory drivers up to a “Sonal device.” This uses certain frequencies to target specific areas of the brain. That may sound like technobabble, but the device’s impacts can be profound.
Wave Neuro, the company behind the Sonal device, has also worked with the U.S. military and football players to help with things like PTSD and brain injuries. It can also be used for less serious conditions, like jet lag and sleep deprivation.
Read: Rats Were Taught By Scientists How To Drive Mini Cars – And They Found It Relaxing!
Working with Wave Neuro, the University of Texas at Austin, as well as Nissan’s senior manager for UX innovation, Dr. Lucian Gheorghe, a special training protocol was developed for the team’s Formula E drivers, and the results are promising.
After using it for the 2022-2023 season, the researchers found that the drivers’ brain speed and clarity supported the hypothesis that the device could improve their performance on track. With further training, they found that the Sonal device could help the drivers improve their lap times, and make fewer mistakes during a race.
“The results following the training program are extremely exciting and demonstrate that with the right tools we can help our drivers reach their full potential,” said Tommaso Volpe, the managing director of Nissan’s Formula E team. “It is thrilling to be pioneers in this area of research within the world of motorsport. Nissan prides itself on daring to do what others don’t.”
Nissan says that the results of this research are likely to extend beyond its Formula E team into the rest of its racing programs. But it’s not just professional drivers that this sci-fi technology may be able to help.
“Following these encouraging results, we believe this technology could provide a substantial benefit far beyond the world of motorsports,” said Dr. Gheorghe. “We are excited to uncover further opportunities for this to be used in Nissan’s electric vehicles of the future.”
In fact, before hooking the Formula E drivers up to the brain stimulator, Dr. Gheorghe worked with the University of Essex and the Campus Biotech in Geneva, Switzerland. There, the team hooked drivers up to a brain stimulator and put them in a sim racing rig where they were asked to complete 10 sessions on a track they had never seen before. They were able to learn tracks 50 percent faster, and lap the track 50 percent quicker, than drivers who hadn’t had their brains stimulated.
Nissan believes that its research shows that even regular drivers, not just professional drivers, can benefit from this technology. As a result, it is exploring how it could be integrated into its dealerships to help customers improve their driving skills. That’s just the beginning, though. Nissan believes that there are plenty of new and exciting ways that brain stimulation could be applied in the future.
AI helps neurosurgeons identify brain tumor types on the spot
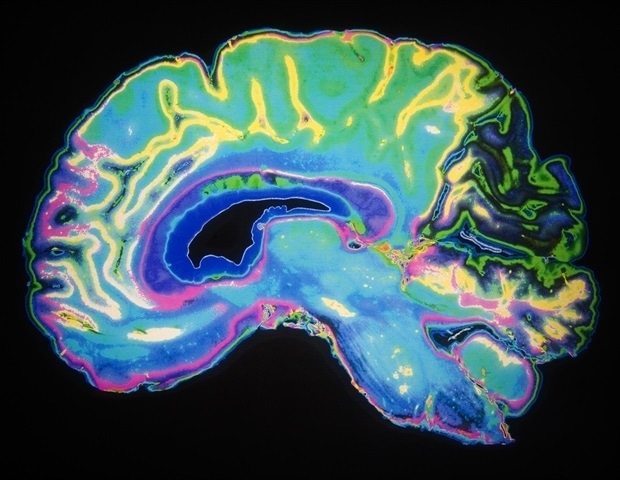
What type of brain tumor does this patient have? AI technology helps to determine this as early as during surgery, within 1.5 hours. This process normally takes a week. The new technology allows neurosurgeons to adjust their surgical strategies on the spot. Today, researchers from UMC Utrecht and researchers, pathologists and neurosurgeons from the Princess Máxima Center for pediatric oncology and Amsterdam UMC have published about this study in Nature .
Every year, 1,400 adults and 150 children are diagnosed with a tumor in the brain or spinal cord in the Netherlands. Surgery is often the first step taken in treatment. Currently, during surgery, neurosurgeons do not precisely know what type of brain tumor and what degree of aggressiveness they are dealing with. The exact diagnosis will usually only be available one week after surgery, after the tumor tissue has been visually and molecularly analyzed by the pathologist. Deep-learning algorithm
Researchers from UMC Utrecht have developed a new ‘deep-learning algorithm’, a form of artificial intelligence, which significantly speeds up diagnosis. Recently, Nanopore sequencing became available: a technology that helps to read DNA in real time. For this, we developed an algorithm that is equipped to learn from millions of simulated realistic ‘DNA snapshots’. With this algorithm, we can identify the tumor type within 20 to 40 minutes. And that is fast enough to directly adjust the surgical strategy, if necessary.” Jeroen de Ridder, research group leader, UMC Utrecht and Oncode Institute Tested and trained with biobank
Bastiaan Tops is in charge of the Pediatric Oncology Laboratory at the Princess Máxima Center. He brought together the new technology and the needs from the operating room. This was made possible by funding from the KiKa foundation and, more specifically, to the extensive biobank that the Máxima Center has maintained for years. Among other things, this biobank stores tissue from children with brain tumors. The algorithm was trained and tested using the biobank.
“That we can now determine the type of brain tumor as soon as during surgery shows how technology can speed up diagnostics. And how we can use an existing biobank to develop new technology”, Tops says. Used during surgery
Consequently, the whole procedure was also carried out several times during actual brain surgeries, from taking the tissue in the operating room to determining the tumor type. In Utrecht, this happened with children, and in Amsterdam with adults. Total length of the procedure: 60 to 90 minutes.
The Princess Máxima Center has decided that the results of the technique are sufficiently reliable and is already using it with children for whom the outcome may determine the surgical strategy. Amsterdam UMC will also use the technique in daily practice, to help them speed up diagnosis.
Eelco Hoving, pediatric neurosurgeon and clinical director of neuro-oncology at the Máxima Center, is excited about the possibilities of DNA analysis during surgery: “During surgery, a small remnant of tumor tissue is sometimes deliberately left behind to prevent neurological damage. But if it will later turn out, for example, that the tumor is very aggressive, a second surgery may still be necessary to remove that last remnant. This will again create risks and stress for patients and their families. This can be avoided now because we will already know during the first surgery what type of tumor we are dealing with.”
Jeroen de Ridder: “It is wonderful that we have been able to actually make the step into clinical practice by combining all areas of expertise, from basic researchers to pathologists and surgeons. By doing so, we can help surgeons to optimize the outcome of brain tumor surgery.” Comparative research
To use the new technique even more widely and structurally, more research is needed. For instance, more tumor types should be added to the algorithm. In this way, international standards will be met, allowing comparison of data. Also, the outcomes of the new and current (lengthier) method will be further compared, in collaboration with other (inter)national centers. This should make clear whether the new method will also contribute to patients’ quality of life in the long term.
Source:
University Medical Center Utrecht
Journal reference:
Vermeulen, C., et al. (2023) Ultra-fast deep-learned CNS tumour classification . Nature. doi.org/10.1038/s41586-023-06615-2 .
Neuralink implant RUPTURED the brain of a female monkey, autopsy finds… what will happen when they are implanted into humans?

Advertisement
An autopsy report has confirmed that a Neuralink implant ruptured the brain of a female macaque during an experiment, forcing scientists to end its suffering.
According to an Oct. 4 report by Wired magazine , the implant “deformed and ruptured” the brain of the test animal after an experiment caused severe cerebral swelling. The 2018 experiment done at the University of California, Davis ‘ (UC Davis) California National Primate Research Center (CNPRC) left the seven-year-old monkey with “severe neurological defects.”
Researchers realized that the test animal was in a terminal state after noting the severity of its brain swelling. But instead of ending its suffering, the scientist overseeing the experiment insisted that the monkey be kept alive another day. Wired then recounted the animal’s torturous final 24 hours before being put down.
“The monkey seized and vomited; [its] pupils reacted less and less to the light. [Its] right leg went limp, and [it] could no longer support the weight of [its] 15-pound body without gripping the bars of [its] cage,” the magazine wrote. “Sometimes [the monkey] would wake and scratch at [its] throat, retching and gasping for air before collapsing again, exhausted.”
An anonymous former Neuralink employee disclosed: “If you want to split hairs, the implant itself did not cause death. We sacrificed her to end her suffering.”
An autopsy disclosed the reason behind the monkey’s suffering. A “toxic adhesive” from the implant leaked internally, causing inflammation and “painful pressure” on a part of the monkey’s brain that secretes cerebrospinal fluid. The effects were so severe that the rear part of the monkey’s brain protruded from its skull.
The results of the experiment opened up Neuralink, which is headed by Elon Musk, to potential legal actions under the Animal Welfare Act. But the CNPRC had proactively reported the violation to authorities, thus it could not be legally cited. Ethics group demands TRANSPARENCY from Neuralink
The incident of the Neuralink monkey’s gruesome consequence as a result of the implants was among the records obtained by Wired . But the magazine noted that this may not be the only instance of monkeys suffering from such experiments as UC Davis has a tight grip on records being released to the public.
In October 2022, the Physicians Committee for Responsible Medicine (PCRM) sued UC Davis in an attempt to gain access to records of Neuralink’s work with the CNPRC, including videos and documents. It argued in California state court that the public has the right to know about any suffering resulting from taxpayer-funded animal tests, given that UC Davis is a public institution. The lawsuit filed in the Yolo County Superior Court is ongoing.
Corey Page, PCRM’s legal counsel, said disclosure of information regarding these monkey experiments “is particularly important because Neuralink actively misleads the public about, and downplays the gruesome nature of, the experiments.”
Despite the lawsuit, the university remains adamant about refusing to release documentation about the female monkey that died during Neuralink’s experiments. It argues that the public is simply unequipped to properly interpret the photographs. Moreover, it also claims that the backlash caused by the content of the photos would not only endanger the scientists but discourage them from taking such photos in the first place.
“Nevertheless, the negative press hasn’t deterred Neuralink from going ahead with human trials,” Futurism ‘s Frank Landymore wrote in an Oct. 7 piece. He pointed out, however, that “the outcome of the [PCRM’s] lawsuit may cast a long shadow over those experiments.” (Related: FDA rejects Elon Musk’s bid to test Neuralink brain implants in humans. )
Visit MedicalExperiments.news for more stories about Neuralink’s experiments with monkeys.
Watch this video of researchers implanting a Neuralink device onto a monkey’s brain . Neuralink Brain Chip Experiment
This is a modal window.
No compatible source was found for this media.
This video is from the Covid Times channel on Brighteon.com . More related stories:
Neuralink brain chip implants to be tried on humans despite causing MULTIPLE DEATHS in animal trials.
Elon Musk’s medical device company Neuralink facing federal investigation over animal testing.
Ethical questions raised after Elon Musk’s Neuralink company implants chip in monkey’s brain.
Elon Musk accused of “mutilating and killing monkeys” in gruesome Neuralink experiments.
Sources include:
Futurism.com
Wired.com
Brighteon.com
18 Ways to Improve Your Mood & Reset Your Headspace in 5 Minutes or Less

When you’re feeling tired, annoyed, or downright sad for no reason—at least a reason that makes sense—it can be difficult to move past it. While therapy can help long-term, I’ve always wondered if there are quick things to do in the moment to shift your headspace before you enter a complete downward spiral. After speaking to a panel of experts, turns out that yes, sometimes shaking things up can shake you out of a negative mindset. Try these 18 tips for re-energizing your mind, body, and spirit , all within five-minutes or less.
Before you get the impression these tips are designed to be an instant cure-all for every bad feeling on the rainbow, keep in mind that all emotions on the spectrum serve a vital purpose to your experience as a human being. These darker and more frustrating emotions help us understand ourselves on a more intrinsic level, pointing to what may be ailing us in ways we may yet not be aware of. And because life is filled with high highs and low lows , you can’t always expect yourself to be able to easily reset your mood with the flip of a switch. Like all of us, you may need to reach out to a therapist or counselor to help yourself process some deeper issues.
More from StyleCaster 6 Smart Ways to Handle Online Bullying, Including the Block Button
How to Deal With the Stress of an Uncertain Future When You’re Generally Unwell
What Do You Have in Common With an Influencer & A Therapist? A Comfort Outfit
However, for those days you just wake up on the wrong side of the bed for no perceivable reason, sometimes all really need to do is try something different. Remember, you are a human being, and by making a point to activate, refresh, and heal your mind and body, you may be able to flush out some of the stale sadness lingering in your joints. After all, your mental health concerns may be coming from boredom, tiredness, or sheer hunger. Here are 18 research-based and expert-approved ways to improve your mood or reset your headspace in five-minutes or less: 1. Be present.
Click here to read the full article.
Whenever you’re feeling sad or anxious, there’s a good chance you may be obsessing over the future or spending too much time reliving your the past. Finding a way to bring yourself back to the present can help you let go of worries or fears that are not rooted in your current reality. Natalie Jambazian M.D., a Sherman Oaks-based licensed marriage and family therapist , recommends the 5-4-3-2-1 method: “Sit in a comfortable area, whether this is in your car or at home and describe five things you see, four things you hear, three things you smell, two things you taste and one thing you smell. This is a wonderful grounding exercise to help stay in the present moment.”
Wendy Schofer M.D., a holistic pediatrician and founder of Family in Focus , recommends focusing on the sensory vibrations that surround you. An example: When eating an apple, “focus on the texture, the taste, the temperature,” she explains. “The focus on the external can help shift your state from focusing on the internal.” 2. Feel your emotions.
Allow yourself to feel whatever you’re feeling. Give yourself permission to cry. It’s important to remember that negative emotions are not to be shunned or ignored, because they’re all part of the natural flow of life.
Shofer also tells StyleCaster that avoiding or repressing the difficult feelings associated with life can create even more obstacles in the long run. She explains: “I practice getting curious about what I am feeling, really going into my body and feeling the vibrations of the emotion,” she says. “I welcome the emotion because it is telling me something important. When we listen to the emotions, welcome and feel them, they can pass through on their journey. That’s how processing is done, in a nutshell. Trying to make it go quicker or resist feeling emotions in the moment can make it harder and perpetuate emotions to become bad moods.” 3. Write it down.
If your mind is overwhelmed by confusing thoughts and concerns, write everything down and get it out of your system, suggests Dr. Jambazian. She explains that you should: “Make it a habit to journal your thoughts and feelings ,” she says. “This will help externalize your emotions and feelings rather than internalize them.” Even setting a timer for five minutes and writing down a stream of consciousness can provide immense relief. 4. Do a breathing exercise.
It’s your body’s natural instinct to inhale and exhale, but conscious and intentional breathing can do wonders for releasing negativity, resetting your headspace, and uplifting your mood.
Maria Andrews, a yoga teacher and the managing editor at Broadsea Media Co. , recommends something called “box breathing”. Influenced by traditional yogic pranayama, this calming technique that is accessible to anyone. The how-to, courtesy of Andrews Close your eyes and visualize a box.
Clockwise, trace the left side of the box in your mind’s eye, breathing in for four seconds,
Trace the top of the box, holding your breath for four seconds as you do that.
Trace the right side of the box, breathing out for four seconds.
Trace the bottom edge of the box, holding your breath again for four seconds.
Repeat this for a few minutes, noticing your body relax as you go.
“By focusing on consciously extending and slowing down the breath, your heart rate slows and you activate your parasympathetic nervous system,” Andrews explains. “This puts your body in a physiologically calmer state called the ‘rest and digest state.” This, in turn, can create a positive feedback loop, positively affecting your mental landscape.”
Another breathing option: “Voo Breathing.” Sarah Rollins, owner & licensed therapist at Embodied Wellness PLLC , “loves this exercise “because it stimulates the vagus nerve, which creates a sense of […]
AI Uncovers Secrets of Brain Aging

Summary: Utilizing artificial intelligence, researchers developed “HistoAge,” an algorithm predicting age at death and unraveling the enigmas of brain aging and neurodegenerative disorders.
By analyzing nearly 700 digitized hippocampal sections from elderly brain donors, the tool forecasts age with striking accuracy and identifies regions susceptible to age-related changes. Remarkably, HistoAge demonstrated a potent correlation with cognitive impairment and Alzheimer’s-type abnormalities, providing a reliable metric for exploring neurodegenerative progression.
This innovative model presents a transformative lens for understanding the aging brain, marking a substantial stride toward decoding and potentially curbing age-accelerated neurodegeneration.
Key Facts:
> Innovative Aging Prediction: The HistoAge algorithm predicts age at death with an average accuracy of within 5.45 years by analyzing the cellular composition of human brain tissue specimens.
HistoAge and Neurological Associations: HistoAge-based age acceleration shows strong associations with cognitive impairment, cerebrovascular disease, and Alzheimer’s-type protein aggregation, outpacing current age acceleration measures like DNA methylation.
AI as a Revolutionary Tool: Not only does HistoAge offer a novel paradigm in evaluating aging and neurodegeneration in human samples, but it also brings forward a robust and unbiased metric that is deployable at scale in research labs, thereby facilitating a deeper understanding of cellular changes underlying degenerative diseases.
Source: Mount Sinai
The aging brain undergoes structural and cellular changes that can impact function and increase susceptibility to neurodegenerative disorders like Alzheimer’s disease.
Age acceleration—or the differences between biological and chronological age—in the brain can reveal insights about mechanisms and normal functions of one of the body’s most important organs. They used the difference between the model-predicted age and actual age to derive the amount of age acceleration in the brain. Credit: Neuroscience News It can also explain age-related changes and functional decline, as well as identify early changes related to diseases, indicating the onset of a brain disorder.
Mount Sinai researchers say they have, for the first time ever, used AI to develop an algorithm they term “HistoAge” which predicts age at death based on the cellular composition of human brain tissue specimens with an average accuracy of within 5.45 years. This powerful tool can also identify neuroanatomical regions vulnerable to age-related changes, an indicator of potential cognitive diseases.
How :
The researchers examined a collection of almost 700 digitized images of slides with human hippocampal sections from aged brain donors to develop the histological brain age estimation algorithm.
The hippocampus is known to be involved in both brain aging and age-dependent neurodegenerative diseases, and thus is an ideal region for this analysis.
The team then trained a machine learning model to estimate a person’s age at death based solely on the digitized section, a task that is impossible for a human observer to perform with any degree of accuracy. They used the difference between the model-predicted age and actual age to derive the amount of age acceleration in the brain.
Results :
When compared with current measures of age acceleration (e.g., DNA methylation), they found that HistoAge-based age acceleration had stronger associations with cognitive impairment, cerebrovascular disease, and the levels of Alzheimer’s-type abnormal degenerative protein aggregation.
The study found that the HistoAge model is a reliable, independent metric for determining brain age and understanding factors that drive neurodegeneration over time.
Why the Research Is Interesting :
The researchers said the HistoAge model, and other subsequent similar algorithms, represent an entirely new paradigm for assessing aging and neurodegeneration in human samples and can easily be deployed at scale in clinical and translational research laboratories. Further, this approach provides more rigorous, unbiased and robust metrics of cellular changes underlying degenerative diseases.
The team will next build a multicenter collaboration to develop a large AI-ready dataset that will be used to develop even more powerful AI models that have the potential to transform and enhance our understanding of brain diseases.
Said Mount Sinai’s Dr. Crary of the research: “AI’s disruptive influence on brain research is a paradigm shift propelling us towards the next generation of cures. The HistoAge model will enable us to uncover crucial causal aspects of debilitating brain diseases such as Alzheimer’s disease.”
Said Mount Sinai’s Dr. Farrell of the research: “Using the latest computational approaches, like AI, on human tissue samples from Mount Sinai’s vast and diverse collections is a shift in the way we assess human diseases. Our novel HistoAge model is just one example of the way AI is paving the way for further discovery about the mechanisms of aging and neurodegeneration.
“Clinical scientists are increasingly using AI in research and diagnostic settings. It’s a tool that is revolutionizing medicine and we are excited to be leaders in this space, optimizing machine learning—not to replace our Health System’s commitment to compassionate care, but to improve diagnosis and treatment for all patients.”
Said Mount Sinai’s Dr. Marx of the research: “This model opens the floodgates for a slew of fascinating and essential analyses that bring us closer to finally understanding the aging brain and age-related brain diseases such as Alzheimer’s. This is the first time we have been able to put a number to how much aging there is in the brain in pathology.
“With this approach, we can discover genes that protect against brain aging or genes that make aging worse in the brain, as well as discover the environmental risk factors that make individuals’ brains age faster.” Funding: The study was supported by funding from the National Institutes of Health (R01AG054008, R01NS095252, R01AG060961, R01NS086736, P30AG066514, P50AG005138, R01AG062348, U24MH100931, and K01AG070326), Alzheimer’s Disease Research Center (P30 AG066514), the Winspear Family Center for Research on the Neuropathology of Alzheimer Disease, Rainwater Charitable Foundation / Tau Consortium, and a generous gift from Stuart Katz and Jane Martin. Researchers from the University of Pennsylvania and Boston University contributed to this study. About this AI and brain aging research Author: Stacy Anderson Source: Mount Sinai Hospital Contact: Stacy Anderson – Mount Sinai Hospital Image: The image is credited to Neuroscience News Original Research: Open access. “ Histopathologic Brain Age Estimation via Multiple Instance Learning ” by John F. Crary et al. Acta Neuropathologica Abstract Histopathologic Brain Age Estimation via Multiple […]
